Abstract
Background
PIK3CA-related disorders include vascular malformations and overgrowth of various tissues that are caused by postzygotic, somatic variants in the gene encoding phosphatidylinositol-3-kinase (PI3K) catalytic subunit alpha. These mutations result in activation of the PI3K/AKT/mTOR signaling pathway. The goals of this review are to provide education on the underlying mechanism of disease for this group of rare conditions and to summarize recent advancements in the understanding of, as well as current and emerging treatment options for PIK3CA-related disorders.
Main body
PIK3CA-related disorders include PIK3CA-related overgrowth spectrum (PROS), PIK3CA-related vascular malformations, and PIK3CA-related nonvascular lesions. Somatic activating mutations (predominantly in hotspots in the helical and kinase domains of PIK3CA, but also in other domains), lead to hyperactivation of the PI3K signaling pathway, which results in abnormal tissue growth. Diagnosis is complicated by the variability and overlap in phenotypes associated with PIK3CA-related disorders and should be performed by clinicians with the required expertise along with coordinated care from a multidisciplinary team. Although tissue mosaicism presents challenges for confirmation of PIK3CA mutations, next-generation sequencing and tissue selection have improved detection. Clinical improvement, radiological response, and patient-reported outcomes are typically used to assess treatment response in clinical studies of patients with PIK3CA-related disorders, but objective assessment of treatment response is difficult using imaging (due to the heterogeneous nature of these disorders, superimposed upon patient growth and development). Despite their limitations, patient-reported outcome tools may be best suited to gauge patient improvement. New therapeutic options are needed to provide an alternative or supplement to standard approaches such as surgery and sclerotherapy. Currently, there are no systemic agents that have regulatory approval for these disorders, but the mTOR inhibitor sirolimus has been used for several years in clinical trials and off label to address symptoms. There are also other agents under investigation for PIK3CA-related disorders that act as inhibitors to target different components of the PI3K signaling pathway including AKT (miransertib) and PI3K alpha (alpelisib).
Conclusion
Management of patients with PIK3CA-related disorders requires a multidisciplinary approach. Further results from ongoing clinical studies of agents targeting the PI3K pathway are highly anticipated.
Similar content being viewed by others
Introduction
PIK3CA-related disorders (including PIK3CA-related overgrowth spectrum, or PROS) are caused by postzygotic, somatic variants in the gene that encodes phosphatidylinositol-3-kinase (PI3K) catalytic subunit alpha (p110α) [1]. These variants are associated with hyperactivation of the PI3K signaling pathway, which includes multiple downstream effectors such as AKT and mTOR, resulting in vascular malformations and abnormal growth of various tissues [1, 2].
PIK3CA-related disorders that fall under the PROS umbrella term are characterized by clinical diagnostic criteria (initially defined by an NIH workshop that convened in 2013): Presence of a somatic PIK3CA pathogenic variant (however, tissue mosaicism can be a barrier to mutation confirmation), congenital or early childhood onset, sporadic occurrence, and a spectrum of two or more clinical features [3]. While each PROS disorder is distinct, they often share overlapping clinical features [3]. However, many patients with PIK3CA-related vascular malformations or other PIK3CA-related lesions do not present with tissue overgrowth [4]. Due to the limitations of the term “PROS,” we propose “PIK3CA-related disorders” as more appropriate to describe non-cancerous clinical characteristics/phenotypes and disorders that result from postzygotic, somatic mutations in PIK3CA. In addition, this label agrees with recent guidelines for naming genetic disorders [5]. PROS would then be considered a subcategory of PIK3CA-related disorders along with PIK3CA-related vascular malformations and PIK3CA-related nonvascular lesions.
The goals of this review are to provide education on the underlying mechanism of disease for this group of rare disorders, to summarize recent advancements in the understanding of PIK3CA-related disorders, and to discuss current and emerging treatment options. A patient-focused, plain language summary of this review can be found in the supplementary information (Additional file 1).
Methods
In December 2020 and January 2021, literature searches were conducted using PubMed and Google Scholar with search terms including “PIK3CA-related overgrowth spectrum,” “PROS,” “PIK3CA somatic mutations,” “PIK3CA signaling,” “alpelisib,” “miransertib,” and “sirolimus.” ClinicalTrials.gov was searched for relevant trials of alpelisib, miransertib, and sirolimus. Additional references and clinical trials were identified through review of retrieved articles and author knowledge and expertise. This review represents the authors’ perspective based on selected literature. This approach had certain limitations, including a lack of comprehensive, prospectively defined criteria to identify, select, and evaluate references. Hence, the search results used as the basis for the review may not be a complete, objective representation of all the published literature related to the topic.
Etiology/mechanism of disease for PIK3CA-related disorders
The PI3K signaling pathway plays a role in many cellular processes, including proliferation, angiogenesis, survival, and metabolism (Fig. 1 [6,7,8]) [9, 10]. In human cells, three main classes of PI3K are categorized based on their structure and substrate preference [11,12,13]. Class II PI3Ks and class III PI3Ks contain 3 enzymes (PI3K-C2α, β, γ) and one enzyme (hVPS34), respectively [11]. In addition, a group of serine/threonine kinases including mTOR is sometimes referred to as class IV PI3Ks [13]. Class I PI3Ks are activated downstream of growth factor receptors such as PDGF receptor (PDGFR), epidermal growth factor receptor (EGFR), insulin-like growth factor receptor (IGFR), and insulin receptor (INSR) [11]. The TIE2 tyrosine kinase receptor, which is specific to endothelial cells, also activates PI3K upon angiopoietin-1 binding [4, 14, 15]. Somatic mutations in TIE2/TEK have been implicated in vascular malformations [16, 17].
The PI3K signaling pathway and inhibitors under investigation. Because PIK3CA mutations underlie the pathogenesis of PIK3CA-related disorders, there are multiple strategies for targeting the PI3K pathway under investigation [6, 8]. AKT: protein kinase B; AMP: adenosine monophosphate; AMPK: AMP-activated protein kinase; ATP: adenosine triphosphate; BAD: Bcl-2-associated death promoter; CDC42: Cell division control protein 42 homolog; ERK: extracellular signal regulated kinase; FKHR: forkhead; GDP: guanosine diphosphate; GPCR, G protein-coupled receptor; Grb2: growth factor receptor-bound protein 2; GSK3: glycogen synthase kinase 3; GTP: guanosine-5'-triphosphate; IRS: insulin receptor substrate; LKB1: liver kinase B1; MAPK: mitogen-activated protein kinase; MDM2: mouse double minute 2; mTOR: mammalian target of rapamycin; NF-κB: nuclear factor kappa B; P: phosphate; PI3K: phosphatidylinositol-3-kinase; PIK3CA: phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha; PIP2: phosphatidylinositol-4,5-bisphosphate; PIP3: phosphatidylinositol-3,4,5-triphosphate; PKA: protein kinases A; PKC: protein kinase C; PROS: PIK3CA-related overgrowth spectrum; PTEN: phosphatase and tensin homolog; RAC1: Ras-related C3 botulinum toxin substrate 1; Ras: rat sarcoma; RTK, receptor tyrosine kinase; SGK: serum- and glucocorticoid-inducible kinase; Src: rous sarcoma; TIE2, angiopoietin-1 receptor. Adapted with permission from Hennessy 2005 [7]
Class I PI3Ks are composed of a catalytic subunit (p110) and a regulatory subunit [11]. The class I p110α isoform, which is encoded by PIK3CA, is one of the four isoforms of the p110 catalytic subunit found in mammals (p110α, β, γ, and δ) and is the focus of this review [9, 11]. Class I PI3Ks catalyze the phosphorylation of phosphatidylinositol-4,5-bisphosphate (PIP2) to produce phosphatidylinositol-3,4,5-trisphosphate (PIP3), which recruits effector proteins such as the AKT subfamily of AGC serine/threonine kinases [9, 11]. Notably, TIE2 mutations have also been shown to activate AKT [4, 14, 15]. AKT indirectly activates the mTOR serine/threonine kinase, which is found in the cellular complexes mTORC1 and mTORC2 [9]. The tumor suppressor protein phosphatase and tensin homolog (PTEN) suppresses PI3K signaling by dephosphorylating PIP3 [9]. Components of the PI3K/AKT/mTOR pathway interact with other signaling pathways, including RAS/RAF/MEK/MAPK [9].
The PIK3CA gene encodes the α isoform of the p110 catalytic subunit of PI3K (PI3Kα) and is ubiquitously expressed [9]. The somatic activating mutations in PIK3CA-related disorders are also frequently observed in numerous cancers including hotspot mutations in the helical and kinase domains (E542K and E545K in the helical domain; H1047L and H1047R in the kinase domain) [3, 18]. These mutations result in hyperactivation of the PI3K signaling pathway, which leads to abnormal growth of tissues, including epithelial and mesenchymal cells [9, 19]. Preclinical studies have shown that these mutations result in AKT activation, changes in cell morphology, and downregulation of angiogenic factors [4, 20]. The resulting overgrowth syndromes often include slow-flow vascular malformations such as lymphatic and venous malformations [19,20,21]. Studies of venous malformations (VM) show that activation of the TIE2/PI3K pathway promotes growth of human umbilical vein endothelial cells in xenograft models, aberrant expression of genes that regulate vascular development (including platelet-derived growth factor, β polypeptide), and disruption of the endothelial cell monolayer [14, 15, 19, 22]. Relative to other PIK3CA-related disorders, the variants observed in patients with megalencephaly-capillary malformation (MCAP/M-CM) are often seen in non-hotspot loci on the PIK3CA gene and are associated with less-activating mutations [23, 24].
The postzygotic, sporadic mutations that occur in PIK3CA-related disorders produce genetically distinct cell lineages found in a mosaic pattern based on the developmental stage in which they occur [9, 12, 24,25,26]. Overall, the variant, timing, and location of these mutations likely contribute to the basis for the wide-ranging manifestations observed in PIK3CA-related disorders [20]. Due to the heterogeneity of these disorders and the wide variety of affected tissues, patients may have different responses to therapeutic intervention; however, prospective, controlled studies are needed.
Classification of PIK3CA-related disorders and relationship to vascular anomaly classifications
Currently identified PIK3CA-related disorders are presented in Fig. 2 [2, 3, 27,28,29,30,31,32,33]. According to the classification from the International Society for the Study of Vascular Anomalies (ISSVA), PROS disorders include the following: Congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal (CLOVES) syndrome; dysplastic megalencephaly (DMEG); fibroadipose hyperplasia or overgrowth (FAO); fibroadipose infiltrating lipomatosis/facial infiltrative lipomatosis (FIL); hemihyperplasia multiple lipomatosis (HHML); Klippel-Trenaunay syndrome (KTS); macrodactyly and MCAP/M-CM [2]. The ISSVA classification also lists other vascular anomalies associated with PIK3CA variants: CLAPO syndrome (lower lip capillary malformation + face and neck lymphatic malformation + asymmetry and partial/generalized overgrowth); common (cystic) lymphatic malformation (LM); common VM; and fibroadipose vascular anomaly (FAVA) [2]. Emerging evidence suggests that PIK3CA mutations can be found in combined lymphatic-venous malformations (LVM) and combined capillary-lymphatic-venous malformations (CLVM) – malformations that are also found in patients with KTS [24, 27, 33]. In addition, the following syndromes and/or isolated phenotypes are classified as PIK3CA-related according to the 2013 NIH workshop: hemimegalencephaly (HMEG), muscular hemihyperplasia (HH), seborrheic keratoses (SK), epidermal nevi (EN), and benign lichenoid keratoses (BLK). Since the latter three phenotypes can occur as isolated features we have categorized these as PIK3CA-related nonvascular lesions [3]. PIK3CA mutations have also been implicated in some cases of diffuse capillary malformation with overgrowth (DCMO), lipomatosis of nerve (LON), and some complicated lymphatic anomalies (CLAs) including generalized lymphatic anomaly (GLA) [28,29,30, 32].
PIK3CA-related disorders. The category of PIK3CA-related disorders can be divided into 3 subcategories: PROS, PIK3CA-related vascular malformations, and PIK3CA-related nonvascular lesions. CLAPO: capillary malformation of the lower lip, lymphatic malformation of the face and neck, asymmetry and partial/generalized overgrowth; CLOVES: congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal; CLVM: combined capillary-lymphatic-venous malformation; DCMO: diffuse capillary malformation with overgrowth; DMEG: dysplastic megalencephaly; FAO/HHML: fibroadipose hyperplasia or overgrowth/hemihyperplasia-multiple lipomatosis; FAVA: fibroadipose vascular anomaly; FIL: fibroadipose or facial infiltrating lipomatosis; GLA, generalized lymphatic anomaly; HH: hemihyperplasia; HMEG: hemimegalencephaly; LM, lymphatic malformation; LON: lipomatosis of nerve; LVM: combined lymphatic-venous malformation; MCAP: megalencephaly-capillary malformation; PIK3CA: phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha; VM, venous malformation. *Malformations that are composed of only one type of vessel are classified as “simple” (with the exception of arteriovenous malformation). If a lesion contains ≥ 2 types of vascular malformations, it is classified as “combined.” Vascular malformations are also classified according to major named vessels or by association with other anomalies (e.g., PROS) Wassef 2015 [33]. †Some common (cystic) LM are classified as PROS when they are associated with overgrowth ISSVA 2018 [2]. ‡Can occur as isolated lesions or with other clinical features. Supporting Sources: PIK3CA-related overgrowth spectrum: Keppler-Noreuil 2015 [3]; ISSVA 2018 [2]; Goss 2020 [28]; Hughes 2020 [29]; Mahan 2014 [30]; Rios 2013 [31]; Rodriguez-Laguna 2019 [32]; PIK3CA-related vascular malformations: ISSVA 2018 [2]; Rodriguez-Laguna 2019 [32]; PIK3CA-related nonvascular lesions: Keppler-Noreuil 2015 [3]; Combined vascular malformations: Wassef 2015 [33]; Brandigi 2018 [27]
Diagnosis and complications associated with PIK3CA-related disorders
Clinical diagnosis is complicated by the variability and overlapping phenotypes of PIK3CA-related disorders [3, 34,35,36]. Diagnosis should be performed by clinicians with expertise followed by coordinated care from a multidisciplinary team, which includes surgeons, radiologists, geneticists, dermatologists, pathologists, and hematologists/oncologists, the latter of whom are critical for the emerging medical management and coordination of the associated long-term follow-up [6, 35,36,37].
Key criteria for diagnosis of PROS disorders have been outlined by Keppler-Noreuil et al. [3]. Simple vascular malformations, including common (cystic) LMs and common VMs, are composed of only one type of vessel, whereas combined vascular malformations, including CLVMs and LVMs, are composed of combinations of vessels. Both may be characterized by clinical and radiological features outlined by ISSVA [33]. A distinct, multidisciplinary set of guidelines for evaluation of CLAs was recently published [38]. The main imaging modalities used to diagnose subcutaneous vascular malformations are Doppler ultrasound and magnetic resonance imaging [39]. For PIK3CA-related nonvascular lesions, specialists should be consulted depending on location of the lesion.
Clinicians should take a careful patient history, including a family history to distinguish between sporadically occurring and inherited disorders [25, 36, 37]. Confirmation of PIK3CA mutation is highly recommended for diagnosis of PIK3CA-related disorders; however, a negative test result does not preclude diagnosis [3]. Due to the mosaic nature of PIK3CA-related disorders and challenges with tissue biopsy collection, it may not always be possible to confirm the presence of the PIK3CA mutation [3]. Given the low level of mosaicism in some patients, next-generation sequencing or specific droplet digital PCR (ddPCR) for hot spot mutations may be the optimal techniques for identifying mutations [4, 24, 34, 40,41,42].
It is important to note that the majority of patients with PIK3CA-related disorders experience a progressive disease course, with clinical manifestations typically observed within the patient’s first year of life, with additional manifestations becoming apparent later [3, 9]. This could pose a challenge to diagnosis and ongoing care of patients with an early diagnosis of vascular malformation, who go on to experience overgrowth or other manifestations in different tissues. When considering the nomenclature for these disorders, care should be taken to consider this possibility.
In the differential diagnosis of PIK3CA-related disorders, it is important to consider other syndromes with overlapping characteristics but different genetic causes, such as Proteus syndrome and PTEN Hamartoma Tumor Syndrome [3]. Proteus syndrome is associated with a somatic activating AKT1 mutation and has distinct clinical findings [43]. PTEN Hamartoma Tumor Syndrome is associated with vascular anomalies in more than 50% of patients as well as fat overgrowth, which can result in misdiagnosis as PROS disorders, such as CLOVES or FAVA [44]. In addition, there are overlapping clinical phenotypes caused by somatic mutations in other related gene pathways, such as in the mosaic RASopathies [45,46,47,48,49].
Complications that are commonly associated with PIK3CA-related disorders, which may or may not be related to vascular malformations, are detailed in Table 1 [1, 3, 9, 42, 50]. Based on the patient’s presentation, clinical imaging evaluations should be performed as needed [3, 51].
Challenges of assessing treatment response
Clinical improvement, radiological response, and patient-reported outcomes are typically used to assess treatment response in clinical studies of patients with PIK3CA-related disorders [22, 36, 53,54,55,56,57]. However assessment of individual patients over time is complicated by the variable natural histories of these disorders and incomplete resolution of symptoms [53]. Accurate and thorough assessment of patient history is also critical to rule out vascular malformations caused by inherited mutations (e.g., hereditary hemorrhagic telangiectasia, glomuvenous malformation, and CM-AVM) or other congenital conditions with similar clinical features or symptoms [36, 57]. Even when properly characterized, these conditions are both rare and highly heterogeneous, which poses challenges to recruitment and completion of clinical studies [53].
Clinical diagnosis of venous malformations can be a significant challenge. D-dimer is frequently elevated in patients with venous malformations and has emerged as a biomarker to aid differential diagnosis [51, 58]. Elevated D-dimer can differentiate KTS from Parkes Weber syndrome as well as multifocal venous lesions versus glomuvenous malformations [58]. Patients with venous malformations are at risk for coagulopathy, and those with elevated levels of D-dimer and low levels of fibrinogen are at particular risk for hemorrhage [52]. Levels of both D-dimer and fibrinogen have been shown to improve in patients with TIE2–mutated and PIK3CA-mutated venous malformations treated with sirolimus [22, 54], suggesting that these markers could be used to monitor response to treatment.
When assessing response with imaging techniques, growth over time and interpatient provides challenges to objective assessments [1, 54]. Notably, even when clinical improvement and successful treatment of symptoms is observed, assessments may continue to appear abnormal [54, 59]. As a result, patient-reported outcome assessments such as quality-of-life questionnaires and pain assessment by visual analog scale may be the best tools to measure efficacy, but these may be confounded effects due to many patients experiencing symptoms since birth [54]. There is an unmet need for validated patient-reported outcome tools that are specifically designed to assess quality of life in these populations; quality of life has been identified as a core outcome domain by the ongoing Outcome Measures for VAscular MAlformations (OVAMA) project [60,61,62,63,64].
Current and emerging treatment options
Current treatment options include debulking surgery, sclerotherapy, and laser therapy [6, 35, 39, 65, 66]. However, recurrence after surgery is common, necessitating repeated surgical procedures [1, 35, 66], which may result in functional complications [66, 67]. Moreover, these modalities and medical interventions such as prophylactic use of antibiotics, anticoagulants, and pain management treat patients’ symptoms rather than the underlying molecular etiology of PI3K pathway hyperactivation.
Current and emerging targeted agents
Systemic agents under investigation for PIK3CA-related disorders target different components of the PI3K signaling pathway (Fig. 1).
Sirolimus
Sirolimus inhibits mTOR, which is a node in the PI3K signaling pathway, and has been investigated in several clinical trials in patients with vascular malformations and overgrowth disorders [1, 6, 21, 53, 54]. Sirolimus is currently used in an off-label capacity to treat these disorders [36, 57].
Sirolimus has shown efficacy in multiple phase 2 studies in this setting. In a study of patients with complicated vascular anomalies, including tumors and malformations (N = 61), 85% of patients who completed 12 courses of treatment (n = 53) had a partial response [53]. In a subgroup of patients with complex lymphatic anomalies (N = 18), 83% of patients showed improvement after sirolimus treatment [59]. Sirolimus has also demonstrated efficacy in patients with complex slow-flow malformations (N = 19) [54]. In the multi-institutional phase 2 PROMISE study of 39 patients with a confirmed PIK3CA variant and progressive overgrowth (a different population from that of the study of complicated vascular anomalies), sirolimus showed modest efficacy at lower doses but only limited reduction in adverse events compared with higher doses [1, 68]. Results are awaited from the completed phase 2 PERFORMUS trial of sirolimus in pediatric patients with complicated superficial slow-flow vascular malformations [69, 70], and from the ongoing phase 3 VASE trial (EudraCT:2015-001703-32) [37, 71].
The safety profile of sirolimus in clinical trials has been encouraging; common grade 1–2 adverse events include headache, fatigue, cutaneous rash, mucositis, gastrointestinal troubles, and flu-like syndrome [21, 57]. A common grade 3 adverse event is mucositis [57]. Although severe opportunistic infections (e.g., Pneumocystis) have not been observed to date in the VASE study, patients at particular risk of these infections (i.e., very young children, those with dose-dependent lymphopenia or neutropenia, or other comorbidities) should be strongly considered for dose reduction and/or Pneumocystis prophylaxis [21]. A retrospective multicenter chart review of off-label use of sirolimus in patients with vascular anomalies (N = 113) identified 17 severe adverse events in 14 patients, most frequently viral pneumonia, highlighting the risk of severe and potentially fatal adverse events in these patients [72].
Several case reports/case series with sirolimus have also reported outcomes in this population [22, 68, 70, 73, 74]. Ongoing studies with sirolimus in PIK3CA-related disorders are described in Table 2. Primary endpoints in the ongoing studies include volumetric changes assessed by MRI or ultrasound, improvement in clinical lab indexes, adverse events, and patient-reported outcomes (NCT04598204, NCT02638389, NCT03767660).
Miransertib
Miransertib, an oral, allosteric inhibitor of AKT, demonstrated antiproliferative activity in primary fibroblasts derived from patients (N = 6) with PIK3CA-related disorders in the presence or absence of growth factors [75]. In preliminary results of an open-label, phase 1/2 study of miransertib in patients (N = 15) with PIK3CA-related Overgrowth Spectrum and Proteus Syndrome (MOSAIC), there was radiologically-confirmed lesion stability, and most patients experienced improvement in Karnofsky/Lansky performance scale, movement fluidity, fatigability, and pain relief (Table 2) [33, 56]. A case series with miransertib in two children with severe PROS reported an objective clinical response in a patient with CLOVES and reduced seizure frequency and improved quality of life in a patient with FIL and HMEG; no significant adverse events were reported [76].
Alpelisib
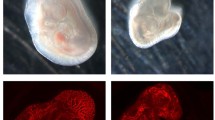
Alpelisib selectively inhibits PI3Kα and therefore directly targets the effects of PIK3CA activating mutations [55, 77]. In a study in human umbilical vein endothelial cells with PIK3CA or TEK mutations, alpelisib reversed abnormal AKT phosphorylation, cell morphology, and extracellular fibronectin levels—further highlighting the connection between TIE2 and PI3Kα in the etiology of common venous malformations. Notably, sirolimus did not restore extracellular fibronectin to wild-type levels in these cells, which suggests that PI3K activity functions upstream or parallel to the AKT/mTOR axis may also contribute to disease pathology [4].
Alpelisib also demonstrated efficacy in a mouse model of PROS/CLOVES, and a study of 19 patients with various PROS disorders revealed treatment with alpelisib led to substantial clinical improvement and a radiological response in all patients [55]. Alpelisib also achieved notable improvements in severe symptoms for individual patients that include opioid dependency and mobility (n = 2), chronic gastrointestinal bleeding (n = 3), and cognitive function (two patients with MCAP/M-CM) [55]. Case reports have described the successful use of alpelisib in patients with CLOVES and PROS [78, 79]. Ongoing alpelisib studies are described in Table 2. Primary endpoints in the ongoing studies include response as indicated by reduction in lesion volume assessed by imaging (NCT04285723, NCT04589650).
Conclusion
There are critical unmet needs for clinicians who treat PIK3CA-related disorders as well as for patients and caregivers. Management of patients with PIK3CA-related disorders requires a multidisciplinary approach to address the spectrum of potential comorbidities [6, 29, 36, 80, 81]. Patients face challenges with continued care as they age into adulthood and have limited access to specialists with adequate expertise with these disorders and emerging systemic treatments [21, 37, 57].
Given the rarity of these disorders and the amount of expertise required, a limited number of centers can offer optimal care. In the US, comprehensive centers for vascular anomalies are often affiliated with children’s hospitals in major cities. The Consortium of iNvestigators of Vascular AnomalieS (CaNVAS; https://www.chop.edu/centers-programs/consortium-investigators-vascular-anomalies-canvas) is composed of 16 US institutions and was founded by pediatric hematologist/oncologists and patient advocacy groups. In the EU, multidisciplinary centers for overgrowth as well as vascular anomalies offer comprehensive care—some of these centers are members of the European Reference Network on Rare Multisystemic Vascular Diseases (VASCERN: https://vascern.eu/). VASCERN’s ongoing establishment of national networks enables follow-up closer to home and advances in virtual care options, such as the Clinical Patient Management System wherein physicians may ask for diagnostic and management assistance for any VASCERN working group disease. However, many patients with PIK3CA-related disorders and their families continue to rely on local physicians who lack experience treating these rare disorders.
New therapies are needed to provide an alternative or supplement to existing therapies that treat symptoms without targeting the underlying cause of these disorders. Inhibitors of the PI3K pathway are currently under clinical investigation and have shown promising results. However, efficacy and safety data from off-label use of these agents in the real-world setting are limited, and patients frequently have underlying comorbid conditions. Because these agents will likely be used in the pediatric setting, data from prospective clinical trials on their long-term safety and pharmacokinetic profiles in young patients are critical. Clinicians will also need to determine how to optimally integrate these emerging targeted therapies into current treatment strategies, and projects are ongoing to develop guidance for local use, which could reduce the frequency of adverse events.
Availability of data and materials
Not applicable.
Abbreviations
- CLOVES:
-
Congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal
- CLVM:
-
Capillary lymphatic venous malformation
- DCMO:
-
Diffuse capillary malformation with overgrowth
- DMEG:
-
Dysplastic megalencephaly
- FAO:
-
Fibroadipose hyperplasia
- FAVA:
-
Fibroadipose vascular anomaly
- FIL:
-
Fibroadipose or facial infiltrating lipomatosis
- GLA:
-
Generalized lymphatic anomaly
- HH:
-
Hemihyperplasia
- HHML:
-
Hemihyperplasia-multiple lipomatosis
- HMEG:
-
Hemimegalencephaly
- LON:
-
Lipomatosis of nerve
- LVM:
-
Lymphatic venous malformation
- MCAP:
-
Megalencephaly-capillary malformation
- PI3K:
-
Phosphatidylinositol-3-kinase
- PIK3CA :
-
Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha
- PIP3 :
-
Phosphatidylinositol-3,4,5-trisphosphate
- PROS:
-
PIK3CA-related overgrowth spectrum
- PS:
-
Proteus syndrome
- VM:
-
Venous malformation
- VMCM:
-
Venous malformation cutaneo-mucosal
References
Parker VER, Keppler-Noreuil KM, Faivre L, Luu M, Oden NL, De Silva L, et al. Safety and efficacy of low-dose sirolimus in the PIK3CA-related overgrowth spectrum. Genet Med. 2019;21(5):1189–98.
International Society for the Study of Vascular Anomalies. ISSVA classification for vascular anomalies. Revised 2018. https://www.issva.org/UserFiles/file/ISSVA-Classification-2018.pdf.
Keppler-Noreuil KM, Rios JJ, Parker VE, Semple RK, Lindhurst MJ, Sapp JC, et al. PIK3CA-related overgrowth spectrum (PROS): diagnostic and testing eligibility criteria, differential diagnosis, and evaluation. Am J Med Genet A. 2015;167A(2):287–95.
Limaye N, Kangas J, Mendola A, Godfraind C, Schlogel MJ, Helaers R, et al. Somatic activating PIK3CA mutations cause venous malformation. Am J Hum Genet. 2015;97(6):914–21.
Biesecker LG, Adam MP, Alkuraya FS, Amemiya AR, Bamshad MJ, Beck AE, et al. A dyadic approach to the delineation of diagnostic entities in clinical genomics. Am J Hum Genet. 2021;108(1):8–15.
Adams DM, Ricci KW. Vascular anomalies: diagnosis of complicated anomalies and new medical treatment options. Hematol Oncol Clin North Am. 2019;33(3):455–70.
Hennessy BT, Smith DL, Ram PT, Lu Y, Mills GB. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov. 2005;4(12):988–1004.
Hillmann P, Fabbro D. PI3K/mTOR pathway inhibition: opportunities in oncology and rare genetic diseases. Int J Mol Sci. 2019;20(22):5792.
Keppler-Noreuil KM, Parker VE, Darling TN, Martinez-Agosto JA. Somatic overgrowth disorders of the PI3K/AKT/mTOR pathway & therapeutic strategies. Am J Med Genet C Semin Med Genet. 2016;172(4):402–21.
Nguyen HL, Boon LM, Vikkula M. Vascular anomalies caused by abnormal signaling within endothelial cells: targets for novel therapies. Semin Intervent Radiol. 2017;34(3):233–8.
Fruman DA, Chiu H, Hopkins BD, Bagrodia S, Cantley LC, Abraham RT. The PI3K pathway in human disease. Cell. 2017;170(4):605–35.
Goncalves MD, Hopkins BD, Cantley LC. Phosphatidylinositol 3-kinase, growth disorders, and cancer. N Engl J Med. 2018;379(21):2052–62.
Liu P, Cheng H, Roberts TM, Zhao JJ. Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov. 2009;8(8):627–44.
Natynki M, Kangas J, Miinalainen I, Sormunen R, Pietila R, Soblet J, et al. Common and specific effects of TIE2 mutations causing venous malformations. Hum Mol Genet. 2015;24(22):6374–89.
Uebelhoer M, Natynki M, Kangas J, Mendola A, Nguyen HL, Soblet J, et al. Venous malformation-causative TIE2 mutations mediate an AKT-dependent decrease in PDGFB. Hum Mol Genet. 2013;22(17):3438–48.
Limaye N, Wouters V, Uebelhoer M, Tuominen M, Wirkkala R, Mulliken JB, et al. Somatic mutations in angiopoietin receptor gene TEK cause solitary and multiple sporadic venous malformations. Nat Genet. 2009;41(1):118–24.
Soblet J, Kangas J, Natynki M, Mendola A, Helaers R, Uebelhoer M, et al. Blue Rubber Bleb Nevus (BRBN) syndrome is caused by somatic TEK (TIE2) mutations. J Invest Dermatol. 2017;137(1):207–16.
Gymnopoulos M, Elsliger MA, Vogt PK. Rare cancer-specific mutations in PIK3CA show gain of function. Proc Natl Acad Sci USA. 2007;104(13):5569–74.
Castel P, Carmona FJ, Grego-Bessa J, Berger MF, Viale A, Anderson KV, et al. Somatic PIK3CA mutations as a driver of sporadic venous malformations. Sci Transl Med. 2016;8(332):332ra42.
Martinez-Corral I, Zhang Y, Petkova M, Ortsater H, Sjoberg S, Castillo SD, et al. Blockade of VEGF-C signaling inhibits lymphatic malformations driven by oncogenic PIK3CA mutation. Nat Commun. 2020;11(1):2869.
Van Damme A, Seront E, Dekeuleneer V, Boon LM, Vikkula M. New and emerging targeted therapies for vascular malformations. Am J Clin Dermatol. 2020;21(5):657–68.
Boscolo E, Limaye N, Huang L, Kang KT, Soblet J, Uebelhoer M, et al. Rapamycin improves TIE2-mutated venous malformation in murine model and human subjects. J Clin Invest. 2015;125(9):3491–504.
Mirzaa G, Timms AE, Conti V, Boyle EA, Girisha KM, Martin B, et al. PIK3CA-associated developmental disorders exhibit distinct classes of mutations with variable expression and tissue distribution. JCI Insight. 2016;1(9):e87623.
Brouillard P, Schlögel MJ, Homayun Sepehr N, Helaers R, Queisser A, Fastré E, et al. Non-hotspot PIK3CA mutations are more frequent in CLOVES than in common or combined lymphatic malformations. Orphanet J Rare Dis. 2021;16(1):267.
Limaye N, Boon LM, Vikkula M. From germline towards somatic mutations in the pathophysiology of vascular anomalies. Hum Mol Genet. 2009;18(R1):R65-74.
Nguyen HL, Boon LM, Vikkula M. Genetics of vascular malformations. Semin Pediatr Surg. 2014;23(4):221–6.
Brandigi E, Torino G, Messina M, Molinaro F, Mazzei O, Matucci T, et al. Combined capillary-venous-lymphatic malformations without overgrowth in patients with Klippel–Trenaunay syndrome. J Vasc Surg Venous Lymphat Disord. 2018;6(2):230–6.
Goss JA, Konczyk DJ, Smits P, Sudduth CL, Bischoff J, Liang MG, et al. Diffuse capillary malformation with overgrowth contains somatic PIK3CA variants. Clin Genet. 2020;97(5):736–40.
Hughes M, Hao M, Luu M. PIK3CA vascular overgrowth syndromes: an update. Curr Opin Pediatr. 2020;32(4):539–46.
Mahan MA, Amrami KK, Howe BM, Spinner RJ. Segmental thoracic lipomatosis of nerve with nerve territory overgrowth. J Neurosurg. 2014;120(5):1118–24.
Rios JJ, Paria N, Burns DK, Israel BA, Cornelia R, Wise CA, et al. Somatic gain-of-function mutations in PIK3CA in patients with macrodactyly. Hum Mol Genet. 2013;22(3):444–51.
Rodriguez-Laguna L, Agra N, Ibanez K, Oliva-Molina G, Gordo G, Khurana N, et al. Somatic activating mutations in PIK3CA cause generalized lymphatic anomaly. J Exp Med. 2019;216(2):407–18.
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, et al. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136(1):e203–14.
Nathan N, Keppler-Noreuil KM, Biesecker LG, Moss J, Darling TN. Mosaic disorders of the PI3K/PTEN/AKT/TSC/mTORC1 signaling pathway. Dermatol Clin. 2017;35(1):51–60.
Boon LM, Vikkula M. Vascular malformations. In: Hoeger P, et al., editors. Harper’s Textbook of Pediatric Dermatology. Wiley; 2019. p. 1399–424.
Dekeuleneer V, Seront E, Van Damme A, Boon LM, Vikkula M. Theranostic advances in vascular malformations. J Invest Dermatol. 2020;140(4):756–63.
Adams DM, Vikkula M, Blei F. Vascular anomalies 101: case-based discussion on the diagnosis, treatment and lifelong care of these patients. In: 62nd ASH annual meeting and exposition; December 5–8, 2020.
Iacobas I, Adams DM, Pimpalwar S, Phung T, Blei F, Burrows P, et al. Multidisciplinary guidelines for initial evaluation of complicated lymphatic anomalies-expert opinion consensus. Pediatr Blood Cancer. 2020;67(1):e28036.
Behravesh S, Yakes W, Gupta N, Naidu S, Chong BW, Khademhosseini A, et al. Venous malformations: clinical diagnosis and treatment. Cardiovasc Diagn Ther. 2016;6(6):557–69.
Chang F, Liu L, Fang E, Zhang G, Chen T, Cao K, et al. Molecular diagnosis of mosaic overgrowth syndromes using a custom-designed next-generation sequencing panel. J Mol Diagn. 2017;19(4):613–24.
Kuentz P, St-Onge J, Duffourd Y, Courcet JB, Carmignac V, Jouan T, et al. Molecular diagnosis of PIK3CA-related overgrowth spectrum (PROS) in 162 patients and recommendations for genetic testing. Genet Med. 2017;19(9):989–97.
Piacitelli AM, Jensen DM, Brandling-Bennett H, Gray MM, Batra M, Gust J, et al. Characterization of a severe case of PIK3CA-related overgrowth at autopsy by droplet digital polymerase chain reaction and report of PIK3CA sequencing in 22 patients. Am J Med Genet A. 2018;176(11):2301–8.
Keppler-Noreuil KM, Sapp JC, Lindhurst MJ, Parker VE, Blumhorst C, Darling T, et al. Clinical delineation and natural history of the PIK3CA-related overgrowth spectrum. Am J Med Genet A. 2014;164A(7):1713–33.
Tan WH, Baris HN, Burrows PE, Robson CD, Alomari AI, Mulliken JB, et al. The spectrum of vascular anomalies in patients with PTEN mutations: implications for diagnosis and management. J Med Genet. 2007;44(9):594–602.
Al-Olabi L, Polubothu S, Dowsett K, Andrews KA, Stadnik P, Joseph AP, et al. Mosaic RAS/MAPK variants cause sporadic vascular malformations which respond to targeted therapy. J Clin Invest. 2018;128(11):5185.
Chacon-Camacho OF, Lopez-Moreno D, Morales-Sanchez MA, Hofmann E, Pacheco-Quito M, Wieland I, et al. Expansion of the phenotypic spectrum and description of molecular findings in a cohort of patients with oculocutaneous mosaic RASopathies. Mol Genet Genomic Med. 2019;7(5):e625.
Gordon K, Varney R, Keeley V, Riches K, Jeffery S, Van Zanten M, et al. Update and audit of the St George’s classification algorithm of primary lymphatic anomalies: a clinical and molecular approach to diagnosis. J Med Genet. 2020;57(10):653–9.
Manevitz-Mendelson E, Leichner GS, Barel O, Davidi-Avrahami I, Ziv-Strasser L, Eyal E, et al. Somatic NRAS mutation in patient with generalized lymphatic anomaly. Angiogenesis. 2018;21(2):287–98.
Barclay SF, Inman KW, Luks VL, McIntyre JB, Al-Ibraheemi A, Church AJ, et al. A somatic activating NRAS variant associated with kaposiform lymphangiomatosis. Genet Med. 2019;21(7):1517–24.
Mirzaa GM, Conway RL, Gripp KW, Lerman-Sagie T, Siegel DH, deVries LS, et al. Megalencephaly-capillary malformation (MCAP) and megalencephaly-polydactyly-polymicrogyria-hydrocephalus (MPPH) syndromes: two closely related disorders of brain overgrowth and abnormal brain and body morphogenesis. Am J Med Genet A. 2012;158A(2):269–91.
Dompmartin A, Vikkula M, Boon LM. Venous malformation: update on aetiopathogenesis, diagnosis and management. Phlebology. 2010;25(5):224–35.
Dompmartin A, Acher A, Thibon P, Tourbach S, Hermans C, Deneys V, et al. Association of localized intravascular coagulopathy with venous malformations. Arch Dermatol. 2008;144(7):873–7.
Adams DM, Trenor CC III, Hammill AM, Vinks AA, Patel MN, Chaudry G, et al. Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics. 2016;137(2):e20153257.
Hammer J, Seront E, Duez S, Dupont S, Van Damme A, Schmitz S, et al. Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: a monocentric prospective phase II study. Orphanet J Rare Dis. 2018;13(1):191.
Venot Q, Blanc T, Rabia SH, Berteloot L, Ladraa S, Duong JP, et al. Targeted therapy in patients with PIK3CA-related overgrowth syndrome. Nature. 2018;558(7711):540–6.
Zampino G, Leoni C, Buonuomo PS, Rana I, Onesimo R, Macchiaiolo M, et al. An open-label, phase 1/2 study of miransertib (ARQ 092), an oral pan-AKT inhibitor, in patients (pts) with PIK3CA-related Overgrowth Spectrum (PROS) and Proteus Syndrome (PS): study design and preliminary results (NCT03094832). European Society of Human Genetics Conference; June 15–18, 2019; Gothenburg, Sweden. Abstract C 18.6.
Seront E, Van Damme A, Boon LM, Vikkula M. Rapamycin and treatment of venous malformations. Curr Opin Hematol. 2019;26(3):185–92.
Dompmartin A, Ballieux F, Thibon P, Lequerrec A, Hermans C, Clapuyt P, et al. Elevated D-dimer level in the differential diagnosis of venous malformations. Arch Dermatol. 2009;145(11):1239–44.
Ricci KW, Hammill AM, Mobberley-Schuman P, Nelson SC, Blatt J, Bender JLG, et al. Efficacy of systemic sirolimus in the treatment of generalized lymphatic anomaly and Gorham–Stout disease. Pediatr Blood Cancer. 2019;66(5):e27614.
Horbach SER, Rongen APM, Elbers RG, van der Horst C, Prinsen CAC, Spuls PI, et al. Outcome measurement instruments for peripheral vascular malformations and an assessment of the measurement properties: a systematic review. Qual Life Res. 2020;29(1):1–17.
Horbach SER, van der Horst C, Blei F, van der Vleuten CJM, Frieden IJ, Richter GT, et al. Development of an international core outcome set for peripheral vascular malformations: the OVAMA project. Br J Dermatol. 2018;178(2):473–81.
Lokhorst MM, Horbach SER, van der Horst C, Spuls PI, Group OS. Finalizing the international core domain set for peripheral vascular malformations: the OVAMA project. Br J Dermatol. 2019;181(5):1076–8.
Lokhorst MM, Horbach SER, Waner M, O TM, van der Vleuten CJM, Mokkink LB, et al. Responsiveness of quality-of-life measures in patients with peripheral vascular malformations: the OVAMA project. Br J Dermatol. 2020;182(6):1395–403.
Lokhorst MM, Horbach SER, Waner M, O TM, van der Vleuten CJM, Spuls PI, et al. Responsiveness of quality of life measures in children with peripheral vascular malformations: the OVAMA project. JPRAS Open. 2021;27:70–9.
Vazquez T, Forouzandeh M, Gurnani P, Akhtar S, Nouri K. Cutaneous vascular lesions in the pediatric population: a review of laser surgery applications and lesion-specific device parameters. Lasers Med Sci. 2020;35(8):1681–7.
Mulliken JB, Burrows PE, Fishman SJ. Mulliken and Young’s vascular anomalies: hemangiomas and malformations. Oxford University Press; 2013.
Mirzaa G, Conway R, Graham JM, Jr., Dobyns WB. PIK3CA-related segmental overgrowth. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, et al., editors. GeneReviews((R)). Seattle; 2013.
Erickson J, McAuliffe W, Blennerhassett L, Halbert A. Fibroadipose vascular anomaly treated with sirolimus: successful outcome in two patients. Pediatr Dermatol. 2017;34(6):e317–20.
Maruani A, Boccara O, Bessis D, Guibaud L, Vabres P, Mazereeuw-Hautier J, et al. Treatment of voluminous and complicated superficial slow-flow vascular malformations with sirolimus (PERFORMUS): protocol for a multicenter phase 2 trial with a randomized observational-phase design. Trials. 2018;19(1):340.
Hammill AM, Wentzel M, Gupta A, Nelson S, Lucky A, Elluru R, et al. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer. 2011;57(6):1018–24.
Phase III multicentric study evaluating the efficacy and safety of sirolimus in vascular anomalies that are refractory to standard care. EudraCT number: 2015001703-32. https://www.clinicaltrialsregister.eu/ctr-search/search?query=2015-001703-32.
Rossler J, Baselga E, Davila V, Celis V, Diociaiuti A, El Hachem M, et al. Severe adverse events during sirolimus “off-label” therapy for vascular anomalies. Pediatr Blood Cancer. 2021;68(8):e28936.
Lackner H, Karastaneva A, Schwinger W, Benesch M, Sovinz P, Seidel M, et al. Sirolimus for the treatment of children with various complicated vascular anomalies. Eur J Pediatr. 2015;174(12):1579–84.
Leoni C, Onesimo R, Resta N, Patti ML, De Santis R, Bagnulo R, et al. Old treatments for new genetic conditions: sirolimus therapy in a child affected by mosaic overgrowth with fibroadipose hyperplasia. Clin Genet. 2019;96(1):102–3.
Ranieri C, Di Tommaso S, Loconte DC, Grossi V, Sanese P, Bagnulo R, et al. In vitro efficacy of ARQ 092, an allosteric AKT inhibitor, on primary fibroblast cells derived from patients with PIK3CA-related overgrowth spectrum (PROS). Neurogenetics. 2018;19(2):77–91.
Forde K, Resta N, Ranieri C, Rea D, Kubassova O, Hinton M, et al. Clinical experience with the AKT1 inhibitor miransertib in two children with PIK3CA-related overgrowth syndrome. Orphanet J Rare Dis. 2021;16(1):109.
Piqray. Prescribing information. Novartis Pharmaceuticals Corporation; 2020.
Lopez Gutierrez JC, Lizarraga R, Delgado C, Martinez Urrutia MJ, Diaz M, Miguel M, et al. Alpelisib treatment for genital vascular malformation in a patient with congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and spinal/skeletal anomalies and/or scoliosis (CLOVES) syndrome. J Pediatr Adolesc Gynecol. 2019;32(6):648–50.
Garneau AP, Haydock L, Tremblay LE, Isenring P. Somatic non-cancerous PIK3CA-related overgrowth syndrome treated with alpelisib in North America. J Mol Med. 2021;99(3):311–3.
Ozeki M, Fukao T. Generalized lymphatic anomaly and Gorham-Stout disease: overview and recent insights. Adv Wound Care (New Rochelle). 2019;8(6):230–45.
Seront E, Vikkula M, Boon LM. Venous malformations of the head and neck. Otolaryngol Clin North Am. 2018;51(1):173–84.
Acknowledgements
Medical editorial assistance was provided by Lisa Cimakasky, PhD, and was funded by Novartis Pharmaceuticals Corporation.
Funding
Financial support for medical editorial assistance was provided by Novartis Pharmaceuticals.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the conception, review, and final approval of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
G. Canaud: Personal fees from Novartis, Fresenius Medical Care, and BridgeBio; patent pending (WO2017140828A1). A. Hammill: Consultant and clinical trial contact for Novartis; clinical trial contact for ArQule/Merck and Venthera; compound received from Pfizer for investigator-initiated studies. D. Adams: Consultant to Novartis/Venthera. M. Vikkula: Consultant to Venthera. KMK-N: Investigator on clinical trial with Alpelisib.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Plain language summary.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Canaud, G., Hammill, A.M., Adams, D. et al. A review of mechanisms of disease across PIK3CA-related disorders with vascular manifestations. Orphanet J Rare Dis 16, 306 (2021). https://doi.org/10.1186/s13023-021-01929-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-021-01929-8