Abstract
Background
Newborns with congenital diaphragmatic hernia (CDH) and esophageal atresia (EA) might experience breastfeeding difficulties. The aim of this study was to detect the prevalence of breastfeeding in newborns with CDH and EA at different time points.
Methods
We performed an epidemiological study and retrospective survey on the prevalence of breastfeeding in CDH and EA affected newborns. We identified 40 CDH and 25 EA newborns who were fed through breastfeeding procedures according to WHO categorized definitions, and compared the breastfeeding procedures at the beginning of hospitalization and at three months of life.
Results
Although all the mothers attempted breastfeeding after birth, only 44 (67.7%) were still breastfeeding at the time of discharge. Exclusive breastfeeding was successful for only 19 (29%) mothers. The rate of exclusive breastfeeding at three months of life did not differ statistically from discharge and between the two groups of study.
Conclusion
A large percentage of mothers of children with CDH and EA who breastfed at the beginning of hospitalization did not continue at three months. It would be important to increase the breastfeeding rate in CDH and EA affected newborns by following specific steps for vulnerable infants and sustaining breastfeeding after discharge.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Breast milk (BM) represents the optimum nutrition for full term newborns, sick neonates and preterm infants, because it contains anti-infectious properties, immune modulators, growth hormones and all the nutrients needed for physiological growth [1, 2]. Several studies have correlated exclusive breastfeeding with a reduced incidence of respiratory and gastrointestinal infections, nosocomial infections, re-hospitalization rates, and metabolic syndrome [3,4,5]. The advantages are particularly relevant in neonates undergoing surgery. BM reduces the incidence of complications in newborns undergoing surgery for cardiac abnormalities, malformations of the nervous system, or other organs [6,7,8,9]. BM is particularly advantageous in vulnerable infants because it is well tolerated and absorbed, allowing faster full enteral intake, early parenteral nutrition suspension, and earlier central venous catheter removal [10]. The first choice is to offer raw and unpasteurized mother’s milk; when the mother’s milk is not available, donor human milk is the recommended alternative [11, 12].
Newborns undergoing surgery for congenital diaphragmatic hernia (CDH) and esophageal atresia (EA) might particularly benefit from BM, because they are vulnerable infants. CDH is a developmental abnormality in which the diaphragm fails to form properly during embryogenesis, and consequently abdominal viscera invade the thoracic cavity, inhibiting pulmonary growth. Despite advances in treatment, mortality and morbidity rates in CDH infants remain high [13]. Morbidities linked to CDH include pulmonary disorders, cardiovascular and gastro-intestinal diseases, failure to thrive, neurocognitive defects, and musculoskeletal abnormalities [14, 15]. Gastro-esophageal reflux disease (GERD) is also an important contributor to overall morbidity, and can be responsible for feeding problems and failure to thrive [16, 17]. It is conceivable that an enteral feeding with a suitable choice like the human milk can improve the fasting tolerance and reduce GERD in CDH infants.
EA is a congenital interruption of the continuity of the esophagus with or without a persistent communication with the trachea. In 86% of cases there is a distal tracheo-oesophageal fistula, in 7% there is no fistulous connection, while in 4% there is a tracheo-oesophageal fistula without atresia [18]. Survival rates are reported to be around 90% in patients with, and almost 100% in term infants without associated anomalies [19]. Early and late complications occur more often in infants treated for a long gap atresia, and include tracheomalacia and GERD. GERD can be associated with long term feeding difficulties such as long mealtimes, food refusal, coughing, choking, vomiting, and delayed introduction of solids [20].
Our hospital is tertiary care referral centers for CDH and EA, and in our experience these condition represent two of the major cause of difficult to starting and continuation of breastfeeding. Therefore, we carried out a study of epidemiology and surveyed mothers to assess the prevalence of breastfeeding in newborns with CDH and EA at different time points.
Methods
We performed a retrospective analysis of all infants who underwent surgery for CDH and EA from October 2011 through October 2014, and in January 2015 collected supplementary data after discharge by telephone interviews with the mothers of these previously hospitalized infants, at three months of life. The exclusion criteria were: need of surgical revision of EA, length of hospitalization over three months, and death before or immediately after surgical procedure. Most of the children had a prenatal diagnosis, and usually the birth of the child was planned. Children with CDH were electively intubated at birth and immediately transferred to our Neonatal Intensive Care Unit (NICU). When the vital parameters remained stable for 24 h, surgery was performed. Children with EA were not electively intubated, but they were also transferred immediately after birth to our NICU with a continuous suction in place, to reduce the incidence of pulmonary aspiration. Surgery was performed in the first days of life (first through fifth day of life).
Our Neonatal Intensive Unit (NICU) has dedicated staff to support breastfeeding: psychologists who support mothers through breastfeeding difficulties, and one International Board Certified Lactation Consultants (IBCLC) not present in the Neonatal Surgery Unit (NSU). Every year we organize a training course to improve staff knowledge about breastfeeding practices. We follow and sustain breastfeeding by the ten expanded steps of WHO [21].
To reduce bias linked with enrollment and disparity of outcome, we also registered the following data: age of the mother at birth, parity of the mother, neonatal clinical characteristics such as gender, weight and age at surgery, at first enteral feeding, at achievement of full enteral feeding, and at achievement of first oral feeding. Age at first enteral feeding was defined as the day of life on which either formula or human milk was first provided. Full enteral feeding was defined as an enteral feeding volume, either oral or gavage, of 150 ml/kg/day. First oral feeding was defined as the first day in which the infant had the entire feeding orally, without gavage. We recorded the different practices of breastfeeding (human milk, including the donor’s and the own mother’s milk), referring to the World Health Organization (WHO) definition: exclusive breastfeeding, predominant breastfeeding (breast milk and non-nutritional fluids), complementary/partial feeding (breast milk and artificial milk or other solid or semisolid nourishments) and bottle feeding [22, 23]. We found some mothers who attempted/ tried to breastfeeding, which means performed skin to skin practice, given breast to newborn, in order to stimulate sucking reflex under nursing advice and supervision. We analyzed each case at the time of discharge from the hospital and at 90 days of life. Survey questions administered to the mothers during phone interviews on the duration of breastfeeding and the type of feeding. The questionnaire is reported in Table 1. The same physician performed all the telephone interviews. We compared the rate of breastfeeding between the two groups of population in order to identify differences and predictable factors that may influence difficulties of breastfeeding.
Statistical analysis
Statistical analysis was carried out by using the Statistical Package for Social Sciences (SPSS Inc., Chicago, Ilinois, USA), version 13.0. Significance was defined as p < 0.05. We performed a comparison between CDH and EA population. The categorical variables were compared using χ2 Person and Fisher tests. The ordinal variables were compared using t-test and non-parametric test (test U di Mann –Whitney). Data are presented as mean +/− standard deviation (SD).
Results
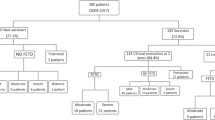
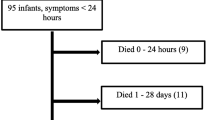
During the study period we admitted 64 newborns with CDH (47.6% males) and 36 newborns with EA (62.1% males). We excluded 10 newborns who underwent revision for EA, 5 infants hospitalized over three months, and 20 neonates who died before or immediately after surgery for CDH. We therefore enrolled 65 newborns (53.8% males), 40 (61.5%) with CDH and 25 (38.5%) with EA. All mothers completed the telephone survey.
Neonates with CDH
The main characteristics of the CDH children are presented in Tables 2 and 3. The mother’s age at birth ranged from 19 to 39 years, and 17 (42.5%) of them had had a previous pregnancy. Two mothers had pregnancy disorders (one hypertension, and one type 2 diabetes mellitus and hypertension). At time of discharge 13 (32.5%) infants were exclusively breastfed, 11 (27.5%) were taking complementary feeding, and 16 (40%) were taking artificial milk. At three months of life 12 infants (30%) were exclusively breastfed, 8 (20%) were having complementary feeding, and 20 (50%) were on artificial milk (Table 3). Enteral or oral feeding was started exclusively with human milk (either mother’s or donor’s milk) in 29 newborns (72.5%). Five neonates (12.5%) were breastfed from the start, 5 (12.5%) were fed with bottle, 7 (17.5%) were fed both ways, and in 23 neonates (57.5%) human milk was delivered through a naso-gastric tube. From questionnaire, we found that the principal cause of breastfeeding’s discontinuation at three months of life was the fear of lack of sufficient milk for the baby’s growth.
Neonates with EA
The main characteristics of the EA children are presented in Tables 2 and 3. The mother’s age at birth ranged from 21 to 40 years, and only one (4%) had had a previous pregnancy. One mother had type 2 diabetes mellitus. At time of discharge 6 (24%) infants were exclusively breastfed, 9 (36%) were taking complementary feeding and 10 (40%) were taking artificial milk (Table 4). At three months of life 3 (12%) infants were exclusively breastfed, 7 (28%) were taking complementary feeding, and 15 (60%) were taking artificial milk (Table 4). Enteral or oral feeding was started exclusively with human milk (either mother’s milk or donor’s milk) in 15 newborns (60%). Five neonates (20%) were breastfed from the start, 12 (48%) were fed with bottle, 7 (19,4%) were fed both ways and in in 12 neonates (48%) human milk was delivered through a naso-gastric tube. In contrast to CDH population, the principal reported cause of discontinuation of breastfeeding at three months of life was GERD.
Comparison between children with CDH and EA
Independently from the type of surgery, 44 mothers (67.7%) tried to breastfeed at discharge. No significant difference was found between neonates with CDH and EA in terms of types of feeding (exclusive breastfeeding, partial breastfeeding and artificial feeding). No significant correlation was found between rate of feeding with human milk and number of previous pregnancies, pregnancy risk factors, or mother’s age. Among children with CDH, a significant difference was found between children breastfed during the first week of hospitalization versus those exclusively breastfed at discharge, and those exclusively breastfed at three months of life: 29 newborns were breastfed at hospitalization. But only 13 continued exclusive breastfeeding at discharge (p = 0.02), and only 12 at 3 months of life (p = 0.001). Among children with EA there was no significant difference between children breastfed during hospitalization versus those exclusively breastfed at discharge or at three months of life (Table 4). In both populations neither weight nor the day at which the babies reached full enteral feeding influenced the rate of breastfeeding. No other variable studied was correlated with the rate of breastfeeding at discharge or at three months of life.
Discussion
Our results show that the rate of breast-feeding is low in CDH and EA newborns versus what it was in 2014 in the Lazio region, where our hospital is located (65.4% at discharge) (http://www.salute.gov.it/imgs/C_17_pubblicazioni_2256_allegato.pdf), but the rate of breastfeeding did not change significantly after hospital discharge.
BM is important for surgical infants, because it provides a barrier to potential illness, and could be beneficial during the newborn period and hospitalization. An epidemiologic study showed that human milk improves the outcome in newborns who undergo gastroschisis repair, with lower rate of positive blood cultures, lower percentage of days on inotropes, and shorter length of stay [24]. The relationship between human milk and CDH is not as extensively studied as for other vulnerable infants [25]. These infants have significant morbidities such as respiratory and gastrointestinal problems, that could benefit from receiving human milk [25]. Ideally, every mother should be encouraged to breastfeed within half an hour of birth. When infants are born with complications, lactation must be initiated using a breast pump, if possible within the first 6 h after birth. During the next days, many mothers of sick newborns can become discouraged because they cannot directly breastfeed their babies. In our Department, after surgery for CDH, neonates are intubated and given total parental nutrition for a time that depends on their clinical conditions. As soon as possible, after surgery the babies are extubated and transferred in the NSU. After surgery for EA, patients are often intubated and sedated for a period of time that depends on the distance between the proximal and distal esophagus. Postoperative elective paralysis is adopted to avoid tension on the esophageal anastomosis in long gaps. Enteral feeding via the trans-anastomotic tube is started around seven days, but before starting oral feeding we perform a routine contrast study. Parenteral nutrition is used in almost 50% of these patients. Once extubated, the babies are transferred to the NSU. For both conditions, breastfeeding or non-nutritive sucking at the breast should be initiated promptly once an infant has been extubated. Generally, healthy newborns learn to suck competently within a few days after birth. Feeding influences the mother’s sense of competence, and thus, mother–child relationship. Sucking and swallowing is a physiological process that the neonate develops in the presence of a normal oral motor function, functional esophagus and gastrointestinal system, independently of whether s/he is breast or bottle-fed. Because infants who undergo CDH surgery often cannot be breastfed for a long time, it might be important to implement the oral practice (stimulation of oral behavior) [26].In our experience to stimulate lactation and rise the mother’s milk supply, we often use the supplemental nursing system (SNS) filled with fresh pumped breast milk by infant suckling [27].
Despite the fact that CDH and EA have different treatment and peri-operative complications, we have evidenced that both have breastfeeding difficulties. Sixty-seven % of the mothers tried to breastfeed their baby after the surgery, but the percentage had declined at the time of discharge. Therefore despite the desire to breastfeed, some factors lead to frequent failure. One possible explanation is that these mothers are immediately separated from their child, delaying both mother-child relationship and the development of a correct rhythm of hunger and satiety, as well as the oral skills needed to competently suck [28]. Furthermore, these infants are subject to frequent oral procedures (aspirations, introduction of nasogastric tubes), possibly causing them to perceive as painful all sensations associated with oral functions. After discharge, the major limiting factor to breastfeeding was feeding difficulty related to GERD, as highlighted during the telephone survey. Indeed, complementary feeding was frequently a choice of the mothers because it allowed a change in the consistency of the milk. Indeed, in the EA population there was a significant decrease in the rate of breastfeeding both during hospitalization and after discharge. Accordingly, it has been highlighted that in this population, GERD and feeding difficulties lead to malnutrition [29, 30] To prepare a mother for breastfeeding at home, she should be afforded maximal opportunity to breastfeed her infant during hospitalization. The medical and nurse staff of the NICU should encourage mothers to spend as much time as possible at their infant’s bedside to learn their infant’s behaviors and feeding clues. For infants born with complex surgical anomalies, additional practice was proposed by Edwards and Spatz [31]. The Kangaroo mother care (KMC) should always be promoted, because the skin-skin contact might prolong and support breastfeeding [32]. Health caregivers should be educated about the benefits of offering as soon as possible to the neonate non-nutritive sucking, of reducing the time of enteral feeding and of transferring the baby as soon as possible to the NSU, giving the mother the possibility to restore a correct mother-child relationship [33]. Indeed, nurse participation and knowledge has been shown to improve the rate of breastfeeding in NICU [34].
Limitations of our study were a small population that reflects the low prevalence of above diseases and a lack of a healthy control group, due to the fact that our Department does not have a birth center. Despite these limitations, we present an important overview of the breastfeeding rate in a tertiary NICU specialized in two rare diseases (CDH and EA) during hospitalization and after discharge.
Conclusions
The percentage of exclusive breastfeeding and complementary feeding for children operated for EA and CDH is low both during hospitalization and after hospital discharge. These rates remain unchanged after three months of life. Children with EA are breastfed at lower frequency compared to those with CDH. The main barriers to breastfeeding are probably related to the surgery and the perioperative course. Our study shows that it is necessary to improve breastfeeding rates in neonates undergoing surgery for CDH and EA already during hospitalization. To our knowledge, this goal should be reached by following the steps proposed by Spatz, not always practiced [31, 34, 35]. A further benefit could be reached by following also the expansion of “The Baby-Friendly Hospital Initiative, Ten Steps” set down by WHO for the NICUs [11, 12, 21], were the babies are hospitalized following surgery. Adequate prenatal counseling, a dedicated room for breast pumping, KMC, training of nurses and doctors and IBCLC supervision should all be considered hospital standards. We also believe that it would be helpful to support breastfeeding after discharge, either with clinic visits and through telephone calls.
Abbreviations
- BF:
-
Breastfeeding
- BM:
-
Breast milk
- CDH:
-
Congenital Diaphragmatic Hernia
- EA:
-
Esophageal Atresia
- GERD:
-
Gastro-esophageal reflux disease
- HM:
-
Human Milk
- IBCLC:
-
International Board Certified Lactation Consultants
- KMC:
-
Kangaroo mother care
- NSU:
-
Neonatal Surgery Unit
- NSU:
-
Neonatal Surgical Unit
References
Menon G, Williams TC. Human milk for preterm infants: why, what, when and how? Arch Dis Child Fetal Neonatal Ed. 2013;98(6):F559–62.
Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 breastfeeding policy statement. Breastfeed Med. 2012;7(5):323–4.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118(1):e115–23.
Underwood MA. Human milk for the premature infant. Pediatr Clin N Am. 2013;60(1):189–207.
Singhal A, Cole TJ, Lucas A. Early nutrition in preterm infants and later blood pressure: two cohorts after randomised trials. Lancet. 2001;357(9254):413–9.
Medoff-Cooper B, Naim M, Torowicz D, Mott A. Feeding, growth, and nutrition in children with congenitally malformed hearts. Cardiol Young. 2010;20(Suppl 3):149–53.
Rosti L, Vivaldo T, Butera G, Chessa M, Carlucci C, Giamberti A. Postoperative nutrition of neonates undergoing heart surgery. Pediatr Med Chir. 2011;33(5–6):236–40.
Hamdan MA, Gaeta ML. Octreotide and low-fat breast milk in postoperative chylothorax. Ann Thorac Surg. 2004;77(6):2215–7.
De Coopman J. Breastfeeding after pituitary resection: support for a theory of autocrine control of milk supply? J Hum Lact. 1993;9(1):35–40.
Kohler JA Sr, Perkins AM, Bass WT. Human milk versus formula after gastroschisis repair: effects on time to full feeds and time to discharge. J Perinatol: official journal of the California Perinatal Association. 2013;33(8):627–30.
Panczuk J, Unger S, O'Connor D, Lee SK. Human donor milk for the vulnerable infant: a Canadian perspective. Int Breastfeed J. 2014;9:4.
Edwards TM, Spatz DL. Making the case for using donor human milk in vulnerable infants. Adv Neonatal Care. 2012;12(5):273–8. quiz 9-80
Shue EH, Miniati D, Lee H. Advances in prenatal diagnosis and treatment of congenital diaphragmatic hernia. Clin Perinatol. 2012;39(2):289–300.
Chiu PP, Ijsselstijn H. Morbidity and long-term follow-up in CDH patients. Eur J Pediat Surg. 2012;22(5):384–92.
Pennaforte T, Rakza T, Fily A, Mur S, Diouta L, Sfeir R, et al. The long-term follow-up of patients with a congenital diaphragmatic hernia: review of the literature. Arch Pediat. 2013;20(Suppl 1):S11–8.
Arena F, Romeo C, Baldari S, Arena S, Antonuccio P, Campenni A, et al. Gastrointestinal sequelae in survivors of congenital diaphragmatic hernia. Ped Int. 2008;50(1):76–80.
de Buys Roessingh AS, Dinh-Xuan AT. Congenital diaphragmatic hernia: current status and review of the literature. Eur J Pediatr. 2009;168(4):393–406.
Pedersen RN, Calzolari E, Husby S, Garne E, group EW. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child. 2012;97(3):227–32.
Koivusalo AI, Pakarinen MP, Rintala RJ. Modern outcomes of oesophageal atresia: single Centre experience over the last twenty years. J Pediatr Surg. 2013;48(2):297–303.
Ramsay M, Birnbaum R. Feeding difficulties in children with esophageal atresia: treatment by a multidisciplinary team. Dis Esophagus. 2013;26(4):410–2.
Nyqvist KH, Haggkvist AP, Hansen MN, Kylberg E, Frandsen AL, Maastrup R, et al. Expansion of the baby-friendly hospital initiative ten steps to successful breastfeeding into neonatal intensive care: expert group recommendations. J Hum Lact. 2013;29(3):300–9.
Practices IfAB. Indicators for Assessing Breastfeeding Practices. Report from an informal meeting WHO. Geneva; 11–12 June 1991.
WHO. Nutrition database system. In: Copenhagen; 1998.
Gulack BC, Laughon MM, Clark RH, Burgess T, Robinson S, Muhammad A, et al. Enteral feeding with human milk decreases time to discharge in infants following gastroschisis repair. J Pediatr. 2016;170:85–9.
Spatz D, Raphael L, Froh EB. Breastfeeding the infant with congenital diaphragmatic hernia post extracorporeal membrane oxygenation. Neonatal Netw. 2012;31(1):31–8.
Rodriguez NA, Meier PP, Groer MW, Zeller JM, Engstrom JL. Fogg L. a pilot study to determine the safety and feasibility of oropharyngeal administration of own mother's colostrum to extremely low-birth-weight infants. Adv Neonat Care. 2010;10(4):206–12.
Penny F, Judge M, Brownell E, McGrath JM. What is the evidence for use of a supplemental feeding tube device as an alternative supplemental feeding method for breastfed infants? Adv Neonat Care. 2018;18(1):31–7.
Lecoufle A. Esophageal atresia: oral behavior in the neonatal period. Arch Pediat. 2012;19(9):939–45.
Menzies J, Hughes J, Leach S, Belessis Y, Krishnan U. Prevalence of malnutrition and feeding difficulties in children with esophageal atresia. J Pediatr Gastroenterol Nutr. 2016
Krishnan U, Mousa H, Dall'Oglio L, Homaira N, Rosen R, Faure C, et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-Tracheoesophageal fistula. J Pediatr Gastroenterol Nutr. 2016;63(5):550–70.
Edwards TM, Spatz DL. An innovative model for achieving breast-feeding success in infants with complex surgical anomalies. J Perin Neonat Nurs. 2010;24(3):246–53. quiz 54-5
Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, Lieberman E, et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2016;137(1):1–16.
Sisk P, Quandt S, Parson N, Tucker J. Breast milk expression and maintenance in mothers of very low birth weight infants: supports and barriers. J Hum Lact. 2010;26(4):368–75.
Hallowell SG, Spatz DL, Hanlon AL, Rogowski JA, Lake ET. Characteristics of the NICU work environment associated with breastfeeding support. Adv Neonat Care. 2014;14(4):290–300.
Spatz DL. Ten steps for promoting and protecting breastfeeding for vulnerable infants. J Perinat Neonat Nurs. 2004;18(4):385–96.
Acknowledgments
We thank Prof. Roberto Salvatori, Johns Hopkins University, Baltimore, MD for editing the manuscript.
Availability of data and materials
Please contact author for data requests.
Author information
Authors and Affiliations
Contributions
GS collected data and wrote article; SF, participated in design of the study, collected data and wrote article; MM collected data; FP contributed to write the article; PB participated in design of the study and collected data; AD conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project proposal received ethical approval from the Hospital Ethics Committee.
Consent for publication
Written informed consent was obtained from the patients’ parents for publication of this study. A copy of the written consents is available for review by the Editor-in Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Salvatori, G., Foligno, S., Massoud, M. et al. The experience of breastfeeding infants affected by congenital diaphragmatic hernia or esophageal atresia. Ital J Pediatr 44, 75 (2018). https://doi.org/10.1186/s13052-018-0509-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-018-0509-6