Abstract
Background
The psychological impact of the COVID-19 pandemic has been understudied among vulnerable populations. This study aimed to examine the immediate and longer-term changes in the mental health of children with parent–child separation experiences during the COVID-19 pandemic, and identify potential buffering opportunities for mental health.
Methods
This longitudinal cohort study used data from 723 rural Chinese children who provided data before (Oct. 2019) the COVID-19 pandemic and during the following 2 years. Changes in the probability of depressive symptoms, anxiety symptoms, non-suicide self-injurious (NSSI), suicidal ideation, suicide plan, and suicide attempt were tested across four waves using generalized estimating models (GEE).
Results
Compared with children who never experienced parent–child separation, children persistently separated from parents since birth experienced greater deterioration in all mental health in the 2-year follow-up (average change: depressive symptoms: β = 0.59, 95% CI [0.26, 0.93]; anxiety symptoms: β = 0.45, 95% CI [0.10, 0.81]; NSSI: β = 0.66, 95% CI [0.31, 1.01]; suicide ideation: β = 0.67, 95% CI [0.38, 0.96]; suicide plan: β = 0.77, 95% CI [0.38, 1.15]; suicide attempt: β = 1.12, 95% CI [0.63, 1.62]). However, children with childhood separation from their parents but reunited with them during the transition to adolescence showed similar even lower changes to counterparts who never experienced parent–child separation (all ps > 0.05).
Conclusion
These results indicating improvements in supportiveness of the caregiving environment during the transition to adolescence may provide the opportunity to buffer the adverse impact of COVID-19 on mental health. Translating such knowledge to inform intervention and prevention strategies for youths exposed to adversity is a critical goal for the field.
Similar content being viewed by others
Introduction
Emerging studies have examined the relationship between pandemic-related disruptions and mental health in the general young population. Longitudinal studies and repeated cross-sectional studies have shown that depressive and anxiety symptoms, suicidal ideation, and suicide attempts increased from before to during the pandemic [2, 3, 29, 35, 40]. However, there is a scarcity of studies on vulnerable and underserved children, especially those born in socioeconomically vulnerable families in rural China and persistently separated from their parents, which have been largely unexplored.
An estimated 69 million children (25.4% of the child population) were experiencing parent–child separation in China, of which 40.51 million rural children are left behind by their parents’ migrating to urban areas to find work to provide for their families [30]. Social isolation and high physical and psychosocial deprivation increase their risk of mental health outcomes [11, 43]. In China, some migrant parents choose to return home when their children start school (around age 6) to support their children emotionally and help them succeed in school [16]. Previous studies have shown that children who experienced parent–child separation are at a high risk of developing psychological problems during the COVID-19 pandemic [34] and after lifting the restrictions [25]. In addition, the parent–child separation duration and timing may be a effective predictor of children’s mental problems. A recent study about 1177 left-behind adolescents’ loneliness revealed that the longer parents are separated from their children, the greater the negative impact on children [42]. An important issue that has been largely unexplored in the existing literature is the pattern (timing and duration) of separation and the effect on children’s mental and behavioral health domains. Given that the sensitivity of neural circuits to adversity undergoes dynamic changes from prenatal to young adulthood, the effects of parent–child separation may vary with the developmental stage at which separation occurs and how long it persists [12, 19]. Among pandemic-related research examining young people’s mental health issues such as depression, anxiety, and suicide related problems, we are yet to see longitudinal data to track the adverse effects on non-suicide self-injurious (NSSI), suicidal ideation, and suicide attempt. Given the increasing rates of NSSI and suicide over the past decade [10], especially among youth, it is concerning.
The current study therefore used a longitudinal sample from a feeder location for migrant employees in the countryside of southern China, with the overall aim of describing the short- and longer-term trajectories in mental health (depressive and anxious symptoms, NSSI, suicide-related problems) of school-aged children before and during the initial and later phases of the pandemic. We aimed to evaluate the differential performance of mental health in children with different experiences of parent–child separation to identify potential remedial windows; and attempted to identify additional risk and protective factors for mental health in response to the pandemic. Findings complement emerging literature [21, 31, 39] by providing insight into the changes in mental health before and during the pandemic among highly vulnerable and neglect-exposed children with parent–child separation experiences.
Methods
Sample
Data came from an ongoing representative longitudinal study of rural children living in Chizhou, Anhui Province. Children in grades 4 through 8 from local primary and junior high schools in Chizhou were recruited and followed up each year since October 2019. After 3 months of lockdown due to the COVID-19 pandemic, schools in Chizhou were reopened on April 26, 2020. An additional investigation was conducted 2 weeks after the school reopening in May 2020.
As illustrated in Additional file 1: Figure S1, of the original 1276 respondents who completed a pre-pandemic survey (Oct. 2019), 1236 participated in Wave 2 (May 2020), 1209 in Wave 3 (Oct. 2020), and 723 in Wave 4 (Oct. 2021).
Measures
Outcomes
The measurements for each outcome were consistent across all four wave surveys. Depressive symptoms were calculated using the 33-item Mood and Feelings Questionnaire (MFQ) [7, 9]. A binary variable was created using a cutoff point of 27 [37]. Anxiety symptoms (generalized anxiety) were calculated by computing the mean item scores for this dimension of the Overanxious subscale of MacArthur HBQ [6, 40]. The baseline's 85th percentile (score 4.08 or higher) was used as the cut-off point for identifying the presence of anxiety symptoms. NSSI behaviors were measured using the 8-item non-suicidal self-injurious (NSSI) behavior questionnaire. A binary variable was defined as three or more NSSI behaviors being reported. Suicidal ideation, suicide plan, and suicide attempt were assessed with reference to the ‘middle school questionnaire’ of the 2013 Youth Risk Behaviour Surveillance System in the USA [8, 33]. Suicidal ideation was defined as a ‘yes’ in response to the question ‘Have you ever thought about killing yourself in the past 3 months?’. Suicide plan was defined as a ‘yes’ in response to the question, “During the past 3 months, did you make any plans to kill yourself?”. Suicide attempt was defined as a ‘yes’ in response to the question, ‘Have you ever tried to kill yourself in the past 3 months?’.
Parent–child separation experiences
In the present study, parents or caregivers were asked if both of the children's parents had migrated to urban areas for work for more than 6 months per year during early childhood (from birth to 6 years old) and/or during the past years (after 6 years old). Four categories were generated based on the timing and duration of parent–child separation: (1) no separation; (2) early childhood separation before 6 years old; (3) recent separation after 6 years old; (4) prolonged separation since birth.
Demographic characteristics
Household socioeconomic status (SES), positive childhood experiences (PCEs), neglect, lifestyle behaviors (sleep-related problems, physical activity, screen time before bedtime), and health-related indicators (self-perceived health) were derived from physical examinations or questionnaires (detailed in Additional file 1).
Statistical analysis
Changes in mental health within individuals during the COVID-19 pandemic were examined using generalized estimating models. First, we tested the whole population-level changes in the probability of the binary depressive symptoms, NSSI, suicidal ideation, and suicide plan before and during the COVID-19 pandemic. We then regressed standardized outcomes scores on COVID-19 period indicators to enable direct comparisons across the six mental health outcomes. Second, we examined the interaction effects between the COVID-19 period and the parent–child separation experiences to understand whether and how mental health outcomes changes during the COVID-19 pandemic periods might vary across different parent–child separation groups. The effects parameters included group and time as categorical predictors, as well as the group × time interaction. The no-separation group was the reference level for group, and the baseline survey was the reference level for time. Finally, we tested the moderating effects of the sociodemographic and lifestyle characteristics by regressing each mental health outcome on each factor. Data management and analyses were conducted in Stata version 15.1.
Results
Table 1 displays the characteristics of the analytical sample. Compared with those lost to follow-up due to graduation at Wave 4 (n = 486), participants included in the analytical model (n = 723) were slightly younger and had a lower percentage of parent–child separation experiences (see Additional file 1: Table S1). The mean (SD) age at Wave 4 (Oct. 2021) was 11.56 (1.35) years, and 514 (38.0%) were girls.
At baseline (pre-pandemic level), 82 (11.3%) of 723 participants scored above the at-risk thresholds for depression, 85 (11.8%) for anxiety symptoms, 67 (9.3%) for NSSI, 137 (18.9%) for suicidal ideation, 53 (7.3%) for suicide plan, and 22 (3.0%) for suicide attempt (see Additional file 1: Table S2). Of the sample included, 132 (18.3%) were separated from their parents only during early childhood (before 6 years), 61 (8.4%) had recently separated from their parents after the age of 6, and 104 (14.4%) persistently separated from their parents since birth. In general, children who experienced parent–child separation tended to have poorer baseline mental health than those who had never been separated from their parents.
Figure 1, Additional file 1: Tables S3 and S4 report the predicted trajectories of mental health outcomes before (October 2019) and during the initial and later phases of the COVID-19 pandemic for the entire population. Compared to pre-pandemic levels, all mental health outcomes except for anxiety symptoms deteriorated after 3-month school lockdown (change in May 2020 compared to pre-epidemic: 4.1% [3.8%, 4.5%] for depressive symptoms; 4.3% [3.9%, 4.7%] for NSSI; 4.1% [3.9%, 4.4%] for suicidal ideation; 4.0% [3.6%, 4.4%] for suicide plan; 2.8% [2.3%, 3.2%] for suicide attempt) and then slightly moderated after 5-month past the school-reopening (October 2020). But surprisingly, instead of further moderation, all mental health outcomes, including anxiety symptoms worsened again during the subsequent 12-month follow-up (Change in October 2021 compared to pre-epidemic: 4.3% (3.9%, 4.6%) for depressive symptoms; 4.0% (3.7%, 4.3%) for anxiety symptoms; 6.0% (5.4%, 6.5%) for non-suicidal self-injury; 5.4% (5.1%, 5.7%) for suicidal ideation; 4.4% (3.9%, 4.9%) for suicide plan; 2.8% (2.3%, 3.2%) for suicide attempt).
There may be a lagged long-term worsening effect of anxiety symptoms that gradually emerges over time; in the present study, anxiety symptoms did not show significant worsening at the time of school reopening and the subsequent 5-month follow-up, whereas when followed up to 19 months, the probability of anxiety symptoms exhibited a significant deterioration than before the pandemic (4.0% (3.7%, 4.3%]). Among the six mental health outcomes, NSSI showed the sharpest deterioration before and during the initial and later phases of the COVID-19 pandemic (Additional file 1: Figure S2, Table S5).
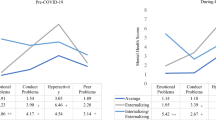
Figure 2 reports the predicted trajectories of mental health outcomes among children with parent–child separation experiences before (Wave 1) and during the initial and later phases of the COVID-19 pandemic. Compared to children never separated from their parents, children who persistently separated from both parents since birth experienced the sharpest immediate deterioration in all mental health outcomes (Table 2, depressive symptoms: β = 0.80, 95% CI [0.37, 1.24], P < 0.001; NSSI: β = 0.67, 95% CI [0.19, 1.15], P = 0.006; suicide ideation: β = 0.67, 95% CI [0.27, 1.07], P = 0.001; suicide plan: β = 0.77, 95% CI [0.26, 1.27], P = 0.003; suicide attempt: β = 1.04, 95% CI [0.35, 1.73], P = 0.003) after 3-month school lockdown (Wave 2); at the subsequent 19-month follow-up, children with persistent parent–child separation since birth continued to show more deterioration in all mental health outcomes (Wave 4, depressive symptoms: β = 0.63, 95% CI [0.15, 1.10], P = 0.01; anxiety symptoms: β = 0.76, 95% CI [0.30, 1.22], P = 0.001; NSSI: β = 0.69, 95% CI [0.20, 1.18], P = 0.002; suicide ideation: β = 0.79, 95% CI [0.37, 1.20], P < 0.001; suicide plan: β = 0.87, 95% CI [0.34, 1.40], P = 0.001; suicide attempt: β = 1.44, 95% CI [0.80, 2.09], P < 0.001).
Similarly, children who had recently separated from their parents after the age of 6 also exhibited greater longer-term deterioration in NSSI and suicide attempts (Wave 4, NSSI: β = 0.66, 95% CI [0.22, 1.11], P = 0.003; suicide attempt: β = 1.30, 95% CI [0.45, 2.24], P = 0.003). In contrast, children separated from both parents in early childhood (before age 6) and then reunited with parents after showed a similar or smaller magnitude of deterioration than children without parent–child separation.
Overall, the immediate and longer-term changes in all mental health outcomes for the full sample were largely driven by the deterioration in children who had been separated from their parents since birth; in addition, the longer-term changes in NSSI and suicide attempts were also explained by deterioration in children with the recent separation from both parents (after the age of 6 years).
Figure 3 reports the results from generalized estimating models for the moderating role of sociodemographic characteristics and lifestyle factors on the binary mental health outcomes before and during the pandemic. Being girls, greater age, low SES, more screen time before bed, sleep-related problems, and self-perceived poor health were associated with worse mental health outcomes (average changes from Wave 1 to 4). Notably, high economic status did not confer a significant protective effect on mental health during the epidemic, especially for suicide plan and attempt. Positive childhood experiences had a buffering effect on changes in mental health during the epidemic, and the effect values showed a dose–response trend (Additional file 1: Table S6).
Moderating effect of the sociodemographic and lifestyle factors on continuous mental health outcomes. Coefficient plot of the point estimates and 95% CIs for the moderating role of sociodemographic and lifestyle characteristics. Estimates for socioeconomic and lifestyle characteristics are from generalized estimating models in which the binary mental health outcome (average changes from Wave 2 to 4) was regressed on this indicator with the variable listed in the vertical axis
Discussion
This study responds to the urgent call for research to further understand the mental health effects of the COVID-19 pandemic across vulnerable groups [13]. This study provides population-based evidence, including multiple time points before and during the initial and later phases of the COVID-19 pandemic, to examine the short- and longer-term trajectories of mental health in the context of left-behind children in rural China. Our results indicated that adolescents’ mental health outcomes continue to worsen even 2 years after the COVID-19 outbreak, especially among those with prolonged parent–child separation experiences. This study also provides preliminary evidence that parent–child reunion during the transition to adolescence may provide buffering opportunities.
After 2 years of follow-up, approximately twice as many children separated from parents since birth experienced depressive symptoms, anxiety symptoms, and NSSI, and three times as many had suicide-related problems compared to the pre-pandemic levels, significantly higher than that in children without parent–child separation. Similarly, children who recently separated from their parents also exhibited greater deterioration (short- and longer-term) in NSSI and suicide attempts than children who had never been separated. However, children with childhood parent–child separation and reunited with parents during the transition to adolescence showed similar mental health trajectories to children who had never experienced parent–child separation. According to the attachment theory, the sense of attachment security might enable the children to better cope with stressors [5, 20]. When children are separated from their parents, they may experience risk for ongoing attachment disruptions [14] and develop an insecure attachment marked by avoidance or anxious-escalation of their attachment needs [20]. The insecure attachment is associated with poor mental health outcomes [18], especially during the COVID-19 pandemic [32]. It may explain worsening mental health outcomes among those who remained the children experiencing prolonged parent–child separation. It also highlights the importance of parental support for helping young children cope with stressors.
Our findings regarding differences in mental health changes across parent–child separation patterns during the COVID-19 pandemic are novel. These results suggest, first and foremost, that early adversity may have a recent and cumulative effect on mental health. The multiple challenges in such a fragile, insecure, and neglected setting increase the vulnerability of children experiencing recent and prolonged parent–child separation to mental health disruptions. Second, the resilient performance in response to the epidemic among children who were separated only until age six but reunited with their parents during the adolescent transition suggests that adolescence as a period of heightened neurobiological plasticity and sensitivity to the social environment [26, 28], may confer unique opportunities for buffering the harmful effects of early childhood through radical improvements in the rearing environment compared to earlier years, and thus potentially acquiring the ability to better cope with future stressors.
Several factors might play a part in the deteriorating mental health of these individuals over this period. For instance, our findings indicated that children with the perception of poor health, longer screen time before bed, and irregular sleep patterns were more likely to have increased psychological distress. Gender may be an additional source of disparities in the adverse psychological impact of the pandemic. Girls have experienced more negative changes in mental health than boys since the pandemic started. Sex-related differences in stress reactivity and resilience may partially account for more psychological distress in girls than boys [36]. The COVID-19 pandemic has further highlighted disparities in mental health burdens for girls [22, 24, 27, 36, 38]. Girls need to undertake more family work than boys, especially in rural [15]. The same was seen in chinese rural girls are left behind, more than one-third of them bear the responsibility for housework and childcare [41]. This labor burden imposes extra stress on girls apart from the COVID-related stressors. Notably, findings suggest that PCEs may mitigate the negative effect of the COVID-19 pandemic on mental health in a dose–response manner. These results are in line with the investigations among Wisconsin adults, indicating that PCEs largely buffered the effect of ACEs on adult mental health when both ACEs and PCEs in the same model [4].
One might hope the negative psychological impact of the COVID-19 pandemic on children and adolescents will be short-lived. However, this is not necessarily the case. Against the backdrop of more than 19 consecutive months of very low confirmed cases in China, psychological burden among children with recent and prolonged parent–child separation remained substantially high. During the last wave (Oct. 2021) of the present study, children reporting suicidal plans and attempts remained twice to three times higher than pre-pandemic levels. Notably, there may be a lagged and lasting effect of the COVID-19 pandemic on youth suicide, as summarized by Asarnow and Chung [1]. Time-limited adverse experiences may fundamentally change the way individuals take to challenges, especially in children and adolescents with developing brains. Furthermore, the interaction between lifestyle changes and psychosocial stress caused by health-related disasters could further aggravate the detrimental effects on children’s physical and mental health, which could cause a vicious cycle.
While mental health services have been provided to left-behind children by some local governments during the pandemic, most of the local governments were unable to afford more mental health services because of a lack of health resources, or even unaware of the problem. The present research provides essential evidence for policy makers and service planners. Based on the current study results, more attention should be paid to the mental health of rural children with parent–child separation experiences, especially during times of stress and crisis. Policy makers should consider this information and channel resources to target children in greatest need.
Limitations
Our findings need to be interpreted in light of several limitations. These include using self-reported mental health outcomes rather than clinical diagnostic data. In several prior longitudinal samples, however, worsening depression and other mental health outcomes self-reported online or by telephone across different age groups correlated significantly with the COVID-19 pandemic [21, 23, 39], suggesting that repeated self-report measures adequately represented the changes of psychological status during the pandemic. Although we explored several potential determinants in this period, we lacked some factors that might give a more complete picture of mental health deterioration, such as parent–child conflict or exposure to violence and abuse. Despite our efforts to control the covariates that affect outcomes, multicollinearity has been recognized as principal difficulties in the present study. In addition, due to graduation from middle school, the response rate in the last survey was considerably lower than in the first three. Given that high school seniors may suffer the most during the pandemic [17], mental health deterioration in 2021 was largely underestimated.
Conclusions
Our findings suggest that, among Chinese rural adolescents, parent–child separation experience was associated with deteriorated mental health outcomes during and after the COVID-19 outbreak. Furthermore, parent–child reunion during the transition to adolescence may provide buffering opportunities. Enhancing the quantity and quality of positive childhood experiences, including warm nurturing, and seizing the unique opportunity for caregiver buffering during adolescence may help steel children's resilience in the face of future stressors. Translating such knowledge to inform intervention and prevention strategies for youths exposed to adversity is a critical goal for the field.
Availability of data and materials
The data-sets analyzed during this study are available from the corresponding author on reasonable request.
Abbreviations
- NSSI:
-
Non-suicide self-injurious
- ACE:
-
Adverse childhood experiences
- PCEs:
-
Positive childhood experiences
References
Asarnow JR, Chung B. Editorial: COVID-19: lessons learned for suicide prevention. J Child Psychol Psychiatry. 2021;62(8):919–21.
Bai W, Cai H, Liu S, Chen X, Sha S, Cheung T, et al. Anxiety and depressive symptoms in college students during the late stage of the COVID-19 outbreak: a network approach. Transl Psychiatry. 2021;11(1):638.
Barendse MEA, Flannery J, Cavanagh C, Aristizabal M, Becker SP, Berger E, et al. Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID-19 pandemic. J Res Adolesc. 2023;33(1):74–91.
Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: associations across adverse childhood experiences levels. JAMA Pediatr. 2019;173(11):e193007.
Bowlby J. Attachment and loss: retrospect and prospect. Am J Orthopsychiatry. 1982;52(4):664.
Boyce WT, Essex MJ, Woodward HR, Measelle JR, Ablow JC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. I: exploring the “head waters” of early life morbidities. J Am Acad Child Adolesc Psychiatry. 2002;41(5):580–7.
Cao FL, Su LY, Cheng PX. Reliability and validity of the mood and feelings questionnaire in chinese adolescents. Chin J Clin Psychol. 2009;17(4):440–2.
Centers for Disease Control and Prevention. Adolescent and School Health: YRBSS Questionnaire. 2013. www.cdc.gov/healthyyouth/data/yrbs/questionnaires.htm. Accessed 28 Mar 2022
Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry. 1988;27(6):726–37.
Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among U.S. undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. 2019;65(5):590–8.
Fellmeth G, Rose-Clarke K, Zhao C, Busert LK, Zheng Y, Massazza A, et al. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet. 2018;392(10164):2567–82.
Gee DG. Early adversity and development: parsing heterogeneity and identifying pathways of risk and resilience. Am J Psychiatry. 2021;178(11):998–1013.
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60.
Humphreys KL. Future directions in the study and treatment of parent-child separation. J Clin Child Adolesc Psychol. 2019;48(1):166–78.
Lin TC, Adserà A. Son preference and children’s housework: the case of India. Popul Res Policy Rev. 2013;32(4):553–84.
Liu Z, Yu L, Zheng X. No longer left-behind: the impact of return migrant parents on children’s performance. China Econ Rev. 2018;49:184–96.
Meade J. Mental health effects of the COVID-19 pandemic on children and adolescents: a review of the current research. Pediatr Clin North Am. 2021;68(5):945–59.
Martínez P, Gloger S, Dagnino P, de Medina DD. Early adverse stress and depression severity: A pilot exploration of mediating psychological mechanisms. Dev Psychopathol. 2023. https://doi.org/10.1017/S0954579423000688.
Méndez Leal AS, Silvers JA. Neurobiological markers of resilience to early-life adversity during adolescence. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(2):238–47.
Mikulincer M, Shaver PR. Attachment orientations and emotion regulation. Curr Opin Psychol. 2019;25:6–10.
Moya A, Serneels P, Desrosiers A, Reyes V, Torres MJ, Lieberman A. The COVID-19 pandemic and maternal mental health in a fragile and conflict-affected setting in Tumaco, Colombia: a cohort study. Lancet Glob Health. 2021;9(8):e1068–76.
O’Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2021;218(6):326–33.
Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8(7):610–9.
Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142–50.
Racine N, Korczak DJ, Madigan S. Evidence suggests children are being left behind in COVID-19 mental health research. Eur Child Adolesc Psychiatry. 2022;31(9):1479–80.
Romeo RD. The metamorphosis of adolescent hormonal stress reactivity: a focus on animal models. Front Neuroendocrinol. 2018;49:43–51.
Saunders NR, Kurdyak P, Stukel TA, Strauss R, Fu L, Guan J, Fiksenbaum L, et al. Utilization of physician-based mental health care services among children and adolescents before and during the COVID-19 pandemic in Ontario, Canada. JAMA Pediatr. 2022;176(4):e216298.
Sisk CL, Romeo RD. Coming of age: The neurobiology and psychobiology of puberty and adolescence. New York, NY: Oxford University; 2020.
Thorisdottir IE, Asgeirsdottir BB, Kristjansson AL, Valdimarsdottir HB, Jonsdottir Tolgyes EM, Sigfusson J, et al. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: a longitudinal, population-based study. Lancet Psychiatry. 2021;8(8):663–72.
National Bureau of Statistics of China and National Bureau of Statistics of China. Population status of children in China in 2015.UNICEF China. 2017. https://www.unicef.cn/en/reports/population-status-children-china-2015. Accessed 28 Mar 2022.
Von Soest T, Kozák M, Rodríguez-Cano R, Fluit DH, Cortés-García L, Ulset VS, et al. Adolescents’ psychosocial well-being one year after the outbreak of the COVID-19 pandemic in Norway. Nat Hum Behav. 2022;6(2):217–28.
Vowels LM, Vowels MJ, Carnelley KB, Millings A, Gibson-Miller J. Toward a causal link between attachment styles and mental health during the COVID-19 pandemic. Br J Clin Psychol. 2023;62(3):605–20.
Wan Y, Chen R, Ma S, McFeeters D, Sun Y, Hao J, Tao F. Associations of adverse childhood experiences and social support with self-injurious behaviour and suicidality in adolescents. Br J Psychiatry. 2019;214(3):146–52.
Wang Y, Liu W, Wang W, Lin S, Lin D, Wang H. Left-behind children’s social adjustment and relationship with parental coping with children’s negative emotions during the COVID-19 pandemic in China. Int J Psychol. 2021;56(4):512–21.
Wang D, Zhao J, Ross B, Ma Z, Zhang J, Fan F, Liu X. Longitudinal trajectories of depression and anxiety among adolescents during COVID-19 lockdown in China. J Affect Disord. 2022;299:628–35.
Wheelock MD, Goodman AM, Harnett NG, Wood KH, Mrug S, Granger DA, Knight DC. Sex-related differences in stress reactivity and cingulum white matter. Neuroscience. 2021;459:118–28.
Wood A, Kroll L, Moore A, Harrington R. Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. J Child Psychol Psychiatry. 1995;36(2):327–34.
Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, et al. Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021;70(24):888–94.
Zaninotto P, Iob E, Demakakos P, Steptoe A. Immediate and longer-term changes in the mental health and well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiat. 2022;79(2):151–9.
Zhang L, Zhang D, Fang J, Wan Y, Tao F, Sun Y. Assessment of mental health of chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2021482.
Zhang XD, Zhao X, Sun HY. The outstanding problems and countermeasures of rural left-behind children. Yunnan Edu. 2015;11(03):9–15.
Zhang YH, Zhang T, Zhao JX. Discrimination perception and loneliness among rural left-behind adolescents: the role of age of parent-child separation and duration of separation. Psychol Dev Educ. 2022;38(1):90–9.
Zhao C, Egger H. Cognitive impact of early separation from migrant parents: a spectrum of risk and key mechanisms in child development contexts. A commentary on Hou et al., (2020). Soc Sci Med. 2020;266:113427.
Acknowledgements
We are extraordinarily grateful to all the children and their caregivers who took part in this study and appreciate the support of the principal and head teachers of the local primary schools. Special thanks to the doctors responsible for the local school check-ups and investigators.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Number: 82173537 and 81872638); and Natural Science Foundation for Distinguished Young Scholars of Anhui Province (Grant Number: 1908085J26).
Author information
Authors and Affiliations
Contributions
YW and PS conceptualized and designed the study. JF and XZ designed the data collection instruments and collected data. SW and PW performed the statistical analyses and wrote the first draft. YS and FT revised the manuscript, and gave the final approval of the version to be published. All authors revised and approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Biomedical Ethics Committee of Anhui Medical University (Project Number 20180082). All respondents and their primary caregivers provided informed consent (through electronic letters sent by mobile devices). All respondents and their primary caregivers provided informed consent (through electronic letters sent by mobile devices).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Enrollment in the study and daily new confirmed COVID-19 cases. Table S1. Comparison of the baseline characteristics of participants included in the analytical sample vs those not included at wave 4. Table S2. Descriptive statistics by different parent–child separation experiences of the mental health outcomes before and during COVID-19. Table S3. Prevalence of mental health outcomes predicted from generalized estimation models before and during COVID-19. Table S4. Generalized estimating models: changes in mental health before and during the COVID-19 pandemic. Figure S2. Standardized Changes in Mental Health Before and During the COVID-19 Pandemic. Table S5. Generalized estimating models: standardized changes in mental health before and during the COVID-19 pandemic. Table S6. Generalized estimating models: interaction effects (time × group) between immediate and longer-term changes in mental health and parent–child separation experiences. Table S7. Moderating effect of socio-demography characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, P., Wang, S., Zhao, X. et al. Immediate and longer-term changes in mental health of children with parent–child separation experiences during the COVID-19 pandemic. Child Adolesc Psychiatry Ment Health 17, 113 (2023). https://doi.org/10.1186/s13034-023-00659-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13034-023-00659-y