Abstract
Background
Generalised anxiety disorder (GAD) is a frequent and severe disorder among older adults. For older adults with GAD the effect of the recommended treatment, cognitive behaviour therapy (CBT), is reduced. Physical exercise (PE) may enhance the effect of CBT by improving cognitive function and increasing levels of brain-derived neurotrophic factor (BDNF), a predictor of the effect of CBT in patients with anxiety. The aim of the study was to assess the feasibility of a randomized controlled trial (RCT) investigating treatment effect of the combination of CBT and PE for GAD in a sample of older adults, including procedures for assessment and treatment.
Methods
Four participants aged 62–70 years (M = 65.5, SD = 3.2) with a primary diagnosis of GAD were included. Participants received 15 weeks of PE in combination with 10 weeks of CBT. Participants completed self-report measures, and clinical, biological, physiological and neuropsychological tests at pre-, interim- and post-treatment.
Results
Procedures, protocols, and results are presented. One participant dropped out during treatment. For the three participants completing, the total adherence to PE and CBT was 80% and 100%, respectively. An independent assessor concluded that the completers no longer fulfilled the criteria for GAD after treatment. Changes in self-report measures suggest symptom reduction related to anxiety and worry. The sample is considered representative for the target population.
Conclusions
The results indicate that combining CBT and PE for older adults with GAD is feasible, and that the procedures and tests are suitable and manageable for the current sample.
Trial registration
ClinicalTrials.gov, NCT02690441. Registered on 24 February 2016, https://clinicaltrials.gov/ct2/show/NCT02690441.
Similar content being viewed by others
Introduction
Generalised anxiety disorder (GAD) is a severe disorder characterised by profound and uncontrollable worry and associated with symptoms such as restlessness, fatigue, muscle tension, irritability, difficulty concentrating, and sleep problems [1].
Cognitive behaviour therapy (CBT) is the recommended treatment [2] and has been found to be more effective as treatment for GAD compared to passive control conditions [3]. However older adults are less responsive to treatment than younger adults [4, 5]. The reduced effect of CBT for older adults with GAD may be explained by age-related cognitive changes or decline in executive functions [6,7,8]. An approach to enhance the effect of CBT has been to add physical exercise (PE) to the treatment [9]. PE improves cognitive function [10], increases brain volume in prefrontal and temporal cortices in non-demented older adults [11] and is associated with increased brain plasticity and cognitive function through the mechanisms of the neurotrophin brain-derived neurotropic factor (BDNF; 12). BDNF has a protective effect on brain health [13], and levels are reduced in patients with depression and anxiety [14, 15]. An increase in BDNF levels through PE can enhance the ability to learn and remember new material. These effects are hypothesised to an enhancement of the effect of CBT in older adults with GAD [16].
There are no previous studies investigating the combination of CBT and PE in older adults with GAD. Previous studies have shown that PE is feasible in the treatment of anxiety disorders [17,18,19] and also specifically in GAD [20,21,22]. The main aim of this study is to investigate the feasibility of the combination of CBT and PE in a sample of older adults with GAD as a precursor to a RCT. The RCT study protocol has been published elsewhere [16].
Objectives
The objectives of the study are (1) to evaluate the feasibility of combining CBT and PE for older adults with GAD, (2) to assess the feasibility of test protocols and scheduled time frames and (3) to troubleshoot screening and inclusion procedures. Results from the questionnaires and physical manipulation checks are discussed.
Methods
Design
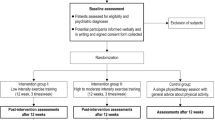
The study had a single-arm design and all participants received CBT combined with PE. The participants completed pre-treatment, interim and post-treatment measures. Figure 1 displays the feasibility study design.
Participants
The participants were recruited from an outpatient, psychiatric secondary care-clinic. Inclusion criteria were (1) age between 60 and 75 years; (2) a primary diagnosis of GAD as evaluated by the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; 23). Exclusion criteria were: (1) substance abuse; (2) habitual use of benzodiazepines; (3) changes in the dose of other psychotropic medication during the study; (4) medical conditions that preclude participation in physical testing and/or PE; (5) severe major depression as determined by the Mini-International Neuropsychiatric Interview (M.I.N.I.; 24, 25), a structured interview for psychiatric disorders in the DSM-IV; (6) life-time history of psychosis and/or mania; (7) participation in other ongoing psychotherapy; (8) organic brain disease; (9) a score of 25 or less on the Mini Mental State Examination (MMS-E; 26), a measure for grading cognitive state and (10) physical exercise of moderate intensity of 60 min or more of two or more sessions per week during an average week for the last three months.
Assessment for eligibility
For eligibility assessment potential participants met twice with a project coordinator (a clinical psychologist) for completion of the Generalized Anxiety Disorder Questionnaire (GAD-7) [27], the GAD-module in the ADIS-IV interview [23], the M.I.N.I [24, 25]., and the MMS-E [26]. Level of physical activity was assessed by registering physical activity during an average week for the last three months.
Interventions
Cognitive behaviour therapy. The CBT intervention consisted of an initial session focused on providing rapport and information, and 10 weekly sessions of 60 min of individual manualised CBT. The CBT intervention was based on Borkovec’s protocol for treatment of GAD [28]. Prior to the feasibility study, the therapists had completed one practice treatment with the CBT manual which were video rated by an independent assessor using the Cognitive Therapy Adherence and Competence Scale [29].
Physical exercise. The PE intervention consisted of 15 weekly supervised and unsupervised individual sessions of resistance and aerobic training, each scheduled to last 45–60 min. Both resistance and aerobic training intensity levels progressed every five weeks. Supervised sessions were led by physiotherapists or an occupational therapist.
Assessments
Questionnaires. The following inventories was administered: The Penn State Worry Questionnaire (PSWQ) [30], the Beck Anxiety Inventory (BAI) [31], the Beck Depression Inventory – II (BDI-II) [32], the Generalized Anxiety Disorder Questionnaire (GAD-7) [27], the Geriatric Anxiety Inventory (GAI) [33], the Bergen Insomnia Scale (BIS) [34], the Credibility/Expectancy Questionnaire [35], the International Physical Activity Questionnaire (IPAQ-short) [36, 37] and a questionnaire for treatment satisfaction post treatment.
Physical measures. The Ekblom-Bak submaximal cycle ergometer test [38] and the Five-Minute Pyramid test [39] were used for assessing aerobic fitness. Four endurance muscle strength tests measured functional physical strength; the Biering-Sørensen test [40] for back muscle strength, a Timed sit-to-stand test (50 times) as a measure of lower-extremity strength, a 45-degree sit-up test for core muscle strength and a dumbbell arm press test for arm and shoulder strength.
Other measures. All measures for the RCT were tested during the feasibility study. The results from these measures are not indicative of the feasibility, and thus not reported. A description of all measures is available elsewhere [16].
Test procedures
Pre- and post-measures were distributed across four days (Fig. 2 displays the distribution of measures). Pre-measures were conducted within two weeks of recruitment and post-measures were conducted within two weeks and completed not more than two weeks after finishing treatment. The interim test was distributed over two days. The interim test was conducted within one week, and not more than one week after finishing pre-treatment.
Statistics
Means (M) and standard deviations (SD) for questionnaires and test results were calculated with IBM SPSS Statistics, version 26 [41] to determine the reliable change index (RCI). The RCI was calculated using the procedure described by Evans and colleagues [42] and Zahra and Hedge [43]. Criteria C from Evans and colleagues [42], which estimates greater likelihood of the patient being in the normative distribution than a clinical distribution after treatment was used to determine the clinical cut off point for the varying measures. The mean and standard deviations for the norm and clinical populations were calculated using the source papers for the Penn State Worry Questionnaire [44], the Beck Anxiety Inventory [45], the Beck Depression Inventory II [46, 47], the Geriatric Anxiety Inventory [33], the Generalized Anxiety Disorder Questionnaire [48], and the Bergen Insomnia Scale [49]. Likewise, the reliability of each measure was the Cronbach’s alpha for each measure. Due to the small sample size in the current study, alpha from the abovementioned source papers were used.
Results
Participant flow
A total of 22 potential participants were assessed for participation (see Fig. 3 for study flow), and nine were considered eligible according to the inclusion- and exclusion criteria. Five subjects decline to participate, with reference to the expected demand of the overall treatment protocol. Four participants were included in the study. The remaining 18 potential participants were excluded according to the exclusion criteria. Excluded patients needing other treatment and/or care were ensured this.
One participant dropped out seven weeks after reporting challenges with combining ongoing treatment with household chores. Results from the three participants who completed the treatment are included in analyses of changes due to intervention. Results from the drop-out participant are included in reports of baseline characteristics. Baseline data displaying demographic and clinical characteristics of the sample is seen in Table 1.
Feasibility data
Completing participants attended 10 CBT sessions (100%), while the drop-out participant attended three CBT sessions (30%). Completers attended 93.3% and 73.3% of supervised and unsupervised PE sessions, respectively, resulting in a total adherence to PE of 80% for completers. The drop-out participant completed seven supervised PE sessions and 12 unsupervised sessions and attended all treatment while still participating. Individual rates of adherence are displayed in Table 2.
Completers adhered 100% to test-protocols at pre-, interim and post-measurement points. The drop-out participant completed all pre- and interim tests and hence had a total of 67% adherence to test-protocols.
All pre- and post-tests were finished within two weeks, respectively. All interim tests were completed within one week, and a maximum of one week after completion of the pre-treatment period. All post-tests started a maximum of two weeks after completed treatment.
Treatment outcomes
Results from each participant are presented in Tables 3 and 4.
Clinical rating. None of the completing participants were assessed as fulfilling criteria for GAD after completion of the treatment after an independent assessment with the GAD-module in ADIS-IV [23].
Primary outcome measure. Table 3 displays individual scores on the PSWQ [34]. Completers had a statistically reliable change as shown by the RCI on the PSWQ from pre- to post-measures. None had a clinically significant change according to the clinical cut-off point as determined by Method C from Evans and colleagues [42].
Secondary outcome measures – questionnaires. Individual scores on the outcome measures BAI [31], BDI-II [32], GAI [33], GAD-7 [27], and BIS [34] are displayed in Table 3. The table also shows the RCI and the clinical cut-off point as determined by Method C from Evans and colleagues [42]. Completers in general showed a statistically reliable change in scores on the anxiety measures BAI, GAI and GAD-7. They additionally changed from above to below clinical cut-off on the BAI and GAD-7. The results for the BDI-II and BIS are mixed, with two out of three participants not showing a statistically reliable change nor a reduction in scores that changed from the clinical to the normal range. All participants had a reduction in scores on the BDI-II. On BIS, two participants had elevated scores from pre- to post-measures.
Participant treatment satisfaction and expectancy/credibility to treatment. Completers filled out a treatment satisfaction questionnaire. Participants reported satisfaction with treatment, that they had changed “quite much” in a positive direction, and that other people had noticed this change. Participants reported that they were “mostly satisfied” with the changes. One participant reported “exclusively positive effects” and one reported “no unfortunate effects of any matter”. One reported “some unfortunate effects” and referred to a strain injury that incurred during PE. Participants reported that the treatment fitted their problems well. All three participants reported that the treatment was “somewhat demanding”, and that they “complied overall well” with treatment demands.
Participants had a mean pre-treatment score of 7.8 (SD = 0.59) on the Expectancy/Credibility scale [35] and an increase in mean post-treatment score to 8.2 (SD = 1.46).
Manipulation check for physical exercise
Results from physical testing pre- and post-treatment showed that completers improved their aerobic physical fitness with an average of 10.7% on the Five-Minute Pyramid test [39] and 18.2% on the The Ekblom-Bak submaximal cycle ergometer test [38]. The completing participants improved their physical strength with an average of 13.7% on the Biering-Sørensen test, 20.6% on the Timed sit-to-stand test, 122.5% on the 45-degree sit-up test, and 47% on the Dumbbell arm press test. One participant had a decrease in results on the Biering-Sørensen test and Dumbbell arm test as a consequence of engaging in heavy physical activity the day before testing. Individual test results are shown in Table 4.
Discussion
Adherence to treatment, test protocols and time frames
The current study showed that the CBT + PE protocol for older adults with GAD is feasible. It appears somewhat more challenging for the participants to adhere to unsupervised PE sessions than the supervised PE sessions. Evaluation indicated that the drop-out was not related to structure or organization of the combined treatment. Additionally, completers reported adequate treatment satisfaction, that the treatment was somewhat demanding, but that they complied quite well with the treatment.
Test protocols were evaluated as feasible. The high adherence may be explained by the participants` motivation to learn about their own physical and mental health, and positive attitudes towards research.
Feasibility of screening and inclusion
The study resulted in two two-hour screening appointments, contrary to an initial three hours per appointment. Regarding the inclusion process, some of the potential participants with symptoms of GAD were excluded as they had a primary panic disorder or severe major depressive disorder. Included participants had symptoms of comorbid panic disorder (75%) and depression (100%) but GAD was assessed as the primary disorder. The comorbidity between GAD and other anxiety disorders and depression is known [50]. There has been critique towards studies aiming at including participants with “pure” GAD, with the argument that the generalizability of the results of these studies are limited as comorbidity is frequent [51]. In the current study, besides primary panic disorder and severe major depression, comorbid anxiety disorders and depression were not reasons for exclusion.
Evaluation of the inclusion process led to the addition of antipsychotic medication to the exclusion criteria due to potential sedative effects that can prevent the treatment effect of CBT. Tapering benzodiazepines was successful through the established procedures.
As a result of the drop out, inclusion procedures were aimed towards not including participants in testing and/or treatment in the time leading up to holidays or events.
Effects of treatment
Scores on the PSWQ [30] showed a statistically, but not clinically, reliable change, according to the cut-off as determined by the analysis in this study. This implies that the scores have not changed from a clinical to a non-clinical population. Also, diagnostic assessment after treatment showed that none of the participants had GAD.
Johnco, Wuthrich, Brenes, Wetherell and Mohlman [52] discuss whether the PSWQ is a suboptimal measure for evaluating treatment outcome in geriatric GAD, as there does not exist a clear cut-off or benchmark for the PSWQ to determine patients in remission and patients that show response to treatment. The authors found that a score of 51 or below is optimal for defining remission status on the PSWQ, and a 9% reduction or > 4-point reduction is optimal for assessing treatment response on the PSWQ. With these criteria, one of the participants in the current study would have been characterised as in remission, and two of the participants would be characterised as having a treatment response as they had 20% reduction on the scores on the PSWQ from pre to post treatment.
Participants showed the greatest reduction in scores on anxiety measures, and least reduction in scores of depression and sleep problems. As the CBT protocol is targeted at reducing anxiety, this is not a surprising finding. The change in depression scores can be associated with the rumination component of depression, which resembles worry – the core component of GAD. A treatment that taps into worry might also influence rumination. In addition, PE has been found to have a robust effect on depressive symptoms [53]. As participants in the current study engaged in PE, this may explain the change in depressive symptoms. However, as this study did not include a control group, the change can also be due to non-treatment related factors.
The manipulation checks overall yielded expected results after 15 weeks of PE and indicate that the intensity of the exercise intervention is sufficient to further investigate the effect on treatment outcomes.
Limitations
The procedures for recruitment for the RCT and the CBT + placebo control condition as described in the RCT design [16] were not tested. Furthermore, the small sample limits the generalisability of results of feasibility. In assessing the feasibility of the study design, one limitation is that only four out of 22 assessed subjects were included in the study. Due to our recruitment strategy, the participants that we assessed were mainly in treatment at the local psychiatric facility. As such, they had other treatment options. We have not investigated this further, but we believe these factors to be relevant in understanding the low inclusion percentage in the feasibility study. To preserve the data quality needed to answer research questions in the RCT, we chose to keep the exclusion criteria from the feasibility, although this strategy can be a limitation to the ecological validity of the study.
Clinical implications
-
The current protocol of CBT + PE, as well as test protocols, for older adults with GAD is feasible.
-
The study indicates treatment effect of the combined treatment for older adults with GAD.
Change history
04 August 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13030-023-00284-3
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
National Institute for Health and Clinical Excellence. Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults. Clinical guideline 113. London: National Institute for Health and Clinical Excellence. http://guidance.nice.org.uk/CG113; 2011. Available at www.nice.org.uk.p.
Hall J, Kellett S, Berrios R, Bains MK, Scott S. Efficacy of cognitive behavioral therapy for generalized anxiety disorder in older adults: systematic review, meta analysis, and meta-regression. Am J Geriatric Psychiatry. 2016;24(11):1063–73.
Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. Anxiety disorders in older adults: a comprehensive review. Depress Anxiety. 2010;27(2):190–211.
Kishita N, Laidlaw K. Cognitive behaviour therapy for generalized anxiety disorder: is CBT equally efficacious in adults of working age and older adults? Clin Psychol Rev. 2017;52:124–36.
Mohlman J, Gorman JM. The role of executive functioning in CBT: a pilot study with anxious older adults. Behav Res Ther. 2005;43(4):447–65.
Mohlman J. More power to the executive? A preliminary test of CBT plus executive skills training for treatment of late-life GAD. Cogn Behav Pract. 2008;15(3):306–16.
Johnco C, Wuthrich VM, Rapee RM. The role of cognitive flexibility in cognitive restructuring skill acquisition among older adults. J Anxiety Disord. 2013;27(6):576–84.
Yochim BP, Mueller AE, Segal DL. Late life anxiety is associated with decreased memory and executive functioning in community dwelling older adults. J Anxiety Disord. 2013;27(6):567–75.
Colcombe SJ, Erickson KI, Scalf PE, Kim JS, Prakash R, McAuley E et al. Aerobic Exercise Training increases brain volume in aging humans. The journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2006;61(11):1166–70.
Smith PJ, Blumenthal JA, Hoffman BM, Cooper H, Strauman TA, Welsh-Bohmer K, et al. Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials. Psychosom Med. 2010;72(3):239–52.
Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58–65.
Mata J, Thompson RJ, Gotlib IH. BDNF genotype moderates the relation between physical activity and depressive symptoms. Health Psychol. 2010;29(2):130–3.
Ströhle A, Stoy M, Graetz B, Scheel M, Wittmann A, Gallinat J, et al. Acute exercise ameliorates reduced brain-derived neurotrophic factor in patients with panic disorder. Psychoneuroendocrinology. 2010;35(3):364–8.
Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59(12):1116–27.
Stavestrand SH, Sirevåg K, Nordhus IH, Sjøbø T, Endal TB, Nordahl HM, et al. Physical exercise augmented cognitive behaviour therapy for older adults with generalised anxiety disorder (PEXACOG): study protocol for a randomized controlled trial. Trials. 2019;20(1):174.
Hovland A, Johansen H, Sjobo T, Vollestad J, Nordhus IH, Pallesen S, et al. A feasibility study on combining internet-based cognitive Behaviour Therapy with Physical Exercise as treatment for panic disorder–treatment protocol and preliminary results. Cogn Behav Ther. 2015;44(4):275–87.
Bischoff S, Wieder G, Einsle F, Petzold MB, Janssen C, Mumm JL, et al. Running for extinction? Aerobic exercise as an augmentation of exposure therapy in panic disorder with agoraphobia. J Psychiatr Res. 2018;101:34–41.
Gaudlitz K, Plag J, Dimeo F, Ströhle A. Aerobic exercise training facilitates the effectiveness of cognitive behavioral therapy in panic disorder. Depress Anxiety. 2015;32(3):221–8.
Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders–a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959–68.
Plag J, Schmidt-Hellinger P, Klippstein T, Mumm JL, Wolfarth B, Petzold MB et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020:102311.
Martinsen EW, Hoffart A, Solberg OY. Aerobic and non-aerobic forms of exercise in the treatment of anxiety disorders. Stress Med. 1989;5(2):115–20.
DiNardo PA, Brow TA, Barlow DH, Peter A, DiNardo TA, Brown. David H. Barlow: Graywind; 1994.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33;quiz 4–57.
Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, et al. The Mini International Neuropsychiatric interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur psychiatry. 1997;12(5):224–31.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol. 1993;61(4):611.
Barber JP, Liese BS, Abrams MJ. Development of the cognitive therapy adherence and competence scale. Psychother Res. 2003;13(2):205–21.
Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the penn state worry questionnaire. Behav Res Ther. 1990;28(6):487–95.
Beck AT, Steer RA. Beck anxiety inventory manual. San Antonio, TX: The Psychological Corporation; 1993.
Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II manual. San Antonio, TX: The Psychological Corporation; 1996. pp. 1–82.
Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and validation of the geriatric anxiety inventory. Int Psychogeriatr. 2007;19(1):103–14.
Pallesen S, Bjorvatn B, Nordhus IH, Sivertsen B, Hjørnevik M, Morin CM. A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills. 2008;107(3):691–706.
Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86.
Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(06):755–62.
Craig C, Marshall A, Sjostrom M, Bauman A, Lee P, Macfarlane D et al. International Physical Activity Questionnaire-Short Form. 2017.
Ekblom-Bak E, Björkman F, Hellenius ML, Ekblom B. A new submaximal cycle ergometer test for prediction of VO2max. Scandinavian journal of medicine & science in sports; 2012.
Andersson EA, Lundahl G, Wecke L, Lindblom I, Nilsson J. Maximal aerobic power versus performance in two aerobic endurance tests among young and old adults. Gerontology. 2011;57(6):502–12.
Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9(2):106–19.
Corp I. IBM SPSS Statistics for Windows, Version 24.0. In: Armonk NIC, editor 24 ed. NY: Armonk; Released 2016.
Evans C, Margison F, Barkham M. The contribution of reliable and clinically significant change methods to evidence-based mental health. Evid Based Ment Health. 1998;1(3):70–2.
Zahra D, Hedge C. The reliable change index: why isn’t it more popular in academic psychology. Psychol Postgrad Affairs Group Q. 2010;76:14–9.
Beck JG, Stanley MA, Zebb BJ. Psychometric properties of the Penn state worry questionnaire in older adults. J Clin Geropsychology. 1995;1(1):33–42.
Morin CM, Landreville P, Colecchi C, McDonald K, Stone J, Ling W. The Beck anxiety inventory: psychometric properties with older adults. J Clin Geropsychology. 1999;5:19–29.
Segal DL, Coolidge FL, Cahill BS, O’Riley AA. Psychometric properties of the Beck Depression Inventory—II (BDI-II) among community-dwelling older adults. Behav Modif. 2008;32(1):3–20.
Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. J Clin Psychol. 1999;55(1):117–28.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Pallesen S, Bjorvatn B, Nordhus I, Sivertsen B, Hjørnevik M, Morin C. A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills. 2008;107(3):691–706.
Wittchen H-U, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(5):355–64.
Bruce SE, Machan JT, Dyck I, Keller MB. Infrequency of “pure” GAD: impact of psychiatric comorbidity on clinical course. Depress Anxiety. 2001;14(4):219–25.
Johnco C, Wuthrich VM, Brenes GA, Wetherell JL, Mohlman J. Evidence-based assessment of treatment outcomes for late-life generalized anxiety disorder using the Penn state worry questionnaire (PSWQ) and Penn State worry questionnaire–abbreviated (PSWQ-A). Int Psychogeriatr. 2021:1–13.
Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:67–86.
Acknowledgements
We want to acknowledge all involved personnel at Solli District Psychiatric Centre for their valuable contribution to the study. Furthermore, radiographs at Haukeland University Hospital, test technicians at Neuropsychological Polyclinic at University of Bergen, and lab personnel at the Department of Biological and Medical Psychology, University of Bergen have been and will be crucial in the data collection. We also want to acknowledge former head of Solli DPS, Inger Johanne Haukedal for the willingness to accommodate the implementation of the feasibility study at Solli DPS.
Author information
Authors and Affiliations
Contributions
KSi and SHS are PhD-students and project coordinators in the PEXACOG study. KSi was involved in planning and implementation of the feasibility study and has written the main drafts for this article. SHS was involved in planning of the feasibility study and adaptation of the CBT manual, and has contributed throughout the work with the manuscript. TS was involved in the planning in implementing of the feasibility study and contributed to the adaptation of the CBT manual. TE was involved in the planning and implementation of the feasibility study and designed the physical exercise intervention. HMN has provided the CBT treatment manual and has been crucial in the adaptation of the manual. He has also contributed to the design of the study, and acts as clinical supervisor for the CBT therapists connected to the study. EA has broad experience with physical testing and has contributed to the selection and implementation of the physical tests in the study. IHN is co-supervisor of KSi and SHS. She has contributed to the design of the study and has provided feedback on this manuscript. ÅR is psychiatrist and medical advisor at Solli DPS and has been involved in the adaptation of the CBT treatment manual, and in development of exclusion criteria related to medication. KSp has been crucial in in the planning and design of the fMRI protocol in the study. ÅH has been crucial in the planning and design of the neuropsychological testing in the study and will contribute to analyses and interpretation of these. AHa is a psychiatrist and head of the biobank in the project. JM is an expert on generalised anxiety disorder in older adults and fMRI and has contributed to the development of the rationale and hypotheses in the study. HH has programmed and helped implement the fMRI protocol in the study. JFT is an expert on heart rate variability and has contributed to the development of the rationale and hypotheses in the study. AH is project leader and supervisor for KSi and SHS and has been involved in all parts of the feasibility study. He has given valuable feedback on this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The Regional Committee for Medical and Health Research Ethics, region North in Norway has approved the study, reference number 2015/2189, approved 11. November 2015. All important protocol modifications are reported to the Regional Committee for Medical and Health Research Ethics for approval. Participants were given written and oral information about the study before enrolment. All participants have signed informed consent before enrolment in the study.
Datasets are available from the corresponding author on reasonable request.
Competing interests
The authors report no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The author names has been updated from I. H. K. Nordhus to I. H. Nordhus, Rekdal to Å. Rekdal, and Hammar to Å. Hammar.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sirevåg, K., Stavestrand, S.H., Sjøbø, T. et al. Physical exercise augmented cognitive behaviour therapy for older adults with generalised anxiety disorder (PEXACOG): a feasibility study for a randomized controlled trial. BioPsychoSocial Med 17, 25 (2023). https://doi.org/10.1186/s13030-023-00280-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13030-023-00280-7