Abstract
Background
Resuscitative thoracotomy (RT) is an intervention that can be performed in the prehospital setting for relieving cardiac tamponade and/or obtaining vascular control of suspected sub-diaphragmatic haemorrhage in patients in traumatic cardiac arrest. The aim of this retrospective case study is to compare the rates of return of spontaneous circulation (ROSC) in RTs performed for both penetrating and blunt trauma over 6 years in a mixed urban and rural environment.
Methods
The electronic records of a single helicopter emergency medical service were reviewed between 1st June 2015 and 31st May 2021 for RTs. Anonymised data including demographics were extracted for relevant cases. Data were analysed with independent t-tests and Χ2 tests. A p value < 0.05 was considered statistically significant.
Results
Forty-four RTs were preformed within the 6 years (26 for blunt trauma). Eleven ROSCs were achieved (nine blunt, two penetrating) but no patient survived to discharge. In contrast to RTs for penetrating trauma, twelve of the RTs for blunt trauma had a cardiac output present on arrival of the prehospital team (p = 0.01). Two patients had an RT performed in a helicopter (one ROSC) and two on a helipad (both achieving ROSC), likely due to the longer transfer times seen in a more rural setting. Four of the RTs for blunt trauma (15%) were found to have a cardiac tamponade versus seven (39%) of the penetrating trauma RTs.
Conclusion
Prehospital RT remains a procedure with low rates of survival but may facilitate a ROSC to allow patients to reach hospital and surgery, particularly when distances to hospitals are greater. A higher-than-expected rate of cardiac tamponade was seen in RTs for blunt trauma, although not caused by a right ventricular wound but instead due to underlying vessel damage.
Similar content being viewed by others
Background
The East of England Ambulance Service Trust (EEAST) serves a population of approximately 6.2 million people in a mixed urban and rural environment covering an area of approximately 19,114 square kilometres [1]. Within EEAST, three services operate a helicopter emergency medical (HEM) service from five bases around the region, with a physician/paramedic model, including Essex and Herts Air Ambulance Trust (EHAAT) (Fig. 1). EHAAT has operated for a full 24 h since 7th October 2019 (only by car at night). HEMs teams are dispatched when predetermined criteria are satisfied (immediate dispatch), following ‘999’ call interrogation by a critical care paramedic or at the request of the attending medical/paramedical team on-scene. Immediate dispatch criteria includes traumatic cardiac arrest. In addition to serving the East of England population, EHAAT will provide mutual aid for neighbouring ambulance services if requested. EHAAT can provide emergency prehospital Resuscitative Thoracotomy (RT) as an intervention to clinically indicated patients. A Standard Operating Procedure (SOP) exists for this, including indications and timings by which clinicians will operate (see Additional file 2: Appendix 2). All EHAAT clinicians are required to partake in regular training relating to this SOP, including simulation, to ensure maintenance of standards, as it is recognised that, whilst RT is infrequent, clinical skills and decision making must be optimal.
The ability for EHAAT to administer prehospital blood products alongside a RT was introduced in 2019 [2]. The introduction of prehospital blood products has allowed a greater possibility for Trauma Unit (TU) bypass and longer onward transfer to Major Trauma Centre (MTC), where specialist services such as cardiothoracic and vascular surgery is available, as patients can be temporarily stabilised on route to hospital.
In general, RT is considered for patients who have suffered penetrating chest trauma with a view to accessing the chest cavity, relieving a cardiac tamponade, and repair of cardiac injuries [3, 4]. London’s Air Ambulance have shown an 18% survival to hospital discharge following RT for penetrating trauma, with 11 patients out of 13 (85%) having a good neurological outcome [5]. Other studies have struggled to replicate these findings [6]. However, RT can also be used in a select cohort of blunt trauma patients with a view to provide thoracic aortic compression (to allow attempt of haemorrhage control below the diaphragm) and/or repair of clinically presumed organ injury within the chest cavity [3, 4, 7]. Whilst evidence for appropriateness and patient survival from prehospital blunt trauma RT is limited there are an increasing number of publications, incorporating both case studies and case series, showing survivors from the procedure both in the prehospital and hospital emergency department environments [8,9,10,11,12]. One case study reports a neurological intact survivor of a prehospital RT following blunt trauma [11]. In 2016, EHAAT published a case series from April 2010 to April 2016 questioning whether RT for blunt trauma was justified as the evidence and indications remained unclear [13]. However, more recently the European Resuscitation Council has included RT in its 2021 guidelines as an option in traumatic cardiac arrest for both relieving tamponade and obtaining vascular control of sub-diaphragmatic bleeding via manual aortic compression [14].
The aim of this retrospective observational case series is therefore to compare RTs performed for both penetrating and blunt trauma between June 2015 and June 2021 in a mixed urban and rural area to understand more about indications and outcomes.
Methods
The computerised records (HEMSbase2.0) of a single HEM service (Essex and Herts Air Ambulance Trust) was interrogated to retrospectively extract anonymised data relating to resuscitative thoracotomies performed between 1st June 2015 and 31st May 2021 inclusive. Data relating to case demographics, time of dispatch, aetiology, presence of cardiac output on the arrival of the first emergency medical responders and the HEM service and outcomes were extracted. In addition, information relating to the likely cause of death based on findings at RT or at post-mortem were recorded. Local research policies were consulted; ethical approval was not required [15].
Prehospital administration of blood products became available to the HEM service in 2019 [2]. This consists of three units of Packed Red Blood Cells (PRCs) (reduced to two units from 2020 due to supply issues in the pandemic) and four units of Lyolysed Plasma (LyoPlas™). The use of blood products on scene following its introduction was therefore analysed versus prior to its introduction.
Data was analysed using Microsoft Excel and SPSS statistics (version 26). A Shapiro–Wilk test was performed for normality on continuous values. Mean or median values were calculated as appropriate. Independent t-tests and Χ2 tests were calculated to allow comparison between thoracotomies performed for penetrating and blunt trauma. A p value < 0.05 was considered statistically significant. The STROBE checklist was followed [16].
Results
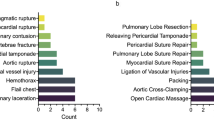
A total of 44 thoracotomies were performed between 1st June 2015 and 31st May 2021, an average of 7.3 per year, including two paediatric thoracotomies and three for patients over the age of 65. 26 were for blunt trauma and 18 were for penetrating. Sadly, there were no survivors to hospital discharge, but 11 patients did achieve return of spontaneous circulation (ROSC) following the thoracotomy. The average time from 999 to HEMS team arrival was 29.9 min. Table 1 shows a summary of the cases attended and Table 2 shows a comparison between the RTs performed for blunt and penetrating trauma. Further details surrounding the cases attended are available in Additional file 1: Appendix 1.
Prior to the introduction of prehospital blood products, 12/29 to whom RTs were performed received blood products in a hospital setting of which 6 achieved ROSC. Since the introduction of prehospital blood products in March 2019, EHAAT performed 15 RTs with blood products being administered to 11 of these patients. Of these 11 patients, 5 were penetrating injury and 6 were blunt injury, with no ROSCs achieved. Only one of the eleven patients (9%) was transported to hospital, the remainder were pronounced life extinct on scene versus 13/29 (44.8%) prior to the introduction of blood.
The distribution of timings for the 999 call is shown below (Fig. 2).
Discussion
This single UK mixed urban and rural HEM service performed a total of 44 RTs over 6 years, with 58% being for blunt trauma. In total 11 patients achieved ROSC but sadly there were no survivors to hospital discharge. Of note, four out of the 26 RTs for blunt trauma were found to have a cardiac tamponade, of which three achieved at least a brief ROSC, and nine out of the 26 achieved a ROSC.
The lack of survivors to hospital discharge from this cohort of patients differs from the findings of London’s Air Ambulance 20 years ago but is not dissimilar to other services abroad [5, 17]. The survival after an RT in the emergency department is estimated at 7.4%; this dropped to 1.4% for blunt RTs [18]. Our findings may therefore be influenced by the higher percentage of RTs for blunt trauma and longer run times to incidents and MTCs. Table One (and Table S1 Additional file 1: Appendix 1) details the extensive distance and travel times (by road only) to the nearest MTC for many of the patients, with a mean distance of 47.5 km (range 3.7–105.6 km) and mean time of 49.7 min (range 19–83 min). Whilst it is possible to transport a patient to whom an RT has been performed in an aircraft and thus reduce the transport time to an MTC, there would be significant difficulties in loading and unloading of these patients and a high possibility of deleterious effects to patient management and care. This is further complicated by the fact that several of the MTC helipads that EHAAT utilise when flying a patient require a secondary transfer by ambulance. For London’s Air Ambulance, the mean time to scene in a RT group was 9.29 min versus in this study at least 29.9 min from 999 to arrival on scene of the HEM service [19]. It has been suggested that RTs need to be performed within 30 min of the injury to have a better chance of survival, and these distances and times make this challenging despite rapid dispatch of the HEM service [20]. There does however appear to be a learning curve and it may be that if numbers increase that long term survivors may be seen [21]. It is also encouraging that, despite the distances to hospital and longer run times to incidents, patients are gaining a ROSC and therefore access to surgery to give them the chance of survival, suggesting that it is worth performing.
When looking at the indications for RT, in the blunt cohort there was a statistically significant increased percentage who had cardiac output (i.e. a central pulse) on arrival of the HEM service (46%) who then went on to require a RT versus penetrating trauma where the vast majority (89%) did not have a cardiac output on arrival of the HEM service. This fits with the suggestion in the literature that an RT should only be performed in patients with blunt thoracic trauma if they have received less than 5 min of CPR, as anything beyond this is considered futile [3, 22]. For in-hospital RTs performed for abdominal exsanguination a review suggests a 0–16% survival rate, which may be slightly higher if it is an isolated iliac injury [9]. However, blunt trauma does appear to have worse outcomes than penetrating [9]. For a prehospital London cohort, 25 patients (47.1%) had no signs of life on arrival of the team, with only one of these 25 patients surviving [19]. Performing a RT when there are signs of life on arrival (for example palpable pulses or respiratory effort) of the first crew is likely to be more successful (9/10 survivors in the London cohort had signs of life on arrival of the crew), although the London data is skewed towards penetrating trauma [19]. The findings of this study therefore appears to support that a blunt RT should only be performed on patients with signs of life on the first emergency responder arrival, or perhaps even the HEMS team arrival, with then witnessed loss of central pulses, as these patients are most likely to be the survivors [19]. Currently, ultrasound to look for cardiac tamponade is not part of the SOP for RT in our service and this too may be something that should be included in the future.
Whilst the vast majority of both penetrating and blunt RTs occurred on scene, two were performed in a helicopter and two on a helipad. ROSC was achieved in three of them. To our knowledge this has not been previously described in the literature. It is important to note that there were no unexpected complications and no needlestick or similar injuries for clinical staff in any of the RTs, including the ones performed in the helicopter or on a helipad. This suggests that whilst this may not be ideal, it is possible to perform RTs in this setting. One study has shown that rapid sequence induction can be performed in a helicopter cabin [23]. In environments where distances to hospital deem aircraft carries necessary, training for in-flight thoracotomies could be considered. The newer airframes being utilised by air ambulances in the UK, with larger cabin space and 360° access to the patient, would potentially make this procedure viable; however, this requires further research and cannot yet be recommended.
It is interesting to note that, in one of the penetrating patients the indication for RT was for aortic control and not to exclude tamponade as the injury was to the femoral artery (see case 21, Table 1, Additional file 1: Appendix 1). In contrast 69% of thoracotomies performed for blunt trauma were performed with an aim of achieving some element of aortic control for sub-diaphragmatic haemorrhage. This suggests that there may be value in exploring the benefits of endovascular resuscitation techniques, such as REBOA in a mixed urban and rural setting. Despite clinicians initially intending to perform the RT for aortic control of sub-diaphragmatic haemorrhage, 15% (4/26) of the blunt RTs were shown to have a cardiac tamponade, higher than may be expected in blunt trauma patients. However, unlike case reports of survivors of blunt cardiac tamponade normally secondary to right ventricular injuries, none of the cases reported here were found to have a right ventricular injury [24]. Three patients were found to have vessel damage (either the left anterior descending coronary artery or the aortic root) and for one patient it was unclear but no ventricular damage could be found. These underlying mechanisms of the tamponade are likely to be much more technically difficult to repair than a single ventricular wound, but relief of the tamponade may facilitate a timely transfer to hospital for further surgery, as was shown for several of the patients in this case series.
Overall, the injuries for both groups identified at RT or post-mortem show similar patterns to previous studies [25]. Survivors do tend to be seen in patients with a single right ventricle wound rather than more complex injury patterns, another reason for the lack of survivors seen in this case series [5, 25]. In addition, there are some patients described in this cohort that had additional injuries, particularly head injuries; it can be difficult on scene to determine the exact cause of cardiac arrest and an RT is performed as an intervention to exclude a “potentially treatable” cause of cardiac arrest, such as a cardiac injury. Other prehospital services can offer techniques such as REBOA for abdominal or pelvic haemorrhage and it may be that, as this becomes more widespread, this current indication for thoracotomies, particularly in blunt trauma, decreases and survival rate increases [26]. However, as studies have shown, RT is still valid for attempting to slow or cease abdominal exsanguination through aortic compression [9].
The mean age of the patients seen in this study were 42.3 years for RT in blunt trauma and 35.9 years for RT in penetrating trauma, with three patients having a RT aged over 65. This is a similar average age seen in other studies [19, 22, 25]. It is recognised that an age over 60 is an independent predictor of mortality [19, 22]. The gender distribution also remains consistent with other studies [22].
Following the prehospital administration of blood products, fewer patients were transported to hospital, with the majority pronounced life extinct on scene. This may be because now all the most significant interventions can be offered on scene without the need to transfer the patient. Of the 6 RTs performed for blunt trauma, the primary reasons for RT as detailed in the notes were: chest injury (4/6), aortic control (of sub-diaphragmatic haemorrhage) (1/6) and chest injury and aortic control (of sub-diaphragmatic haemorrhage) (1/6). The data appears to confirm that the introduction of blood products to the service did not encourage excessive RTs in blunt trauma patients and that the primary reason for performing RT was based on clinical assessment of a potentially treatable internal chest injury with no change in the average number of RTs per year.
Limitations
This study is a single centre cohort study. However, it does show a cohort based in a rural and urban environment, a different environment to many previous studies that are purely urban in nature. In the future, it would be interesting to combine findings with other HEM services operating in a similar setting. The likely cause of death is based on a combination of post-mortem results and findings at RT so may not be fully accurate. However, without post-mortem reports on every patient it is unlikely that a better insight than this will be gained. This may be an area to explore for the service in the future as improved post-mortem reporting and recording will allow a comparison of presumed versus actual injury loads to validate if the service is selecting the correct subset of patients for RT.
Conclusion
Prehospital RTs remains a procedure with low rates of survival but in areas where there are longer transfer times to hospitals patients are given the optimal chance of survival by the procedure being performed prehospital. As such, no difference in survival nor ROSC was seen between RTs performed for blunt and penetrating trauma in this case series. Cardiac tamponade can occur in blunt trauma patients, but this study shows that the cause is less likely to be a right ventricular wound but instead be due to underlying vessel damage.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Statista. Annual population growth in the United Kingdom in 2020 by region. 2021. https://www.statista.com/statistics/294681/population-england-united-kingdom-uk-regional/. Accessed 30 July 2021.
Essex and Herts Air Ambulance. Essex & Herts Air Ambulance to carry blood supplies. 2019. https://www.ehaat.org/press_release/essex-herts-air-ambulance-to-carry-blood-supplies/. Accessed 30 July 2021.
Morgan BS, Garner JP. Emergency thoracotomy-the indications, contraindications and evidence. J R Army Med Corps. 2009;155:87–93.
Aseni P, Rizzetto F, Grande AM, Bini R, Sammartano F, Vezzulli F, et al. Emergency department resuscitative thoracotomy: indications, surgical procedure and outcome. A narrative review. Am J Surg. 2021;221:1082–92.
Davies GE, Lockey DJ. Thirteen survivors of prehospital thoracotomy for penetrating trauma: a prehospital physician-performed resuscitation procedure that can yield good results. J Trauma. 2011;70:E75–8.
Nevins EJ, Moori PL, Smith-Williams J, Bird NTE, Taylor JV, Misra N. Should pre-hospital resuscitative thoracotomy be reserved only for penetrating chest trauma? Eur J Trauma Emerg Surg. 2018;44:811–8.
Lockey D, Crewdson K, Davies G. Traumatic cardiac arrest: Who are the survivors? Ann Emerg Med. 2006;48:240–4.
Schober P, de Leeuw MA, Terra M, Loer SA, Schwarte LA. Emergency clamshell thoracotomy in blunt trauma resuscitation: shelling the paradigm-2 cases and review of the literature. Clin Case Rep. 2018;6:1521–4.
Hughes M, Perkins Z. Outcomes following resuscitative thoracotomy for abdominal exsanguination, a systematic review. Scand J Trauma Resusc Emerg Med. 2020;28:9.
Narvestad JK, Meskinfamfard M, Søreide K. Emergency resuscitative thoracotomy performed in European civilian trauma patients with blunt or penetrating injuries: a systematic review. Eur J Trauma Emerg Surg. 2016;42:677–85.
Rogerson T, Efstratiades T, Von Oppell U, Davies G, Curtin R. Survival after pre-hospital emergency clamshell thoracotomy for blunt cardiac rupture. Injury. 2020;51:122–3.
Lu LH, Choi WM, Wu HR, Liu HC, Chiu WT, Tsai SH. Blunt cardiac rupture with prehospital pulseless electrical activity: a rare successful experience. J Trauma. 2005;59:1489–91.
Forsyth A, Ley E, Phillipson L, Sadek S. Pre-hospital thoracotomy in blunt trauma: Is it justified? Presented at BASICS and the faculty of pre-hospital care annual conference. 2017.
Lott C, Truhlář A, Alfonzo A, Barelli A, González-Salvado V, Hinkelbein J, et al. European resuscitation council guidelines 2021: Cardiac arrest in special circumstances. Resuscitation. 2021;161:152–219.
Health Research Authority. Is my study research? Medical research council. 2021. http://www.hra-decisiontools.org.uk/research/result7.html. Accessed 30 June 2021.
von Elm E, Altman DG, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–4.
Van Vledder MG, Van Waes OJF, Kooij FO, Peters JH, Van Lieshout EMM, Verhofstad MHJ. Out of hospital thoracotomy for cardiac arrest after penetrating thoracic trauma. Injury. 2017;48:1865–9.
Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190:288–98.
Athanasiou T, Krasopoulos G, Nambiar P, Coats T, Petrou M, Magee P, et al. Emergency thoracotomy in the pre-hospital setting: a procedure requiring clarification. Eur J Cardiothorac Surg. 2004;26:377–86.
Frezza EE, Mezghebe H. Is 30 minutes the golden period to perform emergency room thoratomy (ERT) in penetrating chest injuries? J Cardiovasc Surg (Torino). 1999;40:147–51.
van Waes OJF, Leemeyer AR, Kooij FO, Hoogerwerf N, van Vledder MG. Evaluation of out of hospital thoracotomy for cardiac arrest after penetrating thoracic trauma; three years after our first report. Injury. 2019;50:2136–7.
Panossian VS, Nederpelt CJ, El Hechi MW, Chang DC, Mendoza AE, Saillant NN, et al. Emergency resuscitative thoracotomy: a nationwide analysis of outcomes and predictors of futility. J Surg Res. 2020;255:486–94.
McHenry AS, Curtis L, Ter Avest E, Russell MQ, Halls AV, Mitchinson S, et al. Feasibility of prehospital rapid sequence intubation in the cabin of an AW169 helicopter. Air Med J. 2020;39:468–72.
Weber C, Farrah J, Garcia A, Ang D. A first report: two cases of survival and full recovery after blunt cardiac rupture requiring emergency department thoracotomy. Am Surg. 2020;86:538–40.
Coats TJ, Keogh S, Clark H, Neal M. Prehospital resuscitative thoracotomy for cardiac arrest after penetrating trauma: rationale and case series. J Trauma. 2001;50:670–3.
Sadek S, Lockey DJ, Lendrum RA, Perkins Z, Price J, Davies GE. Resuscitative endovascular balloon occlusion of the aorta (REBOA) in the pre-hospital setting: an additional resuscitation option for uncontrolled catastrophic haemorrhage. Resuscitation. 2016;107:135–8.
Funding
There was no funding for this project.
Author information
Authors and Affiliations
Contributions
PA provided the idea for this manuscript and led data collection and authorship of the manuscript. SM was a major contributor in the writing of the manuscript and performed the statistical analysis. MOM contributed to writing the manuscript. ND contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No consent or ethical approval required. Local research guidelines followed.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table S1: A Detailed Description of Cases Attended.
Additional file 2.
EHAAT's Pre-hospital Standard Operating Procedure Resuscitative Thoracotomy: March 2021.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Almond, P., Morton, S., OMeara, M. et al. A 6-year case series of resuscitative thoracotomies performed by a helicopter emergency medical service in a mixed urban and rural area with a comparison of blunt versus penetrating trauma. Scand J Trauma Resusc Emerg Med 30, 8 (2022). https://doi.org/10.1186/s13049-022-00997-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-022-00997-4