Abstract
The success of antibodies targeting Programmed cell death protein 1 (PD-1) and its ligand L1 (PD-L1) in cancer treatment and the need for improving response rates has led to an increased demand for the development of combination therapies with anti-PD-1/PD-L1 blockers as a backbone. As more and more drugs with translational potential are identified, the number of clinical trials evaluating combinations has increased considerably and the demand to prioritize combinations having potential for success over the ones that are unlikely to be successful is rising. This review aims to address the unmet need to prioritize cancer immunotherapy combinations through comprehensive search of potential drugs and ranking them based on their mechanism of action, clinical efficacy and safety. As lung cancer is one of the most frequently studied cancer types, combinations that showed potential for the treatment of lung cancer were prioritized. A literature search was performed to identify drugs with potential in combination with PD-1/PD-L1 blockers and the drugs were ranked based on their mechanism of action and known clinical efficacy. Nineteen drugs or drug classes were identified from an internal list of lead molecules and were scored for their clinical potential. Efficacy and safety data from pivotal studies was summarized for the selected drugs. Further, overlap of mechanisms of action and adverse events was visualized using a heat map illustration to help screen drugs for combinations. The quantitative scoring methodology provided in this review could serve as a template for preliminary ranking of novel combinations.
Similar content being viewed by others
Background
In 2020, cancer remained the second leading cause of death with 2 million new cancer diagnoses and over 0.5 million cancer deaths projected in the United States alone [1]. As a new standard of care validated in at least 17 different types of cancer including 2 tissue-agnostic indications, anti-programmed cell death protein 1 (PD-1) and its ligand L1 (PD-L1)-targeted checkpoint inhibitors have harnessed the immune system to radically combat many cancers. Based on durable responses seen across several tumor types, these agents have become a backbone to the largest clinical trial programs in history, raising the bar for clinical efficacy of new therapeutics [2]. Despite growing interest and high eligibility for patients to receive these agents, the percentage of patients expected to respond remains modest for the most part, ranging from 12 to 65 % [3, 4]. This has motivated investigators to develop drugs that go beyond checkpoint blockade and additional standard of care therapies to target other pathways in combination approaches that overcome primary resistance, deepen existing responses, and rescue patients progressing due to secondary resistance. While the research in combination therapy resulted in approval of PD-1/PD-L1 targeting drug combinations with cytotoxic T-lymphocyte antigen 4 (CTLA-4) blockers, chemotherapy, drugs targeting vascular endothelial growth factor (VEGF) and drugs targeting intracellular kinases for over half-a-dozen types of cancer (Supplementary Table S1), additional studies are needed to further improve the response rates and to treat other types of cancer.
The current search for life-altering combination therapies benefiting a broader number of patients across indications is immense and skyrocketing. As of September 2020, there were 2,949 clinical trials of anti PD-1/PD-L1 agents in combination with hundreds of targets to address multiple mechanisms of immune escape. The existing combination trials are estimated to enroll more than half a million patients [2]. Many of these clinical trials evaluate combinations empirically without sufficient knowledge, or with inconsistent understanding regarding translatability of activity and toxicity amongst a plethora of diverse and novel targets. Many of the approaches are of limited utility and are doomed to fail, contributing to the low success rates of anticancer drug development where only 7 % of drugs tested in phase I are expected to reach licensure [5, 6]. Moreover, despite the potential for a greater immune response with combination strategies, many of these run the risk for harmful adverse events and increased, unexpected, overlapping, and synergistic toxicity that could be serious and even lethal [7]. While safety is prioritized, immense resources and careful consideration are required for the evaluation of organ function, laboratory abnormalities, and other complications [8,9,10,11,12]. For these reasons, there is a need to refine approaches that offer less risk, with objective strategic prioritization of resources and streamlining of efforts to support higher success rates in signal seeking combination trials. Failure to de-prioritize combinations that have questionable benefit at an increased risk is a burdensome disservice to patients that comes at a high cost to the society [5, 13,14,15,16]. Ranking of combinations should be multifactorial, including in-depth assessments for the molecular and immune pathways of drugs that can produce desired effects on immune cells [17, 18], and better understanding of relative benefit/risk characteristics.
Challenges in development of combination therapies
As listed in Table 1, the complexity of combination development of cancer immunotherapies is daunting, and currently benefit of long-term disease control appears possible in roughly only 20 % of patients with checkpoint inhibitors [19]. Further, a variety of responses are seen in patients with the same therapy, along with dissimilar responses by tumor type given high disease heterogeneity and varying tumor immune phenotype [20]. For an immunotherapy to be effective, effector immune cells must traffic to the tumor, infiltrate stroma, and overcome a hostile immunosuppressive tumor microenvironment [21]. Preclinical models poorly predict the success of clinical candidates and translating basic research and preclinical findings to optimal clinical combinations remains arduous [20]. Mechanisms of primary and acquired resistance during treatment with immunotherapies remain to be elucidated. Patient selection and stratification based on relevant biomarkers has been substantially limited and near non-existent; a study of planned clinical trials in 2019 showed that less than 10 % of the studies required biomarkers for enrollment [22]. A very limited number of biomarkers are linked to higher chance of response to anti-PD(L)1-based immunotherapies at the population level, e.g., PD-L1 and tumor mutational burden (TMB) [23]. And, to date, even the most sophisticated biomarker relationships are not entirely predictive of response in individual patients. Benefits for the average patient may not help an individual patient and, although, it is clear that immunotherapies have revolutionized oncology therapy, they have fallen short of widespread successes [24]. For more than 75 % of patients with cancer, the opportunity to participate in a clinical trial is non-existent, due to a lack of local trials for or due to trial ineligibility [25]. For testing of new immunotherapy combinations, there is a fierce competition to recruit any remaining eligible patients, demonstrated by dwindling enrollment rates in the United States [26]. Thus there is an urgent need for clearer mechanistic rationale for prioritizing new clinical trials of combination cancer immunotherapies [24], to allow for better understanding the complex interaction of drugs on a patient’s immune system, the interplay of immune cells and cancer cells, and for prediction of adverse effects.
Review objectives
The aim of this review is to support the development of immunotherapy combinations and address the challenge of identification of potential drugs for combinations. Since the efficacy of immunotherapy as monotherapy and combinations can vary with cancer type, we focused our review on lung cancer, which is one of the most frequently studied cancer types. We propose a ranking system based on the pharmacology of drugs and apply the method to rank the promising drugs for immunotherapy combinations for lung cancer treatment. We present an objective, and comprehensive review of select targets that may serve as a rational basis and illustrative tool to help narrow the selection. We mined and incorporated a wide range of drugs and focused on several of the most interesting targets of high potential for combination immunotherapy. This review is organized as follows: first, the methods section describes the selection of the initial list of drugs and ranking methodology used to select the lead molecules; next, stages involved in selecting the final set of drugs are described; then, the risk-benefit profile with emphasis on overlap of mechanisms of action and safety profile are described; and lastly, the strengths and limitations of the review are discussed along with the summary of the review.
Methods
Selection of initial list of drugs/molecular targets
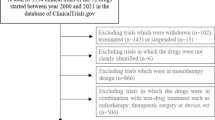
Our approach is illustrated by the flow chart displayed in Fig. 1. A list of drugs and molecular targets was provided from the internal clinical development programs as a starting point. The main criteria for selecting the drugs during our screening were, in order of importance: (1) Drugs for which there is enough information on their mode of action, especially relevant to their action on the immune system; (2) Drugs that have complementary mechanisms of action in cancer immunity and that could potentially work well in combination; (3) Drugs for which there is enough data to derive a preliminary characterization of their efficacy and safety/toxicity profile in human; and lastly, (4) Drugs that have already been approved as monotherapy or combination therapy and with significant information on safety. Drugs already tested in combinations, or applicable to a larger number of cancer types (only solid tumors), carry higher value in our selection process. Points 3 and 4 imply that we limit our analysis to drugs that have already been tested in the clinic. There are several reasons for doing that. First, as pointed out above, identifying combinations that may succeed in the clinic is extremely challenging. Doing so with no monotherapy clinical efficacy and/or safety data would make this analysis too speculative. Second, the vast majority of all combinations being evaluated in clinical trials at this time have previous clinical exposure as monotherapy agents. This is for mitigation of the risk of failure. Our approach proposes a more thorough and analytical assessment of drugs with existing clinical exposure before they are evaluated in combination in the clinic.
Ranking methodology
Our initial screening was done for 72 drugs that were either already approved for clinical use or were in clinical development (Fig. 1). All 72 drugs were carefully assessed, scored, and ranked, based on the scoring criteria summarized in Table 2. While all the selected drugs had promising potential, the cross talk of their mechanism of action with immune response, granular knowledge of downstream pathways effected by the treatment and their efficacy in solid versus heme cancers varied widely. Therefore, drugs were mainly scored for their clinical potential, relevance to immunotherapy, relevance to indication, knowledge of the MOA, effect on immune response, availability of clinical efficacy data.
Scores were derived from the compilation of detailed literature review and ranged from 1 (low) to 3 (high) in each category. After initial screening of drugs based on clinical anti-cancer potential (yes/no) in stage I (Table 2; Fig. 1), 72 drugs/class of drugs were selected. In stage II, all 72 drugs were scored based on relevance to immunotherapy (Table 2; Fig. 1) resulting in the elimination of 38 drugs. The remaining drugs of interest are displayed in Fig. 2, where the diversity in modes of action can easily be perceived. The drugs are arranged radially by their stage of clinical development (from phase 1 to approved). The categories of drugs/mode of action are further grouped by type of cancer-immune phenotypes they are most likely to be applicable to (inflamed/hot, desert/cold or multiple). Lastly, the drugs are labeled as ‘Active’ or ‘Passive’ depending on the way they engage the immune system, either directly (such as immune checkpoint inhibitors) or passively (such as chemotherapy).
Pie chart of molecule classification. Coloring is used to identify tumor type, and mechanism of action, with the inner sectors representing development stage. Drugs are classified using a hybrid of multiple components including development stage, tumor type, mechanism of action, and are bucketed as passive or active immunotherapies based on immune response activation. Passive immunotherapies include molecules expressed in low levels; they rectify deficient immune system typically used for patients with impotent immune systems. These could include the monoclonal antibodies targeting malignant cells, adoptive transfer of immune cells, adjuvants, recombinant cytokines, inhibitors of signaling pathways, delivery of cytotoxins, activators of ADCC, tumor antigen targeting, and oncolytic viruses; which typically require multiple administrations to be efficient. Active immunotherapies are designed to activate effector function of immune cells. These include activation of endogenous and long-lasting immune responses including vaccines, blockade by checkpoint inhibitors, oncolytic viruses, immunomodulatory mAbs, immunostimulatory cytokine adjuvants to augment immunotherapy response, mAbs to proinflammatory cytokines, immunogenic cell death inducers such as chemotherapies, and pattern recognition receptor agonists.
The 34 remaining drugs were then scored in the Stage III screening (Supplementary Table S2) where 8 drugs were excluded (Fig. 1). Finally, in the stage IV screening, 7 more drugs were excluded and 19 drugs were selected. This list is displayed in the Supplementary Table S3 and represents the final step of the methodology flow chart provided in Fig. 1. A key point to be noted in our ranking model is that the availability of data for clinical activity or efficacy scoring is applied at the final stage, which prevents low scoring and eventual screening out of drugs that only have early efficacy data. Similarly, the number of indications in clinical development is only one component of the stage III scoring, allowing drugs in early stages of clinical development to be selected for evaluation of mechanism and safety overlap discussed in later sections. Finally, the current model gives more weight to drugs with clinical data in lung cancer and solid tumors. It can be adapted to other indications such as hematological cancers by weighting the data accordingly.
Literature mining
Literature was collected by screening publicly available information using search portals such as PubMed, Google Scholar, Web of Science, as well as relevant conference websites including ASCO, ESMO, SITC, in addition to clinicaltrials.gov. In reviewing the literature on the mode of action of the drugs in our list, we focused our attention in identifying the most upstream effects of the drugs on the cancer/immune biology, as opposed to downstream effects. This approach allowed for an easier assessment of drugs that may lead to functional interactions in combination.
For our data collection effort of each of the drugs in Supplementary Table S3, we looked for 3 kinds of data, including: (1) Information on ongoing clinical trials that included the developmental phase, combination with other agents, indication, dose (if already established), and primary endpoints; (2) top-down data including baseline characteristics of patient population and clinical readouts from already published clinical trials; and (3) bottom-up data including data pertaining to the mechanism of action of the drugs. For top-down data, priority was given to data from phase 3 clinical trials, then phase 2 and phase 1. Response clinical endpoints such as the objective response rate (ORR) and the disease control rate (DCR) were recorded, as well as time to event endpoints including progression free survival (PFS) and overall survival (OS). All solid tumors were prioritized, and hematological tumors were not considered. For the bottom-up data, priority was given to collecting information on the effect of the drugs on immune cells in human, in plasma and in the tumor microenvironment (when available).
Selected drugs
Out of the 20 drugs (including anti-PD-1/L1 antibodies) selected for our final summary and listed in Supplementary Table S3, 7 drugs/class of drugs are approved for the treatment of cancer (single/multiple types of cancer; monotherapy or combination with other anti-cancer therapies). All of them are currently under investigation or actively considered for combination with PD-1/PD-L1 blockers. Details of the molecular targets for each drug/drug class are included in Supplementary Table S2. In the following section, efficacy of combinations and potential for synergism are explained using the overlap of mechanism of action (MOA), while risks associated with combinations are explained using safety and serious/dose limiting adverse event (AE) overlap.
Benefit risk profile
Efficacy: mechanism of action overlap and potential for synergistic effects
Killing of tumor cells and eradication of tumors from the body by the immune system is illustrated in Fig. 3 with key events highlighted as nodes. Tumor size has been shown to be negatively associated with activation of immune response [27,28,29,30] and tumor cell cytotoxicity can be achieved by activated effector T-cells and natural killer (NK) cells [31, 32]. The levels of activated effector T-cells and NK cells in the tumor microenvironment (TME) is dependent on the ability of the cells to infiltrate the TME and decreased tumor infiltration of immune cells is a common mechanism of immune escape [33,34,35]. Activation of T-cells is dependent on antigen presentation and on phenotype of antigen presenting cells including dendritic cells (DCs) and macrophages [36,37,38]. Activity of effector T-cells and NK depends on levels of immune suppressor cells such as regulatory T-cells (Tregs) and myeloid-derived suppressor cells (MDSCs) in the TME. Similarly, immune cell exhaustion is known to negatively affect the activity of effector T-cells and NK cells. Immune checkpoints such as PD-1, CTLA-4, T cell immunoreceptor with Ig and ITIM domains (TIGIT), T cell immunoglobulin and mucin domain-containing protein 3 (Tim-3) and lymphocyte activation gene-3 (Lag-3) inhibit the activation of effector T-cells and NK cells and promote exhaustion.
Flow chart showing the point of action for screened drugs. Tumor cell cytotoxicity is mainly achieved by effector T-cells and NK cells, which results in antigen release and reduction in tumor size. Release of antigens along with cellular components such as danger associated molecular patterns (DAMPs) result in maturation of DCs and macrophages, which present antigens and activate the T-cells, and promote their differentiation into effector T-cells. Tumor size is known to negatively affect the activity of effector T-cells and NK cells. Similarly, presence of immunosuppressor cells in tumor microenvironment and exhaustion have negative effects on the activity of effector T-cells and NK cells. Finally, decreased infiltration of effector T-cells and NK cells in the tumor also leads to decreased anti-tumor immune response. In the flow diagram, all the major processes that control the anti-tumor immune response are presented as nodes. (+) indicates positive effect of the molecule/target on the node and (-) indicates inhibitory effect of the molecule/target on the node
As illustrated in Fig. 3, drugs can act at multiple nodes and activate the anti-tumor immune response. Drugs that have direct cytotoxic effects, such as chemotherapeutics, can positively influence the immune response by promoting antigen release and thereby modulating DC/macrophage phenotype and antigen presentation; and also, by reducing the concentration of immune-suppressor cells such as Tregs and MDSCs in the TME. Drugs such as selicrelumab can activate effector immune cells directly and indirectly by activating antigen presenting cells (APCs). Monoclonal antibodies against immune checkpoints can block inhibitory effects of checkpoints to reinvigorate exhausted immune cells, regulate APC phenotype (CTLA-4 and TIGIT blockers) and directly modulate antigen presentation (Tim-3 blockers).
On the other hand, multiple drugs can act on a single node and with overlapping mechanisms of action as shown in Fig. 4A. In the drugs screened for the final summary of efficacy, primary overlap was seen in their effects on APC phenotype/maturation, T-cell activation, levels/function of immune suppressor cells and tumor size/antigen release (Fig. 4A). Combination of chemotherapy and PD-1/PD-L1 blockers, which has been approved for treatment of metastatic non-small cell lung cancer (NSCLC) [39,40,41,42], had minimal overlap of mechanisms. Chemotherapy affected the tumor size, induced antigen release and reduced the levels of immune suppressor cells, while PD-1/PD-L1 blockers where shown to activate T-cells, NK-cells and inhibit function and maturation of immune suppressor cells (Fig. 4A). Similarly, bevacizumab additionally induced APC maturation and increased immune cell infiltration [43,44,45]. Ipilimumab, which stimulated APC phenotype and induced central activation of T-cells was a successful combination with PD-1 blockers [46,47,48]. Details from Fig. 4A can thus be used to deduce possibilities of synergism in combinations with complementary non-overlapping mechanisms, or additive effects in novel combinations with some degree of overlapping mechanisms.
Heat map showing overlap of (A) Mechanism of action (B) Serious AEs and/or Grade 3 or above AEs for screened drugs (A) *chemotherapy has also been shown in some studies to downregulate PD-L1 and PD-L2 expression on DCs and induce cytotoxic activity of CTLs and NK cells, B * Early reports from clinical studies evaluating TIGIT did not report any dose limiting toxicities, except a case of grade 2 diarrhea. **Reduced blood cell count is used as a broad category of AEs and includes direct suppression of bone marrow generation of blood cells as well as indirect reductions in blood cell counts resulting in neutropenia, anemia, decreased lymphocyte count and thrombocytopenia. *** SAEs sorted in the ‘Others’ category are sometimes unique for the drug and cannot be combined as a single category. Early phase 1 studies for anti-Tim-3, anti-Lag-3, AB928 and Reolysin did not report serious adverse events but evidence from studies in larger cohort is not available and are represented accordingly (grey). Data includes rare events and may include AEs that are probably not related to study. ARF, acute renal failure; ALF, acute liver failure
While understanding the overlap of molecular mechanism of action could provide an overview of efficacy of the combination, combinations can fail to translate their success from preclinical to clinical studies. Data from clinical studies would therefore be critical in estimating the potential of the combination. Table 3 summarizes the available efficacy data (solid tumors) for the drugs selected in our final stage of screening and scores the data based on availability. For drugs and class of drugs that are approved as monotherapy, only the key studies that are relevant for discussion are summarized. Isatuximab, which was studied mainly in heme cancers, received the lowest score on data availability, while drugs in early clinical development including FAP-IL-2 V, BL-8040, Hu5F9G4, AB928 and tocilizumab (approved in the non-oncology setting), received moderate scores.
Safety: overlap and potential for severe adverse events
Another important factor to be weighed while designing combination therapies is the potential for increased prevalence of severe AEs, which can lead to cessation of therapy or to a fatal outcome. Immunotherapy is considered to have a comparatively mild to moderate safety profile and AEs are mostly managed with corticosteroids [91,92,93]. However, severe dose-limiting immune-related AEs such as hepatitis and myocarditis, colitis, and endocrine disorders, are reported in some patients [91, 92, 94]. More importantly, adverse events of special interest were found to be more commonly reported in responding patients compared to non-responders [95]. Combination of PD-1 and CTLA-4 blockers has been associated with increased incidence of adverse events [46, 47, 96, 97] and with precipitation of severe myocarditis in some patients [98, 99]. Furthermore, the incidence of dose-limiting grade 3–4 AEs is also higher with combination immunotherapy; which was over 50 % in melanoma patients, over 30 %-50 % in lung, prostate and esophageal cancer patients and 14 % in patients with unresectable sarcoma with combination of ipilimumab and nivolumab [100]. Interestingly, incidence of grade 3–4 AEs mirrored the response to therapy and the cancers that were most responsive to the combination had highest incidence [100]. While on one hand, the incidence of all AEs and grade 3–4 AEs provides an overall idea of the safety profile, it cannot clearly identify a risky/unsafe combination. It is possible that the safety profile of drugs used in a combination does not overlap resulting in an overall increase incidence of AEs but without precipitation of serious adverse events. On the other hand, drugs may have manageable safety profile as monotherapy but could precipitate serious AE in susceptible patients when used in combination.
Understanding the safety profile of the drugs used in a combination and the overlap of AEs is essential in designing safe combination therapies. Supplementary Table S4 lists the commonly reported AEs and serious/dose-limiting, grade 3 or above AEs for the drugs selected in our final stage of screening. Figure 4B visualizes serious/dose-limiting, grade 3 or above AEs from Supplementary Table S4 as a heat map and illustrates the possible overlap of AEs. The set of AEs that were most commonly reported included rash, infusion site reaction and fever, followed by abnormalities in blood cell counts, liver abnormalities and gastrointestinal abnormalities (Fig. 4B). The heatmap of AEs presented in Fig. 4B also identifies the possible cases where serious AE can be precipitated. For example, dyspnea and respiratory failure might be expected to be severe in a combination with FAP-IL2v and Imprime PGG. Similarly, hypotension and syncope can be expected to be severe in a combination with FAP-IL2v and BL-8040 (Fig. 4B). While Supplementary Table S4 and Fig. 4B list the commonly seen AEs and illustrate their overlap, they do not capture the incidence or rate of AEs. Information from the AE heatmap together with the incidence of AE can help in identifying potential common serious adverse events.
Strengths and limitations
This review presents a unique approach of identifying potential combinations of high interest for clinical development. The literature was extensively screened for various key pieces of information on mechanism of action, which provides an initial indication of whether the combination has potential for success. The overlap of mechanisms may also provide a possible indication on whether the combination could have additive or synergistic activity. The safety data curated from the literature helps our understanding of the overall AE profile and AE overlap of combinations help in identifying serious AEs in need of careful safety monitoring. Combined analysis of mechanism and safety overlaps for a combination can thus help in anticipating the likelihood of success. For example, looking at the overlaps in the mechanisms of action and safety profiles of anti-VEGF drugs and PD-(L)1 blockers, we see a complementary overlap in mechanisms but no overlap in serious AEs, which could explain the success of bevacizumab plus atezolizumab and cabozatinib plus nivolumab combinations in the clinic. Further, the efficacy data included in the review for the drugs in early stages of clinical development could help rescue drugs with marginal monotherapy efficacy but with promising combination outcomes, as suggested by this analysis and vice versa. Lastly, the methods and ranking protocols used in this review could also be useful in developing combinations based on additional targets introduced in the future.
Our review is not a one size fits all approach but can provide a few examples that assist with asset prioritization, ranking and decision making. One of the main limitations of this review is that it is not a true systematic review, and as such selection bias with respect to the drugs that are included, and literature related to the included drugs is not ruled out. For example, we limited the selection of drugs to a few representatives of each mode of action category to favor diversity of drug mechanisms. Radiation therapy, which is an integral part of cancer treatment could not be included in the review because the scope was limited to pharmacological therapy [101]. Similarly, cell-based therapies such as cancer vaccines, NK cells and chimeric antigen receptor T cells (CAR-T cells) and antibody therapies such as bispecific antibodies could not be included due to limited applications. The ranking of the drugs was mainly based on the availability of clinical data and drugs that were excluded due to lack of clinical data could show promising clinical efficacy in future studies. While strategies for prioritizing drugs in preclinical and early clinical stages was out of scope for this review, we think drugs with promising safety in preclinical studies should be given more weight over efficacy during the development of ranking strategy. Lastly, patient selection, biomarkers, disease/patient prognostic factors, dosage of combinations and sequence of administration that are known to be of significant influence on the success of combination cancer immunotherapies were also out of the scope of the review and were not discussed. This review should be therefore cautiously interpreted and applied with due consideration of the limitations.
Summary
Specific strategies for therapies towards a large number of targets with modern cancer immunotherapy combinations that broadly benefit a larger number of patients with cancer must be brought forward. The analysis conducted herein aims to better understand particular characteristics of potential drugs to co-target in new combinations. We aim to provide clinically relevant insights and quantitative pharmacology-based ranking as a tool to improve combination testing. Our goal is to raise awareness of the multitude of issues impacting combination selection and development to draw attention to the need for further fine-tuned methodologies for more optimal selection for both current and future clinical trials. Our review encourages future efforts of this sort to rank combinations of highest interest as to how they may interact when given together, with a certain consideration for when to move forward, and potential items of caution. While our focus is on patients with metastatic cancers, there is also a paradigm shift and recent focus to test combination immunotherapies against earlier stages of cancer, and similar strategies described herein can also be considered for combination trials in the neoadjuvant and adjuvant setting [4, 102]. Expansion of the quantitative pharmacology based ranking approach herein may be addressed for new targets, lines of therapies, and biomarker selected populations. Moving forward, creative umbrella, basket, broad, and flexible platform trial designs across multiple disease areas that adapt and scale to emerging safety and efficacy findings will be key to testing.
Conclusion
In conclusion, our review highlights the need for strategies to prioritize and rank the potential leads for combination immunotherapy and proposes quantitative pharmacology-based ranking as an approach. Comprehensive ranking based on fundamental molecular and cellular pharmacological foundations and relevant mechanisms of action to hit multiple targets may at least provide a partial solution to the complexity challenge by better predicting optimal strategies.
Availability of data and materials
All data generated in the study has been included in the manuscript and accompanying supplementary information.
Abbreviations
- PD-1:
-
Programmed cell death protein 1
- CTLA-4:
-
Cytotoxic T-lymphocyte antigen 4
- VEGF:
-
Vascular endothelial growth factor
- TMB:
-
Tumor mutational burden
- ORR:
-
Objective response rate
- CR:
-
Complete response
- PR:
-
Partial response
- DCR:
-
Disease control rate
- PFS:
-
Progression free survival
- OS:
-
Overall survival
- MOA:
-
Mechanism of action
- AE:
-
Adverse event
- NK cells:
-
Natural killer cells
- TME:
-
Tumor microenvironment
- DCs:
-
Dendritic cells
- Tregs:
-
Regulatory T-cells
- MDSCs:
-
Myeloid-derived suppressor cells
- TIGIT:
-
T cell immunoreceptor with Ig and ITIM domains
- Tim-3:
-
T cell immunoglobulin and mucin domain-containing protein 3
- Lag-3:
-
Lymphocyte activation gene-3
- APCs:
-
Antigen presenting cells
- CAR-T cells:
-
Chimeric antigen receptor T cells
- mITT:
-
Modified intent to treat population
- NSCLC:
-
Non-small cell lung cancer
- MAP:
-
Metastatic adenocarcinoma of pancreas
- PDAC:
-
Pancreatic ductal adenocarcinoma
- CRC:
-
Colorectal cancer
- TNBC:
-
Triple negative breast cancer
- OC:
-
Ovarian cancer
- CRPC:
-
Castration-resistant prostate cancer
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Upadhaya S, Neftelino ST, Hodge JP, Oliva C, Campbell JR, Yu JX. Combinations take centre stage in PD1/PDL1 inhibitor clinical trials. Nat Rev Drug Discov. 2021;20:168–69.
Haslam A, Prasad V. Estimation of the percentage of us patients with cancer Who are eligible for and respond to checkpoint inhibitor immunotherapy drugs. JAMA Netw Open. 2019;2:e192535.
Topalian SL, Taube JM, Pardoll DM. Neoadjuvant checkpoint blockade for cancer immunotherapy. Science. 2020;367(6477):eaax0182.
Gyawali B, Prasad V. Drugs that lack single-agent activity: are they worth pursuing in combination? Nat Rev Clin Oncol. 2017;14:193–4.
Hay M, Thomas DW, Craighead JL, Economides C, Rosenthal J. Clinical development success rates for investigational drugs. Nat Biotechnol. 2014;32:40–51.
Haanen J, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, Jordan K, Committee EG. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv119-42.
Seymour L, Ivy SP, Sargent D, Spriggs D, Baker L, Rubinstein L, Ratain MJ, Le Blanc M, Stewart D, Crowley J, et al. The design of phase II clinical trials testing cancer therapeutics: consensus recommendations from the clinical trial design task force of the national cancer institute investigational drug steering committee. Clin Cancer Res. 2010;16:1764–9.
LoRusso PM, Boerner SA, Seymour L. An overview of the optimal planning, design, and conduct of phase I studies of new therapeutics. Clin Cancer Res. 2010;16:1710–8.
Senderowicz AM. Information needed to conduct first-in-human oncology trials in the United States: a view from a former FDA medical reviewer. Clin Cancer Res. 2010;16:1719–25.
Paller CJ, Bradbury PA, Ivy SP, Seymour L, LoRusso PM, Baker L, Rubinstein L, Huang E, Collyar D, Groshen S, et al. Design of phase I combination trials: recommendations of the Clinical Trial Design Task Force of the NCI Investigational Drug Steering Committee. Clin Cancer Res. 2014;20:4210–7.
Woodcock J, LaVange LM. Master Protocols to Study Multiple Therapies, Multiple Diseases, or Both. N Engl J Med. 2017;377:62–70.
Gyawali B, Sullivan R. Economics of cancer medicines: for whose benefit? New Bioeth. 2017;23:95–104.
Li GH, Qu Q, Qi TT, Teng XQ, Zhu HH, Wang JJ, Lu Q, Qu J. Super-enhancers: a new frontier for epigenetic modifiers in cancer chemoresistance. J Exp Clin Cancer Res. 2021;40:174.
Luo XY, Wu KM, He XX. Advances in drug development for hepatocellular carcinoma: clinical trials and potential therapeutic targets. J Exp Clin Cancer Res. 2021;40:172.
Prasad V, McCabe C, Mailankody S. Low-value approvals and high prices might incentivize ineffective drug development. Nat Rev Clin Oncol. 2018;15:399–400.
Ochoa de Olza M, Navarro Rodrigo B, Zimmermann S, Coukos G. Turning up the heat on non-immunoreactive tumours: opportunities for clinical development. Lancet Oncol. 2020;21:e419-30.
Abdou Y, Pandey M, Sarma M, Shah S, Baron J, Ernstoff MS. Mechanism-based treatment of cancer with immune checkpoint inhibitor therapies. Br J Clin Pharmacol. 2020;8(9):1690-702.
Schilsky RL, Nass S, Le Beau MM, Benz EJ Jr. Progress in cancer research, prevention, and care. N Engl J Med. 2020;383:897–900.
Hegde PS, Chen DS. Top 10 challenges in cancer immunotherapy. Immunity. 2020;52:17–35.
Ascierto PA, Bifulco C, Galon J, Garbe C, Khleif SN, McQuade J, Odunsi K, Okada H, Paulos CM, Quezada SA, et al: The Great Debate at ‘Immunotherapy Bridge’, Naples, December 5, 2019. J Immunother Cancer. 2019;7(1):221.
Adashek J, Goloubev A, Kato S, Kurzrock R. Immunotherapy trials lack a biomarker for inclusion: implications for drug development. J ImmunoTher Cancer. 2020;8.
Marabelle A, Fakih M, Lopez J, Shah M, Shapira-Frommer R, Nakagawa K, Chung HC, Kindler HL, Lopez-Martin JA, Miller WH Jr, et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020;21:1353–65.
de Miranda N, Trajanoski Z. Advancing cancer immunotherapy: a vision for the field. Genome Med. 2019;11:51.
Minasian LM, Unger JM. What keeps patients out of clinical trials? JCO Oncol Pract. 2020;16:125–7.
Xin Yu J, Hodge JP, Oliva C, Neftelinov ST, Hubbard-Lucey VM, Tang J. Trends in clinical development for PD-1/PD-L1 inhibitors. Nat Rev Drug Discov. 2020;19:163–4.
Milas L, Hunter N, Mason K, Withers HR. Immunological resistance to pulmonary metastases in C3Hf-Bu mice bearing syngeneic fibrosarcoma of different sizes. Cancer Res. 1974;34:61–71.
Nishino M, Giobbie-Hurder A, Ramaiya NH, Hodi FS. Response assessment in metastatic melanoma treated with ipilimumab and bevacizumab: CT tumor size and density as markers for response and outcome. J Immunother Cancer. 2014;2:40.
Joseph RW, Elassaiss-Schaap J, Kefford R, Hwu WJ, Wolchok JD, Joshua AM, Ribas A, Hodi FS, Hamid O, Robert C, et al. Baseline Tumor Size Is an Independent Prognostic Factor for Overall Survival in Patients with Melanoma Treated with Pembrolizumab. Clin Cancer Res. 2018;24:4960–7.
Nesseler JP, Lee MH, Nguyen C, Kalbasi A, Sayre JW, Romero T, Nickers P, McBride WH, Schaue D: Tumor size matters-understanding concomitant tumor immunity in the context of hypofractionated radiotherapy with immunotherapy. Cancers (Basel). 2020;12(3):714–26.
Morvan MG, Lanier LL. NK cells and cancer: you can teach innate cells new tricks. Nat Rev Cancer. 2016;16:7–19.
Malhotra A, Shanker A. NK cells: immune cross-talk and therapeutic implications. Immunotherapy. 2011;3:1143–66.
Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–64.
Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61.
Bhandaru M, Rotte A. Monoclonal antibodies for the treatment of melanoma: present and future strategies. Methods Mol Biol. 2019;1904:83–108.
Palucka K, Banchereau J. Cancer immunotherapy via dendritic cells. Nat Rev Cancer. 2012;12:265–77.
Walsh KP, Mills KH. Dendritic cells and other innate determinants of T helper cell polarisation. Trends Immunol. 2013;34:521–30.
Rotte A, Bhandaru M. Dendritic Cells. Cham: Springer International Publishing; 2016.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, Domine M, Clingan P, Hochmair MJ, Powell SF, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378:2078–92.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gumus M, Mazieres J, Hermes B, Cay Senler F, Csoszi T, Fulop A, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med. 2018;379:2040–51.
Weinberg F, Gadgeel S. Combination pembrolizumab plus chemotherapy: a new standard of care for patients with advanced non-small-cell lung cancer. Lung Cancer. 2019;10:47–56.
Reck M, Ciuleanu TE, Dols MC, Schenker M, Zurawski B, Menezes J, Richardet E, Bennouna J, Felip E, Juan-Vidal O, et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. In ASCO Annual Meeting. J Clin Oncol. 2020;38:9501.
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodriguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med. 2018;378:2288–301.
Reck M, Mok TSK, Nishio M, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodriguez-Abreu D, Moro-Sibilot D, et al. Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir Med. 2019;7:387–401.
Reck M, Shankar G, Lee A, Coleman S, McCleland M, Papadimitrakopoulou VA, Socinski MA, Sandler A. Atezolizumab in combination with bevacizumab, paclitaxel and carboplatin for the first-line treatment of patients with metastatic non-squamous non-small cell lung cancer, including patients with EGFR mutations. Expert Rev Respir Med. 2020;14:125–36.
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med. 2015;373:23–34.
Postow MA, Chesney J, Pavlick AC, Robert C, Grossmann K, McDermott D, Linette GP, Meyer N, Giguere JK, Agarwala SS, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015;372:2006–17.
Long GV, Atkinson V, Cebon JS, Jameson MB, Fitzharris BM, McNeil CM, Hill AG, Ribas A, Atkins MB, Thompson JA, et al: Standard-dose pembrolizumab in combination with reduced-dose ipilimumab for patients with advanced melanoma (KEYNOTE-029): an open-label, phase 1b trial. Lancet Oncol. 2017;18(9):1202–10.
Squibb BM. Bristol Myers Squibb Announces RELATIVITY-047, a Trial Evaluating Anti-LAG-3 Antibody Relatlimab and Opdivo (nivolumab) in Patients with Previously Untreated Metastatic or Unresectable Melanoma, Meets Primary Endpoint of Progression-Free Survival. 2021.
Caruso C. Tiragolumab impresses in multiple trials. Senior Reporter, Cancer Discovery, AACR. Cancer Discov. 2020;10:1086–1087.
Socinski MA, Bondarenko I, Karaseva NA, Makhson AM, Vynnychenko I, Okamoto I, Hon JK, Hirsh V, Bhar P, Zhang H, et al. Weekly nab-paclitaxel in combination with carboplatin versus solvent-based paclitaxel plus carboplatin as first-line therapy in patients with advanced non-small-cell lung cancer: final results of a phase III trial. J Clin Oncol. 2012;30:2055–62.
West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, Kopp HG, Daniel D, McCune S, Mekhail T, et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:924–37.
Takeda M, Yamanaka T, Seto T, Hayashi H, Azuma K, Okada M, Sugawara S, Daga H, Hirashima T, Yonesaka K, et al. Bevacizumab beyond disease progression after first-line treatment with bevacizumab plus chemotherapy in advanced nonsquamous non-small cell lung cancer (West Japan Oncology Group 5910L): an open-label, randomized, phase 2 trial. Cancer. 2016;122:1050–9.
Thatcher N, Goldschmidt JH, Thomas M, Schenker M, Pan Z, Paz-Ares Rodriguez L, Breder V, Ostoros G, Hanes V. Efficacy and Safety of the Biosimilar ABP 215 Compared with Bevacizumab in Patients with Advanced Nonsquamous Non-small Cell Lung Cancer (MAPLE): A Randomized, Double-blind, Phase III Study. Clin Cancer Res. 2019;25:2088–95.
Patel JD, Socinski MA, Garon EB, Reynolds CH, Spigel DR, Olsen MR, Hermann RC, Jotte RM, Beck T, Richards DA, et al. PointBreak: a randomized phase III study of pemetrexed plus carboplatin and bevacizumab followed by maintenance pemetrexed and bevacizumab versus paclitaxel plus carboplatin and bevacizumab followed by maintenance bevacizumab in patients with stage IIIB or IV nonsquamous non-small-cell lung cancer. J Clin Oncol. 2013;31:4349–57.
Seto T, Kato T, Nishio M, Goto K, Atagi S, Hosomi Y, Yamamoto N, Hida T, Maemondo M, Nakagawa K, et al. Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol. 2014;15:1236–44.
Soerensen MM, Ros W, Rodriguez-Ruiz ME, Robbrecht D, Rohrberg KS, Martin-Liberal J, Lassen UN, Bermejo IM, Lolkema MP, Tabernero J, et al: Safety, PK/PD, and anti-tumor activity of RO6874281, an engineered variant of interleukin-2 (IL-2v) targeted to tumor-associated fibroblasts via binding to fibroblast activation protein (FAP). In ASCO Annual Meeting. J Clin Oncol. 2018;36:e15155.
Larkin J, Ascierto PA, Dreno B, Atkinson V, Liszkay G, Maio M, Mandala M, Demidov L, Stroyakovskiy D, Thomas L, et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med. 2014;371:1867–76.
Eng C, Kim TW, Bendell J, Argiles G, Tebbutt NC, Di Bartolomeo M, Falcone A, Fakih M, Kozloff M, Segal NH, et al. Atezolizumab with or without cobimetinib versus regorafenib in previously treated metastatic colorectal cancer (IMblaze370): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2019;20:849–61.
Thomas M, Sadjadian P, Kollmeier J, Lowe J, Mattson P, Trout JR, Gargano M, Patchen ML, Walsh R, Beliveau M, et al. A randomized, open-label, multicenter, phase II study evaluating the efficacy and safety of BTH1677 (1,3 – 1,6 beta glucan; Imprime PGG) in combination with cetuximab and chemotherapy in patients with advanced non-small cell lung cancer. Invest New Drugs. 2017;35:345–58.
Engel-Riedel W, Lowe J, Mattson P, Richard Trout J, Huhn RD, Gargano M, Patchen ML, Walsh R, Trinh MM, Dupuis M, Schneller F. A randomized, controlled trial evaluating the efficacy and safety of BTH1677 in combination with bevacizumab, carboplatin, and paclitaxel in first-line treatment of advanced non-small cell lung cancer. J Immunother Cancer. 2018;6:16.
O’Day S, Borges VF, Chmielowski B, Rao R, Abu-Khalaf MM, Stopeck A, Nikolinakos P, Telli M, Xie B, Shaheen M, et al: IMPRIME 1: An open label, multicenter Ph 2 study combining Imprime PGG with pembrolizumab (pembro) in previously-treated, metastatic Triple Negative Breast Cancer (mTNBC). In ASCO Annual Meeting. 2019.
Naing A, Papadopoulos KP, Autio KA, Ott PA, Patel MR, Wong DJ, Falchook GS, Pant S, Whiteside M, Rasco DR, et al. Safety, Antitumor Activity, and Immune Activation of Pegylated Recombinant Human Interleukin-10 (AM0010) in Patients With Advanced Solid Tumors. J Clin Oncol. 2016;34:3562–9.
Naing A, Wong DJ, Infante JR, Korn WM, Aljumaily R, Papadopoulos KP, Autio KA, Pant S, Bauer TM, Drakaki A, et al. Pegilodecakin combined with pembrolizumab or nivolumab for patients with advanced solid tumours (IVY): a multicentre, multicohort, open-label, phase 1b trial. Lancet Oncol. 2019;20:1544–55.
Hidalgo M, Semenisty V, Bockorny B, Borazanci E, von Hoff DD, Feliu J, Ponz Sarvise M, Gutierrez Abad D, Peled A, Bohana-Kashtan O, et al: A multi-center phase iia trial to assess the safety and efficacy of BL-8040 (A CXCR4 inhibitor) in combination with pembrolizumab and chemotherapy in patients with metastatic pancreatic adenocarcinoma (PDAC). ESMO Immuno-Oncology Congress. Ann Oncol. 2019;30:910.
Vonderheide RH, Flaherty KT, Khalil M, Stumacher MS, Bajor DL, Hutnick NA, Sullivan P, Mahany JJ, Gallagher M, Kramer A, et al. Clinical activity and immune modulation in cancer patients treated with CP-870,893, a novel CD40 agonist monoclonal antibody. J Clin Oncol. 2007;25:876–83.
Beatty GL, Torigian DA, Chiorean EG, Saboury B, Brothers A, Alavi A, Troxel AB, Sun W, Teitelbaum UR, Vonderheide RH, O’Dwyer PJ. A phase I study of an agonist CD40 monoclonal antibody (CP-870,893) in combination with gemcitabine in patients with advanced pancreatic ductal adenocarcinoma. Clin Cancer Res. 2013;19:6286–95.
Bajor DL, Mick R, Riese MJ, Huang AC, Sullivan B, Richman LP, Torigian DA, George SM, Stelekati E, Chen F, et al. Long-term outcomes of a phase I study of agonist CD40 antibody and CTLA-4 blockade in patients with metastatic melanoma. Oncoimmunology. 2018;7:e1468956.
Nowak AK, Cook AM, McDonnell AM, Millward MJ, Creaney J, Francis RJ, Hasani A, Segal A, Musk AW, Turlach BA, et al. A phase 1b clinical trial of the CD40-activating antibody CP-870,893 in combination with cisplatin and pemetrexed in malignant pleural mesothelioma. Ann Oncol. 2015;26:2483–90.
Vonderheide RH, Burg JM, Mick R, Trosko JA, Li D, Shaik MN, Tolcher AW, Hamid O. Phase I study of the CD40 agonist antibody CP-870,893 combined with carboplatin and paclitaxel in patients with advanced solid tumors. Oncoimmunology. 2013;2:e23033.
Villalona-Calero MA, Lam E, Otterson GA, Zhao W, Timmons M, Subramaniam D, Hade EM, Gill GM, Coffey M, Selvaggi G, et al. Oncolytic reovirus in combination with chemotherapy in metastatic or recurrent non-small cell lung cancer patients with KRAS-activated tumors. Cancer. 2016;122:875–83.
Mahalingam D, Fountzilas C, Moseley J, Noronha N, Tran H, Chakrabarty R, Selvaggi G, Coffey M, Thompson B, Sarantopoulos J. A phase II study of REOLYSIN((R)) (pelareorep) in combination with carboplatin and paclitaxel for patients with advanced malignant melanoma. Cancer Chemother Pharmacol. 2017;79:697–703.
Noonan AM, Farren MR, Geyer SM, Huang Y, Tahiri S, Ahn D, Mikhail S, Ciombor KK, Pant S, Aparo S, et al. Randomized Phase 2 Trial of the Oncolytic Virus Pelareorep (Reolysin) in Upfront Treatment of Metastatic Pancreatic Adenocarcinoma. Mol Ther. 2016;24:1150–8.
Cohn DE, Sill MW, Walker JL, O’Malley D, Nagel CI, Rutledge TL, Bradley W, Richardson DL, Moxley KM, Aghajanian C. Randomized phase IIB evaluation of weekly paclitaxel versus weekly paclitaxel with oncolytic reovirus (Reolysin(R)) in recurrent ovarian, tubal, or peritoneal cancer: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol. 2017;146:477–83.
Mahalingam D, Fountzilas C, Moseley JL, Noronha N, Cheetham K, Dzugalo A, Nuovo A, Gutierrez A, Arora SP: A study of REOLYSIN in combination with pembrolizumab and chemotherapy in patients (pts) with relapsed metastatic adenocarcinoma of the pancreas (MAP). In ASCO Annual Meeting. J Clin Oncol. 2017;35(15):e15753.
Mahalingam D, Wilkinson GA, Eng KH, Fields P, Raber P, Moseley JL, Cheetham K, Coffey M, Nuovo G, Kalinski P, et al. Pembrolizumab in Combination with the Oncolytic Virus Pelareorep and Chemotherapy in Patients with Advanced Pancreatic Adenocarcinoma: A Phase Ib Study. Clin Cancer Res. 2020;26:71–81.
Sikic BI, Lakhani N, Patnaik A, Shah SA, Chandana SR, Rasco D, Colevas AD, O’Rourke T, Narayanan S, Papadopoulos K, et al. First-in-Human, First-in-Class Phase I Trial of the Anti-CD47 Antibody Hu5F9-G4 in Patients With Advanced Cancers. J Clin Oncol. 2019;37:946–53.
Fisher GA, Lakhani NJ, Eng C, Hecht JR, Bendell JC, Philip PA, O’Dwyer PJ, Johnson B, Kardosh A, Ippolito TM, et al: A phase Ib/II study of the anti-CD47 antibody magrolimab with cetuximab in solid tumor and colorectal cancer patients. In ASCO. 2020:114.
Hellerstedt BA, Vogelzang NJ, Kluger HM, Yasenchak CA, Aftab DT, Ramies DA, Gordon MS, Lara P Jr. Results of a Phase II placebo-controlled randomized discontinuation trial of cabozantinib in patients with non-small-cell lung carcinoma. Clin Lung Cancer. 2019;20:74–81 e71.
Neal JW, Dahlberg SE, Wakelee HA, Aisner SC, Bowden M, Huang Y, Carbone DP, Gerstner GJ, Lerner RE, Rubin JL, et al. Erlotinib, cabozantinib, or erlotinib plus cabozantinib as second-line or third-line treatment of patients with EGFR wild-type advanced non-small-cell lung cancer (ECOG-ACRIN 1512): a randomised, controlled, open-label, multicentre, phase 2 trial. Lancet Oncol. 2016;17:1661–71.
FDA approves nivolumab plus cabozantinib for advanced renal cell carcinoma https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-nivolumab-plus-cabozantinib-advanced-renal-cell-carcinoma.
Cecchini M, Modiano M, Braiteh F, Gardner OS, Gilbert HN, DiRenzo D, Seitz L, Walters MJ, Yin F, Woloski R, et al: Efficacy and Safety of AB928 Plus Modified FOLFOX-6 in Participants With Metastatic Colorectal Cancer: Initial Results at the Recommended Dose for Expansion (ARC-3). In AACR Annual Meeting. 2019.
Powderly J, Spira A, Gutierrez R, DiRenzo D, Udyavar A, Karakunnel J, Rieger A, Colabella J, Lai D, Yin F, et al. Phase 1 Evaluation of AB928, a Novel Dual Adenosine Receptor Antagonist, Combined With Chemotherapy or AB122 (anti-PD-1) in Patients (pts) With Advanced Malignancies. In ESMO Congress. Ann Oncol. 2019;(Supplement 5):V493.
Gonzalez-Martin A, Pothuri B, Vergote I, DePont Christensen R, Graybill W, Mirza MR, McCormick C, Lorusso D, Hoskins P, Freyer G, et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N Engl J Med. 2019;381:2391–402.
Moore KN, Secord AA, Geller MA, Miller DS, Cloven N, Fleming GF, Wahner Hendrickson AE, Azodi M, DiSilvestro P, Oza AM, et al. Niraparib monotherapy for late-line treatment of ovarian cancer (QUADRA): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2019;20:636–48.
Smith MR, Sandhu SK, Kelly WK, Scher HI, Efstathiou E, Lara P, Yu EV, George DJ, Chi KN, Summa J, et al: Phase II study of niraparib in patients with metastatic castration-resistant prostate cancer (mCRPC) and biallelic DNA-repair gene defects (DRD): Preliminary results of GALAHAD. In ASCO Annual Meeting. J Clin Oncol. 2019;37.
Vinayak S, Tolaney SM, Schwartzberg L, Mita M, McCann G, Tan AR, Wahner-Hendrickson AE, Forero A, Anders C, Wulf GM, et al. Open-label clinical trial of niraparib combined with pembrolizumab for treatment of advanced or metastatic triple-negative breast cancer. JAMA Oncol. 2019;5(8):1132–40.
Konstantinopoulos PA, Waggoner S, Vidal GA, Mita M, Moroney JW, Holloway R, Van Le L, Sachdev JC, Chapman-Davis E, Colon-Otero G, et al. Single-arm Phases 1 and 2 trial of niraparib in combination with pembrolizumab in patients with recurrent platinum-resistant ovarian carcinoma. JAMA Oncol. 2019.
Dijkgraaf EM, Santegoets SJ, Reyners AK, Goedemans R, Wouters MC, Kenter GG, van Erkel AR, van Poelgeest MI, Nijman HW, van der Hoeven JJ, et al. A phase I trial combining carboplatin/doxorubicin with tocilizumab, an anti-IL-6R monoclonal antibody, and interferon-alpha2b in patients with recurrent epithelial ovarian cancer. Ann Oncol. 2015;26:2141–9.
Desai J, Fakih M, Pedersen KS, Hong YS, Segal NH, Allen S, Bailey L, Lenain C, Lu D, Sayyed PZ, et al: Phase Ib/II open-label, randomized evaluation of efficacy and safety of atezolizumab plus isatuximab versus regorafenib in MORPHEUS-colorectal cancer. In ASCO. 2020:82.
Tarhini A. Immune-mediated adverse events associated with ipilimumab ctla-4 blockade therapy: the underlying mechanisms and clinical management. Scientifica (Cairo). 2013;2013:857519.
Michot JM, Bigenwald C, Champiat S, Collins M, Carbonnel F, Postel-Vinay S, Berdelou A, Varga A, Bahleda R, Hollebecque A, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer. 2016;54:139–48.
Magee DE, Hird AE, Klaassen Z, Sridhar SS, Nam RK, Wallis CJD, Kulkarni GS. Adverse event profile for immunotherapy agents compared with chemotherapy in solid organ tumors: a systematic review and meta-analysis of randomized clinical trials. Ann Oncol. 2020;31:50–60.
Scotte F, Ratta R, Beuzeboc P. Side effects of immunotherapy: a constant challenge for oncologists. Curr Opin Oncol. 2019;31:280–5.
Maher VE, Fernandes LL, Weinstock C, Tang S, Agarwal S, Brave M, Ning YM, Singh H, Suzman D, Xu J, et al: Analysis of the Association Between Adverse Events and Outcome in Patients Receiving a Programmed Death Protein 1 or Programmed Death Ligand 1 Antibody. J Clin Oncol. 2019;37(30):2730–7.
Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, Minenza E, Linardou H, Burgers S, Salman P, et al. Nivolumab plus Ipilimumab in Lung Cancer with a High Tumor Mutational Burden. N Engl J Med. 2018;378:2093–104.
Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, Khushalani NI, Lewis K, Lao CD, Postow MA, et al. Combined Nivolumab and Ipilimumab in Melanoma Metastatic to the Brain. N Engl J Med. 2018;379:722–30.
Johnson DB, Balko JM, Compton ML, Chalkias S, Gorham J, Xu Y, Hicks M, Puzanov I, Alexander MR, Bloomer TL, et al. Fulminant Myocarditis with Combination Immune Checkpoint Blockade. N Engl J Med. 2016;375:1749–55.
Mehta A, Gupta A, Hannallah F, Koshy T, Reimold S. Myocarditis as an immune-related adverse event with ipilimumab/nivolumab combination therapy for metastatic melanoma. Melanoma Res. 2016;26:319–20.
Rotte A. Combination of CTLA-4 and PD-1 blockers for treatment of cancer. J Exp Clin Cancer Res. 2019;38:255.
Haikerwal SJ, Hagekyriakou J, MacManus M, Martin OA, Haynes NM. Building immunity to cancer with radiation therapy. Cancer Lett. 2015;368:198–208.
Benitez JC, Remon J, Besse B. Current Panorama and Challenges for Neoadjuvant Cancer Immunotherapy. Clin Cancer Res. 2020;26:5068–77.
Acknowledgements
We thank Vantage Research contracted by Genentech, Inc., for assistance with collection of data inspiring this review.
Funding
This review was sponsored by F. Hoffmann-La Roche Ltd. The sponsor was involved in the design; the collection, analysis, and interpretation of the data; and the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
VL and CSS contributed equally and share first authorship. All authors assisted with writing and analysis, provided strategic input, and contributed to the review and revisions to the article. All authors reviewed or contributed to revisions of the manuscript. All authors approved the final manuscript and agree to be accountable for the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
VL and CSS are employees of Genentech, Inc and Roche stockholders. AR is an independent consultant who was contracted by Genentech Inc during the course of the review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table S1.
Immunotherapy combinations approved for cancer treatment. Supplementary Table S2. Ranking of drugs based on knowledge of MoA, relevance to immunotherapy and importance of indication. Details on the scoring scale is provided in the Table 2. Higher scores are better. Supplementary Table S3. Details of drugs selected in the final phase of screening. Supplementary Table S4. Safety of final phase drugs reported in NSCLC, SCLC, or melanoma.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lemaire, V., Shemesh, C.S. & Rotte, A. Pharmacology-based ranking of anti-cancer drugs to guide clinical development of cancer immunotherapy combinations. J Exp Clin Cancer Res 40, 311 (2021). https://doi.org/10.1186/s13046-021-02111-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13046-021-02111-5