Abstract
Background
Identification of a gene expression signature in primary breast tumors that could classify patients by lymph node status would allow patients to avoid the morbidities of surgical disruption of the lymph nodes. Attempts to identify such a signature have, to date, been unsuccessful. Because breast tumor subtypes have unique molecular characteristics and different sites of metastasis, molecular signatures for lymph node involvement may vary by subtype.
Methods
Gene expression data was generated from HG U133A 2.0 arrays for 135 node positive and 210 node negative primary breast tumors. Intrinsic subtype was assigned using the BreastPRS. Differential gene expression analysis was performed using one-way ANOVA using lymph node status as the variable with a False-discovery rate <0.05, to define significance.
Results
Luminal A tumors were most common (51%) followed by basal-like (27%), HER2-enriched (14%) luminal B (7%) and normal-like (1%). Basal-like and luminal A tumors were less likely to have metastatic lymph nodes (35% and 37%, respectively) compared to luminal B or HER2-enriched (52% and 51%, respectively). No differentially expressed genes associated with lymph node status were detected when all tumors were considered together or within each subtype.
Conclusions
Gene expression patterns from the primary tumor are not able to stratify patients by lymph node status. Although the primary breast tumor may influence tumor cell dissemination, once metastatic cells enter the lymphatics, it is likely that characteristics of the lymph node microenvironment, such as establishment of a pre-metastatic niche and release of pro-survival factors, determine which cells are able to colonize. The inability to utilize molecular profiles from the primary tumor to determine lymph node status suggest that other avenues of investigation, such as how systemic factors including diminished immune response or genetic susceptibility contribute to metastasis, may be critical in the development of tools for non-surgical assessment of lymph node status with a corresponding reduction in downstream sequelae associated with disruption of the lymphatics.
Similar content being viewed by others
Background
Surgical treatment for patients with breast cancer is constantly changing [1]. The radical mastectomy, which removed the breast, underlying chest muscle and axillary lymph nodes has been supplanted by less aggressive approaches such as lumpectomy, and complete removal of the axillary lymph nodes has been replaced by sentinel lymph node biopsy (SLNB) [2],[3]. Recent results from the ACOSOG Z0011 trial demonstrate that SLNB performed without follow up axillary dissection is reasonable for patients with early-stage, lymph node positive breast cancer [4].
Although SLNB is associated with lower morbidities, surgical disruption of the lymphatic system can result in serious side effects, including numbness, decreased mobility and lymphedema, significantly impacting the quality of life of breast cancer patients. For example, lymphedema can result in pain, decreased functional ability, cosmetic deformities and psychological stress [5] and is estimated to affect 10-20% of breast cancer survivors [6]. In addition, SLNB is associated with a false negative rate of 8-10% [7],[8]. Development of a signature that effectively discriminates patients by lymph node status could stratify patients into those needing surgical evaluation of the lymph nodes for prognostic purposes from those at low-risk of metastasis who may be spared possible serious side effects as well as identify those patients misdiagnosed with negative lymph node status after SLNB, who may in fact benefit from more aggressive treatment.
Although a few studies have identified genes or proteins expressed in primary tumors that differ in expression levels based on lymph node status [9]-[14], other studies failed to validate these results and/or found that molecular profiling of primary tumors cannot effectively classify patients by lymph node status [15]-[18]. Inability to identify a signature of lymph node metastasis may be attributable to heterogeneity within primary breast tumors associated with intrinsic subtypes. Breast tumors can be classified into subtypes, including luminal A, luminal B, HER2 positive and basal-like, based on different patterns of gene expression. Molecular heterogeneity within tumor subtypes may also preclude the identification of a single signature of metastasis. Breast tumors can be classified by their intrinsic subtypes, including luminal A, luminal B, HER2 positive and basal-like, based on different patterns of gene expression [19],[20]. These subtypes have been associated with differences in preferential sites of metastasis; for example, bone is the most common site of metastasis for luminal A tumors while brain is most common for basal-like tumors [21]. Because breast tumor intrinsic subtypes have unique molecular characteristics and different sites of metastasis, gene expression patterns for lymph node involvement may vary by subtype, thus gene expression data from primary breast tumors with and without lymph node metastases was evaluated by intrinsic subtype to identify subtype-specific molecular signatures associated with lymph node status.
Methods
For inclusion in the Clinical Breast Care Project, all patients met the following eligibility criteria: 1) adult over the age of 18 years, 2) mentally competent and willing to provide informed consent, and 3) presenting to the breast centers with evidence of possible breast cancer. Tissue and blood samples were collected with approval from the Walter Reed National Military Medical Center Human Use Committee and Institutional Review Board. All subjects voluntarily agreed to participate and gave written informed consent.
Positive lymph node status was defined as having micrometastatic (>0.2 mm but ≤ 2.0 mm) or metastatic (>2.0 mm) lymph node tumors; negative lymph node status was defined as lymph nodes with isolated tumor cells (≤0.2 mm) or no detectable tumor cells. Patients who underwent neoadjuvant therapy and those diagnosed with stage IV breast cancer were not included in this study. Tissue was collected from patients undergoing surgical procedures, including lumpectomy or mastectomy. Within 5–15 minutes of surgical removal, breast tissue was taken on crushed, wet ice to the pathology laboratory where a licensed pathologist or pathologists’ assistant performed routine pathology analyses. Two to five serial sections (8 μm thick) were cut, mounted, stained and laser microdissected as previously described [15]. Slide preparation, staining and cutting were performed within 15 minutes to preserve RNA integrity. RNA for microarray analysis was processed as previously described [22]. Labeled RNA was hybridized to HG U133A 2.0 arrays (Affymetrix, Santa Clara, CA) according to manufacturer’s protocols.
Intrinsic breast subtype was assigned to each tumor specimen using the BreastPRS™ (Signal Genetics, New York, NY) as previously described [23],[24]. Samples were classified as one of five subtypes: luminal A, luminal B, HER2-enriched, basal-like and normal-like. To determine whether genes were differentially expressed by lymph node status by subtype, gene expression data was imported into Partek® Genomics Suite 6.6 (Partek, Inc, St Louis, MO) and analyzed as previously described [15], using a false discovery rate (FDR) < 0.05 to define significance. Additional analyses were performed using an unadjusted P-value to identify any genes differentially expressed between primary breast tumors without and without lymph node metastasis.
Results
Patient and tumor characteristics
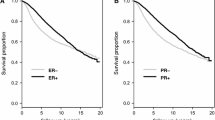
Gene expression data was available for 345 tumors: 210 lymph node negative and 135 lymph node positive. Ethnicity, age at diagnosis and tumor grade did not differ significantly by lymph node status, however, patients diagnosed with positive lymph nodes (7%) were significantly more likely (P < 0.05) to die of disease than those with negative lymph node status (2%) at diagnosis. The most common intrinsic subtype was luminal A (51%), followed by basal-like (27%), HER2-enriched (13%), luminal B (7%) and normal-like (1%) (Figure 1). When stratified by lymph node status, subtype distribution was significantly different, with higher frequencies of HER2-enriched and luminal B subtypes in the lymph node positive group.
Distribution of intrinsic subtypes by lymph node status. Subtype frequencies were significantly different (P < 0.05) between groups, with lymph node negative tumors (top chart) having a higher frequency of luminal A tumors while node positive tumors (bottom chart) had higher frequencies of luminal B and HER2-enriched tumors. Frequencies of normal-like tumors were <1.0% for each group.
Gene expression differences in primary breast tumors by lymph node status
Principal component analysis (PCA) did not cluster the tumors based on lymph node status. Gene expression analysis of all tumors failed to identify any differentially expressed genes using FDR < 0.05, with any fold difference. To determine whether any genes could classify tumors by lymph node status, an unadjusted P-value was used; seven differentially expressed genes were identified, however, these genes were not able to effectively cluster primary tumor specimens (Figure 2). When data were evaluated by size of metastasis (isolated tumor cells, micrometastsis or metastasis) or number of positive nodes (1–3, 4–9 or ≥10) no significant differences were detected.
Heat map of node negative and node positive breast tumors. Seven genes (DKK1, IGJ, SCGB1D2, SERPINA1, TFF1, TFF3 and TMSB15A) were found to be differentially expressed using an unadjusted P-value <0.05 that does not correct for multiple testing. These seven genes were unable to effectively classify tumors by lymph node status. Tumors from node negative patients are represented by light blue squares and node positive patients represented by yellow squares.
Subtype-specific gene expression differences by lymph node status
Although PCA did not cluster samples by lymph node status, it was effective in clustering samples by subtype, underscoring the significantly different molecular characteristics between tumor subtypes. To determine whether a signature(s) of lymph node metastasis was detectable within individual subtypes, data was evaluated for luminal A (n = 177), luminal B (n = 25), HER2-enriched (n = 47) and basal-like (n = 94) lymph node negative and lymph node positive tumors; normal-like tumors (n = 2) were not evaluated. No significant gene expression differences were detected within any of the subtypes.
Discussion
Identification of a gene expression signature predictive of lymph node metastasis would further the evolution of clinical treatment for breast cancer by allowing for the determination of nodal status based on molecular characteristics of the primary breast tumor, allowing women to be spared surgical disruption of the axillary lymph nodes. In addition, a molecular signature would provide a tool to determine lymph node status in those patients not eligible for SLNB and as well as to reduce the false negative rate of SLNB. No differentially expressed genes were identified in node negative compared to node positive tumors either when primary breast tumors were considered as a whole, or within the four intrinsic subtypes luminal A, luminal B, HER2-enriched or basal-like.
The inability to identify a signature of lymph node metastasis underscores the complexity of the metastatic process. Although thousands of cells are disseminated from a primary breast tumor, growth of metastatic tumors requires tumor cells to successfully reach the secondary site, escape senescence and survive and proliferate within a foreign environment [25],[26]. For example, gene expression patterns in primary breast tumors differ significantly from matched metastatic lymph node tumors, with genes expressed in the primary tumor favoring cellular dissemination, while those in metastatic lymph node tumors are involved in cellular proliferation and survival [27]. In addition, tumor cells are not self-reliant but rather depend on a complex interaction with the microenvironment [28]. For example, many signatures of poor prognosis or of metastasis include the expression of stromal genes. Recent data from our laboratory demonstrated that gene expression profiles differed in lymph nodes harboring metastatic breast tumors when compared to negative lymph node tissues and that these differences created an immunotolerant environment promoting cellular proliferation and the mesenchymal-epithelial transition, all of which favors tumor growth [29]. Thus, consideration of only the tumor epithelial component may fail to capture the full metastatic potential of a primary tumor.
In addition, tumor heterogeneity may confound the ability to identify a molecular signature of lymph node metastasis. Primary tumors demonstrate significant heterogeneity at the molecular level include expression of prognostic biomarkers such as ER, PR and HER2, chromosomal alterations and DNA mutations [30]-[34]. Evaluation of protein expression within primary tumors using technologies such as reverse phase protein arrays also demonstrates intratumoral heterogeneity with a mean coefficient of variation of 31% within primary tumors [35]. In this study, laser microdissection was utilized to enrich for tumor epithelial cells and reduce contamination by stromal cells; however, tumor regions isolated for this study may contain cells with heterogeneous molecular profiles and/or different levels of metastatic potential, thus diluting the ability to detect gene expression differences associated with metastasis to the lymph nodes.
In addition to the contribution of the microenvironment to successful metastatic colonization, systemic factors, such as inherent host susceptibility may affect the metastatic process. Decreased immunosurveillance and an increased pro-inflammatory response were characteristics of lymph nodes harboring metastatic breast tumors [29]; what remains unknown is whether these alterations in immune response are local or systemic. Studies in mouse models suggest that there is a genetic susceptibility to metastasis as out-crossing of a highly metastatic mouse to a variety of inbred mouse strains resulted in significant variability in the propensity to metastasize [36]; follow-up studies in humans validated the roles of SIPA1 and RRP1B as metastasis susceptibility genes [37]. Thus, the ability to successfully metastasize may include systemic as well as tumor/stromal factors.
This study does have limitations. Although gene expression data was available from 345 primary breast tumors, only 25 (7%) were of the luminal B subtype. Thus, a gene signature for lymph node metastasis within the primary tumor may be present, although such a signature was undetected within the other subtypes. In addition, only RNA was evaluated in this study: DNA alterations or protein profiles may be effective in discriminating primary tumors by lymph node status. For example, copy number alterations and were detected at significantly higher levels and GSTP1 and RAR-beta2 were more likely to be hypermethylated in primary tumors with metastatic lymph nodes compared to those without [38],[39], although neither of these genes demonstrated differential expression within our dataset. In addition, protein signatures based on differentially expressed protein peaks or proteins have been identified [40],[41], although both protein signatures included pathological characteristics, such as tumor size, in their predictive model that are known to be predictive of lymph node metastasis, thus it is not clear whether these signatures have independent prognostic value.
Conclusions
Significant differences in gene expression levels are not detectable in lymph node positive compared to lymph node negative tumors, even within intrinsic subtypes. The inability to identify a signature of metastasis reflects the complexities underlying the metastatic process, in which tumor cells grow and survive only in collaboration with the microenvironment and against a pro-metastatic genetic background. Because molecular profiles from primary tumors cannot predict nodal status, other avenues of investigation, such as how diminished immune response or genetic susceptibility contribute to metastasis, must be pursued to further the evolution of clinical care of breast cancer patients.
References
Sakorafas GH, Safioleas M: Breast cancer surgery: an historical narrative. Part II. 18th and 19th centuries. Eur J Cancer Care. 2010, 19: 6-29. 10.1111/j.1365-2354.2008.01060.x.
Giuliano AE: Sentinel lymphadenectomy in primary breast carcinoma: an alternative to routine axillary dissection. J Surg Oncol. 1996, 62: 75-77. 10.1002/(SICI)1096-9098(199606)62:2<75::AID-JSO1>3.0.CO;2-N.
Fisher B: From Halsted to prevention and beyond: advances in the management of breast cancer during the twentieth century. Eur J Cancer. 1999, 35: 1963-1973. 10.1016/S0959-8049(99)00217-8.
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch M, Saha S, Hunt KK, Morrow M, Ballman K: Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Annals Surg. 2010, 252: 426-433.
Andersen L, Hojris I, Erlandsen M, Andersen J: Treatment of breast-cancer-related- lymphedema with or without manual lymphatic drainage. A randomized study. Acta Oncol. 2000, 39: 399-405. 10.1080/028418600750013186.
Sakorafas GH, Peros G, Cataliotti L, Vlastos G: Lymphedema following axillary lymph node dissection for breast cancer. Surg Oncol. 2006, 15: 153-165. 10.1016/j.suronc.2006.11.003.
Newman EA, Newman LA: Lymphatic mapping techniques and sentinel lymph node biopsy in breast cancer. Surg Clin North Am. 2007, 87: 353-364. 10.1016/j.suc.2007.01.013.
Wilke LG, McCall LM, Posther KE, Whitworth PW, Reintgen DS, Leitch AM, Gabram SG, Lucci A, Cox CE, Hunt KK, Herndon JE, Giuliano AE: Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol. 2006, 13: 491-500. 10.1245/ASO.2006.05.013.
Abba MC, Sun H, Hawkins KA, Drake JA, Hu Y, Nunez MI, Gaddis S, Shi T, Horvath S, Sahin A, Aldaz CM: Breast cancer molecular signatures as determined by SAGE: correlation with lymph node status. Mol Cancer Res. 2007, 5: 881-889. 10.1158/1541-7786.MCR-07-0055.
Bertucci F, Houlgatte R, Benziane A, Granjeaud S, Adelaide J, Tagett R, Loriod B, Jacquemier J, Viens P, Jordan B, Birnbaum D, Nguyen C: Gene expression profiling of primary breast carcinomas using arrays of candidate genes. Hum Mol Genet. 2000, 9: 2981-2991. 10.1093/hmg/9.20.2981.
Cao YW, Li WQ, Wan GX, Li YX, Du XM, Li YC, Li F: Correlation and prognostic value of SIRT1 and Notch1 signaling in breast cancer. J Exp Clin Cancer Res. 2014, 33: 97-10.1186/s13046-014-0097-2.
Huang E, Cheng SH, Dressman H, Pittman J, Tsou MH, Horng CF, Bild A, Iversen ES, Liao M, Chen CM, West M, Nevins JR, Huang AT: Gene expression predictors of breast cancer outcomes. Lancet. 2003, 361: 1590-1596. 10.1016/S0140-6736(03)13308-9.
Yang Y, Zhang Y, Wu Q, Cui X, Lin Z, Liu S, Chen L: Clinical implications of high NQO1 expression in breast cancers. J Exp Clin Cancer Res. 2014, 33: 14-10.1186/1756-9966-33-14.
Zhang X, Min J, Wang Y, Li Y, Li H, Liu Q, Liang X, Mu P, Li H: RABEX-5 plays an oncogenic role in breast cancer by activating MMP-9 pathway. J Exp Clin Cancer Res. 2013, 32: 52-10.1186/1756-9966-32-52.
Ellsworth RE, Field LA, Love B, Kane JL, Hooke JA, Shriver CD: Differential gene expression in primary breast tumors associated with lymph node metastasis. Int J Breast Cancer. 2011, 2011: 142763-10.4061/2011/142763.
Lu X, Lu X, Wang ZC, Iglehart JD, Zhang W, Richardson AL: Predicting features of breast cancer with gene expression patterns. Breast Cancer R. 2008, 108: 191-201. 10.1007/s10549-007-9596-6.
van de Vijer MJ, He YD, van't Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ, Parrish M, Atsma D, Witteveen A, Glas A, Delahaye L, van der Velde T, Bartelink H, Rodenhuis S, Rutgers ET, Friend SH, Bernards R: A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002, 347: 1999-2009. 10.1056/NEJMoa021967.
Weigelt B, Wessels LFA, Bosma AJ, Nuyten DSA, He YD, Dai H, Peterse JL, van't Veer LJ: No common denominator for breast cancer lymph node metastasis. Br J Cancer. 2005, 93: 924-932. 10.1038/sj.bjc.6602794.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lønning PE, Børresen-Dale AL, Brown PO, Botstein D: Molecular portraits of human breast tumours. Nature. 2000, 406: 747-752. 10.1038/35021093.
Sorlie T, Perou CM, Tibshirania R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, Brown PO, Botstein D, Lønning PE, Børresen-Dale AL: Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001, 98: 10869-10874. 10.1073/pnas.191367098.
Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, Nielsen TO, Gelmon K: Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010, 28: 3271-3277. 10.1200/JCO.2009.25.9820.
Field LA, Deyarmin B, Shriver CD, Ellsworth DL, Ellsworth RE: Improved accuracy of gene expression signatures after laser-microdissection. In Laser Capture Microdissection: Methods and Protocols. 2nd edition. Edited by Murray GI. New York: Humana Press; 2011.
Deyarmin B, Kane JL, Valente AL, van Laar R, Gallagher C, Shriver CD, Ellsworth RE: Effect of ASCO/CAP guidelines for determining ER status on molecular subtype. Ann Surg Oncol. 2013, 20: 87-93. 10.1245/s10434-012-2588-8.
van Laar R: Design and multiseries validation of a web-based gene expression assay for predicting breast cancer recurrence and patient survival. J Mol Diagn. 2011, 13: 297-304. 10.1016/j.jmoldx.2010.12.003.
Bidard F-C, Pierga J-Y, Vincent-Salomon A, Poupon M-F: A "class action" against the microenvironment: do cancer cells cooperate in metastasis?. Cancer Metastasis Rev. 2008, 27: 5-10. 10.1007/s10555-007-9103-x.
Nguyen DX, Massagué J: Genetic determinants of cancer metastasis. Nature Rev Genet. 2007, 8: 341-352. 10.1038/nrg2101.
Ellsworth RE, Seebach J, Field LA, Heckman C, Kane JL, Hooke JA, Love B, Shriver CD: A gene expression signature that defines breast cancer metastases. Clin Exp Metastasis. 2009, 26: 205-213. 10.1007/s10585-008-9232-9.
Cook LM, Hurst DR, Welch DR: Metastasis suppressors and the tumor microenvironment. Semin Cancer Biol. 2011, 21: 113-122. 10.1016/j.semcancer.2010.12.005.
Valente AL, Kane JL, Ellsworth DL, Shriver CD, Ellsworth RE: Molecular response of the axillary lymph node microenvironment to metastatic colonization. Clin Exp Metastasis. 2014, 31: 565-572. 10.1007/s10585-014-9650-9.
Nassar A, Radhakrishnan A, Cabrero IA, Cotsonis GA, Cohen C: Intratumoral heterogeneity of immunohistochemical marker expression in breast carcinoma: a tissue microarray-based study. Appl Immunohistochem Mol Morphol. 2010, 18: 433-441.
Navin N, Krasnitz A, Rodgers L, Cook K, Meth J, Kendall J, Riggs M, Eberling Y, Troge J, Grubor V, Levy D, Lundin P, Månér S, Zetterberg A, Hicks J, Wigler M: Inferring tumor progression from genomic heterogeneity. Genome Res. 2010, 20: 68-80. 10.1101/gr.099622.109.
Navin N, Kendall J, Troge J, Andrews P, Rodgers L, McIndoo J, Cook K, Stepansky A, Levy D, Esposito D, Muthuswamy L, Krasnitz A, McCombie WR, Hicks J, Wigler M: Tumour evolution inferred by single-cell sequencing. Nature. 2011, 472: 90-94. 10.1038/nature09807.
Davis BW, Zava DT, Locher GW, Goldhirsch A, Hartmann WH: Receptor heterogeneity of human breast cancer as measured by multiple intratumoral assays of estrogen and progesterone receptor. Eur J Cancer Clin Oncol. 1984, 20: 375-382. 10.1016/0277-5379(84)90084-1.
Pertschuk LP, Axiotis CA, Feldman JG, Kim YD, Karavattayhayyil SJ, Braithwaite L: Marked intratumoral heterogeneity of the proto-oncogene Her-2/neu determined by three different detection systems. Breast J. 1999, 5: 369-374. 10.1046/j.1524-4741.1999.97088.x.
Malinowsky K, Raychaudhuri M, Buchner T, Thulke S, Wolff C, Hofler H, Becker KF, Avril S: Common protein biomarkers assessed by reverse phase protein arrays show considerable intratumoral heterogeneity in breast cancer tissues. Plos ONE. 2012, 7: e40285-10.1371/journal.pone.0040285.
Hunter KW: The intersection of inheritance and metastasis: the role and implication of germline polymorphism in tumor dissemination. Cell Cycle. 2005, 4: 1719-1721. 10.4161/cc.4.12.2258.
Hsieh FC, Look MP, Sieuwerts AM, Foekens JA, Hunter KW: Distinct inherited metastasis susceptibility exists for different breast cancer subtypes: a prognosis study. Breast Cancer Res. 2009, 11: R75-10.1186/bcr2412.
Desouki MM, Liao S, Huang H, Conroy J, Nowak NJ, Shepherd L, Gaile DP, Geradts J: Identification of metastasis-associated breast cancer genes using a high-resolution whole genome profiling approach. J Cancer Res Clin Oncol. 2011, 137: 795-809. 10.1007/s00432-010-0937-1.
Shinozaki M, Hoon DS, Giuliano AE, Hansen NM, Wang HJ, Turner R, Taback B: Distinct hypermethylation profile of primary breast cancer is associated with sentinel lymph node metastasis. Clin Cancer Res. 2005, 11: 2156-2162. 10.1158/1078-0432.CCR-04-1810.
Nakagawa T, Huang SK, Martinez SR, Tran AN, Elashoff D, Ye X, Turner RR, Giuliano AE, Hoon DS: Proteomic profiling of primary breast cancer predicts axillary lymph node metastasis. Cancer Res. 2006, 66: 11825-11830. 10.1158/0008-5472.CAN-06-2337.
Sauer G, Schneiderhan-Marra N, Kazmaier C, Hutzel K, Koretz K, Muche R, Kreienberg R, Joos T, Deissler H: Prediction of nodal involvement in breast cancer based on multiparametric protein analyses from preoperative core needle biopsies of the primary lesion. Clin Cancer Res. 2008, 14: 3345-3353. 10.1158/1078-0432.CCR-07-4802.
Acknowledgements
The opinion and assertions contained herein are the private views of the authors and are not to be construed as official or as representing the views of the Department of the Army or the Department of Defense.
Funding source
This research was supported by a grant from the Office of the Congressionally Directed Medical Research Programs (Department of Defense Breast Cancer Research Program W81XWH-11-2-0135).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived and designed the experiments: CDS, REE. Analyzed the data: REE. Wrote the first draft of the manuscript: REE. Contributed to the writing of the manuscript: CDS, MTH. Agree with manuscript results and conclusions: CDS, MTH, REE. Jointly developed the structure and arguments for the paper: CDS, MTH, REE. Made critical revisions and approved final version: CDS, MTH, REE. All authors reviewed and approved of the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shriver, C.D., Hueman, M.T. & Ellsworth, R.E. Molecular signatures of lymph node status by intrinsic subtype: gene expression analysis of primary breast tumors from patients with and without metastatic lymph nodes. J Exp Clin Cancer Res 33, 116 (2014). https://doi.org/10.1186/s13046-014-0116-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13046-014-0116-3