Abstract
The syndrome of immune dysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) is a rare disorder caused by mutations in the FOXP3 gene. Diarrhea, diabetes and dermatitis are the hallmark of the disease, with a typical onset within the first months of life. We describe the case of a twelve-year old male affected by a very late-onset IPEX with intractable enteropathy, which markedly improved after starting Sirolimus as second-line treatment. This case suggests that IPEX should always be considered in the differential diagnosis of watery intractable diarrhea, despite its unusual onset.
Similar content being viewed by others
Correspondence
The syndrome of immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) is a rare disorder, characterized by diarrhea, type-1 diabetes mellitus (T1DM) and dermatitis with onset within the first months of life [1],[2]. Diarrhea is intractable and persists despite dietary exclusions and bowel rest, resulting in malabsorption and failure to thrive [3]; T1DM can precede or follow enteritis [4]-[6]; dermatitis is severe with eczematiform, ichthyosiform or psoriasiform aspects [7]-[10], other autoimmune diseases are often associated [11].
IPEX is caused by germ-line mutations in the FOXP3 gene, a key regulator of immune tolerance, located in the X-chromosome at Xp11.23-Xq13.3 [12]-[17]. It is critical for the function of CD4+CD25+ regulatory T-cells (TREG) and for the maintenance of peripheral immunologic tolerance [17],[18].
Findings
We describe a 12-year-old boy born at term from natural birth after an uncomplicated pregnancy from unrelated parents, referred to our hospital for severe enteritis started one month before with liquid mucus-haematic diarrhoea (height: 50th centile, weight: 10th centile, regularly vaccinated). No potentially triggering events have been reported, such as vaccinations, viral infections or changes in nutrition. In his past history he had recurring episodes of mild atopic dermatitis since the first year of life, a high level of total IgE (400 UI/L), and a constipated bowel (once every two/three days).
On admission, he was dehydrated (7% of weight loss). Blood tests revealed hypoproteinaemia and hypogammaglobulinemia (Table 1), so albumin was replaced.
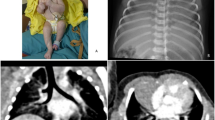
Abdominal ultrasound highlighted wall thickening of the bowel loops. Esophagogastroduodenoscopy (EGDS) and colonoscopy revealed ulcerative lesions at the stomach, duodenum, terminal ileum and colon, giving rise to a suspect of inflammatory bowel disease. Biopsies revealed villous blunting and inflammatory infiltration of the mucosa. After starting intravenous methylprednisolone, metronidazole and parenteral nutrition a partial remission was observed.
Ten days later, for a worsening of symptoms, EGDS and colonoscopy were repeated, with a superimposable picture. Particularly, the biopsies of the colon showed lympho-granulocytic acute inflammation with Graft versus Host Disease-like aspect, a lesion typically reported in IPEX (Figure 1) [30]. Due to the inability to control the symptoms the patient underwent ileostomy.
Despite the age of the patient was atypical for the onset of IPEX, we evaluated the presence of autoantibodies to harmonin, which resulted positive (>100 U.A.). Then, diagnosis was confirmed by the genetic examination of FOXP3 gene, revealing a mutation in the exon 9 (1040G > A), with substitution of Arginine to Histidine (R347H). The mother resulted negative. The total number of lymphocyte and lymphocyte subpopulations was normal, particularly TREG were 5% of the total number.
Intravenous cyclosporine (range: 200-350 mg/dl) and methylprednisolone (2 mg/kg) were started, which reduced diarrhea and abdominal pain. After sixty days of parenteral nutrition the patient returned to oral feeding with the normalization of albumin levels (Table 1). Because of the onset of post-prandial hyperglycaemias, we excluded T1DM (Table 1) and glycaemia normalized after tapering steroid therapy. For a new worsening of the disease we introduced sirolimus (0.15 mg/kg/day; range: 8-12 mg/dl). The patient improved with a progressive reduction of intensity and frequency of abdominal pain and mucus emission. A new colonoscopy highlighted a marked decrease of the inflammation. After thirty-four days since the beginning of sirolimus, cyclosporine was suspended. After twelve months the patient is well, without recurrence of the disease.
Conclusions
This case indicates that IPEX can have an atypical age of presentation. Thus, it should always be considered in the differential diagnosis of intractable diarrhea.
Four patients have been previously reported with IPEX with the same amino-acid substitution (R347H) found in our patient. The age of onset for all these subjects was within the first year of life and the first symptoms were recurrent ear infection, high IgE levels, T1DM, and gastritis. All had gastrointestinal symptoms with failure to thrive: two intractable diarrhea, two severe gastritis with mucosal atrophy or eosinophilic infiltration. Other symptoms were: coombs-negative haemolytic anaemia, food allergy, pancreatic exocrine failure, intractable hypertension, intestinal metaplasia, steatorrhea, and hypogammaglobulinemia. Patients received corticosteroid and calcineurin inhibitors. One patient died after allogeneic hematopoietic stem cell transplantation (HSCT) due to an infection.
Recently, evidence that patients with a severe form of IPEX may have circulating FOXP3+ T cells, as it is the case of our patient, which suggests that the cellular basis for the disease may be a result of a functional defect of Treg cells [1],[26]. Mainly, R347H mutated-FOXP3 has been demonstrated as effective as wild-type-FOXP3 in converting normal T cell into Treg in vitro [31] and in maintaining the ability to suppress the production of cytokines, hallmark of Treg cells, conferring suppressive capacity on CD4+ T cells.
In 2005, three patients were successfully treated with sirolimus [19]. Since then, 16 patients received sirolimus and nine are in complete or partial remission (Table 2). Considering that sirolimus seems to be as effective as the calcineurin inhibitors, with less toxic effects, it can be considered as a valid therapeutic option for bringing these patients to HSCT in their best clinical condition.
Consent
Written informed consent was obtained from the parents of the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethical approval
Internal ethical committee of Sant-Orsola approved the study.
Authors’ contributions
ZD and IC reviewed relevant articles on the literature, collected all the patient’s data and drew the manuscript. FS and PA contributed to the diagnosis and provided clinical assistance. RM, ML and AP contributed to the conception and design, and revisited critically the manuscript. EG carried out the molecular genetic studies and drafted the manuscript. All authors read and approved the final manuscript.
Abbreviations
- IPEX:
-
Syndrome of immune dysregulation, polyendocrinopathy, enteropathy, X linked
- T1DM:
-
Type-1 diabetes mellitus
- EGDS:
-
Esophagogastroduodenoscopy
- FKH:
-
Forkhead/winged helix domain
- mTOR:
-
Mammalian target of rapamycin
- HSCT:
-
Hematopoietic stem cell transplantation
References
Bacchetta R, Passerini L, Gambineri E, Dai M, Allan SE, Perroni L, Dagna-Bricarelli F, Sartirana C, Matthes-Martin S, Lawitschka A, Azzari C, Ziegler SF, Levings MK, Roncarolo MG: Defective regulatory and effector T cell functions in patients with FOXP3 mutations. J Clin Invest. 2006, 116: 1713-1722. 10.1172/JCI25112.
Wildin RS, Smyk-Pearson S, Filipovich AH: Clinical and molecular features of the immunodysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) syndrome. J Med Genet. 2002, 39: 537-545. 10.1136/jmg.39.8.537.
Vliet HJJ Van D, Nieuwenhuis EE: IPEX as a Result of Mutations in FOXP3. Clin Dev Immunol. 2007, 2007: 3-8.
Gambineri E, Perroni L, Passerini L, Bianchi L, Doglioni C: Clinical and molecular profile of a new series of patients with immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome: Inconsistent correlation between forkhead box protein 3 expression and disease severity. J Allergy Clin Immunol. 2008, 122: 1105-1113. 10.1016/j.jaci.2008.09.027.
Peake JE, McCrossin RB, Byrne G, Shepherd R: X-linked immune dysregulation, neonatal insulin dependent diabetes, and intractable diarrhoea. Arch Dis Child Fetal Neonatal Ed. 1996, 74: F195-F199. 10.1136/fn.74.3.F195.
Baud O, Goulet O, Canioni D, Le Deist F, Radford I, Rieu D, Dupuis-Girod S, Cerf-Bensussan N, Cavazzana-Calvo M, Brousse N, Fischer A, Casanova JL: Treatment of the immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) by allogeneic bone marrow transplantation. N Engl J Med. 2001, 344: 1758-1762. 10.1056/NEJM200106073442304.
Ruemmele FM, Moes N, de Serre NP-M, Rieux-Laucat F, Goulet O: Clinical and molecular aspects of autoimmune enteropathy and immune dysregulation, polyendocrinopathy autoimmune enteropathy X-linked syndrome. Curr Opin Gastroenterol. 2008, 24: 742-748. 10.1097/MOG.0b013e32830c9022.
Nieves DS, Phipps RP, Pollock SJ, Ochs HD, Zhu Q, Scott GA, Ryan CK, Kobayashi I, Rossi TM, Goldsmith LA: Dermatologic and immunologic findings in the immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome. Arch Dermatol. 2004, 140: 466-472. 10.1001/archderm.140.4.466.
De Benedetti F, Insalaco A, Diamanti A, Cortis E, Muratori F, Lamioni A, Carsetti R, Cusano R, De Vito R, Perroni L, Gambarara M, Castro M, Bottazzo GF, Ugazio AG: Mechanistic associations of a mild phenotype of immunodysregulation, polyendocrinopathy, enteropathy, x-linked syndrome. Clin Gastroenterol Hepatol. 2006, 4: 653-659. 10.1016/j.cgh.2005.12.014.
Halabi-Tawil M, Ruemmele FM, Fraitag S, Rieux-Laucat F, Neven B, Brousse N, De Prost Y, Fischer A, Goulet O, Bodemer C: Cutaneous manifestations of immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome. Br J Dermatol. 2009, 160: 645-651. 10.1111/j.1365-2133.2008.08835.x.
Torgerson TR: Regulatory T cells in human autoimmune diseases. Springer Semin Immunopathol. 2006, 28: 63-76. 10.1007/s00281-006-0041-4.
Bennett CL, Christie J, Ramsdell F, Brunkow ME, Ferguson PJ, Whitesell L, Kelly TE, Saulsbury FT, Chance PF, Ochs HD: The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet. 2001, 27: 20-21. 10.1038/83713.
Wildin RS, Ramsdell F, Peake J, Faravelli F, Casanova JL, Buist N, Levy-Lahad E, Mazzella M, Goulet O, Perroni L, Bricarelli FD, Byrne G, McEuen M, Proll S, Appleby M, Brunkow ME: X-linked neonatal diabetes mellitus, enteropathy and endocrinopathy syndrome is the human equivalent of mouse scurfy. Nat Genet. 2001, 27: 18-20. 10.1038/83707.
Chatila TA, Blaeser F, Ho N, Lederman HM, Voulgaropoulos C, Helms C, Bowcock AM: JM2, encoding a fork head-related protein, is mutated in X-linked autoimmunity-allergic disregulation syndrome. J Clin Invest. 2000, 106: R75-R81. 10.1172/JCI11679.
Marson A, Kretschmer K, Frampton GM, Jacobsen ES, Polansky JK, MacIsaac KD, Levine SS, Fraenkel E, von Boehmer H, Young RA: Foxp3 occupancy and regulation of key target genes during T-cell stimulation. Nature. 2007, 445: 931-935. 10.1038/nature05478.
Zheng Y, Josefowicz SZ, Kas A, Chu T-T, Gavin MA, Rudensky AY: Genome-wide analysis of Foxp3 target genes in developing and mature regulatory T cells. Nature. 2007, 445: 936-940. 10.1038/nature05563.
Wu Y, Borde M, Heissmeyer V, Feuerer M, Lapan AD, Stroud JC, Bates DL, Guo L, Han A, Ziegler SF, Mathis D, Benoist C, Chen L, Rao A: FOXP3 controls regulatory T cell function through cooperation with NFAT. Cell. 2006, 126: 375-387. 10.1016/j.cell.2006.05.042.
Bettelli E, Dastrange M, Oukka M: Foxp3 interacts with nuclear factor of activated T cells and NF-kappa B to repress cytokine gene expression and effector functions of T helper cells. Proc Natl Acad Sci U S A. 2005, 102: 5138-5143. 10.1073/pnas.0501675102.
Bindl L, Torgerson T, Perroni L, Youssef N, Ochs HD, Goulet O, Ruemmele FM: Successful use of the new immune-suppressor sirolimus in IPEX (immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome). J Pediatr. 2005, 147: 256-259. 10.1016/j.jpeds.2005.04.017.
Yong PL, Russo P, Sullivan KE: Use of sirolimus in IPEX and IPEX-like children. J Clin Immunol. 2008, 28 (5): 581-587. 10.1007/s10875-008-9196-1.
Heltzer ML, Choi JK, Ochs HD, Sullivan KE, Torgerson TR, Ernst LM: A potential screening tool for IPEX syndrome. Pediatr Dev Pathol. 2007, 10 (2): 98-105. 10.2350/06-07-0130.1.
Torgerson TR, Linane A, Moes N, Anover S, Mateo V, Rieux-Laucat F, Hermine O, Vijay S, Gambineri E, Cerf-Bensussan N, Fischer A, Ochs HD, Goulet O, Ruemmele FM: Severe food allergy as a variant of IPEX syndrome caused by a deletion in a noncoding region of the FOXP3 gene. Gastroenterology. 2007, 132: 1705-1717. 10.1053/j.gastro.2007.02.044.
Moes N, Rieux-Laucat F, Begue B, Verdier J, Neven B, Patey N, Torgerson TT, Picard C, Stolzenberg M-C, Ruemmele C, Rings EH, Casanova J-L, Piloquet H, Biver A, Breton A, Ochs HD, Hermine O, Fischer A, Goulet O, Cerf-Bensussan N, Ruemmele FM: Reduced expression of FOXP3 and regulatory T-cell function in severe forms of early-onset autoimmune enteropathy. Gastroenterology. 2010, 139: 770-778. 10.1053/j.gastro.2010.06.006.
Hennezel E, Bin DK, Torgerson T, Piccirillo C: The immunogenetics of immune dysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) syndrome. J Med Genet. 2012, 49: 291-302. 10.1136/jmedgenet-2012-100759.
Taddio A, Faleschini E, Valencic E, Granzotto M, Tommasini A, Lepore L, Andolina M, Barbi E, Ventura A: Medium-term survival without haematopoietic stem cell transplantation in a case of IPEX: insights into nutritionaland immunosuppressive therapy. Eur J Pediatr. 2007, 166 (11): 1195-1197. 10.1007/s00431-006-0395-6.
d’Hennezel E, Ben-Shoshan M, Ochs HD, Torgerson TR, Russell LJ, Lejtenyi C, Noya FJ, Jabado N, Mazer B, Piccirillo CA: FOXP3 forkhead domain mutation and regulatory T cells in the IPEX syndrome. N Engl J Med. 2009, 361: 1710-1713. 10.1056/NEJMc0907093.
Dorsey MJ, Petrovic A, Morrow MR, Dishaw LJ, Sleasman JW: FOXP3 expression following bone marrow transplantation for IPEX syndrome after reduced-intensity conditioning. Immunol Res. 2009, 44: 179-184. 10.1007/s12026-009-8112-y.
Rubio-Cabezas O, Minton JAL, Caswell R, Shield JP, Deiss D, Sumnik Z, Cayssials A, Herr M, Loew A, Lewis V, Ellard S, Hattersley AT: Clinical heterogeneity in patients with FOXP3 mutations presenting with permanent neonatal diabetes. Diabetes Care. 2009, 32: 111-116. 10.2337/dc08-1188.
Lucas KG, Ungar D, Comito M, Groh B: Epstein Barr virus induced lymphoma in a child with IPEX syndrome. Pediatr Blood Cancer. 2008, 50: 1056-1057. 10.1002/pbc.21341.
Patey-Mariaud de Serre N, Canioni D, Ganousse S, Rieux-Laucat F, Goulet O, Ruemmele F, Brousse N: Digestive histopathological presentation of IPEX syndrome. Mod Pathol. 2009, 22: 95-102. 10.1038/modpathol.2008.161.
McMurchy AN, Gillies J, Allan SE, Passerini L, Gambineri E, Roncarolo MG, Bacchetta R, Levings MK: Point mutants of forkhead box P3 that cause immune dysregulation, polyendocrinopathy, enteropathy, X-linked have diverse abilities to reprogram T cells into regulatory T cells. J Allergy Clin Immunol. 2010, 126: 1242-1251. 10.1016/j.jaci.2010.09.001.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Zama, D., Cocchi, I., Masetti, R. et al. Late-onset of immunodysregulation, polyendocrinopathy, enteropathy, x-linked syndrome (IPEX) with intractable diarrhea. Ital J Pediatr 40, 68 (2014). https://doi.org/10.1186/s13052-014-0068-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-014-0068-4