Abstract
Background
The World Health Organization has defined a list of adverse events of special interest (AESI) for safety surveillance of vaccines. AESI have not been adequately assessed following COVID-19 vaccination in patients with cancer contributing to vaccine hesitancy in this population. We aimed to evaluate the association between BNT162b2 and CoronaVac vaccines and the risk of AESI in adults with active cancer or a history of cancer.
Patients and methods
We conducted a territory-wide cohort study using electronic health records managed by the Hong Kong Hospital Authority and vaccination records provided by the Department of Health. Patients with a cancer diagnosis between January 1, 2018, and September 30, 2021, were included and stratified into two cohorts: active cancer and history of cancer. Within each cohort, patients who received two doses of BNT162b2 or CoronaVac were 1:1 matched to unvaccinated patients using the propensity score. Cox proportional hazards regression was used to estimate hazard ratios (HR) and 95% confidence intervals (CIs) for AESI 28 days after the second vaccine dose.
Results
A total of 74,878 patients with cancer were included (vaccinated: 25,789 [34%]; unvaccinated: 49,089 [66%]). Among patients with active cancer, the incidence of AESI was 0.31 and 1.02 per 10,000 person-days with BNT162b2 versus unvaccinated patients and 0.13 and 0.88 per 10,000 person-days with CoronaVac versus unvaccinated patients. Among patients with history of cancer, the incidence was 0.55 and 0.89 per 10,000 person-days with BNT162b2 versus unvaccinated patients and 0.42 and 0.93 per 10,000 person-days with CoronaVac versus unvaccinated patients. Neither vaccine was associated with a higher risk of AESI for patients with active cancer (BNT162b2: HR 0.30, 95% CI 0.08–1.09; CoronaVac: 0.14, 95% CI 0.02–1.18) or patients with history of cancer (BNT162b2: 0.62, 95% CI 0.30–1.28; CoronaVac: 0.45, 95% CI 0.21–1.00).
Conclusions
In this territory-wide cohort study of patients with cancer, the incidence of AESI following vaccination with two doses of either BNT162b2 or CoronaVac vaccines was low. The findings of this study can reassure clinicians and patients with cancer about the overall safety of BNT162b2 and CoronaVac in patients with cancer, which could increase the COVID-19 vaccination rate in this vulnerable group of patients.
Similar content being viewed by others
Introduction
Public health agencies recommend that patients with cancer should be prioritized for COVID-19 vaccination [1,2,3]. Currently, the safety of COVID-19 vaccines remains a concern, especially among the elderly and immunocompromised patients such as patients with cancer [4]. This has led to lower rates of vaccine uptake in patients with cancer in some regions including Hong Kong [5,6,7]. However, the available observational studies of BNT162b2 (mRNA, Pfizer-BioNTech) and CoronaVac (inactivated, Sinovac) vaccines in patients with cancer have only assessed common adverse events, for example headache and fever; have small sample sizes and are therefore unable to detect uncommon or rare adverse events of special interest (AESI); and do not have suitable between-individual comparisons, since they either have no comparator group or use a comparator group of healthy adults without cancer [8,9,10,11,12,13,14,15]. Furthermore, most patients with cancer were excluded from pivotal clinical trials of BNT162b2 and CoronaVac as their cancer treatments may suppress or impair the immune system [16,17,18]. Our study aimed to describe and assess the risk of AESI, as defined by the World Health Organization, among patients with active cancer and a history of cancer who received vaccination with BNT162b2 or CoronaVac.
Methods
Data sources
This study used electronic health records provided by the Hospital Authority and linked vaccination records provided by the Department of Health in Hong Kong. The linked records have been previously used to evaluate the safety of COVID-19 vaccines [19,20,21,22,23]. Diagnosis records were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes (Additional file 1: Table S1), and prescription records were identified using British National Formulary (BNF) codes (Additional file 1: Table S2).
Study population
Patients with a cancer diagnosis record between January 1, 2018, and September 30, 2021, were identified. Since patients with cancer have a weaker immune response after COVID-19 vaccination, AESI outcomes were only evaluated following the second dose of the vaccine [24]. The index date was defined as the date of the second vaccine dose for patients who were vaccinated with either BNT162b2 or CoronaVac. For unvaccinated patients, the pseudo index date was selected from a corresponding vaccine recipient matched on age and sex. Patients younger than 18 years, hospitalized within 30 days before vaccination, or diagnosed with cancer on or after the first dose of vaccination were excluded. Patients who received only the first dose of the vaccine were also excluded. The study population was stratified into two mutually exclusive cohorts: patients with active cancer and patients with a history of cancer (Fig. 1). Active cancer patients were defined as those who had undergone any active cancer treatment or had a diagnosis of metastasis in the last 6 months before their first vaccine dose [25]. The remaining patients were considered as the history of cancer cohort.
Outcomes
The primary outcome of interest in this study was the incidence of 28-day AESI, defined by the World Health Organization as a list of important vaccine safety surveillance events. The list includes conditions such as acute respiratory distress syndrome, acute kidney injury, myocarditis, and thrombocytopenia (Additional file 1: Table S1) [26]. The secondary outcome was 28-day all-cause mortality. Patients were followed from the index date until a diagnosis of the outcome, death, 28 days after the index date, or the end of study period (September 30, 2021), whichever occurred first.
Statistical analysis
Baseline patient characteristics were presented as means (standard deviation) for continuous variables and frequencies (percentages) for categorical variables. To reduce confounding arising from differences in baseline characteristics between vaccinated and unvaccinated patients, propensity score (PS) matching was performed for each type of vaccine (both in active cancer and in history of cancer cohorts). Confounders included in the PS estimation included age, sex, smoking, obesity, index date, history of COVID-19 (history of positive PCR test), latest levels of white blood cells and neutrophils before vaccination, hospitalization, accident and emergency attendance, cancer type and site, comorbidities, and concomitant medication use (Additional file 1: Tables S3, S4). Patients who received BNT162b2 vaccine and unvaccinated patients were matched on a 1:1 ratio using nearest neighbor algorithm with a caliper of 0.01. The same matching procedure was performed for patients who received the CoronaVac vaccine. A standardized mean difference (SMD) of < 0.1 was considered acceptable.
The association of AESI with either BNT162b2 or CoronaVac vaccine among patients with cancer was estimated using Cox proportional hazards regression. The results were reported as hazard ratios (HR) with 95% confidence intervals (CIs). Subgroup analyses were performed on different age-groups, sex, and cancer types. Individuals who experienced severe adverse effects after the first dose would less likely accept the second dose, which could potentially introduce bias in the current two-dose analysis. Hence, a post hoc analysis was conducted to compare the cumulative incidence rate of AESI between patients who received one dose only and unvaccinated patients; chi-square test with a significance level of 0.05 was reported.
R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analyses. The analyses were conducted by WK and cross-checked independently by JJPS and XY for quality assurance.
Results
We identified 90,822 patients with a cancer diagnosis between January 1, 2018, and September 30, 2021. After applying the exclusion criteria, 74,878 patients (25,789 active cancer cohort and 49,089 history of cancer cohort) were included (Fig. 1). After 1:1 PS matching, 15,054 patients with active cancer (4175 BNT162b2; 3352 CoronaVac; 7527 unvaccinated) and 35,870 patients with a history of cancer (9006 BNT162b2; 8929 CoronaVac; 17,935 unvaccinated) were included (Additional file 1: Tables S3, S4). All SMDs of the variables were < 0.1.
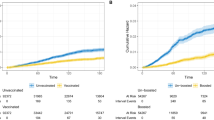
In the active cancer cohort, the incidence of AESI was 0.31 and 1.02 per 10,000 person-days for patients receiving BNT162b2 and matched unvaccinated patients, respectively; 0.13 and 0.88 per 10,000 person-days for patients receiving CoronaVac vaccine and matched unvaccinated patients, respectively (Table 1, Additional file 1: Table S5). In patients with a history of cancer, the incidence of AESI was 0.55 and 0.89 per 10,000 person-days for those who received BNT162b2 and matched unvaccinated patients, respectively; 0.42 and 0.93 per 10,000 person-days for patients who received CoronaVac and matched unvaccinated patients, respectively.
Patients who received BNT162b2 or CoronaVac were not at a higher risk of AESI compared to unvaccinated patients in the active cancer cohort [BNT162b2 HR: 0.30 (95% CI 0.08–1.09); CoronaVac HR: 0.14 (95% CI 0.02–1.18)]. Similarly, patients who received BNT162b2 or CoronaVac were not at a higher risk of AESI compared to unvaccinated patients in the history of cancer cohort [BNT162b2 HR: 0.62 (95% CI 0.30–1.28), CoronaVac HR: 0.45 (95% CI 0.21–1.00)] (Table 1). Results were consistent in all subgroup analyses; vaccinated patients had no increased risk of AESI compared to unvaccinated patients.
Among patients with active cancer, there were two deaths in the BNT162b2 group versus 22 among matched unvaccinated patients; and no deaths in the CoronaVac group versus 12 among matched unvaccinated patients. Among patients with a history of cancer, there was one death in the BNT162b2 group versus 13 among matched unvaccinated patients, and 2 deaths in the CoronaVac group versus 17 among matched unvaccinated patients (Additional file 1: Table S5). In the post hoc analysis, the cumulative incidence rate of AESI was not significantly different between patients who received one dose only, compared to unvaccinated patients (0.5% one-dose only and 0.4% unvaccinated, χ2 = 0.63, p = 0.43; Additional file 1: Table S6).
Discussion
The low rate of COVID-19 vaccine uptake in our study appears to reflect safety concerns among patients with cancer in Hong Kong. On September 30, 2021, our data showed that the overall vaccination rate in Hong Kong was 58.8%, while among patients with cancer it was only 30.2%. Our study provides reassurance that patients with cancer are not at an increased risk of AESI or death following two doses of either BNT162b2 or CoronaVac.
Several small observational studies have evaluated the safety of BNT162b2 or CoronaVac vaccines in patients with cancer [8,9,10,11,12,13,14,15]. All of those studies evaluated short-term common adverse events, including pain and swelling at the injection site, headache, fever, and diarrhea. However, no previous study examined AESI as an outcome and none included both patients with active cancer and patients with a history of cancer. To date, the largest study included 816 patients with active cancer and 274 healthcare workers from a single institution in Italy [9]. However, the comparator group comprised healthy individuals with no cancer diagnosis.
To our knowledge, this is the first study to report on all AESI and to evaluate the association between BNT162b2 and CoronaVac and the risk of AESI among patients with active cancer or history of cancer. Our study is also the first and largest territory-wide cohort study that reports on 25,789 patients vaccinated with either BNT162b2 or CoronaVac. Furthermore, our study provides reassuring safety data on these two vaccines in a predominantly Asian population.
This study has several limitations. Firstly, patients in relatively better health or with better prognosis are more likely to get vaccinated, which may lead to a healthy user bias. Therefore, PS matching was used to minimize baseline confounding. Secondly, most AESI that were examined tend to be severe and relatively rare (< 1/1000 person-years) [27]. As a result, we would have been unable to detect a small increase in AESI risk. Nevertheless, the findings are still reassuring since the number of AESI events was small. Finally, since patients who only received the first dose of the vaccine were excluded, this could bias the current two-dose analysis. Nevertheless, our post hoc analysis did not show any significant difference in the cumulative incidence rate of AESI between patients receiving one dose only compared to unvaccinated patients; hence, this is unlikely to bias our findings [28, 29]. Future studies with a longer follow-up period are needed to further inform about potential longer-term risks.
Conclusion
In Hong Kong, the vaccination rate among patients with cancer is relatively low. In the present study, there was no increased risk of AESI following two doses of either BNT162b2 or CoronaVac vaccines among patients with active cancer or a history of cancer. The findings of this study can reassure clinicians and patients about the overall short-term safety of BNT162b2 and CoronaVac in patients with cancer, which could increase the COVID-19 vaccination rate in this vulnerable group of patients.
Availability of data and materials
The datasets analyzed during the current study are not publicly available.
Abbreviations
- AESI:
-
Adverse events of special interest
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- BNF:
-
British National Formulary
- PS:
-
Propensity score
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- SMD:
-
Standardized mean difference
References
Al-Quteimat OM, Amer AM. The impact of the COVID-19 pandemic on cancer patients. Am J Clin Oncol. 2020;43(6):452–5.
Centre for Health Protection, Hong Kong Department of Health. Interim Guidance Notes On Common Medical Diseases and COVID-19 Vaccination In Primary Care Settings [Internet]. Hong Kong 2021 [updated 2021 November 24; cited 2022 January 25]. https://www.covidvaccine.gov.hk/pdf/Guidance_Notes.pdf.
Centers for Disease Control and Prevention. COVID-19 Vaccines for Moderately or Severely Immunocompromised People [Internet]. 2022 [updated 2022 January 7; cited 2022 January 25]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html.
Xiao J, Cheung JK, Wu P, Ni MY, Cowling BJ, Liao Q. Temporal changes in factors associated with COVID-19 vaccine hesitancy and uptake among adults in Hong Kong: serial cross-sectional surveys. Lancet Reg Health West Pac. 2022;23:100441.
Chun JY, Kim SI, Park EY, Park SY, Koh SJ, Cha Y, et al. Cancer patients’ willingness to take COVID-19 vaccination: a nationwide multicenter survey in Korea. Cancers (Basel). 2021;13(15):3883.
Chan WL, Ho YT, Wong CK, Choi HC, Lam KO, Yuen KK, et al. Acceptance of COVID-19 vaccination in cancer patients in Hong Kong: approaches to improve the vaccination rate. Vaccines (Basel). 2021;9(7):792.
Khiari H, Cherif I, M’Ghirbi F, Mezlini A, Hsairi M. COVID-19 vaccination acceptance and its associated factors among cancer patients in Tunisia. Asian Pac J Cancer Prev. 2021;22(11):3499–506.
So ACP, McGrath H, Ting J, Srikandarajah K, Germanou S, Moss C, et al. COVID-19 vaccine safety in cancer patients: a single centre experience. Cancers (Basel). 2021;13(14):3573.
Di Noia V, Pimpinelli F, Renna D, Barberi V, Maccallini MT, Gariazzo L, et al. Immunogenicity and safety of COVID-19 vaccine BNT162b2 for patients with solid cancer: a large cohort prospective study from a single institution. Clin Cancer Res. 2021;27(24):6815–23.
Ligumsky H, Safadi E, Etan T, Vaknin N, Waller M, Croll A, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine among actively treated cancer patients. J Natl Cancer Inst. 2021;114:203–9.
Karacin C, Eren T, Zeynelgil E, Imamoglu GI, Altinbas M, Karadag I, et al. Immunogenicity and safety of the coronavac vaccine in patients with cancer receiving active systemic therapy. Future Oncol. 2021;17(33):4447–56.
Monin L, Laing AG, Munoz-Ruiz M, McKenzie DR, Barrio DMD, I, Alaguthurai T, et al. Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol. 2021;22(6):765–78.
Trillo Aliaga P, Trapani D, Sandoval JL, Crimini E, Antonarelli G, Vivanet G, et al. Safety of COVID-19 mRNA vaccines in patients with cancer enrolled in early-phase clinical trials. Cancers (Basel). 2021;13(22):5829.
Kian W, Zemel M, Kestenbaum EH, Rouvinov K, Alguayn W, Levitas D, et al. Safety of the BNT162b2 mRNA COVID-19 vaccine in oncologic patients undergoing numerous cancer treatment options: a retrospective single-center study. Medicine (Baltimore). 2022;101(2):e28561.
Tamura T, Ninomiya K, Kubo T, Kuyama S, Tachibana S, Inoue K, et al. Short-term safety of an anti-severe acute respiratory syndrome coronavirus 2 messenger RNA vaccine for patients with advanced lung cancer treated with anticancer drugs: a multicenter, prospective, observational study. Thorac Cancer. 2022;13(3):453–9.
Corti C, Curigliano G. Commentary: SARS-CoV-2 vaccines and cancer patients. Ann Oncol Off J Eur Soc Med Oncol. 2021;32(4):569–71.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15.
Palacios R, Batista AP, Albuquerque CSN, Patiño EG, Santos JdP, Conde MTRP, et al. Efficacy and safety of a COVID-19 inactivated vaccine in healthcare professionals in Brazil: The PROFISCOV Study. SSRN; 2021.
Wan EYF, Chui CSL, Lai FTT, Chan EWY, Li X, Yan VKC, et al. Bell’s Palsy following vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines: a case series and nested case-control study. Lancet Infect Dis. 2022;22(1):64–72.
Lai FTT, Huang L, Chui CSL, Wan EYF, Li X, Wong CKH, et al. Multimorbidity and adverse events of special interest associated with Covid-19 vaccines in Hong Kong. Nat Commun. 2022;13(1):411.
Lai FTT, Li X, Peng K, Huang L, Ip P, Tong X, et al. Carditis after COVID-19 vaccination with a messenger RNA vaccine and an inactivated virus vaccine : a case-control study. Ann Intern Med. 2022;175(3):362–70.
Wan EYF, Chui CSL, Wang Y, Ng VWS, Yan VKC, Lai FTT, et al. Herpes zoster related hospitalization after inactivated (CoronaVac) and mRNA (BNT162b2) SARS-CoV-2 vaccination: a self-controlled case series and nested case-control study. Lancet Reg Health West Pac. 2022;21:100393.
Lai FTT, Huang L, Peng K, Li X, Chui CSL, Wan EYF, et al. Post-Covid-19-vaccination adverse events and healthcare utilization among individuals with or without previous SARS-CoV-2 infection. J Intern Med. 2022.
Massarweh A, Eliakim-Raz N, Stemmer A, Levy-Barda A, Yust-Katz S, Zer A, et al. Evaluation of seropositivity following BNT162b2 messenger RNA vaccination for SARS-CoV-2 in patients undergoing treatment for cancer. JAMA Oncol. 2021;7(8):1133–40.
Khorana AA, Noble S, Lee AYY, Soff G, Meyer G, O’Connell C, et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost. 2018;16(9):1891–4.
World Health Organization. COVID-19 Vaccines: Safety Surveillance Manual [Internet]. [updated 2020; cited 2022 January 25]. https://apps.who.int/iris/handle/10665/338400. License: CC BY-NC-SA 3.0 IGO.
Li XT, Ostropolets A, Makadia R, Shoaibi A, Rao G, Sena AG, et al. Characterising the background incidence rates of adverse events of special interest for covid-19 vaccines in eight countries: multinational network cohort study. BMJ. 2021;373:n1435.
Li X, Tong X, Yeung WWY, Kuan P, Yum SHH, Chui CSL, et al. Two-dose COVID-19 vaccination and possible arthritis flare among patients with rheumatoid arthritis in Hong Kong. Ann Rheum Dis. 2022;81(4):564–8.
Food and Health Bureau The Government of the Hong Kong Special Administrative Region. Report on Evaluation of Safety, Efficacy and Quality of Comirnaty COVID-19 mRNA Vaccine (BNT162b2) Concentrate for Dispersion for Injection [Internet]. [updated 2022 January 12; cited 2022 April 7]. https://www.fhb.gov.hk/download/our_work/health/201200/e_evaluation_report.pdf.
Acknowledgements
We thank colleagues from the Drug Office of the Department of Health and from the Hospital Authority for providing vaccination and clinical data. We also thank Bernard Chan for administrative and technical assistance.
Funding
This work was supported by a research grant from the Food and Health Bureau, the Government of the Hong Kong Special Administrative Region (Grant No. COVID19F01). FTTL and ICKW’s post were partly funded by D24H; hence, this work was partly supported by AIR@InnoHK administered by Innovation and Technology Commission. The study sponsors were not directly involved in the design of the study, the collection, analysis, and interpretation of the data, the writing of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
WK, JJPS, ICKW, and EWC contributed to conception and design of the study and acquisition, analysis, or interpretation of data; WK and JJPS drafted the manuscript and performed statistical analysis; all authors helped in critical revision of the manuscript for important intellectual content; ICKW and EWC provided administrative, technical, or material support and supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference Number: UW21-149) and the Department of Health Ethics Committee (LM21/2021). Informed patient consent was not required as the data used in this study were anonymized.
Consent for publication
Not applicable.
Competing interests
XL has received internal funding from the University of Hong Kong; consultancy fees from Merck Sharp & Dohme; research and educational grants from Janssen and Pfizer; research grants from the Food and Health Bureau of the Government of the Hong Kong Special Administrative Region; all of which are outside this work. CSLC has received personal fees from Prime Vigilance; Hong Kong Innovation and Technology Commission from Pfizer, IQVIA, and Amgen; research grants from the Food and Health Bureau of the Hong Kong Government of the Hong Kong Special Administrative Region; all of which are outside this work. FTTL has received the RGC Postdoctoral Fellowship from the Hong Kong Research Grants Council; research grants from the Food and Health Bureau of the Government of the Hong Kong Special Administrative Region; both of which are outside this work. EYFW has received research grants from the Hong Kong Research Grants Council; research grants from the Food and Health Bureau of the Government of the Hong Kong Special Administrative Region; both of which are outside this work. CKHW reports receipt of research funding from the EuroQoL Group Research Foundation, the Hong Kong Research Grants Council, and the Hong Kong Health and Medical Research Fund; all of which are outside this work. ICKW has received research supports from Amgen, Bayer, Bristol-Myers Squibb, GSK, Janssen, Novartis, Pfizer, the Hong Kong Research Grants Council, the Food and Health Bureau of the Government of the Hong Kong Special Administrative Region; the National Health and Medical Research Council in Australia; National Institute for Health Research in England, European Commission, speaker fees from Janssen and Medice in the previous three years; and is an independent non-executive director of Jacobson Medical in Hong Kong; all of which are outside this work. EWC has received research funds and grants from Research Grants Council (RGC, Hong Kong), Research Fund Secretariat of the Food and Health Bureau, Narcotics Division of the Security Bureau of the Hong Kong Special Administrative Region, National Natural Science Fund of China, Amgen, Bayer, Bristol-Myers Squibb, Janssen, Pfizer, Takeda, Wellcome Trust; and reports honorarium from Hospital Authority; all of which are outside this work. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kang, W., Shami, J.J.P., Yan, V.K.C. et al. Safety of two-dose COVID-19 vaccination (BNT162b2 and CoronaVac) in adults with cancer: a territory-wide cohort study. J Hematol Oncol 15, 66 (2022). https://doi.org/10.1186/s13045-022-01265-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-022-01265-9