Abstract
The use of electronic cigarettes (e-cigarette) and vaping devices started as a potential aid for cessation and reducing the harmful consequences of cigarette smoking, mainly in the adult population. Today e-cigarette use is highly increasing in vulnerable populations, especially young and pregnant women, due to the misconception of its harmless use.
Despite the growing acknowledgment in e-cigarette as a potential harmful device, and due to mixed information found concerning its beneficial aid for smokers, along with an insufficient clinical study done in human models, it is important to further evaluate the possible benefits and risks of non-combusting, vaping nicotine or non-nicotine delivery devices.
In this review we tried to summarize the latest updated information found in the literature, concentrating mainly in the variety of adverse effects of e-cigarette use and its contribution for recent and future health concerns.
Similar content being viewed by others
Introduction
Tobacco smoke undoubtedly remains world’s leading cause of preventable disease [1]. Over the last decade, reducing cigarette consumption has become a Public Health goal, therefore prevention campaigns intensified and restrictions on their marketing and access escalated [2].
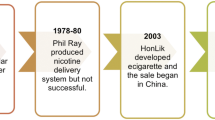
Electronic cigarettes (also known as E-cigs, Electronic Nicotine Delivery Systems-ENDS, vaping device or e-vaporizers) are an electronic device that can vary in size and shape, consisting of a battery, an electrical heater and a liquid, which is aerosolized to be inhaled. Liquid composition can include nicotine, a solvent and an utmost variety of flavorants [3]. Taking shape as a smoking cessation strategy or – in actual fact – as a legal alternative where conventional smoking was prohibited, e-cigarettes, invented by Hon Lik (a Chinese pharmacist), were patented in 2003. However, only in 2007 they became commercially available in USA and Europe [4].
In contrast with a consistent decline in smoking prevalence among youth [5], over the past few years electronic cigarettes have rapidly gained popularity to the point of becoming the most common tobacco product in this age group [6]. Their social acceptance, together with their widespread availability, contributed to drastically increase primary use by adolescents and second-hand exposure in children, outlining the need for an assessment of their health effects in these categories [7].
In 2018, the National Youth Tobacco Survey reported that 20.8% of high school students and 4.9% of middle school students currently used e-cigarettes [8]. Since the introduction of pod-based devices, vaping prevalence has tremendously increased, reaching 28% in 2019 [9] and even 40.5% among 12th graders [10]. In Great Britain, during 2020 16.4% of 11–18-year-old students had tried (at least once) e-cigs, compared to 15.4% in 2019 and to 12.7% in 2015. Also current use increased since 2015 from 2.4 to 4.8% [11]. Prevalence of current e-cigarette smokers in Italy doubled from 2014 (8%) to 2018 (18%), whereas the number of ever smokers has risen by 60% (from 28 to 44%) [12]. According to forecasts, e-cigarettes sales will surpass those of traditional tobacco by 2023 [13].
Marketing has certainly played a major role in vaping prevalence inflection among children and adolescents. E-cigarettes can be purchased in vape shops, tobacco vendors, gas stations, groceries, pharmacies and even online [14]. The manufacturing companies, often owned by tobacco firms, address their products to youth by promoting appealing flavours and using multiple communication channels: television advertisings; targeted advertisements at the point of sale; web sites and social media; celebrity partnerships; free samples at youth-oriented events [15,16,17]. In 2016, 78.2% of middle and high school students have been exposed to e-cigarette advertisements from at least 1 source and increasing exposure seemed associated with higher odds of use [17]. Social media are easily accessible by teenagers and convey the use of e-cigarettes as socially acceptable [18]; despite ENDS being born as a smoking cessation strategy, less than 1% of twitter posts concerning vaping are related to smoke cessation [19]. Apparently, only 8% of adolescents take up e-smoking as a nicotine replacement strategy [20] whereas the most common reasons underlying vaping experimentation in pediatric population are: curiosity, social influence, availability at low cost, enjoyable flavors, ease of concealment [21,22,23]. Sustained use is then encouraged by misperceptions about safety, nicotine content and social prevalence [21, 24,25,26].
A cross-sectional analysis pointed out that positive expectancies regarding e-cigarette use (e.g. gaining respect of peers and chances of being liked by partners, reducing stress, enjoying throat sensation) are related with a greater prevalence of current use [27]. Users exhibit the lowest perceptions of harm and more positive attitudes towards e-cigarettes when compared with non-users [28]. Adolescents perceptions – which affect their decision-making process – are generally biased in the direction of their own experience, a phenomenon referred to as “false consensus effect”[29]: for instance, teens tend to overestimate actual smoking rate among peers [30], therefore they may be more prone to develop such addiction. In this regard, Gorukanti et al. [28] administered 9th and 12th graders from California an online survey to investigate their attitudes towards e-cigarettes and whether they differ by past use. Findings showed that prevalence of both e-cigarette and cigarette use among parents, siblings, and close friends was higher in adolescents who have ever used an e-cigarette. At the same time, vapers believed more peers and relatives smoke e-cigarettes than do non-users. A worrying percentage of participants, especially smokers, thought that e-cigs contained water and claimed that vaping felt cleaner and safer than traditional smoking. Nonusers, instead, were more prone to consider e-cigarette harmful to children.
Device evolvement
Throughout the years, e-cigarettes design and technical features evolved, providing the market with updated products meeting consumers’ different demands. E-cigarette’s modernisation process also helped contain health implications. First generation ECs, usually referred to as cig-a-likes, have been conceived to resemble the design and feeling of traditional cigarettes. In early models, friable solder joints could release in aerosols particles of tin (associated with stannosis and pneumoconiosis [30]), a flaw remedied by coating the thick wire with silver, using rigid joints external to the atomizer or connecting wires without solders rather through clamps [31, 32]. The thick nickel or copper wire, tin- or silver-coated, was not included in second generation products and following [33]. By removing the silicon cover from later products, its presence in aerosols drastically decreased [34]. Nonetheless, the empowerment in second and third generation batteries, along with bigger atomizers and higher amounts of metal, allowed to generate larger volumes of aerosol [35], resulting at the same time in a greater transfer of particles, metals, toxicants [36, 37]. Furthermore, as voltage/power ratio increased, new potentially toxic by-products could emerge from the liquid [34]. Likewise, in larger reservoirs such as those of second and third generation ECs, fluid stagnation could enrich aerosols with additional toxicants through repeated use [37]. Fourth generation ECs, referred to as pod mod devices, have become popular among teenagers as a socially acceptable alternative to conventional cigarettes due to their stylish design (e.g. USB or teardrop shape), wide selection of flavours and user-friendly functions [38, 39]. Their likeness to an USB memory stick allows them to be discretely used in no smoking areas and easily concealed from parents, contributing to a new widespread phenomenon, known as “stealth vaping” [19, 40, 41]. A distinctive feature of fourth generations devices is the use of nicotine in its protonated form, which reduces the irritating effect on throat mucosa while increasing the amount of nicotine delivered in aerosols [42]. The heterogeneity outlined above complicates research on potential health effects, since the variability in design and technical features prevents us from discussing e-cigarettes as a single device. Furthermore, besides type and age of the device, e-cigarette health impact depends on multiple variables including ambient factors (e.g. climate conditions, room size and density of people) and user’s habits (puff length and frequency) [43].
Content
Aerosol composition is affected even by the solvent employed, being vegetable glycerin (VG), propylene glycol (PG) and their mixture the most widely used. They can also influence particle-size distribution, therefore the region of deposition in the respiratory system [44]. A higher percentage of propylene glycol seems enhancing flavour and strengthening the so-called “throat hit”, whereas a higher percentage of vegetable glycerine may increase vapor production [45]. Vegetable glycerine exposure has been associated with irritation of eyes, lungs, and oesophagus mucosa [46]. Likewise, its higher boiling point requires the heating element to reach higher temperatures, resulting in a greater risk of toxicants emission [47]. The highest yield of aldehydes occurs in devices containing propylene glycol [48], also related to upper respiratory infection-like symptoms [49].
A vast amount of studies aimed at characterizing e-cigarettes emissions and variously reported measurable amounts of ethanol, volatile organic compounds (VOCs), polycyclic aromatic hydrocarbons (PAHs), silicon, lead, nickel, air pollutant, formaldehyde, acetaldehyde, isoprene, acetic acid, 2-butanodione, acetone, and propanol [50,51,52]. Volatile organic compounds can provoke eye and respiratory tract irritation, neurological impairment and liver damage [53]. Polycyclic aromatic hydrocarbons demonstrated carcinogenic, respiratory, immunological, neurological and reproductive effects [54]. Reactive carbonyls such as aldehydes and acrolein (product of glycerol constituents vaporization [55]) elicit airway constriction, direct damage to airway epithelium and alterations in gene expression, in addition to neutrophils activation, degranulation and apoptosis [56].
The extraordinarily wide variety of flavorants available amplifies the heterogeneity in E-cigs aerosol composition. These chemical components are generally employed in food industry and recognized as safe additives but this does not imply their harmlessness when inhaled [57]. Some are known allergens (e.g. cinnamaldehyde for cinnamon aroma) [58], others may provoke ocular and airway irritation (e.g. benzaldehyde for fruity aromas) [59]. Pre-clinical studies demonstrated that flavoring chemicals elicit pro-inflammatory responses in lung epithelial cells and fibroblasts and decrease transepithelial resistance in bronchial epithelial cells [60]. Likewise, diacetyl and acetyl propionyl (butter flavoring volatiles) seem to underlie bronchiolitis obliterans, as seen in microwave pop-corn producing factory workers [61, 62]. Besides, flavored e-cigarettes are misleadingly considered less harmful than those with tobacco flavor, therefore used carelessly by youth [63].
An additional concern is represented by the inconsistencies between declared nicotine levels and actual nicotine content, which have been detected even in liquids supplied from the same company [64].
Moreover, e-cigs nicotine derives from tobacco plant, thus e-liquid can include other tobacco-related toxicants, such as tobacco-specific nitrosamines (TSNAs) [65].
Vaping health implications
An uncountable amount of studies aimed at evaluating e-cigarette potential consequences on human health and the most updated panorama of scientific literature provides increasing evidence of vaping harmfulness. According to the centre for disease control and prevention (CDC) [66], although e-cigarettes harmful effects are fewer in comparison to burned cigarettes, they are considered unsafe, harmful for brain development and increase the risk to future addictions especially in kids, adolescence and young adults.
Respiratory effects
Among e-cigarettes adverse health effects, respiratory impact is by far the most extensively studied. In the same way as conventional cigarettes smokers, vapers’ pulmonary epithelium is typically damaged [67] and bronchial mucosa chronically inflamed [68]. Proteomics of e-cigarette users’ sputum document higher levels of myeloperoxidase, neutrophil elastase and proteinase-3, indicative of neutrophil activation. Furthermore, chronic vapers’ neutrophils display a greater propensity for NET formation when compared to cigarette smokers or non-smokers [56]. The significant decrease in Forced Expiratory Volume in 1 s and fractional exhaled Nitrogen Oxide, both observed in e-cigarette users, are suggestive of an underlying bronchial inflammation [68,69,70].
From a clinical perspective, these pathophysiological alterations could underlie the considerable increase in asthma and bronchitic symptoms reported by e-cigarettes users, especially adolescents. According to various studies involving high school students, vapers have a twofold higher risk of chronic cough, phlegm or dyspnea, together with a greater incidence of asthma [71, 72]. A higher prevalence of e-cigarette use is reported among adults living with a child affected by asthma [73], whose risk of acute exacerbation can increase by 30% [74]. Schoolwork is indirectly affected too, as a result of absenteeism secondary to the aforementioned symptoms [75]. Preclinical studies [76] suggest also a detrimental effect on mucociliary clearance which, coupled with a decreased cough sensitivity [77] and the overexpression of PAF-R (pneumococci’s receptor [78]), predispose vapers to increased rates of pneumonia [79].
In parallel to the increasingly wide distribution of e-cigarette, a growing number of cases helped characterize a new nosological entity, which is now referred to as E-cigarette or Vaping Associated Lung Injury (EVALI). It is a diagnosis of exclusion that requires use of e-cigarettes and related products within the previous 90 days, in addition to pulmonary infiltrates on imaging [80]. The prevalence seems higher in youth: indeed, the median age of the initially reported cases was 19 [81]. The hypothesized causative agent of lung injury is vitamin E acetate, which may be found in cartridges of THC flavored e-cigarettes, widespread among high school students [82]. Its aerosolization generates ketene, that is irritant to airways and disrupts phospholipid bilayer decreasing surfactant effectiveness [83]. EVALI can occur with shortness of breath, cough, tachycardia, tachypnea, pleuritic pain and rarely hemoptysis. Nausea and abdominal pain, as well as fevers and chills are not infrequent. Up to 30% of the affected require mechanical ventilation and up to 70% the admission to intensive care units [83,84,85]. Bilateral lower-lobe predominant ground glass and consolidative opacities with subpleural sparing are the most typical findings at chest imaging. Other possible radiographic patterns include multiple dense consolidations (as in Acute Respiratory Distress Syndrome), multifocal patchy opacities (as in Cryptogenic Organizing Pneumonia) or ground glass pattern with air trapping (as in hypersensitivity pneumonitis) [85, 86]. A bronchoscopy with Broncho-Alveolar Lavage and, if possible, transbronchial biopsies should be performed after ruling out cardiac causes (through chest X-rays and/or echocardiography) and other respiratory or systemic infections (viral assay, urine, sputum and blood cultures), consistently with clinical severity [83, 87]. Steroids should be started concomitantly with antibiotics, especially in patients with respiratory failure; in less severe presentations they can be delayed after infectious causes are ruled out. Response to methylprednisolone is generally excellent [84]. Based on the severity of the clinical picture, patients can benefit from high-flow oxygen therapy, noninvasive ventilation or require mechanical ventilation [81, 84, 88].
Case reports point out an association between e-cigarette smoking and lipoid pneumonia, acute eosinophilic pneumonia, subacute bronchial toxicity and even reversible cerebral vasoconstriction syndrome [89,90,91,92].
Cardiovascular effects
Laboratory studies have pointed out that exposure to e-cigarette can induce platelet aggregation by upregulating expression of CD41 (GPIIb), CD42b, and CD62p (P-selectin) [93]. It also underlies oxidative stress elevation, impairment of antioxidant defenses (vitamin E reduction) and endothelium dysfunction/damage, evidenced by the detection of endothelial progenitor cells and microvescicles into the bloodstream [94,95,96]. All these alterations could play a role in cardiovascular risk increasement. It has been proven, indeed, that daily vaping represents an independent risk factor for myocardial infarction [97], synergically amplified by exposure to nicotine, a parasympathomimetic alkaloid increasing heart rate and blood pressure [98]. Additionally, a 30 minutes vaping session seems inducing an unfavorable effect on aortic stiffness similar to traditional smoking [99].
Neurological effects
Nicotine is widely recognized as a psychoactive substance [100]. Vapers experience craving, impaired capacity to stop and withdrawal symptoms during abstinence (e.g. irritability), which all suggest e-cigs potential of inducing nicotine dependence [101, 102]. Similarly to other substance use disorders, adolescents are characteristically more vulnerable to addiction [103].
Despite ENDS representing a tobacco cessation strategy, the risk of transition to conventional cigarettes in previously never smokers represents an emerging issue of critical relevance, especially in young people [104,105,106,107]. A recent meta-analysis showed that in a population of teens and young adults who have never smoked, odds of smoking initiation were 3 to 6 times higher in those who have ever used e-cigarettes [108]. Evidence suggest also that elevated nicotine concentrations may heighten the likelihood of progression [109]. In this perspective, the renormalization of a smoking culture among teenagers threatens to subvert decades of anti-smoking efforts.
Structural and neurochemical changes in the central nervous system lie beneath the behavioral evolution that characterizes adolescence. Against this background, nicotine can affect its regular course, contributing to attention and cognitive deficits and exacerbating mood disorders [110].
Furthermore, in such a critical phase of human development, nicotine exposure may prime the brain’s reward system increasing pleasing effects of other substances of abuse [111, 112]. As evidence of this, youngsters smoking e-cigarettes display a greater risk of co-occurring alcohol and/or marijuana use [113].
Gastroenteric effects
In spite of small evidence on the matter, e-cigarettes’ detrimental effects do not spare gastrointestinal system. Smoking represents a well-known risk factor for gastro-esophageal reflux, especially since nicotine has been shown to regulate transient lower esophageal sphincter relaxations [114]. Electronic nicotine delivery systems have been associated to esophageal symptoms and are now considered potential triggers of esophagitis exacerbations [115]. Animal studies pointed out that vaping can induce hepatic steatosis through heterogeneous mechanisms, involving oxidative stress, hepatocytes apoptosis and impairment of cholesterol and lipid metabolism [116]. A recent case report documented e-cigs-induced hepatic injury even in humans, describing an increase of liver enzymes in a young vaper presenting to the emergency department for fever, abdominal pain, vomiting and diarrhea [117]. In this regard, clinicians must always consider – or better solicit – patient’s vaping history, since health effects of electronic cigarettes are disparate and sometimes unexpected.
Acute adverse effects
As regards e-cigarettes potential harmful effects, consideration should be given to acute injuries. A fair amount of reports to poison centers concern children incidentally exposed to e-cig liquids through ingestion (70%), inhalation (15%), ocular (8.5%) and dermal contact (6%) [118]. Nicotine poisoning can result in tachycardia, dizziness and even seizures [119]. Ingestion of 0,1 mg/kg of nicotine-containing fluid can be fatal to a child [7]. Acute exposure to e-cigarettes seems associated with a worse prognosis compared with that of conventional tobacco [120]. As electronic devices, batteries could also explode provoking severe burns [121].
Second- and thirdhand exposure
Concerning e-cigarettes impact on pediatric population, an often-underestimated aspect is second- and third-hand smoke. Approximately 20% of parents using e-cigarettes follow strictly enforced vape-free home and car policies; among dual users, 64% has a smoke-free and only 26% a vape-free home policy, which implies a general misperception about e-cigarettes safety, especially among younger parents [122]. There is evidence that nicotine metabolites in serum, as well as saliva and urine cotinine levels, are superimposable among non-using adults secondhandedly exposed to e-cigarettes and conventional cigarettes [123]. Even secondhand particular matter exposure levels can equal that of traditional smoking [124] and appear to be greater in nicotine-free devices [125].
Vaping during pregnancy (fetal developmental effects)
Of no less importance is fetal exposure to nicotine during pregnancy. Vaping prevalence in pregnant women has been estimated to stand between 0.6 and 15% [126]. Nicotine can cross the placenta and measurable nicotine levels can been detected in offspring of mothers smoking during pregnancy [127]. In uterus nicotine exposure increases the risk for eclampsia, premature birth, cleft lip and palate, reduced birth weight [128,129,130], sudden infant death syndrome, altered corpus callosum, auditory defects, besides being related to future compromised fertility, type 2 diabetes, obesity, hypertension and respiratory dysfunction [131, 132]. Nicotinic acetylcholine receptors regulate critical stages of brain development and nicotine neurotoxic effects on the developing brain have been widely demonstrated, including future hyperactivity, cognitive impairment, anxiety, mood and attention symptoms, sensitivity to stimulant drugs [131, 133,134,135,136,137]. To date, e-cigarette impact on pregnant women and fetuses remains uncertain and further research should be established. A vast amount of studies carried out on animal models suggest pre- and postnatal alterations related with the exposure to both, nicotine and nicotine-free aerosols, including the down-regulation of genes implied in lung development [138], an inverse relationship between plasma and urine cotinine level and body weight [139], in addition to neuro-behavioural and developmental disorders similar to those resulting from conventional cigarette exposure [140].
E-cigarettes and COVID-19
In the course of COVID-19 pandemic, forced social isolation due to quarantine measures has been associated with the onset and exacerbation of psychological problems, including substance use [141]. Boredom, loneliness, and loss of daily structure during confinement led people to consume larger quantities of alcohol and smoke more cigarettes, an ever-worrying global concern [142]. In Italy, e-cigarette use increased by 12.1% and almost 2% of non-users started vaping during the lockdown, especially vulnerable categories such as youngsters, drug-addicted (of less available substances) or people experiencing anxiety symptoms (worsened by the pandemic background) [143]. In such a dramatic framework, e-cigarette companies seized the moment to exploit a global pandemic for their marketing purposes: using tv advertising and social media (hence addressing to younger customers) they offered pandemic supplies (e.g., masks, hand sanitisers) as gifts with the purchase of their products, suggested online shopping with pandemic-themed discount codes (e.g. “STAYHOME”) and encouraged home vaping to cope with confinement-related stress [144].
Most concerning is that smoking and vaping has proven to impact on individual’s susceptibility to coronavirus infection, rate of symptomatic disease course other than overall prognosis [145,146,147]. E-cigs users display indeed a 5–7 times higher risk of COVID-19 diagnosis compared to non-users [145]. Mask removal and the gesture of vaping facilitate viral hand-to-mouth transmission (especially with shared devices), increasing smokers’ susceptibility to infections, which is synergically enhanced through lung inflammation, impaired clearance, oxidative stress and immune dysregulation [147]. Angiotensin-converting enzyme 2 (ACE-2), a ubiquitous transmembrane metallocarboxypeptidase, is the receptor SARS-CoV2 utilizes to enter human cells [147]. Recent research provides evidence that a nicotine-related overexpression of ACE-2 in bronchial epithelial cells is mediated by α7-subtype nicotinic receptors (nAChRα7), which could facilitate SARS-CoV2 biological cycle [148, 149]. Furthermore, chronic exposure to nicotine aerosol seems responsible for lung inflammation through a dysregulated repair response and extracellular matrix remodelling mediated by nAChRα7 itself [150]. In this regard, ECs may not only ease virus entry, but even exacerbate the resulting lung injury. E-cigarettes detrimental effects are not confined to respiratory involvement: vaping and its consequent low-grade brain inflammation results in a procoagulant condition increasing stroke risk, a known and fearsome complication of SARS-CoV2 infection [151]. Although direct evidence remains forthcoming, such mechanisms are supposed to be mediated by ACE-2 pro-inflammatory pathway, which is extensively expressed in central nervous system too [147]. Electronic smoking has also been proven to adversely affect the clinical course of SARS-CoV2 infection: McFadden et al. recorded significantly higher rates of COVID-19 symptoms among vapers when compared to non-users, with manifestations of increased severity in dual users (traditional and e-cigarettes) [152]. Within the framework of the ongoing COVID-19 pandemic, such findings oriented the scientific interest towards the relationship between SARS-CoV2 and exposure to nicotine, yet current literature provides inconsistent conclusions. Cross-sectional data from HEBECO study excluded any association between COVID-19 diagnosis and vaping habits [153], while Miyara and colleagues have even documented a lower probability of a symptomatic or severe disease in current smokers as compared to the general population [154]. This led to hypothesize that nicotine might achieve a preventive effect. nAChRα7s are known to modulate the phlogistic response by calcium-mediated activation under inflammatory conditions (such as cytokine storm in severe COVID-19) thus some Authors speculate that nicotinic agents might represent a therapeutic opportunity for acute COVID-19 [155, 156]. In the light of available evidence, we can presume that nicotine antiphlogistic effect (potentially achieved through nAChRα7 modulation) mitigates the inflammatory response to the virus and acute lung injury, but chronic exposure may possibly increase the susceptibility to its infection [147].
Interestingly, SARS-CoV2 respiratory involvement is associated with an increase of CCL2–4 levels in bronchoalveolar fluid and mononuclear cells, an alteration recorded also in EVALI, whose clinical and radiological presentation is to a certain extent similar [157,158,159]. Chest imaging can occasionally help narrow the diagnosis since COVID-19 frequently presents with multifocal ground-glass peripheral opacities, on the contrary subpleural sparing is common in vaping-associated lung injury [160]. Despite the absence of pathognomonic features, EVALI should be considered in younger patients, displaying leucocytosis and responsive to corticosteroids (being COVID-19 more likely in older ages and often associated with lymphopenia) [159]. Accordingly, vaping history should always be investigated – and excluded – in young patients presenting to emergency departments for acute fever and respiratory symptoms, especially in individuals with no epidemiologic links to SARS-CoV2 infection [158, 161].
Conclusions
Traditional tobacco impairing effects have been widely demonstrated, in contrast, vaping mid- and long-term complications remain unclear. Nonetheless, there is increasing evidence that e-cigarettes can no longer be considered as harmless devices. As a result of vaping cross-generational diffusion, e-cigarettes health implications have become an issue of pediatric interest since children are at greater risk of their chronic effects. Despite its lesser harmfulness than traditional smoking, a vast amount of research revealed that vaping is far from being safe. Its risk-benefit ratio remains acceptable only if used as a smoking-cessation device, available under medical prescription for teenagers truly planning to quit traditional smoking for good. The remaining pediatric population does not get any benefit from electronic smoking. Therefore, based on a precautionary principle e-cigarettes should in any event be considered unhealthy hence consequently banned in this age group and restricted in its close contacts. In this perspective, governments should strengthen prevention strategies as well as restrictions and regulations on e-cigarettes marketing and advertisings. In parallel, teachers and pediatricians must play a crucial role in children and parents’ education by raising their awareness about vaping harmful effects and dispelling widespread misperceptions. Given its ever-growing relevance as a worldwide health concern, further investigation in this regard is in our main interest.
Availability of data and materials
N/A
References
Heiss C. Electronic cigarettes: Replacing one evil with another? Eur J Prev Cardiol. 2019;26(11):1217–8.
Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013;23(2):103–12.
Thirion-Romero I, Pérez-Padilla R, Zabert G, Barrientos-Gutierrez I. Respiratory impact of electronic cigarettes and low-risk tobacco. Rev Investig Clin. 2019;71(1):17–27.
Gravely S, Fong GT, Cummings KM, Yan M, Quah AC, Borland R, et al. Awareness, trial, and current use of electronic cigarettes in 10 countries: Findings from the ITC project. Int J Environ Res Public Health. 2014;11(11):11691–704.
Gorini G, Gallus S, Carreras G, Cortini B, Vannacci V, Charrier L, et al. A long way to go: 20-year trends from multiple surveillance systems show a still huge use of tobacco in minors in Italy. Eur J Pub Health. 2019;29(1):164–9.
Jenssen BP, Walley SC; SECTION ON TOBACCO CONTROL. E-cigarettes and similar devices. Pediatrics. 2019;143(2):e20183652.
Binns C, Lee MK, Low WY. Children and E-Cigarettes: a new threat to health. Asia Pac J Public Health. 2018;30(4):315–20.
Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students - United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276–7.
Cullen KA, Gentzke AS, Sawdey MD, Chang JT, Anic GM, Wang TW, et al. e-Cigarette Use Among Youth in the United States, 2019. JAMA. 2019;322(21):2095–103.
Miech R, Johnston L, O'Malley PM, Bachman JG, Patrick ME. Trends in Adolescent Vaping, 2017-2019. N Engl J Med. 2019;381(15):1490–1.
ASH. Use of e-cigarettes among young people in Great Britain. https://ash.org.uk/wp-content/uploads/2021/02/YouthEcig2020.pdf. Published 2021. Accessed 15 Mar 2021.
Gorini G, Gallus S, Carreras G, et al. Prevalence of tobacco smoking and electronic cigarette use among adolescents in Italy: Global Youth Tobacco Surveys (GYTS), 2010, 2014, 2018. Prev Med (Baltim). 2020;131:105903.
Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Phys Lung Cell Mol Phys. 2017;313(2):L193–206.
Frieden TR, Jaffe HW, Richards CL, Iademarco MF. E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. Mmwr; 2014.
Duke JC, Lee YO, Kim AE, Watson KA, Arnold KY, Nonnemaker JM, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–36.
Richardson A, Ganz O, Vallone D. Tobacco on the web: surveillance and characterisation of online tobacco and e-cigarette advertising. Tob Control. 2015;24(4):341–7.
Singh T, Agaku IT, Arrazola RA, Marynak KL, Neff LJ, Rolle IT, et al. Exposure to Advertisements and Electronic Cigarette Use Among US Middle and High School Students. Pediatrics. 2016;137(5):e20154155.
Ayers JW, Leas EC, Allem JP, Benton A, Dredze M, Althouse BM, et al. Why do people use electronic nicotine delivery systems (electronic cigarettes)? A content analysis of Twitter, 2012-2015. PLoS One. 2017;12(3):e0170702.
Allem JP, Dharmapuri L, Unger JB, Cruz TB. Characterizing JUUL-related posts on Twitter. Drug Alcohol Depend. 2018;190:1–5.
Tsai J, Walton K, Coleman BN, Sharapova SR, Johnson SE, Kennedy SM, et al. Reasons for Electronic Cigarette Use Among Middle and High School Students - National Youth Tobacco Survey, United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(6):196–200.
Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17(7):847–54.
Bold KW, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for Trying E-cigarettes and Risk of Continued Use. Pediatrics. 2016;138(3):e20160895. https://doi.org/10.1542/peds.2016-0895 Epub 2016 Aug 8. Erratum in: Pediatrics. 2018 Dec;142(6).
Singh S, Windle SB, Filion KB, Thombs BD, O'Loughlin JL, Grad R, et al. E-cigarettes and youth: Patterns of use, potential harms, and recommendations. Prev Med. 2020;133:106009.
Ambrose BK, Rostron BL, Johnson SE, Portnoy DB, Apelberg BJ, Kaufman AR, et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2 Suppl 1):S53–60.
Anand V, McGinty KL, O'Brien K, Guenthner G, Hahn E, Martin CA. E-cigarette Use and Beliefs Among Urban Public High School Students in North Carolina. J Adolesc Health. 2015;57(1):46–51.
Roditis M, Delucchi K, Cash D, Halpern-Felsher B. Adolescents’ perceptions of health risks, social risks, and benefits differ across tobacco products. J Adolesc Health. 2016;58(5):558–66.
Pokhrel P, Little MA, Fagan P, Muranaka N, Herzog TA. Electronic cigarette use outcome expectancies among college students. Addict Behav. 2014;39(6):1062–5.
Gorukanti A, Delucchi K, Ling P, Fisher-Travis R, Halpern-Felsher B. Adolescents’ attitudes towards e-cigarette ingredients, safety, addictive properties, social norms, and regulation. Prev Med. 2017;94:65–71.
Henry DB, Kobus K, Schoeny ME. Accuracy and bias in adolescents' perceptions of friends' substance use. Psychol Addict Behav. 2011;25(1):80–9.
Rimal RN, Real K. How behaviors are influenced by perceived norms a test of the theory of normative social behavior. Commun Res. 2005;32(3):389–414.
Williams M, Ghai S, Talbot P. Disposable electronic cigarettes and electronic hookahs: evaluation of performance. Nicotine Tob Res. 2015;17(2):201–8.
Hua M, Omaiye EE, Luo W, McWhirter KJ, Pankow JF, Talbot P. Identification of Cytotoxic Flavor Chemicals in Top-Selling Electronic Cigarette Refill Fluids. Sci Rep. 2019;9(1):2782.
Williams M, Bozhilov KN, Talbot P. Analysis of the elements and metals in multiple generations of electronic cigarette atomizers. Environ Res. 2019;175:156–66.
Williams M, Talbot P. Design features in multiple generations of electronic cigarette atomizers. Int J Environ Res Public Health. 2019;16(16):2904.
Fox L. The Basics of Vaping - Types of E-Cig Atomizers and Vape Tanks. https://ecigarettereviewed.com/types-of-atomizer/. Accessed 7 Mar 2021.
Hess CA, Olmedo P, Navas-Acien A, Goessler W, Cohen JE, Rule AM. E-cigarettes as a source of toxic and potentially carcinogenic metals. Environ Res. 2017;152:221–5.
Olmedo P, Goessler W, Tanda S, Grau-Perez M, Jarmul S, Aherrera A, et al. Metal Concentrations in e-Cigarette Liquid and Aerosol Samples: The Contribution of Metallic Coils. Environ Health Perspect. 2018;126(2):027010.
Omaiye EE, McWhirter KJ, Luo W, Pankow JF, Talbot P. High-Nicotine Electronic Cigarette Products: Toxicity of JUUL Fluids and Aerosols Correlates Strongly with Nicotine and Some Flavor Chemical Concentrations. Chem Res Toxicol. 2019;32(6):1058–69.
Kavuluru R, Han S, Hahn EJ. On the popularity of the USB flash drive-shaped electronic cigarette Juul. Tob Control. 2019;28(1):110–2.
Barrington-Trimis JL, Leventhal AM. Adolescents’ Use of “Pod Mod” E-Cigarettes - Urgent Concerns. N Engl J Med. 2018;379(12):1099–102.
Yingst JM, Lester C, Veldheer S, Allen SI, Du P, Foulds J. E-cigarette users commonly stealth vape in places where e-cigarette use is prohibited. Tob Control. 2019;28(5):493–7.
Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ. 2019;366:1–16.
Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23(SUPPL. 2):ii36–40.
Etter JF, Bullen C, Flouris AD, Laugesen M, Eissenberg T. Electronic nicotine delivery systems: a research agenda. Tob Control. 2011;20(3):243–8.
Li Q, Zhan Y, Wang L, Leischow SJ, Zeng DD. Analysis of symptoms and their potential associations with e-liquids' components: a social media study. BMC Public Health. 2016;16:674.
Phillips B, Titz B, Kogel U, Sharma D, Leroy P, Xiang Y, et al. Toxicity of the main electronic cigarette components, propylene glycol, glycerin, and nicotine, in Sprague-Dawley rats in a 90-day OECD inhalation study complemented by molecular endpoints. Food Chem Toxicol. 2017;109(Pt 1):315–32.
Talih S, Balhas Z, Salman R, Karaoghlanian N, Shihadeh A. “Direct dripping”: a high-temperature, high-formaldehyde emission electronic cigarette use method. Nicotine Tob Res. 2016;18(4):453–9.
Kosmider L, Sobczak A, Fik M, Knysak J, Zaciera M, Kurek J, et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16(10):1319–26.
Laino T, Tuma C, Moor P, Martin E, Stolz S, Curioni A. Mechanisms of propylene glycol and triacetin pyrolysis. J Phys Chem A. 2012;116(18):4602–9.
Fernández E, Ballbè M, Sureda X, Fu M, Saltó E, Martínez-Sánchez JM. Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: a Systematic Review and Observational Study. Curr Environ Health Rep. 2015;2(4):423–9.
Wang G, Liu W, Song W. Toxicity assessment of electronic cigarettes. Inhal Toxicol. 2019;31(7):259–73.
Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10(2):e0116732.
Environmental Protection Agency. Volatile Organic Compounds’ Impact on Indoor Air Quality: Epa; 2018. https://www.epa.gov/indoor-air-quality-iaq/volatile-organic-compounds-impact-indoor-air-quality. Accessed 8 Mar 2021.
Agency for Toxic Substances and Disease Registry (ATSDR). Public Health Statement: Polycyclic Aromatic Hydrocarbons (PAHs). Atlanta: Department of Health and Human Services, Public Health Service; 1995.
Pamies D, Vilanova E. Acrolein. In: Encyclopedia of Toxicology. 3rd ed; 2014.
Reidel B, Radicioni G, Clapp PW, Ford AA, Abdelwahab S, Rebuli ME, et al. E-Cigarette Use Causes a Unique Innate Immune Response in the Lung, Involving Increased Neutrophilic Activation and Altered Mucin Secretion. Am J Respir Crit Care Med. 2018;197(4):492–501.
Breland A, Soule E, Lopez A, Ramôa C, El-Hellani A, Eissenberg T. Electronic cigarettes: what are they and what do they do? Ann N Y Acad Sci. 2017;1394(1):5–30.
Clapp PW, Jaspers I. Electronic Cigarettes: Their Constituents and Potential Links to Asthma. Curr Allergy Asthma Rep. 2017;17(11):79.
Kosmider L, Sobczak A, Prokopowicz A, Kurek J, Zaciera M, Knysak J, et al. Cherry-flavoured electronic cigarettes expose users to the inhalation irritant, benzaldehyde. Thorax. 2016;71(4):376–7.
Gerloff J, Sundar IK, Freter R, Sekera ER, Friedman AE, Robinson R, et al. Inflammatory response and barrier dysfunction by different e-Cigarette flavoring chemicals identified by gas chromatography-mass spectrometry in e-liquids and e-vapors on human lung epithelial cells and fibroblasts. Appl In Vitro Toxicol. 2017;3(1):28–40.
Barrington-Trimis JL, Samet JM, McConnell R. Flavorings in electronic cigarettes: an unrecognized respiratory health hazard? JAMA. 2014;312(23):2493–4.
National Institute for Occupational Safety and Health. Flavorings- Related Lung Disease. https://www.cdc.gov/niosh/topics/flavorings/exposure.html. Accessed 8 Mar 2021.
Pepper JK, Ribisl KM, Brewer NT. Adolescents' interest in trying flavoured e-cigarettes. Tob Control. 2016;25(Suppl 2):ii62–6.
Morean ME, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Nicotine concentration of e-cigarettes used by adolescents. Drug Alcohol Depend. 2016;167:224–7.
Kim HJ, Shin HS. Determination of tobacco-specific nitrosamines in replacement liquids of electronic cigarettes by liquid chromatography-tandem mass spectrometry. J Chromatogr A. 2013;1291:48–55.
CDC. About Electronic Cigarettes. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/about-e-cigarettes.html. Accessed 9 Apr 2021.
Schweitzer KS, Chen SX, Law S, Van Demark M, Poirier C, Justice MJ, et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. Am J Phys Lung Cell Mol Phys. 2015;309(2):L175–87.
Ghosh A, Coakley RC, Mascenik T, Rowell TR, Davis ES, Rogers K, et al. Chronic E-Cigarette Exposure Alters the Human Bronchial Epithelial Proteome. Am J Respir Crit Care Med. 2018;198(1):67–76.
Marini S, Buonanno G, Stabile L, Ficco G. Short-term effects of electronic and tobacco cigarettes on exhaled nitric oxide. Toxicol Appl Pharmacol. 2014;278(1):9–15.
Vardavas CI, Anagnostopoulos N, Kougias M, Evangelopoulou V, Connolly GN, Behrakis PK. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141(6):1400–6.
McConnell R, Barrington-Trimis JL, Wang K, Urman R, Hong H, Unger J, et al. Electronic Cigarette Use and Respiratory Symptoms in Adolescents. Am J Respir Crit Care Med. 2017;195(8):1043–9.
Wang MP, Ho SY, Leung LT, Lam TH. Electronic Cigarette use and respiratory symptoms in Chinese Adolescents in Hong Kong. JAMA Pediatr. 2016;170(1):89–91.
Carwile JL, Fleisch AF, Young K, Ahrens KA. Electronic cigarette use in US households with children: The “New” secondhand smoke. JAMA Pediatr. 2019;173(7):693–5.
Bayly JE, Bernat D, Porter L, Choi K. Secondhand exposure to aerosols from electronic nicotine delivery systems and asthma exacerbations among youth with asthma. Chest. 2019;155(1):88–93.
Cho JH, Paik SY. Association between electronic cigarette use and asthma among High School Students in South Korea. PLoS One. 2016;11(3):e0151022.
Carson JL, Zhou L, Brighton L, Mills KH, Zhou H, Jaspers I, et al. Temporal structure/function variation in cultured differentiated human nasal epithelium associated with acute single exposure to tobacco smoke or E-cigarette vapor. Inhal Toxicol. 2017;29(3):137–44.
Dicpinigaitis PV, Lee Chang A, Dicpinigaitis AJ, Negassa A. Effect of e-Cigarette Use on Cough Reflex Sensitivity. Chest. 2016;149(1):161–5.
Miyashita L, Suri R, Dearing E, Mudway I, Dove RE, Neill DR, et al. E-cigarette vapour enhances pneumococcal adherence to airway epithelial cells. Eur Respir J. 2018;51(2):1701592.
Hwang JH, Lyes M, Sladewski K, Enany S, McEachern E, Mathew DP, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med (Berl). 2016;94(6):667–79.
Cherian SV, Kumar A, Estrada-Y-Martin RM. E-Cigarette or vaping product-associated lung injury: a review. Am J Med. 2020;133(6):657–63.
Layden JE, Ghinai I, Pray I, Kimball A, Layer M, Tenforde MW, et al. Pulmonary illness related to E-cigarette use in Illinois and Wisconsin - Final Report. N Engl J Med. 2020;382(10):903–16.
Kowitt SD, Osman A, Meernik C, Zarkin GA, Ranney LM, Martin J, et al. Vaping cannabis among adolescents: prevalence and associations with tobacco use from a cross-sectional study in the USA. BMJ Open. 2019;9(6):e028535.
Blount BC, Karwowski MP, Shields PG, Morel-Espinosa M, Valentin-Blasini L, Gardner M, et al. Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI. N Engl J Med. 2020;382(8):697–705.
Kalininskiy A, Bach CT, Nacca NE, Ginsberg G, Marraffa J, Navarette KA, et al. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. Lancet Respir Med. 2019;7(12):1017–26.
Triantafyllou GA, Tiberio PJ, Zou RH, Lamberty PE, Lynch MJ, Kreit JW, et al. Vaping-associated acute lung injury: a case series. Am J Respir Crit Care Med. 2019;200(11):1430–1.
Henry TS, Kanne JP, Kligerman SJ. Imaging of vaping-associated lung disease. N Engl J Med. 2019;381(15):1486–7.
Mukhopadhyay S, Mehrad M, Dammert P, Arrossi AV, Sarda R, Brenner DS, et al. Lung biopsy findings in severe pulmonary illness associated with E-Cigarette Use (Vaping). Am J Clin Pathol. 2020;153(1):30–9.
Blagev DP, Harris D, Dunn AC, Guidry DW, Grissom CK, Lanspa MJ. Clinical presentation, treatment, and short-term outcomes of lung injury associated with e-cigarettes or vaping: a prospective observational cohort study. Lancet. 2019;394:2073–83.
McCauley L, Markin C, Hosmer D. An unexpected consequence of electronic cigarette use. Chest. 2012;141(4):1110–3.
Thota D, Latham E. Case report of electronic cigarettes possibly associated with eosinophilic pneumonitis in a previously healthy active-duty sailor. J Emerg Med. 2014;47(1):15–7.
Hureaux J, Drouet M, Urban T. A case report of subacute bronchial toxicity induced by an electronic cigarette. Thorax. 2014;69(6):596–7.
Vannier S, Ronziere T, Ferre JC, Lassalle V, Verin M. Reversible cerebral vasoconstriction syndrome triggered by an electronic cigarette: case report. Eur J Neurol. 2015;22(5):e64–5.
Hom S, Chen L, Wang T, Ghebrehiwet B, Yin W, Rubenstein DA. Platelet activation, adhesion, inflammation, and aggregation potential are altered in the presence of electronic cigarette extracts of variable nicotine concentrations. Platelets. 2016;27(7):694–702.
Antoniewicz L, Bosson JA, Kuhl J, Abdel-Halim SM, Kiessling A, Mobarrez F, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150(3):606–12.
Staudt MR, Salit J, Kaner RJ, Hollmann C, Crystal RG. Altered lung biology of healthy never smokers following acute inhalation of E-cigarettes. Respir Res. 2018;19(1):78.
Alzahrani T, Pena I, Temesgen N, Glantz SA. Association Between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55(4):455–61.
Yan XS, D'Ruiz C. Effects of using electronic cigarettes on nicotine delivery and cardiovascular function in comparison with regular cigarettes. Regul Toxicol Pharmacol. 2015;71(1):24–34.
Vlachopoulos C, Ioakeimidis N, Abdelrasoul M, et al. Electronic cigarette stiffness and blood pressure in young smokers treatment of pure aortic regurgitation using a second-generation. J Am Coll Cardiol. 2016;67(23):2802–3.
Murray JB. Nicotine as a psychoactive drug. J Psychol. 1991;125(1):5–25.
Foulds J, Veldheer S, Yingst J, Hrabovsky S, Wilson SJ, Nichols TT, et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob Res. 2015;17(2):186–92.
Etter JF, Eissenberg T. Dependence levels in users of electronic cigarettes, nicotine gums and tobacco cigarettes. Drug Alcohol Depend. 2015;147:68–75.
Pentz MA, Shin H, Riggs N, Unger JB, Collison KL, Chou CP. Parent, peer, and executive function relationships to early adolescent e-cigarette use: a substance use pathway? Addict Behav. 2015;42:73–8.
Spindle TR, Hiler MM, Cooke ME, Eissenberg T, Kendler KS, Dick DM. Electronic cigarette use and uptake of cigarette smoking: a longitudinal examination of U.S. college students. Addict Behav. 2017;67:66–72.
Bold KW, Kong G, Camenga DR, Simon P, Cavallo DA, Morean ME, et al. Trajectories of E-Cigarette and Conventional Cigarette Use Among Youth. Pediatrics. 2018;141(1):e20171832.
Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–7.
Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–23.
Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. Association between initial use of e-Cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–97.
Goldenson NI, Leventhal AM, Stone MD, McConnell RS, Barrington-Trimis JL. Associations of Electronic Cigarette Nicotine Concentration With Subsequent Cigarette Smoking and Vaping Levels in Adolescents. JAMA Pediatr. 2017;171(12):1192–9.
Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–412.
Agrawal A, Madden PA, Martin NG, Lynskey MT. Do early experiences with cannabis vary in cigarette smokers? Drug Alcohol Depend. 2013;128(3):255–9.
Huang YY, Kandel DB, Kandel ER, Levine A. Nicotine primes the effect of cocaine on the induction of LTP in the amygdala. Neuropharmacology. 2013;74:126–34.
Camenga DR, Kong G, Cavallo DA, Liss A, Hyland A, Delmerico J, et al. Alternate tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smokers. J Adolesc Health. 2014;55(4):588–91.
Kahrilas PJ, Gupta RR. Mechanisms of acid reflux associated with cigarette smoking. Gut. 1990;31(1):4–10.
Pasricha TS, Kochar B. Vaping-associated esophagitis. BMC Gastroenterol. 2021;21(1):106.
Hasan KM, Friedman TC, Shao X, Parveen M, Sims C, Lee DL, et al. E-cigarettes and western diet: important metabolic risk factors for hepatic diseases. Hepatology. 2019;69(6):2442–54.
Fan T, DuBose L, Wayne C, Sisniega C. E-cigarette, or vaping, associated lung and hepatic injury. J Pediatr Gastroenterol Nutr. 2020;71(3):e98–e100.
Collaco JM, McGrath-Morrow SA. Electronic cigarettes: exposure and use among pediatric populations. J Aerosol Med Pulm Drug Deliv. 2018;31(2):71–7.
Govindarajan P, Spiller HA, Casavant MJ, Chounthirath T, Smith GA. E-cigarette and liquid nicotine exposures among young children. Pediatrics. 2018;141(5):e20173361.
Kamboj A, Spiller HA, Casavant MJ, Chounthirath T, Smith GA. Pediatric exposure to E-cigarettes, nicotine, and tobacco products in the United States. Pediatrics. 2016;137(6):e20160041.
Patterson SB, Beckett AR, Lintner A, Leahey C, Greer A, Brevard SB, et al. A novel classification system for injuries after electronic cigarette explosions. J Burn Care Res. 2017;38(1):e95–e100.
Drehmer JE, Nabi-Burza E, Walters BH, et al. Parental smoking and E-Cigarette use in homes and cars. Pediatrics. 2019;143(4):e20183249.
Ballbè M, Martínez-Sánchez JM, Sureda X, Fu M, Pérez-Ortuño R, Pascual JA, et al. Cigarettes vs. e-cigarettes: Passive exposure at home measured by means of airborne marker and biomarkers. Environ Res. 2014;135:76–80.
Soule EK, Maloney SF, Spindle TR, Rudy AK, Hiler MM, Cobb CO. Electronic cigarette use and indoor air quality in a natural setting. Tob Control. 2017;26(1):109–12.
Ruprecht AA, De Marco C, Pozzi P, Munarini E, Mazza R, Angellotti G, et al. Comparison between particulate matter and ultrafine particle emission by electronic and normal cigarettes in real-life conditions. Tumori. 2014;100(1):e24–7.
Whittington JR, Simmons PM, Phillips AM, Gammill SK, Cen R, Magann EF, et al. The use of electronic cigarettes in pregnancy: a review of the literature. Obstet Gynecol Surv. 2018;73(9):544–9.
Spector LG, Murphy SE, Wickham KM, Lindgren B, Joseph AM. Prenatal tobacco exposure and cotinine in newborn dried blood spots. Pediatrics. 2014;133(6):e1632–8.
Gunnerbeck A, Edstedt Bonamy AK, Wikström AK, Granath F, Wickström R, Cnattingius S. Maternal snuff use and smoking and the risk of oral cleft malformations--a population-based cohort study. PLoS One. 2014;9(1):e84715.
Dahlin S, Gunnerbeck A, Wikström AK, Cnattingius S, Edstedt Bonamy AK. Maternal tobacco use and extremely premature birth - a population-based cohort study. BJOG. 2016;123(12):1938–46.
Baba S, Wikström AK, Stephansson O, Cnattingius S. Changes in snuff and smoking habits in Swedish pregnant women and risk for small for gestational age births. BJOG. 2013;120(4):456–62.
Bruin JE, Gerstein HC, Holloway AC. Long-term consequences of fetal and neonatal nicotine exposure: a critical review. Toxicol Sci. 2010;116(2):364–74.
Dhalwani NN, Szatkowski L, Coleman T, Fiaschi L, Tata LJ. Nicotine replacement therapy in pregnancy and major congenital anomalies in offspring. Pediatrics. 2015;135(5):859–67.
Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12):a012120.
Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122(2):125–39.
England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49(2):286–93.
Schraufnagel DE. Electronic Cigarettes: Vulnerability of Youth. Pediatr Allergy Immunol Pulmonol. 2015;28(1):2–6.
Pauly JR, Slotkin TA. Maternal tobacco smoking, nicotine replacement and neurobehavioural development. Acta Paediatr. 2008;97(10):1331–7.
Noël A, Hansen S, Zaman A, Perveen Z, Pinkston R, Hossain E, et al. In utero exposures to electronic-cigarette aerosols impair the Wnt signaling during mouse lung development. Am J Phys Lung Cell Mol Phys. 2020;318(4):L705–22.
McGrath-Morrow SA, Hayashi M, Aherrera A, Lopez A, Malinina A, Collaco JM, et al. The effects of electronic cigarette emissions on systemic cotinine levels, weight and postnatal lung growth in neonatal mice. PLoS One. 2015;10(2):e0118344.
Lauterstein DE, Tijerina PB, Corbett K, Akgol Oksuz B, Shen SS, Gordon T, et al. Frontal cortex transcriptome analysis of mice exposed to electronic cigarettes during early life stages. Int J Environ Res Public Health. 2016;13(4):417.
Usher K, Bhullar N, Jackson D. Life in the pandemic: social isolation and mental health. J Clin Nurs. 2020;29(15–16):2756–7.
Vanderbruggen N, Matthys F, Van Laere S, Zeeuws D, Santermans L, Van den Ameele S, et al. Self-Reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur Addict Res. 2020;26(6):309–15.
Gallus S, Stival C, Carreras G, Gorini G, Amerio A, McKee M, et al. Use of electronic cigarettes and heated tobacco products during the Covid-19 pandemic. Sci Rep. 2022;12(1):702.
Ramamurthi D, Chau C, Jackler RK. Exploitation of the COVID-19 pandemic by e-cigarette marketers. Tob Control. 2021;30(e1):e56–9.
Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67(4):519–23.
Chen DT-H, Kyriakos CN. Cigarette and E-cigarettes dual users, exclusive users and COVID-19: Findings from Four UK Birth Cohort Studies. Int J Environ Res Public Health. 2021;18(8):3935.
Sifat AE, Nozohouri S, Villalba H, Vaidya B, Abbruscato TJ. The Role of Smoking and Nicotine in the Transmission and Pathogenesis of COVID-19. J Pharmacol Exp Ther. 2020;375(3):498–509.
Maggi F, Rosellini A, Spezia PG, et al. Nicotine upregulates ACE2 expression and increases competence for SARS-CoV-2 in human pneumocytes. ERJ Open Res. 2021;7:00713–2020.
McAlinden KD, Lu W, Ferdowsi PV, Myers S, Markos J, Larby J, et al. Electronic cigarette aerosol is cytotoxic and increases ACE2 expression on human airway Epithelial cells: implications for SARS-CoV-2 (COVID-19). J Clin Med. 2021;10(5):1028.
Wang Q, Sundar IK, Li D, Lucas JH, Muthumalage T, McDonough SR, et al. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR α7 receptor: role of nAChR α7 in SARS-CoV-2 Covid-19 ACE2 receptor regulation. Respir Res. 2020;21(1):154.
Kaisar MA, Villalba H, Prasad S, Liles T, Sifat AE, Sajja RK, et al. Offsetting the impact of smoking and e-cigarette vaping on the cerebrovascular system and stroke injury: Is Metformin a viable countermeasure? Redox Biol. 2017;13:353–62.
McFadden DD, Bornstein SL, Vassallo R, Salonen BR, Bhuiyan MN, Schroeder DR, et al. Symptoms COVID 19 Positive Vapers Compared to COVID 19 Positive Non-vapers. J Prim Care Community Health. 2022;13:21501319211062672.
Kale D, Herbec A, Perski O, Jackson SE, Brown J, Shahab L. Associations between vaping and Covid-19: Cross-sectional findings from the HEBECO study. Drug Alcohol Depend. 2021;221:108590.
Miyara M, Tubach F, Pourcher V, Morelot-Panzini C, Pernet J, Haroche J. Low incidence of daily active tobacco smoking in patients with symptomatic COVID-19 [Internet]. Qeios [Preprint]. 2020. p. 13. Available from: https://doi.org/10.32388/WPP19W.3. [cited 2022 Apr 3].
Gonzalez-Rubio J, Navarro-Lopez C, Lopez-Najera E, et al. Cytokine Release Syndrome (CRS) and Nicotine in COVID-19 Patients: Trying to Calm the Storm. Front Immunol. 2020;11:1359.
Changeux JP, Amoura Z, Rey FA, Miyara M. A nicotinic hypothesis for Covid-19 with preventive and therapeutic implications. C R Biol. 2020;343(1):33–9.
Xiong Y, Liu Y, Cao L, Wang D, Guo M, Jiang A, et al. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg Microbes Infect. 2020;9(1):761–70.
Hassoun A, Brady K, Arefi R, Trifonova I, Tsirilakis K. Vaping-associated lung injury during COVID-19 multisystem inflammatory syndrome outbreak. J Emerg Med. 2021;60(4):524–30.
Callahan SJ, Harris D, Collingridge DS, et al. Diagnosing EVALI in the Time of COVID-19. Chest. 2020;158(5):2034–7.
Foust AM, Winant AJ, Chu WC, Das KM, Phillips GS, Lee EY. Pediatric SARS, H1N1, MERS, EVALI, and Now Coronavirus Disease (COVID-19) Pneumonia: What Radiologists Need to Know. AJR Am J Roentgenol. 2020;215(3):736–44.
Helfgott D, Capozzoli G, Madray J, Baig A, Uppaluri L, Gaur S, et al. E-cigarette or vaping product use associated lung injury (EVALI) in the time of COVID-19:a clinical dilemma. Pediatr Pulmonol. 2022;57(3):623–30.
Acknowledgements
N/A
Funding
N/A
Author information
Authors and Affiliations
Contributions
FV: conceptualization (supporting); investigation; writing – original draft preparation (lead). RN: conceptualization (lead); writing – review & editing (lead). SBD: writing – original draft preparation (supporting). LP: writing – review & editing (supporting). EM: Writing – Review & Editing (supporting). GDM: Writing – Review & Editing (supporting). LM: writing – review & editing (supporting). FM: supervision. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Virgili, F., Nenna, R., Ben David, S. et al. E-cigarettes and youth: an unresolved Public Health concern. Ital J Pediatr 48, 97 (2022). https://doi.org/10.1186/s13052-022-01286-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-022-01286-7