Abstract
Background
Charcot neuroarthropathy (Charcot foot) is a serious limb-threatening complication most commonly seen in individuals with diabetic peripheral neuropathy. Although dermal thermometry is widely used by clinicians to assist in the diagnosis, monitoring, and management of the disease, there is limited high-quality evidence to support its reliability. Therefore, this study investigated the intra-rater and inter-rater reliability of infrared dermal thermometry in patients with Charcot neuroarthropathy.
Methods
We collected clinical, demographic, health status, and foot examination information on 32 adults with Charcot neuroarthropathy from a metropolitan high-risk foot service in Melbourne, Australia. Infrared dermal thermometry assessments were conducted by two independent raters at 10 anatomical sites of the Charcot foot using both a (i) touch and (ii) non-touch technique. Intra-rater and inter-rater reliability of the two assessment techniques were evaluated using intra-class correlation coefficients (ICCs), limits of agreement, standard error of measurement, and minimal detectable change statistics.
Results
Mean age was 59.9 (standard deviation [SD], 10.5) years, 68.8% were male, average duration of diabetes was 20.6 (SD, 15.1) years, 71.9% had type 2 diabetes, 93.8% had peripheral neuropathy, 43.8% had peripheral arterial disease, and 50% had previous foot ulceration. Charcot foot most commonly affected the tarsometatarsal joints (38.9%), had a median duration of 2.8 (interquartile range [IQR], 1.3 to 5.9) months, and a large proportion were being treated with total contact casting (69.4%). Overall, there was good to excellent intra-rater and inter-rater relative reliability for the ‘touch’ technique (ICC, 0.87 to 0.99; ICC, 0.83 to 0.98, respectively), and excellent intra-rater and inter-rater relative reliability for the ‘non-touch’ technique (ICC, 0.93 to 0.99; ICC, 0.91 to 0.99, respectively). In addition, measurement error was found to be relatively low across the 10 anatomical sites.
Conclusions
Infrared dermal thermometry can now be used with confidence in clinical and research settings to provide a reliable assessment of skin temperature in patients with Charcot neuroarthropathy, using either a touch or non-touch technique at 10 commonly used testing sites. A non-touch technique, however, was observed to have slightly higher reliability indicating it may be associated with less measurement error than the touch technique.
Similar content being viewed by others
Background
Charcot neuroarthropathy (CN), commonly referred to as ‘Charcot foot’, is a serious limb-threatening complication seen in individuals with peripheral neuropathy. Although diabetic neuropathy is the most common cause [1, 2], it can also result from other conditions with neuropathic manifestations, such as alcoholism and renal failure [1, 3]. The estimated prevalence of CN ranges from 0.08% in the general diabetes population to 13% in the diabetes high-risk foot population [1, 4].
CN is a progressive and destructive bone and joint disease that can affect single or multiple joints of the foot and ankle [1, 2, 5]. It is characterised by acute fractures, joint subluxation, dislocation and instability, and bony destruction [2, 6, 7]. Acute CN typically presents as a warm, erythematous, and oedematous foot [5]. Misdiagnosis in its early stages can lead to gross foot deformity, ulceration and amputation [7, 8]. Therefore, early detection and management are paramount.
Hand-held infrared dermal thermometry is a non-invasive skin temperature assessment used to assist clinical diagnosis, monitor disease progression and resolution, and guide management principles [7, 9,10,11]. A temperature difference of more than two degrees Celsius between the affected and non-affected Charcot foot is used as a clinical marker to detect acute (i.e. active) CN, while temperature differences of less than two degrees Celsius support safe withdrawal of immobilisation (e.g. total contact cast) [7, 10, 12, 13].
Commercially available, low-cost, hand-held infrared thermometers have been shown to have good accuracy, reliability and performance in assessing temperatures within a laboratory setting [14]. Other studies have shown a comparative level of agreement and repeatability between infrared thermometers and thermistor-type thermometers [15, 16]. Despite the wide clinical use of infrared dermal thermometry in the diagnosis, monitoring, and management of CN, there is surprisingly a lack of high-quality evidence to support its reliability. In addition, there is no consensus as to which anatomical sites should be included when performing this assessment. Common testing sites reported in the literature include: the hallux, medial 1st metatarsal head, lateral 5th metatarsal head, plantar metatarsal heads 1, 3 and 5, dorsal midfoot, 1st metatarsocuneiform joint, talonavicular joint, cuboid, plantar heel, and ankle [7, 11, 17, 18]. However, there have been no studies to date that have objectively compared the reliability of these testing sites.
Given the limitations of current evidence, this study aimed to investigate: (i) intra-rater and inter-rater reliability of infrared dermal thermometry using a ‘touch’ and ‘non-touch’ technique, and (ii) provide recommendations on the most reliable anatomical sites to test in patients with CN.
Methods
Ethics approval
This study was approved by the relevant institutional ethics committee (LR74–2014) and all participants gave written informed consent prior to enrolment and data collection.
Participants
Thirty-four participants with CN were consecutively recruited from a metropolitan high-risk foot service (HRFS) in Melbourne, Australia from February 2015 to December 2018 (Fig. 1 and Table 1). Eligibility for the study was determined by an interview and a non-invasive foot assessment. Participants were eligible if they had diabetes mellitus (type 1 or type 2), Charcot foot (defined as modified Eichenholtz stages 0 to 3) [19,20,21], were at least 18 years of age and were cognitively aware (i.e. they could provide informed consent). Participants were excluded if they had insufficient English skills to provide informed consent or follow instructions, had a current foot ulcer or had a lower extremity amputation (defined as a ‘complete loss of any part of the lower extremity’ [22], including any digit and/or partial foot amputation) on the Charcot foot.
Two participants who were eligible and provided consent were lost to follow-up prior to data collection (one was discharged from the HRFS due to completion of care, and the other self-discharged from the HRFS). Thirty-two participants attended their baseline assessment (interview and neurovascular foot examination), but only 30 had their dermal temperatures measured (one self-discharged from the HRFS and one transferred to a different health service) (Fig. 1).
Raters
Two independent raters were used in this study. Rater 1 (N.P.) was a podiatrist with 5 years’ clinical experience, and rater 2 (S.M.D.) was a senior podiatrist with 9 years’ clinical experience of using infrared dermal thermometry in patients with CN.
Procedure
Written informed consent was obtained prior to the collection of any data. Data were collected over one to two appointments, which included a baseline assessment (interview and neurovascular foot examination) and the assessment of dermal temperatures. Figure 1 outlines the study design and flow of participants.
Baseline assessment
Data collection at baseline consisted of an interview with the participant, reviewing medical records, and conducting a non-invasive neurovascular foot assessment. Three examiners (S.M.D., D.K. and N.P.) were involved in the collection of baseline data and performed the foot assessments. Baseline variables relating to participant characteristics, comorbidities, and foot history can be found in Tables 1 and 2. Medical records were referred to for confirmation of medical and foot history.
Participants had their height and weight measured to determine their body mass index. The neurovascular foot assessments were performed as per a previous protocol [23]. Neurological status was determined by evaluating the vibration perception threshold (VPT) with a Horwell® neurothesiometer at the apex of the hallux (average of three measurements), and protective sensation with a Bailey Instruments Ltd.® Semmes-Weinstein 5.07/10 g monofilament at the plantar hallux and plantar 1st and 5th metatarsophalangeal joints. Peripheral neuropathy was defined as VPT > 25 V and/or monofilament score < 3/3 sites in either foot. Arterial status was determined by evaluating pedal pulses (dorsalis pedis and posterior tibial), ankle brachial pressure indices (ABPI) using a Hadeco ES100V3 Bidop® Doppler ultrasound and a WelchAllyn® sphygmomanometer and cuff, and toe-brachial pressure indices (TBPI) using a Hadeco® photoplethysmography probe and toe cuff. Peripheral arterial disease was defined as absence of ≥2 pedal pulses, ABPI ≤0.9, and/or TBPI ≤0.6 [23].
Dermal temperature assessment
Two independent raters (N.P. and S.M.D.) were involved in the collection of dermal temperature data, which was performed during the participants’ usual review appointments in the HRFS. In cases of bilateral CN, the most acute Charcot foot at the time of data collection was included in the statistical analysis of the temperature data.
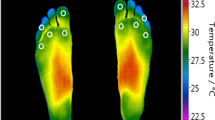
Room and outside temperatures were recorded prior to data collection. The infrared dermal thermometer ‘DermaTemp (DT)-1001’ from Exergen Corporation® (Watertown, Massachusetts) was chosen for this study, as it is a commonly used device in clinical practice [6, 11, 12, 24, 25]. Features of this device include: 1:1 distance-to-spot ratio, sensor diameter of 3 mm, fixed emissivity, and is accurate to ±0.1 °C [7, 14]. To ensure stabilisation of skin temperature prior to assessment, a minimum 15-min acclimatisation period was used (i.e. time from removal of footwear/hosiery) [26]. Dermal temperatures were assessed by the two independent raters on the Charcot foot using a (i) touch and (ii) non-touch technique at 10 anatomical sites of interest (Table 3). The ‘touch’ technique was defined as lightly pressing the device against the skin at the point of interest during measurement. The ‘non-touch’ technique was defined as holding the device approximately 5 mm away from the skin surface at the point of interest during measurement (Fig. 2) [11, 27]. A randomised computer-generated number sequence was used to determine the order of raters and technique used (i.e. touch versus non-touch).
Following each session of the dermal temperature assessments, data sheets were sealed in opaque envelopes. Therefore, raters were blinded to each other’s results and were not able to revise their own results between tests. Independent members of the study team (D.K. and M.R.K.) entered the data into a spreadsheet on the two raters’ behalf.
Statistical analysis
Participant characteristics were calculated and expressed as mean (standard deviation, SD), median (interquartile range, IQR), or number (proportion). Relative reliability was evaluated using intra-class correlation coefficients (ICCs) with corresponding 95% confidence intervals (CI) based on a single rating, absolute agreement, two-way random-effects model. ICC values greater than 0.9 were considered excellent, 0.75 to 0.9 considered good, 0.5 to 0.75 considered moderate, and less than 0.5 considered poor [28]. Absolute reliability was evaluated using standard error of measurement (SEM), minimal detectable change (MDC) and limits of agreement (LOA) statistics. IBM SPSS version 23.0 (IBM Corp, Somers, NY, USA) was used for statistical analysis.
Results
We collected data on 32 adults with diabetes mellitus and CN. The mean age was 59.9 (SD, 10.5) years, 68.8% were male, and the average body mass index was 33.1 (SD, 7.9) kg/m2. The majority had type 2 diabetes (71.9%). The mean duration of diabetes was 20.6 (SD, 15.1) years and the average glycated haemoglobin was 7.7% (SD, 1.3). Peripheral neuropathy, peripheral arterial disease and previous foot ulceration were highly prevalent (93.8, 43.8 and 50%, respectively). Overall, there were a total of 36 Charcot feet among the 32 participants (four participants had bilateral CN). Charcot foot most commonly affected the tarsometatarsal joints (38.9%), followed by the naviculocuneiform, talonavicular, and calcaneocuboid joints (27.8%). The median duration of Charcot foot at the time of the baseline assessment was 2.8 (IQR, 1.3 to 5.9) months. A large proportion of Charcot feet were receiving total contact casting treatment (69.4%). A quarter of the sample (n = 8) had a previous (i.e. resolved) Charcot foot. Participant characteristics, foot history, and foot examination information are shown in Tables 1 and 2.
The average room and outside temperatures recorded at the first dermal temperature assessment were 22.4 °C (SD, 1.0) and 17.3 °C (SD, 5.4), respectively. Following the minimum 15-min acclimatisation period, the median time to performing the dermal temperature assessments was 1.1 (IQR, 0.3 to 5.0) minutes. The results of the relative and absolute reliability of the dermal temperature assessments in the units of measurement degrees Celsius (°C) are shown in Tables 4 and 5.
Intra-rater reliability
Relative reliability was found to be ‘good to excellent’ for the touch technique and ‘excellent’ for the non-touch technique across the 10 sites. ICCs ranged from 0.87 to 0.99 for the touch technique, and 0.93 to 0.99 for the non-touch technique across the two raters. Measurement error was found to be relatively low across the 10 sites for the two raters. MDC values ranged from 0.48 to 1.61 °C (SEM, 0.17 to 0.58 °C) for the touch technique, and 0.40 to 0.96 °C (SEM, 0.15 to 0.35 °C) for the non-touch technique (Table 4).
Inter-rater reliability
Relative reliability was found to be ‘good to excellent’ for the touch technique and ‘excellent’ for the non-touch technique across the 10 sites. ICCs ranged from 0.83 to 0.98 for the touch technique, and 0.91 to 0.99 for the non-touch technique across the two raters. Between the two raters, measurement error was found to be relatively low across the 10 sites. MDC values ranged from 0.64 to 1.30 °C (SEM, 0.23 to 0.47 °C) for the touch technique, and 0.39 to 1.23 °C (SEM, 0.14 to 0.44 °C) for the non-touch technique (Table 5).
Discussion
This study found that infrared dermal thermometry is a highly reliable tool in the clinical assessment of patients with CN. Overall, there was ‘good to excellent’ intra-rater and inter-rater reliability for the touch technique, and ‘excellent’ intra-rater and inter-rater reliability for the non-touch technique. In addition, measurement error was relatively low across the 10 anatomical sites tested. These findings suggest that either a touch or non-touch technique can be used confidently in clinical practice or research settings.
Intra-rater reliability was found to be better than inter-rater reliability for both techniques. Given that infrared thermometry is used to compare dermal temperatures between an affected and non-affected Charcot foot at a particular point in time (rather than across different days), and that the full assessment is most commonly performed by one clinician at any one point in time, intra-rater reliability is most relevant to clinical practice when performing this assessment. That being said, this study also showed high inter-rater reliability for both techniques, therefore, clinicians can remain confident with the temperature readings if the assessment is shared between clinicians.
Interestingly, a non-touch technique was observed to have slightly higher reliability and lower measurement error than the touch technique. This finding was unexpected as the non-touch technique required examiners to estimate a 5 mm distance from the device to the skin surface. One possible explanation for this finding is that the amount of pressure being applied by the raters for the touch technique may have varied, and therefore caused some inconsistencies in the temperature readings. This finding is in contrast to recommendations outlined in the Exergen Corporation® DT-1001 user manual, which states for “maximum accuracy the probe must contact the surface at the point of interest” [29]. While a touch technique may improve accuracy (i.e. temperature measured is reflective of the true temperature), our findings suggest that a non-touch technique is slightly more reliable than the touch technique. The current study focused on investigating the reliability of dermal temperature assessments (i.e. test-retest performance), which from a clinical perspective, is considered most important in establishing temperature differences between an affected and non-affected Charcot foot.
Measurement error was found to be relatively low across the 10 testing sites for the two raters and techniques, as indicated by the MDC values obtained (Tables 3 and 4). The MDC value represents an estimate of the amount of change required (in this case to dermal temperatures) for the change to be considered ‘real’, which is over and above measurement error [30]. As an example, if the MDC value is equal to 0.5, a change in Charcot foot temperature that is ≤0.5 °C in a test-retest scenario (e.g. trial 1 = 28 °C then trial 2 = 27.5 °C) would be accountable to measurement error (e.g. operator error). Inversely, any change in temperature that is greater than 0.5 °C would be due to a true change in temperature. Of the 10 anatomical sites assessed in this study, sites 1 and 2 (plantar 1st and 3rd metatarsal heads) were observed to have consistently high reliability across the raters and techniques. These sites were less likely to be affected by CN in this study, as a large proportion of participants presented with midfoot Charcot. Therefore, a potential explanation for this finding is that sites correlating to joints affected by CN may be less reliable and requires further investigation. Considering previous studies have found that sites of elevated dermal temperature correlate with the joints affected by CN [7, 11, 17], the presentation or pattern of CN is often variable with multiple joints affected, and the number of sites that should be tested in patients with CN is currently unclear, dermal temperature assessments should include an appropriate number and range of relevant sites to account for this. Given that there was no discernible difference in reliability across the 10 anatomical sites used in this study, and the assessment is non-invasive and quick to perform, the 10-site protocol presented in this study can be confidently used in clinical practice.
There are several potential limitations of this study. First, we did not assess different acclimatisation periods and whether they have an impact on the reliability of dermal temperature assessments. As per a previous study’s [26] recommendations, we used a minimum 15-min acclimatisation period to ensure stabilisation of foot temperatures prior to testing. Despite our best efforts to be consistent in the timing of dermal temperature assessments among participants, there was some variability from the end of the 15-min acclimatisation period to the start of the dermal temperature assessment. To adjust for this, room and outside temperatures were recorded prior to data collection to ensure no significant changes to foot temperatures may have occurred. Second, both raters in this study had high levels of clinical experience using infrared dermal thermometry to assess patients with CN. Therefore, it remains unclear whether less experienced clinicians or those with no experience would have reduced reliability when conducting this assessment. Third, we did not assess for the accuracy of the infrared dermal thermometer, therefore, our results can only be used for interpreting reliability of this assessment. Fourth, it remains unclear whether room or outside temperature changes may have had an impact on the dermal temperature measurements. However, as room and outside temperatures were recorded for each assessment by the two raters, and all participants were assessed in the same clinical environment, this was unlikely. In addition, temperature differences between an affected and non-affected Charcot foot is the key clinical factor when assessing CN, therefore, climate control of the environment is not as essential. Fifth, this study used either a touch or non-touch ‘pin-point’ testing method, therefore, our results are not generalisable to clinicians that use the ‘scanning’ method (i.e. moving probe around anatomical site to get highest reading). Sixth, our findings are only generalisable to patients with diabetes-related CN (i.e. not from renal disease, alcoholism etc.). Finally, recall bias may have been present (e.g. participants self-reported previous foot ulcers and CN duration), however medical records were referred to if clarification was needed, so this was unlikely.
There are several strengths of this study. To our knowledge, it is the first study to investigate intra-rater and inter-rater reliability of infrared dermal thermometry in CN. This study had a rigorous inclusion and exclusion criteria, sufficient sample size [28], robust study protocol, and our findings are able to be generalised to clinical practice as our study included patients with CN from a HRFS.
As this is the first study to evaluate the reliability of infrared dermal thermometry in the assessment of patients with CN, there is limited capacity to compare the current study findings to previous literature. Our finding that infrared dermal thermometry is a highly reliable assessment tool, is consistent with a previous laboratory-based study [14]. This study found high reliability (r > 0.989) between temperature change measurements of two raters when comparing nine commercially available infrared thermometers (including the Exergen Corporation® DT-1000) [14]. Infrared thermometry has also been shown to have high correlations between: (i) different thermometers (r > 0.80) in assessing other high-risk foot conditions such as peri-wound temperatures and (ii) the assessment of skin temperature via palpation (rs = 0.81, p < 0.000) [27, 31].
Further research is needed to establish an evidence-based protocol for dermal temperature assessment in patients with CN. Future research may be directed towards investigating the reliability of: (i) a touch and/or non-touch technique of the ‘pin-point’ versus ‘scanning’ method, (ii) the comparison of an affected and non-affected Charcot foot, (iii) different acclimatisation periods, and (iv) the level of clinician experience and/or comparisons between different health professionals in performing dermal temperature assessments.
Conclusions
This is the first study to assess the reliability of dermal temperature assessments in patients with CN. Infrared dermal thermometry can now be used with confidence in clinical and research settings to provide a reliable assessment of skin temperature in patients with CN, using either a touch or non-touch technique at 10 commonly used testing sites. A non-touch technique, however, was observed to have slightly higher reliability indicating it may be associated with less measurement error than the touch technique.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABPI:
-
Ankle-brachial pressure index
- CI:
-
Confidence interval
- CN:
-
Charcot neuroarthropathy
- DT:
-
DermaTemp
- HRFS:
-
High-risk foot service
- ICC:
-
Intraclass correlation coefficient
- IQR:
-
Interquartile range
- LOA:
-
Limits of agreement
- MDC:
-
Minimal detectable change
- SD:
-
Standard deviation
- SEM:
-
Standard error of measurement
- TBPI:
-
Toe-brachial pressure index
- VPT:
-
Vibration perception threshold
References
Frykberg RG, Belczyk R. Epidemiology of the Charcot foot. Clin Podiatr Med Surg. 2008;25:17–28.
Rogers LC, Frykberg RG, Armstrong DG, Boulton AJ, Edmonds M, Van GH, et al. The Charcot foot in diabetes. Diabetes Care. 2011;34:2123–9.
Kaminski MR, Raspovic A, McMahon LP, Lambert KA, Erbas B, Mount PF, et al. Factors associated with foot ulceration and amputation in adults on dialysis: a cross-sectional observational study. BMC Nephrol. 2017;18:293.
Wukich DK, Sung W. Charcot arthropathy of the foot and ankle: modern concepts and management review. J Diabetes Complicat. 2009;23:409–26.
Pitocco D, Scavone G, Di Leo M, Vitiello R, Rizzi A, Tartaglione L, et al. Charcot neuroarthropathy: from the laboratory to the bedside. Curr Diabetes Rev. 2019;16:62–72.
Foltz KD, Fallat LM, Schwartz S. Usefulness of a brief assessment battery for early detection of Charcot foot deformity in patients with diabetes. J Foot Ankle Surg. 2004;43:87–92.
Milne T, Rogers J, Kinnear E, Martin H, Lazzarini P, Quinton T, et al. Developing an evidence-based clinical pathway for the assessment, diagnosis and management of acute Charcot neuro-arthropathy. J Foot Ankle Res. 2013;6:30.
Wukich D, Sung W, Wipf S, Armstrong D. The consequences of complacency: managing the effects of unrecognized Charcot feet. Diabet Med. 2011;28:195–8.
Nubé VL, McGill M, Molyneaux L, Yue DK. From acute to chronic: monitoring the progress of Charcot’s arthropathy. J Am Podiatr Med Assoc. 2002;92:384–9.
van Netten JJ, Prijs M, van Baal JG, Liu C, van der Heijden F, Bus SA. Diagnostic values for skin temperature assessment to detect diabetes-related foot complications. Diabetes Technol Ther. 2014;16:714–21.
Armstrong DG, Lavery LA. Monitoring healing of acute Charcot's arthropathy with infrared dermal thermometry. J Rehabil Res Dev. 1997;34:317–21.
McGill M, Molyneaux L, Bolton T, Ioannou K, Uren R, Yue DK. Response of Charcot's arthropathy to contact casting: assessment by quantitative techniques. Diabetologia. 2000;43:481–4.
Moura-Neto A, Fernandes TD, Zantut-Wittmann DE, Trevisan RO, Sakaki MH, Santos ALG, et al. Charcot foot: skin temperature as a good clinical parameter for predicting disease outcome. Diabetes Res Clin Pract. 2012;96:e11–4.
Foto JG, Brasseaux D, Birke JA. Essential features of a handheld infrared thermometer used to guide the treatment of neuropathic feet. J Am Podiatr Med Assoc. 2007;97:360–5.
Kelechi TJ, Good A, Mueller M. Agreement and repeatability of an infrared thermometer. J Nurs Meas. 2011;19:55–64.
Kelechi TJ, Michel Y, Wiseman J. Are infrared and thermistor thermometers interchangeable for measuring localized skin temperature? J Nurs Meas. 2006;14:19–30.
Bramham R, Wraight P, May K. Management of Charcot neuroarthropathy. Diabetic Foot J. 2011;14:163–70.
Sinacore DR, Hastings MK, Bohnert KL, Fielder FA, Villareal DT, Blair VP III, et al. Inflammatory osteolysis in diabetic neuropathic (Charcot) arthropathies of the foot. Phys Ther. 2008;88:1399–407.
Shibata T, Tada K, Hashizume C. The results of arthrodesis of the ankle for leprotic neuroarthropathy. J Bone Joint Surg Am. 1990;72:749–56.
Rosenbaum AJ, DiPreta JA. Classifications in brief: Eichenholtz classification of Charcot arthropathy. Clin Orthop Relat Res. 2015;473:1168–71.
Eichenholtz SN. Charcot joints. Springfield: Charles C. Thomas; 1966.
Rayman G, Krishnan STM, Baker NR, Wareham AM, Rayman A. Are we underestimating diabetes-related lower-extremity amputation rates?: results and benefits of the first prospective study. Diabetes Care. 2004;27:1892–6.
Kaminski MR, Raspovic A, McMahon LP, Erbas B, Landorf KB. Risk factors for foot ulceration in adults with end-stage renal disease on dialysis: study protocol for a prospective observational cohort study. J Foot Ankle Res. 2015;8:53.
Petrova NL, Moniz C, Elias DA, Buxton-Thomas M, Bates M, Edmonds ME. Is there a systemic inflammatory response in the acute Charcot foot? Diabetes Care. 2007;30:997–8.
Petrova NL, Dew TK, Musto RL, Sherwood RA, Bates M, Moniz C, et al. Inflammatory and bone turnover markers in a cross-sectional and prospective study of acute Charcot osteoarthropathy. Diabet Med. 2015;32:267–73.
Sun P-C, Jao S-HE, Cheng C-K. Assessing foot temperature using infrared thermography. Foot Ankle Int. 2005;26:847–53.
Hoeksma AF, Faber WR. Assessment of skin temperature by palpation in leprosy patients: interobserver reliability and correlation with infrared thermometry. Int J Lepr Other Mycobact Dis. 2000;68:65–7.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Corporation E. DermaTemp 1001 series: User’s manual and reference. Watertown: Exergen Corporation; 2019.
Rohner-Spengler M, Mannion AF, Babst R. Reliability and minimal detectable change for the figure-of-eight-20 method of measurement of ankle edema. J Orthop Sports Phys Ther. 2007;37:199–205.
Mufti A, Somayaji R, Coutts P, Sibbald RG. Infrared skin thermometry: validating and comparing techniques to detect periwound skin infection. Adv Skin Wound Care. 2018;31:607–11.
Acknowledgements
The authors would like to thank Eastern Health for their support of the project and for supplying the equipment used in this study. The authors would like to acknowledge Professor Nicholas Taylor from Eastern Health and La Trobe University for his assistance with the data analysis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
N.P., M.R.K. and S.M.D. contributed to the study conception and design. S.M.D., N.P. and D.K. acquired the data. All authors contributed to the analysis and interpretation of the data. M.R.K., S.M.D. and N.P. drafted the first version of the manuscript. All authors critically revised the manuscript and approved the final text. All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Eastern Health Human Research and Ethics Committee (LR74–2014) and all participants gave written informed consent prior to enrolment and data collection.
Consent for publication
The results presented in this paper have not been published previously in whole or part, except in abstract form. Participant photographs were reprinted with permission.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Adobe professional (.pdf). Screening tool and data collection form. Description of data: Screening tool used for prospective participants and data collection form used to collate the baseline and dermal temperature data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dallimore, S.M., Puli, N., Kim, D. et al. Infrared dermal thermometry is highly reliable in the assessment of patients with Charcot neuroarthropathy. J Foot Ankle Res 13, 56 (2020). https://doi.org/10.1186/s13047-020-00421-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13047-020-00421-z