Abstract
Background
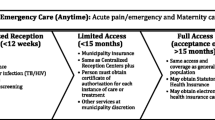
Providing adequate healthcare to newly arrived refugees is considered one of the significant challenges for the German healthcare system. These refugees can be classified mainly into two groups: asylum seekers (who have applied for asylum after arrival in Germany and are waiting for the refugee-status decision) and resettlement refugees (who have already been granted asylum status before arriving in Germany). Whereas earlier studies have explored the health status of asylum seekers especially in terms of mental and behavioural disorders and infectious diseases without distinguishing between these two groups, our study aims to evaluate possible relationships of asylum status and medical needs of these two groups with a special focus on mental and behavioural disorders and infectious diseases.
Methods
In this retrospective observational study, collected data on all asylum-seeker and resettlement-refugee patients (N = 2252) of a German reception centre (August 2017 to August 2018) is analysed by absolute and relative frequencies and medians. Patient data, collected by chart review, include age, gender, country of origin, asylum status, and diagnoses (ICD-10). To describe the relationship between sociodemographic factors (including asylum status) and diagnoses, we used tests of significance and bivariate correlations with Spearman correlation coefficients. All collected data are pseudonymised.
Results
Of all 2252 patients, 43% were resettlement refugees. In almost all ICD-10 categories, asylum seekers received significantly more diagnoses than resettlement refugees. According to our data, asylum seekers presented with mental and behavioural disorders nine times more often (9%) than resettlement refugees (1%). In the case of infectious diseases, the results are mixed: asylum seekers were twice as frequently (11%) diagnosed with certain infectious and parasitic diseases than resettlement refugees (5%), but resettlement refugees were treated twice as often (22% of the asylum seekers and 41% of the resettlement refugees) for diseases of the respiratory system, of which 84% were acute respiratory infections (in both groups).
Conclusion
This study indicates that patients with unregulated migration more frequently present symptoms of psychiatric diseases and somatoform symptoms than resettlement refugees. A health policy approach within migration policy should aim to enable persecuted persons to migrate under regulated and safe conditions.
Trial registration
German Clinical Trials Register: DRKS00013076, retrospectively registered on 29.09.2017.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
As a result of the ongoing global migrant and refugee crisis, medical conditions and needs of recently arrived refugees are an increasingly frequent subject of research [1,2,3,4], especially in terms of infectious diseases and mental health issues. For infectious diseases, studies verify partly poor vaccination conditions and high rates of bacterial and viral respiratory system infections among newly arrived refugees [5,6,7,8]. Publications regarding mental health issues in their turn show higher rates of anxiety, depression, traumatisation, and post-traumatic stress disorder, as well as symptoms of somatisation [9, 10].
The relationship between refugee or asylum conditions on the one hand and the medical needs of refugees on the other has not been scientifically studied so far. Nonetheless, evidence suggests that conditions related to escape, such as experiences of uncertainty and lack of control over current/future life, strongly influence the health status of affected people and place them at high risk for psychosocial distress [11]. During a long migration process, overcrowding, inadequate water supply, malnutrition, poor sanitation, and physical and psychological stress also predispose refugees to several infectious diseases [2, 7]. Riccardo et al. (2015) identified migration-specific risks for infectious diseases, such as country of origin and migration trajectory, and migration-specific health access barriers that differ according to the migration status [12]. Based on this background, we were interested to determine whether a correlation between escape conditions and medical needs of newly arrived refugees could be found.
Refugee status is a very strong indicator of escape conditions. The United Nations High Commission for Refugees (UNHCR) distinguishes between “internally displaced people” (40 million worldwide who fled within their home country), “refugees” (25.4 million worldwide who fled outside their home country) and “asylum-seekers” (3.1 million worldwide whose request for sanctuary has yet to be processed). Eighty-five percent of the world’s displaced people are hosted in developing countries. The top refugee-hosting countries are Turkey (3 million refugees), Uganda (1.4 million refugees), Pakistan (1.4 million refugees), Lebanon (1 million refugees), and Iran (979,400 refugees) [13]. A subgroup of the 25.4 million refugees is the group of 102,800 resettled refugees. These resettlement refugees have no prospects of becoming integrated into the first country they entered as refugees and are unable to return to their home countries. The UNHCR resettlement programme intends to permanently redistribute refugees from third countries for purposes of humanitarian reception. At their arrival in the new hosting country, resettlement refugees have already gone through the UNHCR refugee-status determination process and therefore do not need to apply for asylum there. In addition to Germany, other European countries (e.g. the United Kingdom, Sweden, and France) as well as the United States, Canada, and Australia take part in the UNHCR resettlement programme.
The UNHCR defines the following categories for resettlement submission: legal and/or physical protection, medical needs (in particular, life-saving treatment that is unavailable in the initially receiving country), women and girls at risk, family reunification, children and adolescents at risk, and lack of foreseeable alternative durable solutions [14].
Displaced people who have legal residence status in western industrialised nations can be divided into two groups: asylum seekers, and resettlement refugees. These two groups differ significantly in their escape conditions and their legal status [15]. In addition to these two groups, there are refugees without legal residence status. Due to the lack of registration, no valid data is available for this group. Therefore, they are not taken into account here.
Asylum seekers and resettlement refugees in Germany
In Germany, most refugees arrive as asylum seekers after having followed an individual escape route through several countries. They apply for asylum recognised under the German asylum law or the Geneva Convention [16]. Almost 200,000 asylum applications were submitted in 2017 and about 150,000 in 2018. Most asylum seekers came from Syria (25%), Iraq (11%), Afghanistan (8%), and Eritrea (5%) [17]. Asylum seekers are initially housed in refugee camps in various locations in Germany (usually several weeks to months) before they are assigned to other dormitories or move to individual apartments with supervision and support of the social services.
The number of resettlement refugees is much smaller than that of asylum seekers: 3867 resettlement refugees (mainly of Syrian nationality) arrived in Germany in 2017 [18], of which 2988 came from refugee camps in Lebanon and Turkey [19]. In addition to UNHCR submission categories, resettlement refugees who wish to come to Germany must also meet at least one of the following criteria: preservation of the integrity of the family unit; family or other ties to Germany that promote integration; the ability to become integrated (e.g. the level of schooling/vocational training received, work experience, knowledge of the language); or a degree of vulnerability [20,21,22].
With the exception of people with medical conditions that are so serious that they need immediate hospital treatment, all resettlement refugees in Germany are first sent to the transit camp in Friedland, Lower Saxony. Here they are given initial admission forms, and after a welcoming course, they are distributed to other German Federal States [22].
Safe escape routes have for a long time been part of the political demands because they can contribute significantly to the physical and mental state of health of refugees. In addition, medical needs (in particular, life-saving treatment that is unavailable in the initially receiving country) are part of the five categories for resettlement submission of the UNHCR.
Regarding the conditions of escape and residence, Table 1 shows the main differences between asylum seekers and resettlement refugees. These differences may result in greater physical and psychological stress that asylum seekers suffer compared to resettlement refugees. Our hypothesis is that these differences indicate that asylum seekers have higher medical needs, particularly in regard to infectious diseases, mental and behavioural disorders.
The aim of this study therefore is to project the possible medical needs of asylum seekers and resettlement refugees by means of their utilization of health services resulting in the medical diagnoses given by the general practitioners. The focus is on mental and behavioural disorders and infectious diseases through analysis of primary care medical charts.
Methods
Setting
The transit camp in Friedland was founded in 1945 in the middle of Germany at the former border between East and West Germany in Lower Saxony. Since its foundation, it has accommodated over 4 million people arriving in the Federal Republic of Germany [10]. The camp has a capacity of 1000 beds and is operated by about 100 employees. The transit camp has a primary healthcare centre, which is run by six part-time general practitioners (GPs) and nurses. Consultation hours are Monday through Friday for 2–3 h. Asylum seekers and resettlement refugees who are housed in Friedland have to visit during these consultation hours for any type of medical care, except in case of emergency. This enabled us to record an almost full survey of all resettlement refugees coming to Germany and additionally all asylum seekers housed in Friedland. To minimise the influence of the different lengths of stay of asylum seekers and resettlement refugees, we calculated a weighting factor of 1.86 for resettlement refugees based on person days (number of attendance days in the camp of resettlement refugees (N = 39,347) and asylum seekers (N = 73,532)). This weighting was used for all further analyses, except for sociodemographic data.
Data management
We here analyse data of all 2252 resettlement-refugee and asylum-seeker patients who visited the primary healthcare centre in Friedland between 15 August 2017 and 15 August 2018 (366 days). The patient data were collected by chart review and included age, gender, country of origin, asylum status, and diagnoses. All collected data are pseudonymised. A detailed description of the project was published elsewhere [23]. All diagnoses and symptoms were coded according to the International Classification of Diseases (ICD-10). The results were converted into dichotomous variables. Additionally, a new variable “somatoform symptoms” was calculated. This variable includes diffuse symptoms such as headaches, nausea, dizziness, or insomnia (complete presentation can be found in Additional file 1) if they were not associated with any other disease explaining the symptom. The variable “somatoform symptoms” serves to supplement the diagnoses of mental and behavioural disorders (F00-F99). These diagnoses can be difficult to assess due to the short duration of treatment and severe language barriers. Some symptoms must persist for a certain period of time in order to be diagnosed (e.g., symptoms as lowering of mood, reduction of energy, or decrease in activity must be present for at least 2 weeks to diagnose depression). Therefore, it can be assumed that residents of initial reception facilities are underdiagnosed regarding mental and behavioural disorders.
Infectious diseases were recorded using ICD-10 category A00-B99, that is, certain infectious and parasitic diseases. Management of infectious respiratory diseases in primary care does not depend mainly on laboratory results but on clinical presentation, therefore we also took acute diagnoses of respiratory diseases (J00-J22) into account. The five most common diagnoses of asylum seekers and resettlement refugees within all ICD-10 chapters are shown in Additional file 2.
The statistical software package IBM SPSS statistics 25 was used for all analyses. Sociodemographics were described by absolute and relative frequencies and by medians. For a group comparison of diagnoses, we split the sample into the two groups of refugees (asylum seekers and resettlement refugees). Differences between the two groups were tested using Fisher’s exact test. For differences in age, the Mann-Whitney U test was used. The influence of age, gender, and asylum status on diagnoses and prescriptions was measured using bivariate correlations with Spearman correlation coefficients.
Results
Within the observed time, a total of 5206 people (2140 asylum seekers (41%) and 3066 resettlement refugees (59%)) were temporarily accommodated in the transit camp in Friedland. Of these 5206 attendees, 2252 persons (43%) had at least one regular consultation at Friedland primary healthcare centre. Therefore, 1293 (60%) of all present asylum seekers and 959 (30%) of all present resettlement refugees are regarded as patients. Fifty-one percent of asylum-seeker patients and 49% of resettlement-refugee patients were female.
Asylum-seeker patients mostly came from Iraq (17%), Syria (11%), Georgia (11%), Afghanistan (10%), and Iran (8%). For resettlement-refugee patients, the country in which they had applied for resettlement was registered instead of their country of origin. At least 81% of these patients were Syrians. The median age of all patients was 26 years, SD 18.529 (asylum seekers: 27 years, range 0–79; resettlement refugees: 20 years, range 0–81, p = 0.001). Figure 1 shows that there are more children than adults among the resettlement refugees. Twenty-nine percent of asylum seekers and 48% of resettlement refugees were younger than 18 years.
Most frequent symptoms of illness in medical consultations
Of all 2252 patients, 2054 patients (91.2%) received at least one diagnosis according to ICD-10. Figure 2 shows that 43% of asylum-seeker patients and 42% of resettlement-refugee patients presented diagnoses in the category R00-R99, which includes symptoms, signs, abnormal clinical and laboratory findings, and ill-defined conditions for which no diagnosis classifiable elsewhere is recorded. Most common diagnoses in this category are cough, headache, sore throat, fever and abdominal pain. These unspecific codes are very common in general practice in Germany. Other common reasons for consultation are diseases of the respiratory system (22% of asylum seekers, 41% of resettlement refugees) and diseases of the musculoskeletal system and connective tissue (18% of asylum seekers and 10% of resettlement refugees). Considering only adult patients, 42% of asylum seekers and 35% of resettlement refugees presented symptoms, signs, and abnormal clinical and laboratory findings in the category R00-R99 (p ≤ 0.01), and 14% of asylum seekers and 28% of resettlement refugees had diseases of the respiratory system (p ≤ 0.001). Diseases of the musculoskeletal system were represented slightly more frequently than in the overall sample, with 23% for asylum seekers and 19% for resettlement refugees (p ≤ 0.05). In total, asylum seekers were diagnosed more frequently in almost all diagnostic categories. Resettlement refugees, on the other hand, were only more frequently affected by respiratory and ear diseases. This difference also persists when only adult patients are considered.
Mental and behavioural disorders
Regarding mental and behavioural disorders, Fig. 2 shows that 9% of asylum seekers and 1% of resettlement refugees have received diagnoses in the category F00-F99 (p ≤ 0.001). This effect increases when only adult patients are considered (11% of asylum seekers, and 1% of resettlement refugees). The most frequent diagnoses were depressive episodes, reaction to severe stress, and adjustment disorders as well as other anxiety disorders (see Table 2). In addition, 15% of asylum seekers (N = 194) and 7% of resettlement refugees (N = 117) presented somatoform symptoms (p ≤ 0.001).
In summary, 24% of asylum seekers (N = 304) and 7% of resettlement refugees (N = 132) sought medical help for mental health problems.
Infectious diseases
To detect infectious diseases, we used the ICD-10 category certain infectious and parasitic diseases (A00-B99). As shown in Fig. 2, 11% of asylum seekers and 5% of resettlement refugees have received diagnoses from this category (p ≤ 0.001), with gastroenteritis and colitis, scabies, and chronic viral hepatitis as the most frequent diagnoses (see Table 3).
The relation between asylum seekers and resettlement refugees is reversed in the diagnoses of respiratory diseases: 22% of asylum seekers and 41% of resettlement refugees received such a diagnosis (see Fig. 2).
In both groups, 84% of all “J-diagnoses” concern acute infectious diseases (J00-J22). Most common are acute upper respiratory infections, followed by other acute lower respiratory infections (see Table 4).
Sociodemographic factors influencing mental illnesses and infectious diseases
Regarding the hypothesis that asylum seekers have higher medical needs in relation to treatments for mental and behavioural disorders and infectious diseases, Table 5 shows bivariate correlations for these diagnoses and symptoms. Accordingly, there are slightly negative correlations between asylum status and mental and behavioural disorders, and somatoform symptoms as well as certain infectious and parasitic diseases. This supports the hypothesis that asylum seekers are more frequently affected by all these diagnoses than resettlers, but resettlement refugees are more often affected by diseases of the respiratory system. However, age also has a significant influence in the sense that adult patients are more often affected by mental and behavioural disorders and somatoform symptoms. Children and adolescents younger than 18 years, on the other hand, are more frequently affected by certain infectious and parasitic diseases and diseases of the respiratory system. Gender has only a weak influence on the diagnosis of somatoform symptoms in the sense that women are slightly more likely to seek medical help with somatoform symptoms. Gender had no influence on mental and behavioural disorders and certain infectious and parasitic diseases (see Table 5).
To preclude the influence of age, Table 6 shows bivariate correlations only on patients older than 18 years. The highly significant correlations between asylum status and diagnostic groups clearly still persist, although there are minimal shifts. In mental and behavioural disorders and certain infectious and parasitic diseases, the effect increases somewhat, whereas it decreases slightly in somatoform symptoms and diseases of the respiratory system.
Discussion
Based on the background of different conditions of escape and residence, diagnoses of newly arrived asylum seekers and resettlement refugees in an on-site primary healthcare ward in an initial reception centre were recorded. To our knowledge, this is the first survey that acquired diagnoses of almost the complete group of resettlement refugees in Germany and gives a direct comparison with asylum seekers in the same setting. We found significantly more diagnoses in the field of specific infectious diseases and especially psychiatric disorders in the group of asylum seekers. According to our data, asylum seekers presented with mental and behavioural disorders nine times more often (9%) than resettlement refugees (1%). Somatoform symptoms (e.g. headaches, nausea, unspecific abdominal pain, and insomnia) were diagnosed more frequently in both groups. This may be because a diagnosis of a mental and behavioural disorder requires more background information of the patients and a long observation period, which was not possible in this context. The limited length of stay and existing language barriers often prevent a detailed psychosocial anamnesis, especially in Friedland, where interpreters are usually rarely available during medical consultations. Under these conditions, it is difficult to diagnose a mental and behavioural disorder, and the GPs only describe somatoform symptoms. However, somatoform symptoms were also diagnosed twice as often in asylum seekers (15%) than in resettlement refugees (7%). On one hand, these results correspond to the risk factors described in the literature, such as insecurity about current life and future [11, 24], to which asylum seekers are much more exposed. Similarly, resettlement refugees most probably also experienced traumatic events, but since their trip to Germany is already organized, they travel in much better conditions and have a secure perspective, while for asylum seekers the uncertainty remains for a longer period of time. On the other hand, it is also possible that resettlement refugees do not consult a physician because they know that they will reach their final residence 2 weeks later and then will be allowed to use regular healthcare services. However, this risk of bias appears to be quite low because Wetzke et al. (2018) were able to show in a comparable initial reception centre that asylum seekers most often sought medical help during the first week and that their use of the medical services decreased with longer periods of stay [25].
These data do not straightforwardly support our hypothesis that asylum seekers suffer more frequently from infectious diseases than resettlement refugees. However, the evidence from this study shows that asylum seekers were diagnosed twice as frequently with certain infectious and parasitic diseases (e.g., scabies, hepatitis C, gastroenteritis) but only half as often for acute infectious respiratory diseases. These differences may be due to different escape conditions, like inadequate water supply, malnutrition, poor sanitation, and lack of medical care (regarding asylum seekers) [2, 7] or group accommodation and flights (regarding resettlement refugees): There is some evidence that air-conditioning systems used in airplanes might increase the incidence of upper respiratory symptoms, which could explain the higher prevalence of acute infectious respiratory diseases in resettlement refugees in our data [26,27,28].
Our study is limited by a lack of systematic screening regarding infectious diseases or mental and behavioral disorders, thus only refugees who presented to medical care could be included in this study. The diagnosis was mainly based on the clinical judgement of the experienced general practitioners, laboratory or standardised mental health questionnaires were rarely used. A further aspect is the retrospective study design, which made it impossible to take other influencing factors into account (e.g. physical and psychological living conditions before and during the escape journey or changes in political conditions in the countries of origin during the study period). However, the influence of age and gender of refugees were controlled on the basis of sociodemographic data, with women presenting slightly more often with somatoform symptoms than men. Age had a much greater influence than gender, especially on respiratory diseases, which affected children significantly more often than adults. Even after children were excluded, a highly significant correlation between asylum status and all diagnostic groups remains, with asylum seekers receiving diagnoses with mental and behavioural disorders, somatoform symptoms, and certain infectious and parasitic diseases more frequently than resettlement refugees, even though the effect is rather weak. Small correlations can best be identified in studies with large samples, which is a major strength of this study. Here, medical data of almost all resettlement refugees coming to Germany during their first weeks of stay are presented for the first time.
Conclusions
The increasing population of refugees and asylum seekers poses new challenges to the healthcare systems of the receiving host countries and communities. The present study shows that asylum seekers seem to need more healthcare service than resettlement refugees in the context of an initial reception center with regard to psychological disorders and symptoms as well as specific infectious and parasitic diseases. To reduce the need for medical treatment in these settings, resettlement programs may be considered a better alternative that will enable a planned safe migration with more secure prospects, for host countries and migrants.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AS:
-
Asylum Seeker
- GP:
-
General Practitioner
- ICD-10:
-
International Classification of Diseases
- RR:
-
Resettlement Refugee
- UNHCR:
-
United Nations High Commission for Refugees
References
Frank L, Yesil-Jürgens R, Razum O, Bozorgmehr K, Schenk L, Gilsdorf A, et al. Gesundheit und gesundheitliche Versorgung von Asylsuchenden und Flüchtlingen in Deutschland: health and health care of asylum seekers and refugees in Germany [article in German]. J Health Monit. 2017;2(1):24–47. https://doi.org/10.17886/RKI-GBE-2017-005
Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med. 2017;24. https://doi.org/10.1093/jtm/tax016.
Rojek AM, Gkolfinopoulou K, Veizis A, Lambrou A, Castle L, Georgakopoulou T, et al. Clinical assessment is a neglected component of outbreak preparedness: evidence from refugee camps in Greece. BMC Med. 2018;16:43. https://doi.org/10.1186/s12916-018-1015-9.
van Loenen T, van den Muijsenbergh M, Hofmeester M, Dowrick C, van Ginneken N, Mechili EA, et al. Primary care for refugees and newly arrived migrants in Europe: a qualitative study on health needs, barriers and wishes. Eur J Pub Health. 2018;28:82–7. https://doi.org/10.1093/eurpub/ckx210.
Jablonka A, Behrens GMN, Stange M, Dopfer C, Grote U, Hansen G, et al. Tetanus and diphtheria immunity in refugees in Europe in 2015. Infection. 2017;45:157–64. https://doi.org/10.1007/s15010-016-0934-7.
Jablonka A, Happle C, Grote U, Schleenvoigt BT, Hampel A, Dopfer C, et al. Measles, mumps, rubella, and varicella seroprevalence in refugees in Germany in 2015. Infection. 2016;44:781–7. https://doi.org/10.1007/s15010-016-0926-7.
Doganay M, Demirasalan H. Refugees of the Syrian civil war: impact on reemerging infections, health services, and biosecurity in Turkey. Health Secur. 2016;14:220–5.
Redditt VJ, Janakiram P, Graziano D, Rashid M. Health status of newly arrived refugees in Toronto, Ont: part 1: infectious diseases. Can Fam Physician. 2015;61(7):e303–9.
Schweitzer RD, Vromans L, Brough M, Asic-Kobe M, Correa-Velez I, Murray K, Lenette C. Recently resettled refugee women-at-risk in Australia evidence high levels of psychiatric symptoms: individual, trauma and post-migration factors predict outcomes. BMC Med. 2018;16:149. https://doi.org/10.1186/s12916-018-1143-2.
Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302:537–49. https://doi.org/10.1001/jama.2009.1132.
Bjertrup PJ, Bouhenia M, Mayaud P, Perrin C, Ben Farhat J, Blanchet K. A life in waiting: Refugees’ mental health and narratives of social suffering after European Union border closures in march 2016. Soc Sci Med. 2018;215:53–60. https://doi.org/10.1016/j.socscimed.2018.08.040.
Riccardo F, Dente MG, Kärki T, Fabiani M, Napoli C, Chiarenza A, et al. Towards a European framework to monitor infectious diseases among migrant populations: design and applicability. Int J Environ Res Public Health. 2015;12:11640–61. https://doi.org/10.3390/ijerph120911640.
United Nations High Commissioner for Refugees (UNHCR). Figures at a glance. 2018. http://www.unhcr.org/figures-at-a-glance.html.
United Nations High Commissioner for Refugees. UNHCR Resettlement Handbook. 2011.
Kinlen L. Welcome to Ireland: seeking protection as an asylum seeker or through resettlement—different avenues, different reception. Refuge - Canada's Journal on Refugees. 2011;8:31–47.
Federal Office for Migration and Refugees. Asylum and refugee protection. 2018. http://www.bamf.de/EN/Fluechtlingsschutz/fluechtlingsschutz-node.html.
Bundesamt für Migration und Flüchtlinge. Aktuelle Zahlen zu Asyl. 2018.
United Nations High Commissioner for Refugees (UNHCR). Resettlement Data Finder. http://rsq.unhcr.org/en/#C0Kq. Accessed 15 May 2019.
resettlement. de. Aktuelle Aufnahmen. http://resettlement.de/aktuelle-aufnahmen/. Accessed 5 Jan 2018.
BAMF - Bundesamt für Migration und Flüchtlinge - Resettlement and humanitarian reception. http://www.bamf.de/EN/Fluechtlingsschutz/HumAufnahmeResettlement/ResettlementHumanitaereAufnahme/resettlement-node.html. Accessed 22 Jan 2018.
Federal Office for Migration and Refugees. Resettlement and humanitarian reception. 2018. http://www.bamf.de/EN/Fluechtlingsschutz/HumAufnahmeResettlement/ResettlementHumanitaereAufnahme/resettlement-node.html.
Baraulina T, Bitterwolf M. Resettlement in Germany – what is the programme for particularly vulnerable refugees accomplishing? In: Brief analyses of the migration, Integration and asylum research Centre at the Federal office for migration and refugees; 2018. p. 1–13.
Furaijat G, Kleinert E, Simmenroth A, Müller F. Implementing a digital communication assistance tool to collect the medical history of refugee patients: DICTUM Friedland - an action-oriented mixed methods study protocol. BMC Health Serv Res. 2019;19:103. https://doi.org/10.1186/s12913-019-3928-1
Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294:602–12. https://doi.org/10.1001/jama.294.5.602.
Wetzke M, Happle C, Vakilzadeh A, Ernst D, Sogkas G, Schmidt RE, et al. Healthcare utilization in a large cohort of asylum seekers entering Western Europe in 2015. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15102163.
Zitter JN, Mazonson PD, Miller DP, Hulley SB, Balmes JR. Aircraft cabin air recirculation and symptoms of the common cold. JAMA. 2002;288:483–6.
Svendsen IS, Taylor IM, Tønnessen E, Bahr R, Gleeson M. Training-related and competition-related risk factors for respiratory tract and gastrointestinal infections in elite cross-country skiers. Br J Sports Med. 2016;50:809–15.
Whelan EA, Lawson CC, Grajewski B, Petersen MR, Pinkerton LE, Ward EM, Schnorr TM. Prevalence of respiratory symptoms among female flight attendants and teachers. Occup Environ Med. 2003;60:929–34.
Acknowledgements
We acknowledge the efforts and help of Malteser Friedland, the social services office at Friedland transit camp, the Landesaufnahmebehörde Niedersachsen (Migration Authority of Lower Saxony), and Karin Patock (BAMF - Bundesamt für Migration und Flüchtlinge - Resettlement and humanitarian reception).
Funding
The study is funded by the Robert Bosch Foundation, the state of Lower Saxony (the subsidy guidelines for the healthcare region), and the European Social Fund (the subsidy guidelines for social innovation). The funding body played no role in the design of the study and collection, analysis, and interpretation of data.
Author information
Authors and Affiliations
Contributions
EK and FM were mainly responsible for the analysis and interpretation of data and share first authorship. Data collection and data preparation was primarily led by FM and NH. EK wrote the manuscript with support of GF. Study design was mainly contributed by FM and AS. AJ and CH provided substantially input for the interpretation of findings. All authors revised critically and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was given by the ethics committee of the University Medical Centre Göttingen (Ethics Approval No. 18/5/16). All participants provided voluntary informed consent and consent to publish anonymized, grouped data.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Somatoform symptoms. (DOCX 13 kb)
Additional file 2:
Overview diagnoses. (DOCX 21 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kleinert, E., Müller, F., Furaijat, G. et al. Does refugee status matter? Medical needs of newly arrived asylum seekers and resettlement refugees - a retrospective observational study of diagnoses in a primary care setting. Confl Health 13, 39 (2019). https://doi.org/10.1186/s13031-019-0223-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13031-019-0223-z