Abstract
Background
Certain rare syndromes with developmental delay or intellectual disability caused by genomic copy number variants (CNVs), either deletions or duplications, are associated with higher rates of obesity. Current strategies to diagnose these syndromes typically rely on phenotype-driven investigation. However, the strong phenotypic overlap between syndromic forms of obesity poses challenges to accurate diagnosis, and many different individual cytogenetic and molecular approaches may be required. Multiplex ligation-dependent probe amplification (MLPA) enables the simultaneous analysis of multiple targeted loci in a single test, and serves as an important screening tool for large cohorts of patients in whom deletions and duplications involving specific loci are suspected. Our aim was to design a synthetic probe set for MLPA analysis to investigate in a cohort of 338 patients with syndromic obesity deletions and duplications in genomic regions that can cause this phenotype.
Results
We identified 18 patients harboring copy number imbalances; 18 deletions and 5 duplications. The alterations in ten patients were delineated by chromosomal microarrays, and in the remaining cases by additional MLPA probes incorporated into commercial kits. Nine patients showed deletions in regions of known microdeletion syndromes with obesity as a clinical feature: in 2q37 (4 cases), 9q34 (1 case) and 17p11.2 (4 cases). Four patients harbored CNVs in the DiGeorge syndrome locus at 22q11.2. Two other patients had deletions within the 22q11.2 ‘distal’ locus associated with a variable clinical phenotype and obesity in some individuals. The other three patients had a recurrent CNV of one of three susceptibility loci: at 1q21.1 ‘distal’, 16p11.2 ‘distal’, and 16p11.2 ‘proximal’.
Conclusions
Our study demonstrates the utility of an MLPA-based first line screening test to the evaluation of obese patients presenting with syndromic features. The overall detection rate with the synthetic MLPA probe set was about 5.3% (18 out of 338). Our experience leads us to suggest that MLPA could serve as an effective alternative first line screening test to chromosomal microarrays for diagnosis of syndromic obesity, allowing for a number of loci (e.g., 1p36, 2p25, 2q37, 6q16, 9q34, 11p14, 16p11.2, 17p11.2), known to be clinically relevant for this patient population, to be interrogated simultaneously.
Similar content being viewed by others
Background
Obesity is defined as an abnormal or excessive fat accumulation that presents a risk to health, and is commonly classified using the body mass index (BMI = weight/height2). It is well established that single-gene defects or genomic copy number variants (CNVs), either deletions or duplications, can lead to both syndromic and non-syndromic forms of obesity [1]. The term syndromic obesity refers to rare or uncommon genetic syndromes, in which obesity is one of a range of symptoms, often including developmental delay (DD) and intellectual deficit (ID). Prader-Willi syndrome (PWS; OMIM 176270) is the most common known genetic cause of obesity, resulting more frequently from a deletion in the paternal 15q11.2-q13 chromosomal region. The diagnosis is typically made in early infancy due to hypotonia and poor feeding, prior to the onset of obesity and hyperphagia [2].
Several other clinically well-defined microdeletion syndromes also have an increased prevalence of obesity, but they are often clinically difficult to diagnose due to extensive phenotypic overlap and lack of a diagnostic testing path. Examples are 1p36 monosomy (OMIM 607872), brachydactyly-mental retardation (BDMR) syndrome (OMIM 600430), 6q16 deletion syndrome (OMIM 603128), Kleefstra syndrome (KS; OMIM 610253), Wilms tumor, aniridia, genitourinary anomalies, and mental retardation (WAGR) syndrome (OMIM 194072, 612469), and Smith-Magenis syndrome (SMS; OMIM 182290). Some of these syndromes have now been explained by haploinsufficiency of a single gene in the critical deletion intervals, including BDMR (HDAC4) [3], KS (EHMT1) [4], and SMS (RAI1) [3]-[5]. In addition, the obesity phenotype in patients with 6q16 deletion is likely explained by haploinsufficiency of the transcription factor single-minded 1 (SIM1) gene [6], whereas obesity susceptibility in WAGR syndrome mainly depends on haploinsufficiency for the brain-derived neurotrophic factor (BDNF) gene [7].
Since in recent years chromosomal microarray analysis (CMA) has become the method of choice for detecting copy number imbalances in the genome, a great number of rare CNVs and microdeletion/duplication syndromes have been found that cause, or predispose to, obesity along with DD/ID and other phenotypic findings, such as 1p21.3 microdeletions [8], 2p25.3 deletions [9],[10], interstitial deletions within 6q14.1q15 [11], 6q22 deletions [12], translocation der(8)t(8;12)(p23.1;p13.31) [13], interstitial deletions on 11p14.1 [14], 12q subtelomeric deletions [15], 16p11.2 distal and proximal deletion [16],[17], 17q24.2 microdeletions [18], chromosome 19q duplications [19], and several others [20]-[22]. Multiplex ligation-dependent probe amplification (MLPA) is more cost and time-efficient than microarray-based approaches, and provides an alternate method of simultaneously determining copy number status at multiple target loci. In this study, we have designed a synthetic probe set to interrogate the copy number status at previously described loci associated with syndromic obesity, and defined the length of the lost or gained DNA regions by SNP-array and/or oligoarray-CGH or, alternatively, using commercial MLPA kits. We report our findings from screening in a cohort of 338 patients with syndromic obesity.
Results
Results are shown in Table 1. Copy number imbalances were detected in 18 patients (diagnostic yield of 5.3%); 18 deletions and 5 duplications. The alterations in ten cases were confirmed (delineated) by SNP-array (patients 2 and 18) and oligoarray-CGH (patients 1, 3–8, 17), while the alterations in eight cases were fine-mapped using the commercial MLPA kits P064-B2 (patients 9–12) and P023-B (patients 13–16), with more probes in sequences adjacent to the genes in which copy number gains or losses were detected.
Patient 1 had duplication for two gene probes from 1q21.1, PRKAB2 and ACP6 (Figure 1A). The duplication was shown to have a size of ~1.8 Mb with breakpoints in segmental duplication (SD), or low-copy repeat (LCR), blocks BP3 (distally) and BP4 (proximally), located in the distal 1q21.1 region (as delimitated by CMA). Four patients were deleted for probes mapped to the 2q37.3 locus: patients 2–4 had deletion for probes HDAC4 and GPR35 (Figure 1B), and patient 5 had a deletion for probe GPR35 (Figure 1C); no deletion of the region detected by probe HDAC4 was observed in the latter case. The CMA results showed an additional ~1.7 Mb duplication adjacent and proximal to the deletion of patient 2, and a concurrent 17q25.3 duplication of ~2.3 Mb in patient 5. Present deletions vary in size from ~2.2 Mb to 6.2 Mb. Patient 6 had a deletion for the 9q34.3 probe EHMT1 (Figure 1D). Subsequent CMA demonstrated a submicroscopic deletion of ~0.4 Mb extending from EHMT1 (exon 17) to the most distal gene CACNA1B. Two patients were found with CNVs at the 16p11.2 locus: patient 7 had a deletion for the most distal probe SH2B1 (Figure 2E), and patient 8 had duplication for the most proximal probes CDIPT and MAPK3 (Figure 2F). Testing of parental DNAs showed that the deletion occurred apparently de novo, while the duplication was inherited from the normal father. CMA confirmed that the deletion in patient 7 is confined to the distal 16p11.2 region flanked by SD blocks BP2 and BP3, and the duplication in patient 8 to the proximal 16p11.2 region flanked by SD blocks BP4 and BP5.
Partial electropherograms for control individuals (red) and for the patient (blue) normalized by the GeneMarker software showing the custom probes with reduced or amplified peak heights (arrows). A) sample with increased copy number for the probes PRKAB2 and ACP6. B) sample with reduced copy number for the probes HDAC4 and GPR35. C) sample with reduced copy number for the probe GPR35. D) sample with reduced copy number for the probe EHMT1. E) sample with reduced copy number for the probe SH2B1. F) sample with increased copy number for the probes CDIPT and MAPK3. G) sample with reduced copy number for the probe RAI1. H) sample with reduced copy number for the probe CRKL. I) sample with increased copy number for the probe CRKL. J) sample with reduced copy number for the probe RAB36.
Electropherograms patterns using control DNAs. The two MLPA testing panels are shown (‘A’ probe set added to P300; ‘B’ probe set added to P200). Each peak represents the amplicon signal from a correspondent gene or control probe loci as labeled at bottom X-axis. The top X-axis indicates the size of the amplicon and the Y-axis indicates the fluorescent intensity. Arrows indicate X and Y chromosome specific control probes. For normal female control (A), it was observed absence of Y-specific DNA sequences. For normal male sample (B), it was observed a decrease for the dosage of X-specific control probe with respect to a female control.
Deletion in 17p11.2 probe RAI1 has been found in patients 9–12 (Figure 2G), and in all of these patients deletion within the FLCN gene, which is reference probe in the P200 and P300 MLPA kits, mapped to chromosome 17p11.2, has been detected (data not shown). The P064-B2 MLPA kit used in this study includes five probes specific for sequences in the SMS 17p11.2 region, with the most distal probe in the gene TNFRSF13B, near the distal SMS repeat (SMS-REP), and the most proximal probe in MFAP4, between the middle and proximal SMS-REPs. According to these MLPA results, the deletion of patient 9 has a minimum size of 2.2 Mb, with the distal breakpoint occurring between probes TNFRSF13B (not deleted) and FLCN (deleted), and extended proximally through MFAP4 (deleted). The deletions of patients 10–12 have a minimum size of 2.4 Mb mapping between deleted MLPA probes TNFRSF13B and MFAP4.
The remaining 6 patients had CNVs at the 22q11.2 locus: patients 13–15 had a deletion for the most proximal probe CRKL (Figure 2H), patient 16 had a duplication for this same probe (Figure 2I), and patients 17 and 18 had a deletion for the most distal probe RAB36 (Figure 2J); no deletion of the region detected by probe MAPK1 was observed in any of these patients. Two of the CNVs were apparently de novo (patients 13 and 14), while three CNVs were inherited from an unaffected parent (patients 15–17); the inheritance could not be explored for patient 18 who is an adopted teen. According to the results of the P023-B MLPA probes, all deletions and the duplication of proximal 22q11.2 have a minimum size of 2 Mb mapping between deleted MLPA probes HIRA proximally, which is located between LCR22-A and LCR22-B, and LZTR1 distally, located between LCR22-C and LCR22-D. The deletions of patients 17 and 18 were delineated by CMA and shown to have a size of ~0.6 Mb. The deletions boundaries are within SD blocks LCR22-E and LCR22-F at the distal 22q11.2 region.
Discussion
In the present study, we aimed to develop an alternative, more cost-efficient tool than chromosomal microarrays to be used in the initial screening of a large cohort of patients presenting with syndromic obesity. As many of the currently known loci associated with syndromic forms of obesity have their causative genes already discovered, or have their breakpoints localized to flanking repeat sequences, we thought these disorders would be amenable to detection by MLPA using a synthetic probe set. In our cohort of 338 patients, 5.3% (18 patients) had a pathogenic diagnosis detected primarily by MLPA. Our detection rate is lower compared with 22% of patients with a potentially pathogenic diagnosis reported by Vuillaume et al. [22] for array-CGH in a similar cohort. The lesser diagnostic yield in the present study may be explained by the targeted approach versus the whole genome approach in Vuillaume’s paper, as the criteria to select cases is very similar in the two studies (i.e., obesity and at least one other feature such as DD, ID, congenital anomalies or dysmorphic features). Although whole genome array allows the investigation of known syndromes and abnormalities that have not been described before, yet cost considerations still limit its use in routine clinical application in developing countries, whereas MLPA has been found to be a good option in situations of cost constraints [23],[24]. In our experience, the per sample cost of MLPA to CMA is in the ratio of 1:5. Moreover, MLPA does not require validation of copy number changes detected by more than one probe, thus eliminating costs with additional tests for establishing the diagnosis. In addition, the probe set as we have developed it detects only known aberrations so that the clinical interpretation of the data is straightforward.
We diagnosed nine of patients with clinically well-defined microdeletion syndromes complicated by obesity. Among these, four cases had 2q37 deletions ranging from 2.2 to 6.2 Mb. In all patients, except one, the deletions involved HDAC4 (histone deacetylase 4), the primary causative gene for BDMR syndrome [3], and that could be responsible for obesity (seen in >40% of patients [25]). The protein encoded by this gene is involved in histone acetylation and chromatin remodeling. Consistent with a role of HDAC4 in the development of obesity, deletion in or mutation of HDAC4 was reported as resulting in reduced expression of the retinoic acid induced 1 (RAI1) gene, whose haploinsufficiency leads to obesity in SMS [3]. Moreover, HDAC4 was shown to be downregulated in obese compared with lean subjects, and then induced by physical activity [26]. Of note, the only two patients with HDAC4 point mutations reported to date were detected in BDMR patients who were obese [3]. Other two genes, CAPN10 and HDLBP, that are located distal to HDAC4, were also associated with obesity [27] and deleted for patient 5 carrying a 2q37 deletion that is distal to and did not include HDAC4. Another obese patient with a terminal deletion distal to HDAC4 was reported by Williams et al. [3]. These results may suggest one more distal locus at 2q37.3 critical for obesity.
A relatively small 9q34.3 deletion including only partially the euchromatic histone methyltransferase 1 (EHMT1) gene, in which deletion (seen in >85% of cases) or mutation (rarely) causes KS, was found in one patient. Recent reports support previous observations that obesity is present in a higher frequency in KS [28]-[30]. In the latest study of 83 KS patients with BMI data, including both patients with deletions and point mutations of EHMT1, Williemsem et al. [30] showed that ~30-40% of the KS patients were overweight (BMI >25), and observed that this feature was more frequent among patients with a mutation than in patients with a deletion (42 vs. 28%, respectively). In a recent study by Ohno et al. [31], it was demonstrated that deficiency of EHMT1 in brown fat cells leads to obesity and insulin resistance. This reinforces the notion that haploinsufficiency of EHMT1 is causative for obesity. Four patients carried a 17p11.2 deletion, including RAI1, the major gene for the phenotypic features of SMS. Obesity has been reported in >50% of SMS patients with either deletion or mutation of the RAI1[32],[33]. Supporting the fact that RAI1 is involved in the obesity phenotype, Bdnf, a gene associated with obesity and hyperphagia, was found downregulated in the hypothalamus of the mouse model for Rai1 haploinsufficiency [34]. Furthermore, it was found in the same study that human RAI1 directly regulates the expression of BDNF.
Six patients were diagnosed with chromosome 22q11.2 abnormalities at both proximal and distal intervals. The 22q11.2 deletion spanning the four proximal LCR22s A to D within the DiGeorge (DG) and velo-cardio-facial syndrome (VCFS) region was found in three patients and the reciprocal duplication was found in another. Approximately one in every 167 patients with neurocognitive disorders and multiple congenital anomalies has a deletion in the 22q11.2 DG region, while its reciprocal duplication occurs in 1 of every 384 such cases [35],[36]. Two distinct studies have reported a high prevalence of obesity in adolescents and adults with DG [37],[38]. In one of these studies, it was shown that at adolescence or early adulthood, up to 35% of DG deletion carriers developed obesity [38]; data on the prevalence of obesity in 22q11.2 duplication has not been published.
We have identified two patients with the 22q11.2 ‘distal’ deletion associated with a variable clinical phenotype [39]. The deletions boundaries for the two individuals are within LCR22s E and F, whereas most reported distal 22q11.2 deletions has been shown to extend from LCR22-D to LCR22s E or F [40],[41]. Obesity (weight-for-age >90th percentile) was reported in 6 of 22 previously published cases [39]-[42], and three patients had a postnatal weight between the 75th and 90th percentile [40],[41]. In addition, two of the obese patients reported by Fagerberg et al. [40] had neurobehavioral problems such as food seeking behaviors and hyperphagia. Thus, our findings further suggest that the 22q11.2 distal deletion may predispose to obesity and overweight.
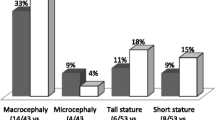
Additionally, three other patients were found to have recurrent CNVs associated with incomplete penetrance and variable expressivity. A child presenting with an overgrowth phenotype (macrocephaly, growth acceleration, and obesity) had the distal 1q21.1 duplication previously associated with macrocephaly (the reciprocal deletion is associated with microcephaly) and other features of overgrowth [43]-[45]. This locus includes the brain-specific HYDIN2 gene and a cluster of NBPF genes, which have been proposed as candidates for the abnormal head size [43],[46]. The 16p11.2 distal deletion associated with DD and obesity [16] was found in one individual. This deletion was shown to account for 0.5% of severe childhood obese cases [47], and was reported in 46 of 38851 (0.12%) patients with DD in two recent large studies [36],[48]. This locus includes the SH2B adaptor protein 1 (SH2B1) gene, which is likely responsible for obesity in these individuals [16]. Another patient was found with the proximal 16p11.2 duplication associated with neurocognitive deficits and known to increase the risk of being underweight [49], whereas the reciprocal deletion cosegregates with severe early-onset obesity [17]. Both the deletion and the duplication were shown to occur in 0.2-0.4% patients submitted for clinical CMA testing [35],[36].
As for the remaining probes in the probe set, we were unable to identify copy number imbalances in patients from our cohort. At least two CNVs, of SIM1 at 6q16 and BDNF at 11p14, are well known to include obesity as a phenotype [6],[7],[14],[50],[51]. In addition, 2p25.3 deletions spanning MYT1L have now been reported in a number of patients with a PWS-like phenotype [9],[10],[21]. The Imprinted in Prader-Willi (IPW) non-coding RNA is located to the critical region containing the functional PWS gene locus, including the SNORD109A and SNORD116 snoRNA cluster [52]. This minimal region was delineated based on the study of rare cases resulting from atypical 15q11q12 microdeletions without methylation abnormalities [52]-[55]. Extremely rare mutations in NTRK2, which encodes a highly specific receptor for BDNF, were found in severely obese children with DD [56],[57]. However, it is currently unknown whether or not CNVs of the NTRK2 gene also can result in a comparable phenotype. None of the probes within new candidate loci for syndromic obesity (i.e., 3p26.3, 4p16.1, 7q22.1, 12q15q21.1, 14q11.2, and 14q12) [21],[58]; Table 2], were found as copy number variable in any additional patient. Hence, the contribution of these CNVs to obesity still remains uncertain and yet to be demonstrated.
Conclusions
Our study demonstrates the utility of an MLPA-based first line screening test in the evaluation of the genetic etiology of syndromic obesity in 338 patients. The overall detection rate with the synthetic MLPA probe set was about 5.3% (18 out of 338). As compared to chromosomal microarrays, it is an efficient, rapid, less labour intensive and cost-effective alternative for interrogating the copy number status at multiple loci that are known to cause this phenotype. Application of CMA testing to as yet undiagnosed individuals will uncover new loci responsible for the patients’ phenotype, which would otherwise remain undetected based solely on the MLPA evaluation. These could eventually become new microdeletion/duplication syndromes associated with syndromic obesity. Our results also suggest that obesity could likely be a feature of the 22q11.2 distal deletion syndrome. Finally, our experience leads us to suggest that incorporating an MLPA-based first line screening test targeting various loci in which altered dosage is known to result in obesity as a phenotype (such as 1p36, 2p25, 2q37, 6q16, 9q34, 11p14, 16p11.2, and 17p11.2), could provide an effective alternative diagnostic approach to chromosomal microarrays for syndromic obesity, especially in clinical settings where CMA is not available.
Methods
Patients
Three hundred and thirty-eight nonrelated individuals with a prior negative methylation test for PWS were included in this study. The study protocol was reviewed and approved by the Human Research Ethics Committee at the Institute of Biosciences, University of São Paulo (CEP/IB/021/2004). Parents or guardians also provided written informed consent. All the patients had a general diagnosis of DD/ID along with obesity or overweight. However, this cohort also includes other phenotypic findings including, but not restricted to, congenital malformations, hypotonia and feeding difficulties, behavioral issues, autism spectrum disorders, hyperphagia, hearing impairment, epilepsy, and dysmorphic features. Part of this cohort had previously been discarded for microdeletions of chromosome 1p36 by the syndrome-specific SALSA MLPA kit (P147, MRC Holland, Amsterdam, The Netherlands) [61]. All DNA samples were obtained from peripheral blood using the Autopure LS® (Gentra Systems, Inc., Minneapolis, MN).
Multiplex-ligation dependent probe amplification (MLPA)
Synthetic MLPA probe set
The probe set includes 31 MLPA probes for the detection of copy number imbalances involving the following chromosomal regions (genes): 1q21.1 (PRKAB2, ACP6), 2p25.3 (ACP1, TPO, MYT1L), 2q37 (HDAC4, GPR35), 3p26.3 (CNTN6, CHL1), 4p16.1 (ACOX3, CPZ), 6q16 (SIM1), 7q22.1 (RELN), 9q21.33 (NTRK2), 9q34 (EHMT1), 11p14 (BDNF, MPPED2), 12q15q21 (PTPRB, RAB21, TPH2), 14q11.2 (CHD8, RAB2B), 14q12 (PRKD1), 15q11.2 (IPW), 16p11.2 (SH2B1, CDIPT, MAPK3), 17p11.2 (RAI1) and 22q11.2 (CRKL, MAPK1, RAB36) (Table 2). Up to three probes were designed preferably in coding regions of specific genes within the regions of interest. The probes were designed online using the publicly available MAPD software [62]. Individual oligonucleotide probes (size range 100–168 nt) were synthesized by IDT® (Integrated DNA Technologies, Belgium) and added to the SALSA® MLPA® P200 and P300 Human DNA reference kits (Table 3). The MLPA reactions were performed on 100–250 ng genomic DNA samples following the MRC-Holland protocol [63]. MLPA products were size-separated by capillary electrophoresis on the 3730 Genetic Analyser (Applied Biosystems, UK) and interpreted with the GeneMarker (v1.95) software (SoftGenetics, LLC. State College, PA, USA) using the “population normalization” method. Peak ratios between 0.75 and 1.25 were considered normal (i.e. two copies). Figure 2 shows the MLPA profiles for the two testing panels in control samples of different sex. These panels were validated by the analysis of DNA of patients with known CNVs (data not shown). When available, blood samples were obtained from patients’ parents, and CNV inheritance was investigated.
Follow-up MLPA kits
When an alteration was found within the 17p11.2 (SMS) region or in 22q11.2 within the DG/VCFS region, confirmatory testing was performed with commercial MLPA kits (MR-1 MLPA kit P064-B2 and DG/VCFS MLPA kit P023-B, respectively).
Chromosomal microarray analysis (CMA)
The alterations in 10 patients were verified using at least one array platform. The arrays used in this study are the Affymetrix 500 K SNP-array (Affymetrix, Santa Clara, CA, USA), the CytoSure ISCA 180 K oligoarray-CGH (Oxford Gene Technology, Oxford, UK), and a 60 K custom-designed 60-mer oligoarray (Agilent Technologies, Palo Alto, CA, USA). SNP-array testing was performed as previously described [21]. Oligoarrays were hybridized according to the manufacturer’s’ instructions. Hybridizations were performed in duplicates with dye-reversal method. Scanned images were processed using Agilent Feature Extraction software and analyzed with Genomic Workbench software (both from Agilent Technologies) applying the statistical algorithm ADM-2 with a sensitivity threshold of 6.7. Duplication or deletion was considered when the log2 ratio of the Cy3/Cy5 intensities of a given region encompassing at least three probes was >0.3 or - < 0.3, respectively. Genomic coordinates were converted to UCSC genome browser build February 2009 (GRCh37/hg19).
Authors’ contributions
D’Angelo CS was the principal investigator and takes primary responsibility for the paper; D’Angelo CS performed the laboratory work, data interpretation and drafted the manuscript; Varela MC performed the methylation test that ruled out the diagnosis of PWS in all patients; Castro CIE gave technical support on MLPA analysis; Kim CA, Bertola DR and Lourenço CM are the primary physicians of most patients; Koiffmann CP co-ordinated the research. All authors read and approved the final manuscript.
Abbreviations
- DD:
-
Developmental delay
- ID:
-
Intellectual disability
- MLPA:
-
Multiplex ligation-dependent probe amplification
- CNV:
-
Copy number variant
- CMA:
-
Chromosomal microarray analysis
- BMI:
-
Body mass index
- PWS:
-
Prader-Willi syndrome
- BDMR:
-
Brachydactyly-mental retardation
- KS:
-
Kleefstra syndrome
- WAGR:
-
Wilms tumor, aniridia, genitourinary anomalies, and mental retardation
- SMS:
-
Smith-Magenis syndrome
- DG:
-
DiGeorge
- VCFS:
-
Velo-cardio-facial syndrome
- SD:
-
Segmental duplication
- LCR:
-
Low-copy repeat
References
D’Angelo CS, Koiffmann CP: Copy number variants in obesity-related syndromes: review and perspectives on novel molecular approaches. J Obes 2012, 2012: 1–15. 10.1155/2012/845480
Cassidy SB, Schwartz S, Miller JL, Driscoll DJ: Prader-Willi syndrome. Genet Med 2012, 14: 10–26. 10.1038/gim.0b013e31822bead0
Williams SR, Aldred MA, Der Kaloustian VM, Halal F, Gowans G, McLeod DR, Zondag S, Toriello HV, Magenis RE, Elsea SH: Haploinsufficiency of HDAC4 causes brachydactyly mental retardation syndrome, with brachydactyly type E, developmental delays, and behavioral problems. Am J Hum Genet 2010, 87: 219–228. 10.1016/j.ajhg.2010.07.011
Kleefstra T, Smidt M, Banning MJ, Oudakker AR, Van Esch H, de Brouwer AP, Nillesen W, Sistermans EA, Hamel BC, de Bruijn D, Fryns JP, Yntema HG, Brunner HG, de Vries BB, van Bokhoven H: Disruption of the gene Euchromatin Histone Methyl Transferase1 (Eu-HMTase1) is associated with the 9q34 subtelomeric deletion syndrome. J Med Genet 2005, 42: 299–306. 10.1136/jmg.2004.028464
Slager RE, Newton TL, Vlangos CN, Finucane B, Elsea SH: Mutations in RAI1 associated with Smith-Magenis syndrome. Nat Genet 2003, 33: 466–468. 10.1038/ng1126
Bonaglia MC, Ciccone R, Gimelli G, Gimelli S, Marelli S, Verheij J, Giorda R, Grasso R, Borgatti R, Pagone F, Rodrìguez L, Martinez-Frias ML, van Ravenswaaij C, Zuffardi O: Detailed phenotype–genotype study in five patients with chromosome 6q16 deletion: narrowing the critical region for Prader-Willi-like phenotype. Eur J Hum Genet 2008,16(12):1443–1449. 10.1038/ejhg.2008.119
Han JC, Liu QR, Jones M, Levinn RL, Menzie CM, Jefferson-George KS, Adler-Wailes DC, Sanford EL, Lacbawan FL, Uhl GR, Rennert OM, Yanovski JA: Brain-derived neurotrophic factor and obesity in the WAGR syndrome. N Engl J Med 2008, 359: 918–927. 10.1056/NEJMoa0801119
Willemsen MH, Vallès A, Kirkels LA, Mastebroek M, Olde Loohuis N, Kos A, Wissink-Lindhout WM, de Brouwer AP, Nillesen WM, Pfundt R, Holder-Espinasse M, Vallèe L, Andrieux J, Coppens-Hofman MC, Rensen H, Hamel BC, van Bokhoven H, Aschrafi A, Kleefstra T: Chromosome 1p21.3 microdeletions comprising DPYD and MIR137 are associated with intellectual disability. J Med Genet 2011, 48: 810–818. 10.1136/jmedgenet-2011-100294
Stevens SJ, van Ravenswaaij-Arts CM, Janssen JW, Klein Wassink-Ruiter JS, van Essen AJ, Dijkhuizen T, van Rheenen J, Heuts-Vijgen R, Stegmann AP, Smeets EE, Engelen JJ: MYT1L is a candidate gene for intellectual disability in patients with 2p25.3 (2pter) deletions. Am J Med Genet A 2011,155(11):2739–2745. 10.1002/ajmg.a.34274
Doco-Fenzy M, Leroy C, Schneider A, Petit F, Delrue MA, Andrieux J, Perrin-Sabourin L, Landais E, Aboura A, Puechberty J, Girard M, Tournaire M, Sanchez E, Rooryck C, Ameil A, Goossens M, Jonveaux P, Lefort G, Taine L, Cailley D, Gaillard D, Leheup B, Sarda P, Genevieve D: Early-onset obesity and paternal 2pter deletion encompassing the ACP1, TMEM18, and MYT1L genes. Eur J Hum Genet 2014, 22: 471–479. 10.1038/ejhg.2013.189
Wentzel C, Lynch SA, Stattin EL, Sharkey FH, Annerén G, Thuresson AC: Interstitial Deletions at 6q14.1-q15 Associated with Obesity, Developmental Delay and a Distinct Clinical Phenotype. Mol Syndromol 2010,1(2):75–81. 10.1159/000314025
Rosenfeld JA, Amrom D, Andermann E, Andermann F, Veilleux M, Curry C, Fisher J, Deputy S, Aylsworth AS, Powell CM, Manickam K, Heese B, Maisenbacher M, Stevens C, Ellison JW, Upton S, Moeschler J, Torres-Martinez W, Stevens A, Marion R, Pereira EM, Babcock M, Morrow B, Sahoo T, Lamb AN, Ballif BC, Paciorkowski AR, Shaffer LG: Genotype-phenotype correlation in interstitial 6q deletions: a report of 12 new cases. Neurogenetics 2012,13(1):31–47. 10.1007/s10048-011-0306-5
Goldlust IS, Hermetz KE, Catalano LM, Barfield RT, Cozad R, Wynn G, Ozdemir AC, Conneely KN, Mulle JG, Dharamrup S, Hegde MR, Kim KH, Angle B, Colley A, Webb AE, Thorland EC, Ellison JW, Rosenfeld JA, Ballif BC, Shaffer LG, Demmer LA: Unique Rare Chromosome Disorder Support Group, Rudd MK: Mouse model implicates GNB3 duplication in a childhood obesity syndrome. Proc Natl Acad Sci U S A 2013,110(37):14990–14994. 10.1073/pnas.1305999110
Shinawi M, Sahoo T, Maranda B, Skinner SA, Skinner C, Chinault C, Zascavage R, Peters SU, Patel A, Stevenson RE, Beaudet AL: 11p14.1 microdeletions associated with ADHD, autism, developmental delay, and obesity. Am J Med Genet A 2011,155(6):1272–1280. 10.1002/ajmg.a.33878
Niyazov DM, Nawaz Z, Justice AN, Toriello HV, Martin CL, Adam MP: Genotype/phenotype correlations in two patients with 12q subtelomere deletions. Am J Med Genet A 2007, 143: 2700–2705. 10.1002/ajmg.a.32005
Bochukova EG, Huang N, Keogh J, Henning E, Purmann C, Blaszczyk K, Saeed S, Hamilton-Shield J, Clayton-Smith J, O'Rahilly S, Hurles ME, Farooqi IS: Large, rare chromosomal deletions associated with severe early-onset obesity. Nature 2010, 463: 666–670. 10.1038/nature08689
Walters RG, Jacquemont S, Valsesia A, de Smith AJ, Martinet D, Andersson J, Falchi M, Chen F, Andrieux J, Lobbens S, Delobel B, Stutzmann F, El-Sayed Moustafa JS, Chèvre JC, Lecoeur C, Vatin V, Bouquillon S, Buxton JL, Boute O, Holder-Espinasse M, Cuisset JM, Lemaitre MP, Ambresin AE, Brioschi A, Gaillard M, Giusti V, Fellmann F, Ferrarini A, Hadjikhani N, Campion D, et al.: A new highly penetrant form of obesity due to deletions on chromosome 16p11.2. Nature 2010, 463: 671–675. 10.1038/nature08727
Vergult S, Dauber A, Delle Chiaie B, Van Oudenhove E, Simon M, Rihani A, Loeys B, Hirschhorn J, Pfotenhauer J, Phillips JA 3rd, Mohammed S, Ogilvie C, Crolla J, Mortier G, Menten B: 17q24.2 microdeletions: a new syndromal entity with intellectual disability, truncal obesity, mood swings and hallucinations. Eur J Hum Genet 2012, 20: 534–539. 10.1038/ejhg.2011.239
Davidsson J, Jahnke K, Forsgren M, Collin A, Soller M: Dup(19)(q12q13.2): Array-based genotype-phenotype correlation of a new possibly obesity-related syndrome. Obesity 2010, 18: 580–587. 10.1038/oby.2009.298
Dasouki MJ, Youngs EL, Hovanes K: Structural chromosome abnormalities associated with obesity: Report of four new subjects and review of literature. Curr Genom 2011, 12: 190–203. 10.2174/138920211795677930
D’Angelo CS, Kohl I, Varela MC, de Castro CI, Kim CA, Bertola DR, Lourenco CM, Perez AB, Koiffmann CP: Obesity with associated developmental delay and/or learning disability in patients exhibiting additional features: Report of novel pathogenic copy number variants. Am J Med Genet A 2013,161(3):479–486. 10.1002/ajmg.a.35761
Vuillaume M-L, Naudion S, Banneau G, Diene G, Cartault A, Cailley D, Bouron J, Toutain J, Bourrouillou G, Vigouroux A, Bouneau L, Nacka F, Kieffer I, Arveiler B, Knoll-Gellida A, Babin PJ, Bieth E, Jouret B, Julia S, Sarda P, Genevie`ve D, Faivre L, Lacombe D, Barat P, Tauber M, Delrue M-A, Rooryck C: New candidate loci identified by array-CGH in a cohort of 100 children presenting with syndromic obesity. Am J Med Genet A 2014,164(8):1965–1975. 10.1002/ajmg.a.36587
Dutra RL, Honjo RS, Kulikowski LD, Fonseca FM, Pieri PC, Jehee FS, Bertola DR, Kim CA: Copy number variation in Williams-Beuren syndrome: suitable diagnostic strategy for developing countries. BMC Res Notes 2012,9(5):13. 10.1186/1756-0500-5-13
Boggula VR, Shukla A, Danda S, Hariharan SV, Nampoothiri S, Kumar R, Phadke SR: Clinical utility of multiplex ligation-dependent probe amplification technique in identification of aetiology of unexplained mental retardation: a study in 203 Indian patients. Indian J Med Res 2014,139(1):66–75.
Falk RE, Casas KA: Chromosome 2q37 deletion: clinical and molecular aspects. Am J Med Genet C 2007, 145C: 357–371. 10.1002/ajmg.c.30153
Abu-Farha M, Tiss A, Abubaker J, Khadir A, Al-Ghimlas F, Al-Khairi I, Baturcam E, Cherian P, Elkum N, Hammad M, John J, Kavalakatt S, Warsame S, Behbehani K, Dermime S, Dehbi M: Proteomics analysis of human obesity reveals the epigenetic factor HDAC4 as a potential target for obesity. PLoS One 2013,8(9):e75342. 10.1371/journal.pone.0075342
Leroy C, Landais E, Briault S, David A, Tassy O, Gruchy N, Delobel B, Grégoire MJ, Leheup B, Taine L, Lacombe D, Delrue MA, Toutain A, Paubel A, Mugneret F, Thauvin-Robinet C, Arpin S, Le Caignec C, Jonveaux P, Beri M, Leporrier N, Motte J, Fiquet C, Brichet O, Mozelle-Nivoix M, Sabouraud P, Golovkine N, Bednarek N, Gaillard D, Doco-Fenzy M: The 2q37-deletion syndrome: an update of the clinical spectrum including overweight, brachydactyly and behavioural features in 14 new patients. Eur J Hum Genet 2013, 21: 602–640. 10.1038/ejhg.2012.230
Cormier-Daire V, Molinari F, Rio M, Raoul O, de Blois MC, Romana S, Vekemans M, Munnich A, Colleaux L: Cryptic terminal deletion of chromosome 9q34: a novel cause of syndromic obesity in childhood? J Med Genet 2003,40(4):300–303. 10.1136/jmg.40.4.300
Kleefstra T, van Zelst-Stams WA, Nillesen WM, Cormier-Daire V, Houge G, Foulds N, van Dooren M, Willemsen MH, Pfundt R, Turner A, Wilson M, McGaughran J, Rauch A, Zenker M, Adam MP, Innes M, Davies C, López AG, Casalone R, Weber A, Brueton LA, Navarro AD, Bralo MP, Venselaar H, Stegmann SP, Yntema HG, van Bokhoven H, Brunner HG: Further clinical and molecular delineation of the 9q subtelomeric deletion syndrome supports a major contribution of EHMT1 haploinsufficiency to the core phenotype. J Med Genet 2009,46(9):598–606. 10.1136/jmg.2008.062950
Willemsen MH, Vulto-van Silfhout AT, Nillesen WM, Wissink-Lindhout WM, van Bokhoven H, Philip N, Berry-Kravis EM, Kini U, van Ravenswaaij-Arts CM, Delle Chiaie B, Innes AM, Houge G, Kosonen T, Cremer K, Fannemel M, Stray-Pedersen A, Reardon W, Ignatius J, Lachlan K, Mircher C, van den Enden PT H, Mastebroek M, Cohn-Hokke PE, Yntema HG, Drunat S, Kleefstra T: Update on Kleefstra Syndrome. Mol Syndromol 2012,2(3–5):202–212.
Ohno H, Shinoda K, Ohyama K, Sharp LZ, Kajimura S: EHMT1 controls brown adipose cell fate and thermogenesis through the PRDM16 complex. Nature 2013, 504: 7478. 10.1038/nature12652
Edelman EA, Girirajan S, Finucane B, Patel PI, Lupski JR, Smith AC, Elsea SH: Gender, genotype, and phenotype differences in Smith-Magenis syndrome: a meta-analysis of 105 cases. Clin Genet 2007,71(6):540–550. 10.1111/j.1399-0004.2007.00815.x
Vilboux T, Ciccone C, Blancato JK, Cox GF, Deshpande C, Introne WJ, Gahl WA, Smith AC, Huizing M: Molecular analysis of the Retinoic Acid Induced 1 gene (RAI1) in patients with suspected Smith-Magenis syndrome without the 17p11.2 deletion. PLoS One 2011,6(8):e22861. 10.1371/journal.pone.0022861
Burns B, Schmidt K, Williams SR, Kim S, Girirajan S, Elsea SH: Rai1 haploinsufficiency causes reduced Bdnf expression resulting in hyperphagia, obesity and altered fat distribution in mice and humans with no evidence of metabolic syndrome. Hum Mol Genet 2010,19(20):4026–4042. 10.1093/hmg/ddq317
Kaminsky EB, Kaul V, Paschall J, Church DM, Bunke B, Kunig D, Moreno-De-Luca D, Moreno-De-Luca A, Mulle JG, Warren ST, Richard G, Compton JG, Fuller AE, Gliem TJ, Huang S, Collinson MN, Beal SJ, Ackley T, Pickering DL, Golden DM, Aston E, Whitby H, Shetty S, Rossi MR, Rudd MK, South ST, Brothman AR, Sanger WG, Iyer RK, Crolla JA, et al.: An evidence-based approach to establish the functional and clinical significance of copy number variants in intellectual and developmental disabilities. Genet Med 2011,13(9):777–784. 10.1097/GIM.0b013e31822c79f9
Cooper GM, Coe BP, Girirajan S, Rosenfeld JA, Vu TH, Baker C, Williams C, Stalker H, Hamid R, Hannig V, Abdel-Hamid H, Bader P, McCracken E, Niyazov D, Leppig K, Thiese H, Hummel M, Alexander N, Gorski J, Kussmann J, Shashi V, Johnson K, Rehder C, Ballif BC, Shaffer LG, Eichler EE: A copy number variation morbidity map of developmental delay. Nat Genet 2011,43(9):838–846. 10.1038/ng.909
Digilio MC, Marino B, Cappa M, Cambiaso P, Giannotti A, Dallapiccola B: Auxological evaluation in patients with DiGeorge/velocardiofacial syndrome (deletion 22q11.2 syndrome). Genet Med 2001,3(1):30–33. 10.1097/00125817-200101000-00007
Bassett AS, Chow EW, Husted J, Weksberg R, Caluseriu O, Webb GD, Gatzoulis MA: Clinical features of 78 adults with 22q11 deletion syndrome. Am J Med Genet A 2005, 138: 307–313. 10.1002/ajmg.a.30984
Ben-Shachar S, Ou Z, Shaw CA, Belmont JW, Patel MS, Hummel M, Amato S, Tartaglia N, Berg J, Sutton VR, Lalani SR, Chinault AC, Cheung SW, Lupski JR, Patel A: 22q11.2 distal deletion: a recurrent genomic disorder distinct from DiGeorge syndrome and velocardiofacial syndrome. Am J Hum Genet 2008, 82: 214–221. 10.1016/j.ajhg.2007.09.014
Fagerberg CR, Graakjaer J, Heinl UD, Ousager LB, Dreyer I, Kirchhoff M, Rasmussen AA, Lautrup CK, Birkebaek N, Sorensen K: Heart defects and other features of the 22q11 distal deletion syndrome. Eur J Med Genet 2013,56(2):98–107. 10.1016/j.ejmg.2012.09.009
Mikhail FM, Burnside RD, Rush B, Ibrahim J, Godshalk R, Rutledge SL, Robin NH, Descartes MD, Carroll AJ: The recurrent distal 22q11.2 microdeletions are often de novo and do not represent a single clinical entity: a proposed categorization system. Genet Med 2013,16(1):92–100. 10.1038/gim.2013.79
Mikhail FM, Descartes M, Piotrowski A, Andersson R, Diaz de Ståhl T, Komorowski J, Bruder CE, Dumanski JP, Carroll AJ: A previously unrecognized microdeletion syndrome on chromosome 22 band q11.2 encompassing the BCR gene. Am J Med Genet A 2007,43A(18):2178–2184. 10.1002/ajmg.a.31882
Brunetti-Pierri N, Berg JS, Scaglia F, Belmont J, Bacino CA, Sahoo T, Lalani SR, Graham B, Lee B, Shinawi M, Shen J, Kang SH, Pursley A, Lotze T, Kennedy G, Lansky-Shafer S, Weaver C, Roeder ER, Grebe TA, Arnold GL, Hutchison T, Reimschisel T, Amato S, Geragthy MT, Innis JW, Obersztyn E, Nowakowska B, Rosengren SS, Bader PI, Grange DK, et al.: Recurrent reciprocal 1q21.1 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat Genet 2008, 40: 1466–1471. 10.1038/ng.279
Mefford HC, Sharp AJ, Baker C, Itsara A, Jiang Z, Buysse K, Huang S, Maloney VK, Crolla JA, Baralle D, Collins A, Mercer C, Norga K, de Ravel T, Devriendt K, Bongers EM, de Leeuw N, Reardon W, Gimelli S, Bena F, Hennekam RC, Male A, Gaunt L, Clayton-Smith J, Simonic I, Park SM, Mehta SG, Nik-Zainal S, Woods CG, Firth HV, et al.: Recurrent rearrangements of chromosome 1q21.1 and variable pediatric phenotypes. N Engl J Med 2008,359(16):1685–1699. 10.1056/NEJMoa0805384
Dolcetti A, Silversides CK, Marshall CR, Lionel AC, Stavropoulos DJ, Scherer SW, Bassett AS: 1q21.1 microduplication expression in adults. Genet Med 2013, 15: 282–289. 10.1038/gim.2012.129
Dumas L, Sikela JM: DUF1220 domains, cognitive disease, and human brain evolution. Cold Spring Harb Symp Quant Biol 2009, 74: 375–382. 10.1101/sqb.2009.74.025
Walters RG, Coin LJM, Ruokonen A, de Smith AJ, El-Sayed Moustafa JS, Jacquemont S, Elliott P, Esko T, Hartikainen AL, Laitinen J, Männik K, Martinet D, Meyre D, Nauck M, Schurmann C, Sladek R, Thorleifsson G, Thorsteinsdóttir U, Valsesia A, Waeber G, Zufferey F, Balkau B, Pattou F, Metspalu A, Völzke H, Vollenweider P, Stefansson K, Järvelin MR, Beckmann JS, Froguel P, et al.: Rare genomic structural variants in complex disease: lessons from the replication of associations with obesity. PLoS One 2013,8(3):e58048. 10.1371/journal.pone.0058048
Bachmann-Gagescu R, Mefford HC, Cowan C, Glew GM, Hing AV, Wallace S, Bader PI, Hamati A, Reitnauer PJ, Smith R, Stockton DW, Muhle H, Helbig I, Eichler EE, Ballif BC, Rosenfeld J, Tsuchiya KD: Recurrent 200-kb deletions of 16p11.2 that include the SH2B1 gene are associated with developmental delay and obesity. Genet Med 2010,12(10):641–647. 10.1097/GIM.0b013e3181ef4286
Jacquemont S, Reymond A, Zufferey F, Harewood L, Walters RG, Kutalik Z, Martinet D, Shen Y, Valsesia A, Beckmann ND, Thorleifsson G, Belfiore M, Bouquillon S, Campion D, de Leeuw N, de Vries BB, Esko T, Fernandez BA, Fernández-Aranda F, Fernández-Real JM, Gratac’s M, Guilmatre A, Hoyer J, Jarvelin MR, Kooy RF, Kurg A, Le Caignec C, Männik K, Platt OS, Sanlaville D, et al.: Mirror extreme BMI phenotypes associated with gene dosage at the chromosome 16p11.2 locus. Nature 2011, 478: 97–102. 10.1038/nature10406
Holder JL Jr, Butte NF, Zinn AR: Profound obesity associated with a balanced translocation that disrupts the SIM1 gene. Hum Mol Genet 2000,9(1):101–108. 10.1093/hmg/9.1.101
Gray J, Yeo GS, Cox JJ, Morton J, Adlam AL, Keogh JM, Yanovski JA, El Gharbawy A, Han JC, Tung YC, Hodges JR, Raymond FL, O'rahilly S, Farooqi IS: Hyperphagia, severe obesity, impaired cognitive function and hyperactivity associated with functional loss of one copy of the BDNF gene. Diabetes 2006, 55: 3366–3371. 10.2337/db06-0550
Bieth E, Eddiry S, Gaston V, Lorenzini F, Buffet A, Conte Auriol F, Molinas C, Cailley D, Rooryck C, Arveiler B, Cavaillé J, Salles JP, Tauber M: Highly restricted deletion of the SNORD116 region is implicated in Prader–Willi Syndrome. Eur J Hum Genet 2014. in press.
Sahoo T, del Gaudio D, German JR, Shinawi M, Peters SU, Person RE, Garnica A, Cheung SW, Beaudet AL: Prader-Willi phenotype caused by paternal deficiency for the HBII-85 C/D box small nucleolar RNA cluster. Nat Genet 2008,40(6):719–721. 10.1038/ng.158
de Smith AJ, Purmann C, Walters RG, Ellis RJ, Holder SE, Van Haelst MM, Brady AF, Fairbrother UL, Dattani M, Keogh JM, Henning E, Yeo GS, O'Rahilly S, Froguel P, Farooqi IS, Blakemore AI: A deletion of the HBII-85 class of small nucleolar RNAs (snoRNAs) is associated with hyperphagia, obesity and hypogonadism. Hum Mol Genet 2009,18(17):3257–3265. 10.1093/hmg/ddp263
Duker AL, Ballif BC, Bawle EV, Person RE, Mahadevan S, Alliman S, Thompson R, Traylor R, Bejjani BA, Shaffer LG, Rosenfeld JA, Lamb AN, Sahoo T: Paternally inherited microdeletion at 15q11.2 confirms a significant role for the SNORD116 C/D box snoRNA cluster in Prader-Willi syndrome. Eur J Hum Genet 2010,18(11):1196–1201. 10.1038/ejhg.2010.102
Yeo GS, Connie Hung CC, Rochford J, Keogh J, Gray J, Sivaramakrishnan S, O'Rahilly S, Farooqi IS: A de novo mutation affecting human TrkB associated with severe obesity and developmental delay. Nat Neurosci 2004,7(11):1187–1189. 10.1038/nn1336
Gray J, Yeo G, Hung C, Keogh J, Clayton P, Banerjee K, McAulay A, O'Rahilly S, Farooqi IS: Functional characterization of human NTRK2 mutations identified in patients with severe early-onset obesity. Int J Obes (Lond) 2007,31(2):359–364. 10.1038/sj.ijo.0803390
Williams SR, Girirajan S, Tegay D, Nowak N, Hatchwell E, Elsea SH: Array comparative genomic hybridisation of 52 subjects with a Smith-Magenis-like phenotype: identification of dosage sensitive loci also associated with schizophrenia, autism, and developmental delay. J Med Genet 2010,47(4):223–229. 10.1136/jmg.2009.068072
Uliana V, Grosso S, Cioni M, Ariani F, Papa FT, Tamburello S, Rossi E, Katzaki E, Mucciolo M, Marozza A, Pollazzon M, Mencarelli MA, Mari F, Balestri P, Renieri A: 3.2 Mb microdeletion in chromosome 7 bands q22.2q22.3 associated with overgrowth and delayed bone age. Eur J Med Genet 2010, 53: 168–170. 10.1016/j.ejmg.2010.02.003
D’Angelo CS, Jehee FS, Koiffmann CP: An inherited atypical 1 Mb 22q11.2 deletion within the DGS/VCFS 3 Mb region in a child with obesity and aggressive behavior. Am J Med Genet A 2007, 143A: 1928–1932. 10.1002/ajmg.a.31787
D’Angelo CS, Kohl I, Varela MC, de Castro CI, Kim CA, Bertola DR, Lourenco CM, Koiffmann CP: Extending the phenotype of monosomy 1p36 syndrome and mapping of a critical region for obesity and hyperphagia. Am J Med Genet Part A 2010, 152A: 102–110. 10.1002/ajmg.a.33160
MAPD: MLPA Probe Design. , [http://bioinform.arcan.stonybrook.edu/mlpa2/cgi-bin/mlpa.cgi]
MRC-Holland – MLPA Technology – Synthetic Probe Design Protocol. , [http://www.mlpa.com/]
Acknowledgements
We are grateful to the patients and their families for participating in this study. The work was supported by grants from The State of Sao Paulo Research Foundation, FAPESP [09/52523-1 to C.S.D.], The Centers for Research, Innovation and Diffusion, CEPID- FAPESP [1998/14254-2], and The National Council for Scientific and Technological Development, CNPq [304381/2007-1 to C.P.K.].
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
D’Angelo, C.S., Varela, M.C., de Castro, C.I. et al. Investigation of selected genomic deletions and duplications in a cohort of 338 patients presenting with syndromic obesity by multiplex ligation-dependent probe amplification using synthetic probes. Mol Cytogenet 7, 75 (2014). https://doi.org/10.1186/s13039-014-0075-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-014-0075-6