Abstract
Background
The pro-oncogenic anterior gradient 2 (AGR2) is involved in tumor growth and drug resistance of breast cancer. Mechanisms that regulate expression of AGR2 still need to be elucidated.
Methods
In this study, expression levels of AGR2 and miR-135b-5p were analyzed in different breast cancer cell lines as well as in clinical breast cancer tissues. The in vitro and in vivo functional effect of AGR2 and miR-135b-5p were also investigated. A luciferase reporter assay was applied to confirm the interaction between miR-135b-5p and AGR2 mRNA.
Results
We identified AGR2 as a target of miR-135b-5p. Expression of AGR2 was up-regulated in doxorubicin-resistant breast cancer cells. AGR2 mediated doxorubicin-sensitivity of breast cancer cells both in vitro and in vivo. miR-135b-5p negatively regulated AGR2-expression of breast cancer cells increasing doxorubicin-sensitivity. However, miR-135b-5p was down-regulated in doxorubicin-resistant breast cancer cells as well as during treatment with doxorubicin, which might be a probable reason for over-expression of AGR2. Up-regulation of miR-135b-5p increased doxorubicin-sensitivity of breast cancer cells in vivo. In addition, levels of AGR2 negatively correlated with levels of miR-135b-5p in clinical breast cancer tissue samples.
Conclusion
Our results highlight the potential of miR-135b-5p as a target for treating AGR2-expressing breast cancer with doxorubicin-resistance.
Similar content being viewed by others
Background
Breast cancer is one of the most common malignant tumors worldwide [1, 2]. Although surgical treatments are curative for some early stage cases, adjuvant systemic therapies are important for improving survival of patients especially those who with advanced stage diseases [3]. Doxorubicin, a topoisomerase II inhibitor, is a backbone drug in most chemotherapeutic regimens [4]. However, intrinsic or acquired drug resistance to doxorubicin limited the efficacy of doxorubicin-based treatments [5, 6]. Mechanisms mediating drug resistance to doxorubicin still need to be elucidated.
The human anterior gradient 2 (AGR2), a member of protein disulphide isomerases (PDIs) family, regulates protein folding in endoplasmic reticulum and normal mammary gland development [7, 8]. Over-expression of AGR2 is involved in pathogenesis of breast cancer including growth, drug resistance and metastasis of tumors, which is associated with poor prognosis [9]. Intrinsic or acquired over-expression of AGR2 was shown to mediate resistance to hormone therapies in estrogen receptor (ER)-positive breast cancers [10]. AGR2 was also implied to mediate doxorubicin resistance in breast cancer cells [11]. These findings suggest that AGR2 is an important mediator of drug resistance in breast cancer. AGR2 was shown to be a target of ER, which regulates expression of AGR2 in both normal mammary gland and breast cancer [12, 13]. However, over-expression of AGR2 is not restricted to ER-positive breast cancer. High AGR2 expression could be observed in ER-negative breast cancers, while some ER-positive cases showed low levels of AGR2 suggesting that mechanisms other than ER might control expression of AGR2 in breast cancer [10].
MicroRNAs (miRNAs) are single strand non-coding RNAs which regulate expression of genes at post-transcriptional level through binding 3′-untranslated region (3′-UTR) of mRNA. Some reports had shown that decreased levels of miRNAs led to over-expression of specific oncogenes promoting pathogenesis of cancers [14, 15]. Aberrant levels of miRNAs were also recognized as predictive factors of drug resistance in breast cancer [16]. Based on the important roles of AGR2 and miRNAs in breast cancer, we interrogated how miRNAs regulate expression of AGR2 in breast cancer cells. In this study, we found AGR2 was up-regulated in doxorubicin-resistant breast cancer cells. miR-135b-5p negatively regulates expression of AGR2 which increased sensitivity to doxorubicin in breast cancer cells both in vitro and in vivo. Our finding is indicative for an important role of miR-135b-5p/AGR2 pathway in regulating doxorubicin-sensitivity of breast cancer cells.
Methods
Clinical breast cancer specimens
Twenty-eight breast cancer samples were collected at the Affiliated Hospital of Xuzhou Medical University between October 2017 and April 2018. Subject and disease related variables are shown in Table 1. All the patients have not being treated before resection.
Mice
BALB/c Nude mice were purchased from Vital River (Charles River, Beijing, China). Mice were bred in a special pathogen free room.
Cell culture
MCF-7 cells (ATCC HTB-22) were cultured in DMEM medium (Thermo Fisher Scientific, Waltham, MA, USA) supplied with 10% FBS (Biowest, Nuaillé, France), penicillin and streptomycin. MDA-MB-231 (ATCC HTB-26) cells were cultured in Leibovitz’s L-15 medium (Thermo Fisher Scientific) supplied with 10% FBS, penicillin and streptomycin. MDA-MB-231 cells were maintained without CO2 equilibration.
Doxorubicin-resistant MCF-7 cells (MCF-7/DOXR) were selected as previously described [17]. MCF-7 cells were sequentially exposed to increasing doses of doxorubicin (0.1, 0.5, 1.0, 2.0 and 5.0 μM). Cells were initially cultured in DMEM medium with 0.1 μM doxorubicin for 1 d, followed by culture with doxorubicin free DMEM medium for 4 d. Selection with the same concentration of doxorubicin was repeated twice before moving to selection with the next dose.
Reagents
Doxorubicin, paclitaxel, docetaxel and 4-hydroperoxy cyclophosphamide were purchased from ApexBio (Houston, TX, USA). Puromycin was purchased from Sigma-Aldrich (Shanghai, China).
Quantitative polymerase chain reaction (qPCR)
Relative expression level of AGR2 mRNA was detected using qPCR as described previously [18]. Total RNA was isolated using TRIzol reagent (Invitrogen, Thermo Fisher Scientific). cDNA was synthesized with a PrimeScript cDNA Synthesis Kit (Takara Bio Inc., Shiga, Japan) followed analysis with a LightCycler 480 SYBR Green I Master qRT-PCR kit (Roche, Mannheim, Germany). ACTB was used as a normalization gene. The following primers were synthesized from Invitrogen (Thermo Fisher Scientific, Shanghai, China): AGR2 (GTGTAGGAGAGGGCCACAAG and CGACTCACACAAGGCAGGT) and ACTB (GTTGTCGACGACGAGCG and GCACAGAGCCTCGCCTT).
For detecting expression levels of mature miRNAs, cDNA was synthesized from total RNA using a miScript II RT Kit (QIAGEN, Shanghai, China). qPCR was performed using a miScript SYBR Green PCR Kit (QIAGEN) with U6 as a normalization gene. The following primers were used: miR-342-3p (Forward: TCTCACACAGAAATCGCACCCGT), miR-217 (Forward: TACTGCATCAGGAACTGATTGGA), miR-135b-5p (Forward: TATGGCTTTTCATTCCTATGTGA), miR-194-5p (Forward: TGTAACAGCAACTCCATGTGGA), miR-543 (Forward: AAACATTCGCGGTGCACTTCTT), miR-24-3p (Forward: TGGCTCAGTTCAGCAGGAACAG), miR-377-3p (Forward: ATCACACAAAGGCAACTTTTGT), miR-3158-3p (Forward: AAGGGCTTCCTCTCTGCAGGAC), miR-216b-3p (Forward: ACACACTTACCCGTAGAGATTCTA), miR-124-5p (Forward: CGTGTTCACAGCGGACCTTGAT), miR-1267 (Forward: CCTGTTGAAGTGTAATCCCCA), miR-624-3p (Forward: CACAAGGTATTGGTATTACCT) and U6 (CTCGCTTCGGCAGCACA and AACGCTTCACGAATTTGCGT). The results were analyzed by using the method of comparison on –ΔΔct values. qPCR was performed on an LC480 cycler (Roche).
Western blot analysis
Proteins were extracted from cells or tissues using Cell Lysis Buffer (Cell Signaling Technology, Danvers, MA, USA). Western blot analyses were performed with the following antibodies: Cleaved Caspase-3 (Asp175), Mcl-1 (D2W9E), Bcl-2 (D17C4), Bcl-xL (54H6), Bim (C34C5), Bak (D4E4), Cyclin D1 (92G2), Cyclin E1 (D7T3U), CDK2 (78B2), CDK4 (D9G3E), CDK6 (D4S8S), AGR2 (D9V2F) and GAPDH (D16H11), all of which were purchased from Cell Signaling Technology.
Cell viability assay
Cell viability was detected using a Cell Counting Kit-8 (CCK-8) from DOJINDO (CK04, Tokyo, Japan). Briefly, cells were incubated with CCK-8 reagent for 1 h followed by reading optical density at 450 nm.
Short hairpin RNA (shRNA)-mediated knockdown of AGR2
Three pairs of human AGR2-specific shRNAs (AGR2-shRNA) were synthesized according to the human AGR2 gene sequence (NM_006408). An unrelated negative shRNA was used as control. All shRNAs were cloned to a pLVX-shRNA2-Puro lentiviral vector (Genecreate, Wuhan, China). Lentiviral shRNA particles were obtained by transfecting 293FT cells with the constructed lentiviral vector packed in a ViraPower HiPerform Lentiviral Expression System (Invitrogen, Thermo Fisher Scientific). MCF-7 cell line, stably expressing AGR2-shRNA, was established by transducing cells with lentiviral shRNA particles, followed by selection with puromycin. Our preliminary experiment identified one of the AGR2-shRNA as the most efficient one in silencing AGR2-expression.
Over-expression of AGR2
CDS fragment (528 bp) of human AGR2 (NM_006408) was synthesized and cloned to pCDH-CMV-MCS-EF1-GFP-Puro lentiviral vector (Genecreate). Lentiviral AGR2 particles were obtained as described above. MCF-7 and MDA-MB-231 cell lines, over-expressing AGR2, were established as described above. A blank vector was used as control.
Xenograft experiments
BALB/c Nude mice were anesthetized and inoculated subcutaneously with 5 × 106 gene modified MCF-7 cells. Mice were injected intraperitoneally (i.p.) with PBS or doxorubicin (5 mg/kg) once on day 12, 15 and 18 after cell inoculation. Tumor size was measured continuously. Tumor volume was calculated with the formula: Tumor volume (mm3) = length (mm) × width (mm) × width (mm) × 0.5. Tumors were collected on day 32 for histological analyses.
H&E staining and immunohistochemistry
Tissue slides were prepared from tumors collected from xenograft experiments. H&E staining was performed as previously described [19].
Immunohistochemistry was performed to detect expression of Ki-67 and cleaved caspase-3 in tumor tissues. Anti-Ki-67 and peroxidase-conjugated goat anti-rabbit IgG were from ZSGB-BIO (Beijing, China). Anti-cleaved caspase-3 (Asp175) was from Cell Signaling Technology. DAB substrate was used for visualization (ZSGB-BIO).
TUNEL assay
TUNEL assay was performed to detect apoptotic cells in tissue slides using a TUNEL Kit per manufacturer’s instructions (KGA702, KeyGEN BioTECH, Beijing, China).
β-Galactosidase staining
Senescence of cells was analyzed using a β-Galactosidase Staining Kit per manufacturer’s instructions (KGPAG001, KeyGEN BioTECH).
Prediction of miRNA target
Several candidate miRNAs were predicted and selected from literature [20] and miRNA databases (TargetScan and miRBase). All these candidate miRNAs had a potential targeting 3′-UTR of AGR2 mRNA (Additional file 1 Table S1).
Luciferase reporter assay
3′-UTR (1097 bp) of AGR2 mRNA was synthesized and cloned to pmirGLO Dual-Luciferase miRNA Target Expression Vector (Promega, Madison, WI, USA). A mutant AGR2 3′-UTR (1090 bp) luciferase vector, lacking the binding site AAGCCAT of miR-135b-5p, was also constructed. Luciferase vector and miRNA mimics (Genecreate) were co-transfected into MCF-7 cells using Attractene Transfection Reagent (QIAGEN). Twenty-four hours after transfection, firefly and renilla luciferase activities of cell lysate were analyzed by using a Dual-Luciferase Reporter Assay kit (Promega). Firefly luciferase is a reporter, and renilla luciferase is a normalizer.
Lentivirus mediated over-expression of miR-135b
Lentiviral particles, expressing a control miRNA or hsa-miR-135b double strand precursors, were obtained from Genechem (Shanghai, China). MCF-7 cell lines, stably expressing control miRNA or hsa-miR-135b, were established by transducing cells with lentiviral particles, followed by selection with puromycin.
RNA interference
ESR1-targeting small interfering RNAs (siRNA) (ESR1 siRNA-1: CCGGCAUUCUACAGGCCAA, ESR1 siRNA-2: GGAGAAUGUUGAAACACAA, ESR1 siRNA-3: GCUAGAGAUCCUGAUGAUU), synthesized from Genecreate (Wuhan, China), were transfected into MCF-7 cells using HiPerFect Transfection Reagent (QIAGEN). An irrelevant siRNA (Genecreate) was used as negative control.
Statistics
Data are presented as mean ± standard deviation (SD). Comparison of means was performed with unpaired Student t test or one-way ANOVA test followed by Bonferroni post-tests. Correlations were analyzed using Pearson correlation test. Value of p < 0.05 was considered statistically significant.
Results
Knockdown of AGR2 increased doxorubicin-sensitivity of breast cancer cells in association with enhanced apoptosis
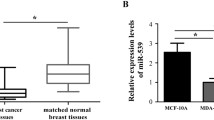
To assess the correlation between expression of AGR2 and doxorubicin-sensitivity in breast cancer cells, we analyzed expression of AGR2 mRNA in MDA-MB-231 and MCF-7 cells as well as doxorubicin-resistant MCF-7/DOXR cells. MCF-7 cells expressed higher levels of AGR2 than MDA-MB-231 cells at both mRNA and protein levels. Expression of AGR2 protein was not observed in MDA-MB-231 cells, although we could detect low level of AGR2 mRNA in this cell line (Fig. 1a and b). Interestingly, expression of AGR2 was up-regulated in MCF-7/DOXR cells as compared with MCF-7 cells (Fig. 1a and b). IC50 of doxorubicin in MDA-MB-231, MCF-7 and MCF-7/DOXR cells was 48.16 nM, 147.10 nM and 1.87 μM, respectively (Fig. 1c).
AGR2 correlated with doxorubicin-resistance in breast cancer cells. a-b Total RNA and protein were extracted from MDA-MB-231, MCF-7 and MCF-7/DOXR cells. a qPCR and b western blot were applied to analyze mRNA and protein levels of AGR2. c Cells were treated with gradient doses of doxorubicin for 48 h. MDA-MB-231: 1, 10, 30, 50, 100, 200, 400 nM; MCF-7: 10, 50, 100, 150, 200, 400, 800 nM; MCF-7/DOXR: 0.01, 0.1, 0.5, 1.0, 5.0, 20, 50 μM. Cell viability was measured by CCK-8 assay (n = 6). Viability of untreated cells was set as 100%. Experiment was repeated twice. Expression levels of mRNA represent fold changes. Data are shown as mean ± SD, compared using one-way ANOVA test. *, p < 0.05; MCF-7/DOXR, doxorubicin-resistant MCF-7 cells
Next, we examined if AGR2 had an impact on doxorubicin-sensitivity in breast cancer cells, through modulating expression of AGR2 with AGR2-shRNA or AGR2-over-expression vectors. Knockdown and over-expression of AGR2 increased and decreased sensitivity to doxorubicin in MCF-7 cells, respectively (Fig. 2a and b). Since MDA-MB-231 cells did not expression AGR2 protein, we only constructed over-expression model in this cell line and found that forced expression of AGR2 increased resistance to doxorubicin (Fig. 2c). Impact of AGR2 on apoptosis was further analyzed. Knockdown of AGR2 increased level of cleaved caspase-3 in MCF-7 cells treated by doxorubicin. Knockdown of AGR2 increased level of pro-apoptotic Bak and Bim, but decreased level of anti-apoptotic Mcl-1 (Fig. 2d). These findings indicated that AGR2 mediated drug resistance to doxorubicin in breast cancer cells.
AGR2 mediated doxorubicin-sensitivity of breast cancer cells in vitro. a MCF-7 cells were stably transduced with a control shRNA vector or an AGR2-shRNA vector. b MCF-7 and c MDA-MB-231 cells were stably transduced with a control vector or an AGR2 over-expression vector. a-c Cells were analyzed for expression of AGR2 protein (left panel). Cells were analyzed for cell viability (middle panel), and viability of control was set as 100%. Cells were treated with doxorubicin for 48 h (right panel), followed by measuring for cell viability (n = 6), and viability of untreated cells was set as 100%. d MCF-7 cells, stably expressing a control shRNA vector or an AGR2-shRNA vector, were treated with doxorubicin (100 nM) for 48 h. Protein levels were detected by western blotting with indicated antibodies. Experiment was repeated three times. Data are shown as mean ± SD, compared using unpaired t test.*, p < 0.05; n.s., no significance
In addition, we also tested the effect of AGR2 in treatment with other chemotherapeutics including paclitaxel, docetaxel and cyclophosphamide in MCF-7 cells. Knockdown of AGR2 increased sensitivity to paclitaxel and docetaxel. However, over-expression of AGR2 did not decrease sensitivity to paclitaxel and docetaxel. In addition, modulating expression of AGR2 had no impact on drug sensitivity to cyclophosphamide (Additional file 1: Figure S1).
Silence of AGR2 enhanced doxorubicin-sensitivity of MCF-7 cells in vivo
To assess the impact of AGR2 on doxorubicin-sensitivity in vivo, we applied a xenograft model in nude mice. AGR2-shRNA MCF-7 cells showed a similar growth rate as control-shRNA MCF-7 cells (Fig. 3a and b). After being treated by doxorubicin, AGR2-shRNA tumors grew more slowly and were smaller than control-shRNA tumors (Fig. 3a and b). Proliferation and apoptosis in these tumors were further analyzed. AGR2-shRNA tumors had less Ki-67-positive cells than control-shRNA tumors after being treated by doxorubicin, whereas AGR2-shRNA tumors had more apoptotic cells and higher level of cleaved caspase-3 than control-shRNA tumors after being treated by doxorubicin (Fig. 3c-e). These findings indicated that knockdown of AGR2 increased doxorubicin-sensitivity of MCF-7 cells in vivo in association with increased apoptosis.
Silence of AGR2 enhanced doxorubicin-sensitivity of MCF-7 cells in vivo. MCF-7 cells, stably transduced with a control shRNA vector or an AGR2-shRNA vector, were inoculated subcutaneously into BALB/c Nude mice at a dose of 5 × 106 per mouse (n = 4 in each group). Mice were injected intraperitoneally with PBS or doxorubicin (5 mg/kg) once on day 12, 15 and 18 after cell inoculation (indicated by arrows in panel A). a Tumor size was measured continuously. b-e On day 32, tumors were collected from mice followed by morphological (b) and histological analyses (c). d-e Immunohistochemistry was performed to detect expression of Ki-67 and cleaved caspase-3 in tumor tissues. TUNEL assay was applied to dectec apoptosis. Scale bar in (c and d): 500 μm. e Percent of Ki-67-positive cells, apoptotic cells and cleaved caspase-3-positive cells were counted. Experiment was repeated twice. Data are shown as mean ± SD, compared using one-way ANOVA test. *, p < 0.05; n.s., no significance; Doxo, doxorubicin
Decreased levels of miR-135b-5p correlated with up-regulation of AGR2 in breast cancer cells
Given that miRNAs are potent regulators of AGR2, we predicted several candidate miRNAs targeting AGR2 mRNA. As we found MCF-7 cells (ER-positive) expressed higher level of AGR2 than MDA-MB-231 (ER-negative) did, we compared levels of candidate miRNAs in these cell lines. ER-expression status is correlated with several miRNAs including miR-342-3p, miR-299-3p, miR-217, miR-190, miR-135b-5p and miR-218 [20]. We found that knockdown of ER-expression increased level of miR-135b-5p but decreased level of miR-342-3p in MCF-7 cells (Additional file 1: Figure S2), so we predicted if those miRNAs would bind 3′-UTR of AGR2 mRNA by searching databases on www.mirbase.org and www.targetscan.org. miR-342-3p, miR-217 and miR-135b-5p were chosen as candidate miRNAs due to their binding potential with 3′-UTR of AGR2 mRNA. We also picked several other high ranked candidate miRNAs including miR-194-5p, miR-543, miR-24-3p, miR-377-3p, miR-3158-3p, miR-216b-3p, miR-124-5p, miR-1267 and miR-624-3p (Additional file 1: Table S1). Expression levels of the latter five miRNAs were undetectable in these cells (Fig. 4a). Comparing with MDA-MB-231 cells, MCF-7 cells expressed lower levels of miR-135b-5p and miR-194-5p. On the contrary, MCF-7 cells had higher levels of miR-342-3p and miR-217 than MDA-MB-231 cells (Fig. 4a). Expression of miR-135b-5p was down-regulated in MCF-7/DOXR cells as compared with MCF-7 cells (Fig. 4a).
Decreased levels of miR-135b-5p correlated with up-regulation of AGR2 in breast cancer cells. a cDNA was synthesized from total RNA extracted from MDA-MB-231, MCF-7 and MCF-7/DOXR cells. qPCR was applied to measure levels of mature miRNAs with U6 as a normalization gene. b Correlation between levels of AGR2 mRNA and miRNAs were analyzed using Pearson correlation test. c-e MCF-7 and MDA-MB-231 cells were treated with gradient doses of doxorubicin for 48 h. Expression levels of AGR2 mRNA and miRNAs were measured by qPCR (n = 3). Experiment was repeated twice. Expression levels of RNAs represent fold changes. Data are shown as mean ± SD and are compared using unpaired t test or one-way ANOVA test. *, p < 0.05 compared with MDA-MB-231 cells; #, p < 0.05 compared with untreated cells. 0 nM represents untreated cells
Levels of AGR2 mRNA showed negative correlation with levels of miR-135b-5p and miR-194-5p in these breast cancer cells (Fig. 4b). Since reduced expression of miRNAs lead to up-regulation of target genes [15], we further analyzed correlation between miR-135b-5p or miR-194-5p and AGR2. Short term exposure to doxorubicin induced up-regulation of AGR2 mRNA both in MCF-7 and MDA-MB-231 cells. MCF-7 cells expressed higher levels of AGR2 mRNA than MDA-MB-231 cells after doxorubicin treatment (Fig. 4c). Doxorubicin reduced levels of miR-135b-5p both in MCF-7 and MDA-MB-231 cells (Fig. 4d). Doxorubicin reduced levels of miR-194-5p of MCF-7 cells, but increased levels of miR-194-5p of MDA-MB-231 cells (Fig. 4e). These findings indicated that down-regulation of miR-135b-5p correlated with up-regulation of AGR2 in breast cancer cells.
miR-135b-5p negatively regulated expression of AGR2 and increased doxorubicin-sensitivity of MCF-7 cells
Through transfecting MCF-7 cells with miRNAs mimics, we found that miR-135b-5p mimic reduced levels of AGR2 mRNA, whereas miR-194-5p had no impact on levels of AGR2 mRNA (Fig. 5a). Next, we analyzed if miR-135b-5p targeted 3′-UTR of AGR2 mRNA. As MCF-7 cells expressed a relative low level of background miR-135b-5p, MCF-7 cells were used as transfection host of a luciferase reporter vector expressing 3′-UTR of AGR2 mRNA. Co-transfection with miR-135b-5p mimic suppressed luciferase activity, compared with a negative control miRNA. We also constructed a mutant AGR2 3′-UTR luciferase reporter vector by deleting the binding site of miR-135b-5p, and found that miR-135b-5p mimic failed to suppress luciferase activity of cells transfected with the mutant vector (Fig. 5b). Doxorubicin-treatment reduced levels of miR-135b-5p of MCF-7 cells (Fig. 4d). To test if doxorubicin induced down-regulation of miR-135b-5p is a probable reason for over-expression of AGR2, cells were transfected with miR-135b-5p mimic before treatment with doxorubicin. Doxorubicin induced up-regulation of AGR2 level was reduced by miR-135b-5p mimic (Fig. 5c).
miR-135b-5p negatively regulated expression of AGR2 and increased doxorubicin-sensitivity of MCF-7 cells in vitro. a MCF-7 cells were transfected with mimics of a control miRNA, miR-135b-5p or miR-194-5p. Twenty-four hours after transfection, level of AGR2 mRNA was measured by qPCR (n = 3). b AGR2 3′-UTR (1097 bp) and a mutant AGR2 3′-UTR (1090 bp) fragments were synthesized and cloned to pmirGLO Dual-Luciferase miRNA Target Expression Vector. Luciferase vector and miR-135b-5p mimic were co-transfected into MCF-7 cells. Twenty-four hours after transfection, firefly and renilla luciferase activities of cell lysate were analyzed. Luciferase activity was expressed as ratio of Firefly/Renilla. c MCF-7 cells were transfected with mimics of a control miRNA or miR-135b-5p, followed by treatment with doxorubicin (100 nM) for 48 h. AGR2-expression was detected using western blot. d-e MCF-7 cells were stably transduced with lentivirual vector expressing double strand precursors of a control miRNA or miR-135b. d AGR2-expression was detected using western blot. e Cell viability was measured by CCK-8 assay (n = 6). f Cells were treated with doxorubicin for 48 h followed by measuring for cell viability (n = 6). Experiment was repeated three times. Expression levels of mRNA represent fold changes. Data are shown as mean ± SD and are compared using unpaired t test or one-way ANOVA test. *, p < 0.05; n.s., no significance
Furthermore, we up-regulated expression of miR-135b-5p in MCF-7 cells by transducing cells with a lentivirus vector expressing double strand miR-135b precursor. Transduction of miR-135b vecter reduced expression of AGR2 (Fig. 5d). Transduction of miR-135b vecter had no impact on viability of cells in the absence of doxorubicin (Fig. 5e). Forced expression of miR-135b-5p in MCF-7 cells increased doxorubicin-sensitivity as compared with negative control (Fig. 5f). Next, we tested the impact of miR-135b-5p on doxorubicin-sensitivity in the murine xenograft model. The miR-135b vecter-transduced MCF-7 cells showed a similar growth rate as control (Fig. 6a and b). Transduction of miR-135b vecter reduced level of AGR2 in the tumors (Fig. 6c). After being treated by doxorubicin, miR-135b tumors grew more slowly (Fig. 6a and b) and had less Ki-67-positive cells (Fig. 6d-f) than control. These findings confirmed that miR-135b-5p negatively regulated expression of AGR2 through targeting 3′-UTR and increased doxorubicin-sensitivity of MCF-7 cells.
miR-135b-5p increased doxorubicin-sensitivity of MCF-7 cells in vivo. MCF-7 cells, stably transduced with lentivirual vector expressing double strand precursors of a control miRNA or miR-135b, were inoculated subcutaneously into BALB/c Nude mice at a dose of 5 × 106 per mouse (n = 4 in each group). Mice were injected intraperitoneally with PBS or doxorubicin (5 mg/kg) once on day 12, 15 and 18 after cell inoculation (indicated by arrows in panel A). a Tumor size was measured continuously. b-f On day 32, tumors were collected from mice. c Proteins extracted from tumors were analyzed by western blotting with indicated antibodies. d Histological analysis was performed using H&E staining. e Immunohistochemistry was performed to detect Ki-67-expression in tumor tissues. Scale bar in (d and e): 500 μm. f Percent of Ki-67-positive cells was counted. Experiment was repeated twice. Data are shown as mean ± SD, compared using one-way ANOVA test. *, p < 0.05; n.s., no significance
Levels of miR-135b-5p negatively correlated with levels of AGR2 in clinical breast cancer samples
Clinical breast cancer samples were collected and subjected to analysis for expression of AGR2 protein and miR-135b-5p. ER-positive tumors (n = 20) expressed higher levels of AGR2 than ER-negative ones (n = 8). On the contrary, ER-positive tumors showed lower levels of miR-135b-5p comparing with ER-negative ones (Fig. 7a and b). Although expression of AGR2 was reported to be regulated by ER, we observed that expression of AGR2 are at low levels or undetectable in some ER-positive samples. In addition, ER-negative sample #6, #7 and #8 expressed low or middle levels of AGR2 (Fig. 7a). Interestingly, we observed a negative correlation between levels of AGR2 and miR-135b-5p in these samples (Fig. 7c). These findings indicated that level of miR-135b-5p might be a predictive marker for AGR2-expression in breast cancer.
Levels of miR-135b-5p negatively correlated with levels of AGR2 in clinical breast cancer tissues. Twenty-eight breast cancer tissue samples were collected from patients. Total RNA and protein were extracted from tissues. a AGR2-expression was detected using western blot. Intensities of AGR2-bands were analyzed with ImageJ software, and were normalized to GAPDH. b qPCR was applied to measure levels of miR-135b-5p with U6 as a normalization gene. Expression levels of RNA represent fold changes. Data are shown as mean ± SD and are compared using unpaired t test. c Correlation between levels of AGR2 protein and miR-135b-5p was analyzed using Pearson correlation test
Discussion
AGR2 is a protein disulphide isomerase regulating protein folding in endoplasmic reticulum which is important for survival of tumor cells, as many tumor cells produce abundant proteins which would cause proteotoxic stress to cells in case of insufficient or inappropriate protein-folding [7, 21]. Importantly, AGR2 was implied to mediate drug resistance in breast cancer [7, 10, 11]. Expression level of AGR2 correlated with doxorubicin-sensitivity of breast cancer cells in our study. Up-regulation and down-regulation of AGR2 decreased and increased doxorubicin-sensitivity, respectively (Fig. 2), and this effect is associated with apoptotic process. Knockdown of AGR2 increased apoptosis and reduced proliferation of the xenograft tumors (Fig. 3). AGR2 was shown to induce expression of cyclin D1 in breast cancer cells [22]. Cyclin D1 is a critical driver of tumorigenesis of breast cancer [23, 24]. On the other hand, dysregulation of cyclin D1 is a marker of senescence, which counteracts tumor genesis [25, 26]. However, exposure to doxorubicin had no impact on senescence or expression of cyclin D1 in our study (Additional file 1: Figure S3). Li and colleague had shown that AGR2 stabilized hypoxia inducible factor-1α enhancing hypoxia-induced doxorubicin resistance in breast cancer cells [11]. Over-expression of AGR2 alone seems insufficient for tumorigenesis of breast cancer [27], but rather can contribute to drug resistance. Consistently, our results showed that knockdown or over-expression of AGR2 in MCF-7 and MDA-MB-231 cells had no significant impact on cell viability in the absence of doxorubicin. AGR2 mediated drug resistance seems more related with topoisomerase II inhibitor. Knockdown of AGR2 increased sensitivity to paclitaxel and docetaxel. However, over-expression of AGR2 had no impact on sensitivity to these drugs in MCF-7 cells (Additional file 1: Figure S1). AGR2 also mediates resistance to hormone therapy in breast cancer [9]. All these suggest that manipulating expression of AGR2 might counteract drug-resistance in breast cancer, especially in those who with high level of AGR2.
Others reported that level of AGR2 positively correlated with expression of ER in breast cancer. ER binds directly to AGR2 promoter to activate transcription of AGR2 in both cell lines and tumor samples of breast cancers [12, 13]. AKT signaling pathway was also reported to induce AGR2 expression [28]. Our data on clinical breast cancer samples also showed that ER-positive tumors expressed higher levels of AGR2 than ER-negative ones (Fig. 7). MCF-7 and MDA-MB-231 cells are ER-positive and ER-negative cells, respectively. Thus, expression of ARG2 in these two cell lines might have correlation with expression of ER (Fig. 1). Some clinical data showed that over-expression of AGR2 can also be found in ER-negative breast cancers [10], which indicates that other mechanisms might also participate in regulating AGR2-expression. Interestingly, we found expression of AGR2 could be further regulated by miR-135b-5p.
miRNAs play important roles in multiple cellular processes such as proliferation and differentiation [29, 30]. Prognostic miRNAs, such as miR-342 and miR-30e, were reported in breast cancer and some miRNAs were proposed as predictive markers of drug resistance [16, 31, 32]. However, miRNAs-mediated regulation of AGR2 is still unclear in breast cancer. Since AGR2 mediates doxorubicin-resistance, we further focused on miRNAs-mediated regulation of AGR2. Among these candidate miRNAs, down-regulation of miR-135b-5p was in parallel with up-regulation of AGR2 in breast cancer cells. Doxorubicin-treatment induced up-regulation of AGR2 in association with down-regulation of miR-135b-5p (Fig. 4). miR-135b-5p negatively regulated expression of AGR2 through targeting 3′-UTR confirmed that AGR2 is a target gene of miR-135b-5p in breast cancer cells (Fig. 5). As expected, miR-135b-5p reduced expression of AGR2 and increased doxorubicin-sensitivity of MCF-7 cells both in vitro and in vivo (Figs. 5 and 6). Doxorubicin treatment induced down-regulation of miR-135b-5p is a probable reason for over-expression of AGR2 in breast cancer (Figs. 4 and 5), which is indicative for a treatment related drug resistance. Intriguingly, we also observed a negative correlation between levels of AGR2 and miR-135b-5p in clinical breast cancer samples (Fig. 7). Level of miR-194-5p also negatively correlated with level of AGR2 in breast cancer cell lines. Interestingly, doxorubicin treatment increased level of miR-194-5p in MDA-MB-231 cells (Fig. 4). Expression of miR-194-5p is regulated by some upstream regulators such as GATA2 and non-coding RNAs [33, 34]. The difference on levels of miR-194-5p in MCF-7 and MDA-MB-231 might have some relations with ER or those upstream regulators of miR-194-5p. In addition, transfection with miR-194-5p did not down-regulate expression of AGR2 (Fig. 5). miR-194-5p might not be a direct regulator of AGR2 in breast cancers. Thus, in addition to ER-dependant mechanism, we identified that miR-135b-5p is another regulator of AGR2 in breast cancer.
Others reported that increased levels of miR-342-3p and miR-217 positively correlated with expression of ER in breast cancer [20]. Consistently, we showed MCF-7 had higher levels of miR-342-3p and miR-217 than MDA-MB-231. Their relations with AGR2 were reported by others recently. miR-342-3p targets AGR2 and down-regulation of miR-342-3p is associated with over-expression of AGR2 in non-small cell lung cancer [35]. Down-regulation of miR-217 was associated with over-expression of AGR2 in chronic myelogenous leukemia cells [36]. Doxorubicin-treatment had no impact on level of miR-342-3p or miR-217 in breast cancer cells (data not shown). Since levels of miR-342-3p and miR-217 positively correlated with level of AGR2 in breast cancer cells, we deduce that miR-135b-5p is a more dominant regulator of AGR2-expression in breast cancer, comparing with miR-342-3p and miR-217. miR-1291 was shown to regulate expression of AGR2 in pancreatic cancer cell [37]. The findings suggest that miRNAs mediated regulation on AGR2 differs in different type of cancers.
Conclusion
In conclusion, AGR2 is a target of miR-135b-5p. Decreased levels of miR-135b-5p correlated with over-expression of AGR2 in breast cancer cells during doxorubicin treatment. Up-regulation of miR-135b-5p suppressed expression of AGR2 increasing doxorubicin-sensitivity of breast cancer cells. Our results highlight the potential of miR-135b-5p as a target for treating AGR2-expressing breast cancer with doxorubicin-resistance.
Abbreviations
- AGR2:
-
Anterior gradient 2
- DOXR:
-
Doxorubicin resistant
- ER:
-
Estrogen receptor
- miRNAs:
-
microRNAs
- PDIs:
-
Protein disulphide isomerases
- shRNA:
-
Short hairpin RNA
- UTR:
-
Untranslated region
References
Turner NC, Neven P, Loibl S, Andre F. Advances in the treatment of advanced oestrogen-receptor-positive breast cancer. Lancet. 2017;389:2403–14.
Carey L, Winer E, Viale G, Cameron D, Gianni L. Triple-negative breast cancer: disease entity or title of convenience? Nat Rev Clin Oncol. 2010;7:683–92.
Trudeau M, Charbonneau F, Gelmon K, et al. Selection of adjuvant chemotherapy for treatment of node-positive breast cancer. Lancet Oncol. 2005;6:886–98.
Loi S, Sirtaine N, Piette F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 2013;31:860–7.
Yu P, Yu H, Guo C, et al. Reversal of doxorubicin resistance in breast cancer by mitochondria-targeted pH-responsive micelles. Acta Biomater. 2015;14:115–24.
Wijdeven RH, Pang B, van der Zanden SY, et al. Genome-wide identification and characterization of novel factors conferring resistance to topoisomerase II poisons in Cancer. Cancer Res. 2015;75:4176–87.
Brychtova V, Mohtar A, Vojtesek B, Hupp TR. Mechanisms of anterior gradient-2 regulation and function in cancer. Semin Cancer Biol. 2015;33:16–24.
Verma S, Salmans ML, Geyfman M, et al. The estrogen-responsive Agr2 gene regulates mammary epithelial proliferation and facilitates lobuloalveolar development. Dev Biol. 2012;369:249–60.
Chevet E, Fessart D, Delom F, et al. Emerging roles for the pro-oncogenic anterior gradient-2 in cancer development. Oncogene. 2013;32:2499–509.
Salmans ML, Zhao F, Andersen B. The estrogen-regulated anterior gradient 2 (AGR2) protein in breast cancer: a potential drug target and biomarker. Breast Cancer Res. 2013;15:204.
Li Z, Zhu Q, Hu L, Chen H, Wu Z, Li D. Anterior gradient 2 is a binding stabilizer of hypoxia inducible factor-1alpha that enhances CoCl2 -induced doxorubicin resistance in breast cancer cells. Cancer Sci. 2015;106:1041–9.
Fullwood MJ, Liu MH, Pan YF, et al. An oestrogen-receptor-alpha-bound human chromatin interactome. Nature. 2009;462:58–64.
Ross-Innes CS, Stark R, Teschendorff AE, et al. Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature. 2012;481:389–93.
Gandellini P, Doldi V, Zaffaroni N. microRNAs as players and signals in the metastatic cascade: implications for the development of novel anti-metastatic therapies. Semin Cancer Biol. 2017;44:132–40.
Lu J, Tang L, Xu Y, et al. Mir-1287 suppresses the proliferation, invasion, and migration in hepatocellular carcinoma by targeting PIK3R3. J Cell Biochem. 2018;119(11):9229–38.
Nicolini A, Ferrari P, Duffy MJ. Prognostic and predictive biomarkers in breast cancer: past, present and future. Semin Cancer Biol. 2018;52(Pt 1):56–73.
Liu Z, Balasubramanian V, Bhat C, et al. Quercetin-based modified porous silicon nanoparticles for enhanced inhibition of doxorubicin-resistant cancer cells. Adv Healthc Mater. 2017;6(3). https://doi.org/10.1002/adhm.201601009. Epub 2016 Dec 12.
Pan B, Wang X, Kojima S, et al. The fifth epidermal growth factor-like region of Thrombomodulin alleviates murine graft-versus-host disease in a G-protein coupled receptor 15 dependent manner. Biol Blood Marrow Transplant. 2017;23:746–56.
Pan B, Wang X, Kojima S, et al. The fifth epidermal growth factor like region of thrombomodulin alleviates LPS-induced sepsis through interacting with GPR15. Thromb Haemost. 2017;117:570–9.
Lowery AJ, Miller N, Devaney A, et al. MicroRNA signatures predict oestrogen receptor, progesterone receptor and HER2/neu receptor status in breast cancer. Breast Cancer Res. 2009;11:R27.
Higa A, Mulot A, Delom F, et al. Role of pro-oncogenic protein disulfide isomerase (PDI) family member anterior gradient 2 (AGR2) in the control of endoplasmic reticulum homeostasis. J Biol Chem. 2011;286:44855–68.
Vanderlaag KE, Hudak S, Bald L, et al. Anterior gradient-2 plays a critical role in breast cancer cell growth and survival by modulating cyclin D1, estrogen receptor-alpha and survivin. Breast Cancer Res. 2010;12:R32.
Casimiro MC, Di Sante G, Di Rocco A, et al. Cyclin D1 restrains oncogene-induced autophagy by regulating the AMPK-LKB1 signaling Axis. Cancer Res. 2017;77:3391–405.
Wander SA, Mayer EL, Burstein HJ. Blocking the cycle: cyclin-dependent kinase 4/6 inhibitors in metastatic, hormone receptor-positive breast cancer. J Clin Oncol. 2017;35:2866–70.
Rajarajacholan UK, Thalappilly S, Riabowol K. The ING1a tumor suppressor regulates endocytosis to induce cellular senescence via the Rb-E2F pathway. PLoS Biol. 2013;11:e1001502.
Qie S, Diehl JA. Cyclin D1, cancer progression, and opportunities in cancer treatment. J Mol Med (Berl). 2016;94:1313–26.
Liu D, Rudland PS, Sibson DR, Platt-Higgins A, Barraclough R. Human homologue of cement gland protein, a novel metastasis inducer associated with breast carcinomas. Cancer Res. 2005;65:3796–805.
Hrstka R, Murray E, Brychtova V, Fabian P, Hupp TR, Vojtesek B. Identification of an AKT-dependent signalling pathway that mediates tamoxifen-dependent induction of the pro-metastatic protein anterior gradient-2. Cancer Lett. 2013;333:187–93.
Li J, Sen GL. Post-transcriptional mechanisms regulating epidermal stem and progenitor cell self-renewal and differentiation. J Invest Dermatol. 2016;136:746–52.
Shenoy A, Blelloch RH. Regulation of microRNA function in somatic stem cell proliferation and differentiation. Nat Rev Mol Cell Biol. 2014;15:565–76.
Goh JN, Loo SY, Datta A, et al. microRNAs in breast cancer: regulatory roles governing the hallmarks of cancer. Biol Rev Camb Philos Soc. 2016;91:409–28.
Li HY, Liang JL, Kuo YL, et al. miR-105/93-3p promotes chemoresistance and circulating miR-105/93-3p acts as a diagnostic biomarker for triple negative breast cancer. Breast Cancer Res. 2017;19:133.
Das R, Gregory PA, Fernandes RC, et al. MicroRNA-194 promotes prostate cancer metastasis by inhibiting SOCS2. Cancer Res. 2017;77:1021–34.
Ye Y, Zhang F, Chen Q, Huang Z, Li M. LncRNA MALAT1 modified progression of clear cell kidney carcinoma (KIRC) by regulation of miR-194-5p/ACVR2B signaling. Mol Carcinog. 2019;58(2):279–92.
Xue X, Fei X, Hou W, Zhang Y, Liu L, Hu R. miR-342-3p suppresses cell proliferation and migration by targeting AGR2 in non-small cell lung cancer. Cancer Lett. 2018;412:170–8.
Pan B, Yang J, Wang X, Xu K, Ikezoe T. miR-217 sensitizes chronic myelogenous leukemia cells to tyrosine kinase inhibitors by targeting pro-oncogenic anterior gradient 2. Exp Hematol. 2018;68:80–88.
Tu MJ, Pan YZ, Qiu JX, Kim EJ, Yu AM. MicroRNA-1291 targets the FOXA2-AGR2 pathway to suppress pancreatic cancer cell proliferation and tumorigenesis. Oncotarget. 2016;7:45547–61.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from National Natural Science Foundation of China (No. 81372479 and No. 81671584).
Availability of data and materials
All data generated or analysed during this study are included in this article.
Author information
Authors and Affiliations
Contributions
YW contributed to the concept and design, analyzed data and revised the manuscript. YZ performed experiments, analyzed data, wrote the manuscript and helped to design experiments. FX and FZ performed experiments and analyzed data (xenograft model, cell culture, constructing vector and PCR). YC collected clinical samples. QW and HL advised on experimental design and provided experimental expertise. YZ, FX and FZ contributed equally to this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures regarding animal care and experiments were approved by the Experimental Animal Care and Use Committee of Xuzhou Medical University. Collection and analysis of clinical samples were approved by the Institutional Ethic Committee of the Affiliated Hospital of Xuzhou Medical University.
Consent for publication
Informed consents were received from all patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Candidate miRNAs with AGR2-targeting potential. Figure S1. Knockdown of AGR2 increased sensitivity to paclitaxel and docetaxel in MCF-7 cells. Figure S2. Knockdown of estrogen receptor 1 (ESR1) increased level of miR-135b-5p but decreased level of miR-342-3p in MCF-7 cells. Figure S3. Long term exposure to doxorubicin had no impact on senescence. (DOCX 1106 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, Y., Xia, F., Zhang, F. et al. miR-135b-5p enhances doxorubicin-sensitivity of breast cancer cells through targeting anterior gradient 2. J Exp Clin Cancer Res 38, 26 (2019). https://doi.org/10.1186/s13046-019-1024-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13046-019-1024-3