Abstract
In recent years, the incidence of lung cancer is increasing. Lung cancer has become one of the most malignant tumors with the highest incidence in the world, which seriously affects people’s health. The most important cause of death of lung cancer is metastasis. Therefore, it is crucial to understand the mechanism of lung cancer progression and metastasis. This review article discusses the physiological functions, pathological states and disorders of the lung and intestine based on the concepts of traditional Chinese medicine (TCM), and analyzes the etiology and mechanisms of lung cancer formation from the perspective of TCM. From the theory of “the exterior and interior of the lung and gastrointestinal tract”, the theory of “the lung-intestinal axis” and the progression and metastasis of lung cancer, we proposed e “lung-gut co-treatment” therapy for lung cancer. This study provides ideas for studying the mechanism of lung cancer and the comprehensive alternative treatment for lung cancer patients.
Similar content being viewed by others
Introduction
Over the past decades, lung cancer has persisted as one of the most common cancers in both men and women worldwide [1, 2]. Although progress in its diagnosis and treatment has been made in recent years, lung cancer still accounts for a high proportion of cancer-related deaths, and the 5-year survival rate is low [3, 4]. Recent studies suggest that intestinal flora have immune functions in addition to its barrier role in the gastrointestinal tract, and that dysbiosis of the intestinal flora is associated with inflammatory and malignant diseases of the gastrointestinal system. In recent years, it has been shown that imbalance or dysregulation of the gut microbiota is associated with development of various tumors [5,6,7]. There is a close relationship between the theory of "the lung and large intestine are external and internal" and the concept of the “lung-gut axis” in clinical medicine. However, the research on lung microecology, intestinal flora, and lung cancer development and treatment are limited. This review article will discuss the connection between "the lung and large intestine are external and internal" and lung-gut microecology, and finally explore the pathogenesis and the “lung-gut co-treatment” therapy to provide evidence for comprehensive alternative therapy for lung cancer.
The physiological functions of the lung and intestine in traditional Chinese medicine (TCM)
The physiological functions of the lung and intestine have been documented in ancient Chinese literatures. The main physiological functions of the lung according to TCM (Fig. 1) are: (1) The lung governs Qi and is responsible for respiration. This function of the lung includes the propagation of Wei Qi (defense Qi ). The body needs to continuously inhale clean air from the nature and eliminate turbid gas from the body in the process of metabolism. The lungs are the place of gas exchange in the body. Through the respiratory function of the lungs, the body continuously breathes in and out to maintain its vital activities. The function of the lungs in respiration is dependent on its function in governing gas diffusion and purification. In addition, the main function of the lung is to promote and disperse the Wei Qi. The lung is closely related to skin, sweat glands and hair follicle tissue functions, achieving the regulation of the lung Qi to prevent the invasion of external evils from the skin and hair. (2) The lung connects and regulates all blood vessels, which means that the whole body’s blood converges on the lung through hundreds of veins and arteries, and the heart. Through the respiration of the lung, the exchange of clean air in the lungs is carried out, and then the oxygenated blood is carried through the circulation (heart) to the whole body. The ancient Chinese medical book “Inner Canon of Yellow Emperor” says that the function of the lungs is equivalent to that of a court chancellor, assisting the monarch (heart) and governing the regulation of of Qi in the internal organs and blood. Chinese medicine believes that Qi, blood, and fluids are the fundamental substances of the human body, and the lung plays the role of governing and regulating the whole body through governing and regulating Qi, blood, and fluids, among them, governing and regulating Qi is most critical. (3) The lungs are responsible for regulating the water channels. It means that the lung governs the distribution, operation, and excretion of water and fluid in the body. Through the descent action of the lungs, the water is distributed upward and outward, spreading throughout the body, reaching the skin and hair, and is metabolized and excreted in the form of sweat; the water goes downward and becomes the source of urine production, and through the transpiration and gasification of the kidneys, the metabolized water is liquefied into urine and stored in the bladder, and then eliminated from the body. According to the Inner Canon of Yellow Emperor, the large intestine is the organ in charge of transmission and removing solid waste. Chinese medicine believes that the main physiological function of the large intestine is to transmit and transform the dregs. The large intestine accepts the food residues and fluid after digestion in the small intestine. Then it absorbs the remaining fluid to form feces, which is transmitted to the end of the large intestine and eliminated from the body through the anus. The primary physiological function of the small intestine is to digest and absorb foods and to transmit its essence. The small intestine is a vital organ that transmits food residues and plays an essential role in converting food into nutrients [8,9,10].
Physiological functions of lung and intestine in Traditional Chinese Medicine. The lungs are responsible for gas exchange and respiration, and are closely related to skin (A). Lung governance regulates blood circulation (B), The lungs participate the body’s water and fluid metabolism (C). Physiological functions of large intestine and small intestine in Traditional Chinese Medicine(D).
Pathological states and disorders of the lung and intestine
The Inner Canon of Yellow Emperor said that the lung and the gastrointestinal tract have the same Qi in the exterior and interior, so the condition of the large intestine can be reflected in the skin. Lung meridian begins at the heart and lungs and travels down to the large intestine. Yang is Zang (solid organs, such as the lungs), and the Yang meridians travel on the outer side of the hand; Yin is Fu (hollow organs, such as the gastrointestinal tract), and the Yin meridians travel on the inner side of the hand. This is also called the “exterior and interior relationship” of the hand. The lung and large intestine are related to each other through the meridians [11]. The lung governs Qi, moves water and disperses fluids; the large intestine governs fluids and enables normal fecal excretion. If the lung Qi cannot go down, dry stool and constipation can occur. If the lung Qi is weak and unable to push the force, the stool is hard and astringent, so called “Qi deficiency constipation”. If the Qi and blood cannot be consolidated and the clearing and turbidity are mixed and move downward, diarrhea will occur. The descending of lung Qi helps the function of large intestine conduction, and the normal function of large intestine conduction helps the descending function of the lung. Conversely, intestinal disease can transmit to the lung, and if the “evil” (pathogenic factors in TCM) is in the large intestine, or if the large intestine has excess heat and that rushes up to the lung, the lung will be impaired, the internal Qi will be blocked, which will affect the diffusion of lung and produce symptoms such as chest fullness and cough [12, 13]. It can be seen that lung and large intestine interact with each other. The lung disease can affect the intestine, and intestine disease affects the lung, and the lung and intestine can become dis-functioning at the same time (Fig. 2).
The etiology and mechanisms of lung cancer formation in TCM
The Chinese medical name for lung cancer is "Xiben" The Inner Canon of Yellow Emperor states that “the buildup of disease is gradually accumulated and cannot be cured in 2 or 3 years”. The Genuine Meaning of the Difficult Classic said that if Xiben is not cured, it will make people sensitive to cold and heat, with symptoms of shortness of breath and cough, and in serious cases, abscess of the lung may occur. Integrating ancient literature and modern concepts, Chinese medicine believes that the formation of lung cancer is mainly due to the following aspects (Fig. 3): First, internal deficiency of Yang Qi and imbalance of Yin and Yang in the internal organs are the main causes of lung cancer. Chronic lung diseases, depletion of lung Qi, or overexertion and deficiency of lung Qi and lung Yin will lead to external evil taking advantage of the deficiency and staying in the lungs, resulting in stagnation of blood flow in the lungs and becoming a mass. The second is injury caused by the seven emotions. Impatience will lead to counterflow of Qi and then cause Qi stagnation in the lung. The third is the internal accumulation of toxic smoke. Long-term smoking and fluid depletion would result in lung Yin deficiency. Qi with Yin deficiency, coupled with the smoke containing nicotine and tar and other toxic substances, can detain the lung orifices, block the airway, resulting in phlegm and dampness, blood clotting, and the formation of tumors. Fourth, the lung is attacked by evil toxic substances. The lung is a delicate viscus and is susceptible to be attacked by evil toxic substances, such as air pollution, asbestos, ore dust, airborne dust and radioactive substances, which lead to dysregulation of the purification of the lung Qi, stagnation of the lung Qi and promote blood stasis, resulting in the formation of tumors. Fifth, phlegm and dampness gather in the lungs; the spleen is responsible for transporting water and grain; spleen deficiency and dysregulation of transporting and transforming, and water cannot be transported and distributed, resulting in the production of phlegm from dampness and retention in the lungs, or uncontrolled diet and long-term use of fatty foods, resulting in water and dampness and phlegm, and phlegm gathering in the lungs, leading to stagnation of Qi and blood and stagnation in the lungs, and gradual formation of masses [14,15,16,17].
Lung and gastrointestinal microecology in the pathogenesis and treatment of lung cancer
Respiratory tract microbiota and lung cancer formation
New gene sequencing technologies have fundamentally revolutionized the understanding of lung as a sterile organ, suggesting that healthy human lungs are also colonized by bacterial flora [17], which is important for the formation of immune system [18] and the development of tolerance to allergens[19]. The biomass of the pulmonary microbiota is significantly lower than that of the intestinal flora, with approximately 10–100 bacteria per 1000 human cells [20, 21]. The pulmonary flora is a dynamic ecosystem, with the main bacterial phyla in the lungs and intestines of healthy subjects broadly consistent, containing the Firmicutes (Staphylococcus, Streptococcus, and Lactobacillus) and the bacteroidetes, followed by the Pseudomonadota and Actinomycetes, which tend to be increased in lung tumors [22,23,24,25,26]. There is a cross-border influence in pulmonary flora formation that may involve several pathways such as physical interactions, population sensing molecules, inflammatory responses, antimicrobial drugs, immune response modulation and nutrient exchange. For example [27], there is a synergistic effect between Pseudomonas and Streptococcus, where Pseudomonas stimulates Streptococcus growth, increases biofilm formation, or enhances Candida pathogenicity via Streptococcus. However, the regulation of the pulmonary flora is not limited to internal associations but also depends on the interaction between the intestine and the lungs. The human mouth and lung are the gateway for many microbial particles and bacteria to enter the human body [25]. There is evidence of an association between the pulmonary microbiota and lung health, and the pulmonary flora is thought to underlie the pathophysiology of many respiratory diseases [28]. The pulmonary flora is altered in many respiratory diseases, such as obstructive lung disease, interstitial lung disease, infectious diseases, and lung cancer. One study found a significant association between Mycobacterium tuberculosis (TB) and lung cancer [29, 30], and a possible reason for this is that persistent TB infection can cause production of tumor necrotic factors and lead to lung inflammation, pulmonary fibrosis leading to increase extracellular stroma, and finally lung cancer formation [31, 32]. Several other studies have shown that a low-density, diverse microbial ecosystem is present in bronchoalveolar lavage fluid, sputum, and lung tissue [33]. For example, Lee et al. reported that analysis of bronchoalveolar lavage fluid from 20 lung cancer patients showed that the abundance of two bacteria (Firmicutes and TM7) and two genera were significantly higher in lung cancer patients than in the healthy population [34, 35]. Moreover, TM7-3, Capnocytophaga, Sediminibacterium, and Microbacterium were also significantly enriched compared to controls [36,37,38] (Fig. 4). Lung cancers of different pathological tissue types are associated with specific microflora in the lung. A study in which sputum and saliva samples from 30 lung cancer patients [39] were analyzed by high-throughput sequencing of the 16 S ribosomal RNA (rRNA), which showed that the genera Capnocytophaga, Selenomonas, Veillonella, and Neisseria were associated with adenocarcinoma (AC) and small cell carcinoma (SCC), and these genera could be used as biomarkers for the diagnosis of different types of lung cancer. Currently, samples are obtained mainly by means of bronchoalveolar lavage fluid or tissue samples, which does not exclude the possibility of cross-contamination. In addition, studies have shown that the microbiota of the upper and lower airways are different; therefore, the results of this study need validation using larger sample experiments, better sampling methods, and considering the influence of different airway sites [40,41,42]. Studies on the connection between lung flora and lung cancer are gaining attention, however, there is a lack of exploration of the mechanisms of the role of lung flora in lung carcinogenesis. Large cohort, macrogenomic and metabolomic studies on the mechanisms are needed in the future.
Composition of respiratory tract flora in lung cancer patients and characteristics of intestinal flora in different types of lung cancers. The left side shows the main composition of respiratory microbiota in lung cancer patients, and the right side shows the composition of intestinal microbiota of three common types of lung cancers
The association between gastrointestinal flora imbalance and lung cancer
H. pylori infection may be related to the progression and treatment of lung cancer [43]. A retrospective study was conducted in two independent cohorts of PD-1-treated patients with non-small-cell lung cancer (NSCLC). Using enzyme-linked immunosorbent assay (ELISA) to measure serum H. pylori antigen-directed IgG antibodies, H. pylori seropositivity was associated with lower efficacy of anti-PD-1 immunotherapy [44]. The intestinal flora, the “connecting network” of biological metabolism, is a collection of bacteria colonizing the gastrointestinal tract [45, 46]. The intestinal microbiota is a critical component of the host immune response, performing many essential functions for the maintenance of human health. The gastrointestinal tract is the primary site of microbial growth in the human body. A 20–30-year-old person weighing 70 kg is estimated to have approximately 3.8 × 1013 bacteria colonizing the gastrointestinal tract, with over 1000 species representing 0.3% of the body weight. The flora composition is similar in most healthy populations, with more than 90% of all bacteria being of the firmicutes and bacteroidetes, followed by the Actinomycetes, Pseudomonadota and Verrucomicrobia, which together constitute 99% of the commensal flora [45, 46]. About 60 genera have been identified as “core” flora, mainly derived from Bacteroides, Bifidobacterium, Eubacterium, Rumenococcus, and E. faecalis [47]. Growing evidence suggests a close association of microbiota between the gastrointestinal and respiratory tracts, and that exacerbation of chronic intestinal and pulmonary diseases is associated with disorders and imbalances of microbial ecosystem [48, 49]. Intestinal dysbacteriosis is linked to different lung diseases, such as asthma [50], chronic obstructive pulmonary disease (COPD) [51], and lung cancer [52]. The intestinal flora provides energy by breaking down food and produces major metabolites such as short-chain fatty acids (SCFAs) [53,54,55]. The concentration of intestinal circulating SCFAs affects the level of IL-6 and IL-8 in lung tissues and is associated with the development of lung cancer [56, 57]. In addition, previous studies have found that butyrate-producing bacteria are dysregulated in the intestine of patients with non-small cell lung cancer [58]. Gut microbiota alpha diversity (number and abundance) and taxa homogeneity were significantly higher in non-malignant lung tissues than in tumor-bearing lung tissues, with no significant differences in beta diversity. Streptococcus, Prevotella, Blautia, Coprococcus, Bifidobacterium and Helicobocton Pyloni were found to be enriched in the intestinal flora of lung cancer patients [52, 59]. By analysis of 216 bronchoscopic samples, it was found that Gram-negative bacteria such as Haemophilus influenzae, Enterobacteriaceae and Escherichia coli were found to be prone to colonize in lung cancer tissues [60]. Tsay et al. demonstrated that patients with stage IIb-IV non-small cell lung cancer of the lower airway had more abundant disorders of the intestinal flora, which were associated with upregulation of IL17, PI3K, MAPK and ERK pathways in the airway transcriptome. It was suggested that Peillonella parvula plays a major driving role and promotes cancer progression [61]. In addition, microbiota-induced helper T-cell 17 (Th17) can promote lung cancer cell proliferation and angiogenesis[62]. Symbiotic bacteria are essential for γδT17 cell responses in the mouse lung as a potential mechanism for the shortened mean survival time in the Lewis lung cancer model. It has been shown [63, 64] that in the intestinal flora of lung adenocarcinoma patients, Bifidobacterium, Clostridium, and Prevotella were the dominant strains; in lung squamous cell carcinoma patients, a higher proportion of Bifidobacterium tumefaciens, Trichosporon spp. and Lactobacillus spp. were found; while Streptococcus spp., Anaerobes spp. and Bacillus spp. were more frequently shown in small cell lung cancer. These observations suggest that microbiota in the distal gut can also be used as a biomarker for lung cancer (Fig. 4).
Mechanism of lung-gut axis dysregulation in lung cancer progression
Although the composition of flora in the intestinal and respiratory tracts differs, the epithelia of both gastrointestinal and respiratory tracts develop structurally from the same embryonic structure, with similar mucosa in both anatomical structure and function. The early microbial colonization of the intestine and lung is similar. Thus, there is growing evidence highlighting the relationship and interactions between the intestine and lung, called the lung-gut axis [65, 66]. The lung-gut axis refers to the interface of immune information between two microbiota systems in the lung and the intestine. The “lung-gut axis” is mediated by inflammation and includes the gut-induced entry of immune cells, cytokines, bacteria, bacterial products, and some other microorganisms across the gastrointestinal barrier and into the body circulation through the blood and lymphatic systems [67]. The gut microbiota can modulate and alter the immune activity of the lung through bacterial lipopolysaccharides (LPS) and various bacterial metabolites (e.g., SCFA and others), which subsequently cause activation of multiple T lymphocytes (especially T-reg, T-h17, and Th1) after stimulation of dendritic cell production and migration to the lower respiratory tract through the circulating bloodstream. In contrast, bacterial metabolites lead to a decrease in tumor necrosis factor (TNF-a) through the mobilization of activated B cells and nuclear factor kappa-light-chain-enhancer (NFκB), which leads to a down-regulation of pattern recognition receptors (PRRs) and thus a decrease in cytokines (interleukin-1, interleukin-12, interleukin-18, TNF-α, IFN-γ and GM-CSF) (Fig. 5). This vital link maintains homeostasis of the pulmonary immune system and vice versa, thus avoiding ecological dysregulation of microorganisms [28, 68,69,70,71,72,73] .
Lung-gut axis theory and mechanisms of lung-gut interaction. The upper part shows the influence of intestinal microecology on lung diseases and the main pathways. The lower part shows pulmonary inflammation affects intestinal function. The lung and gut interact with each other through blood and lymphatic pathways
For that matter, how does the gut influence the progression of lung disease and even lung cancer? Gastrointestinal commensal flora maintains a stable state by regulating the immune function of the digestive system and distant organs, and regulates the T cell population outside the gastrointestinal tract and acts on regulatory T cells (Treg) to produce SCFAs and trigger systemic inflammatory responses. [68]. Intestinal commensal flora enhances host defense against bacterial pneumonia by adding interleukin 17 A(IL17A) and regulating GM-CSF signaling (Fig. 5) [74]. One study reported that excessive airway response syndrome in germ free mice was closely associated with T helper 2 (Th2) cells, cytokine (IL-4 and IL-5), and IgE levels in the lungs [75]. It has been shown that in antibiotic-treated mice, respiratory viral infections result in a substantial increase in mortality, which is correlated with reduced abundance of Treg cells in the respiratory and gastrointestinal tracts [76, 77] .
The study of gut microbiota provides a new reference for exploring the causes of malignant tumors. The escape of intestinal microorganisms and their toxic metabolites, such as surviving gastrointestinal bacteria, cell wall fragments, or protein fragments from bacterial death, occur together and enter the pulmonary circulation through the blood and lymphatic systems, causing an imbalance in the physiological state and influencing specific lung inflammation and tumorigenesis through various active molecules [78]. The bi-directional pulmonary-intestinal axis connects the microbiota of the lung and the intestine, and since they both belong to the mucosal immune system organ (MIS) and are covered by similar mucous membranes, they have similar functions of interaction between the immune system and the microbiota. In addition, they are indirectly linked to the lymphatic and circulatory systems and can therefore affect the immune system locally or cause systemic effects. The intensity of their immune response depends on the location of the first interaction. It has been shown that the clinical response and prognosis of lung and intestinal flora to immunotherapy are closely related to the induction of inflammatory processes and immune checkpoint inhibition [79]. Gut microbiota can affect the occurrence, development and prognosis of lung cancer by acting on the respiratory system through the gut-lung axis. Lymph and blood circulation provide physiological pathways for this process [80]. Protein fragments and cell wall components of dead or surviving bacteria will enter the chyle pool through the intestinal lymphatic system, and then enter the lungs through the blood circulation to activate adaptive immunity, leading to the differentiation and activation of T cells, as well as the activation of macrophages and dendritic cells, thus affecting the occurrence and treatment of lung cancer [81, 82]. Patients with lung cancer treated with antibiotics prior to chemotherapy or immunotherapy have less efficacy and shorter survival compared to subjects who did not receive antibiotics [83]. The intestinal microenvironment has an influential impact on the occurrence, progression and treatment of lung cancer, and intestinal flora can affect the development and metastasis of lung cancer through, regulation of the microecological system, the immune system and metabolites, and intestinal microenvironmental homeostasis plays a key role in the efficacy and prognosis of lung cancer radiotherapy, targeted therapy and immunotherapy.
Regulation of lung and intestinal micro-immune ecology inhibiting the progression of lung cancer
In the Northern Song Dynasty, it is said in the Classified Materia Medica from Historical Classics for Emergency that Tangerine peel decoction is used to treat pulmonary carbuncles caused by Xiben (lung cancer), and is taken with a decoction of gecko, donkey-hide gelatin, deerhorn glue, rhinoceros horn and antelope horn. In the Northern Song Dynasty, a formula book named Taiping Shenghui Fang recorded that Sangbaipi decoction was used to treat cough caused by lung cancer, coughing up blood and thick phlegm. In the Ming Dynasty, the literature Qixiao Liangfang (miracle cure) recorded that Xiben was treated with Xibendecoction, a formula containing pinellia ternata, cinnamon, ginseng, tetradium ruticarpum, mulberry root bark, lepidium, and prepared liquorice root, which was decocted in water and taken before meals. In the Ming Dynasty, it was recorded in the Chishui Xuanzhu Quanji that the Xiben was under the right side of the hypochondrium and developed into pulmonary carbuncle, and it is treated with Jujube paste pill (composed with tangerine peel, balloon flower root, lepidium and jujube). In the Qing Dynasty, A Brief Guide to Medical Formulas has written that Xiben is treated with a decoction of helianthus bark and lily with wine. A famous book The Divine Husbandman’s Herbal Foundation Canon of the Han Dynasty said that Xiben cannot be treated with moxibustion but must be treated with functional training in adjunct to medicine. Besides, the book Integration of Acupuncture and Moxibustion in Qing dynasty records that the Chize acupoint is used to treat shoulder and back pain, numbness, or pain in the limbs. In the Ming Dynasty, the medical book Lei Jing Tu Yi says that Xiben is under the right side of the ribs, and is treated with the Chize, Zhangmen, and Zusanli acupoints. The Source of Acupuncture and Moxibustion said that Qimen, Zhangmen, and Shouze acupoints can be used to treat lung cancer. In summary, ancient Chinese literature indicates that the symptoms of lung cancer are consistent with the clinical manifestations of lung cancer today, with local manifestations including cough, blood in sputum or coughing up blood, chest pain, and dyspnea, and systemic manifestations of emaciation, anemia, and cachexia [84,85,86,87]. In ancient times, the treatment plan for lung cancer was based on Chinese herbal formulas, and supplemented with functional training and acupuncture treatment. Based on the treatment of local symptoms of the lung, emphasis was placed on overall condition, especially the use of medicines that regulate the Qi and functions of the gastrointestinal tract, such as ginger, jujube, roasted licorice, hedgehog, and tangerine peel, etc. Moreover, immunity-boosting agents, such as ginseng, ass-hide gelatin, and deerhorn glue, were incorporated.
A growing set of studies suggests that dysregulation of the gut microbiota plays an important role in cancer progression and prognosis, and that changes in gut microbiome have the potential to increase immune checkpoint inhibitor (ICIs)-related adverse effects and severe immune-related toxicities (IrAEs) in patients with advanced metastases from NSCLC and hepatocellular liver cancer (HCC).Treatment with ICIs prior to antibiotics was associated with poor progression free survival (PFS) and overall survival (OS) [40, 88]. Routy et al. demonstrated that transplantation of gut microbiota from lung cancer patients that responded to immunosuppressive therapy (PD-1/PD-L1) into antibiotic-treated mice restored immune response, with bacteria Akkermansia muciniphila and Aliistipes uninctus being highly influential [40]. In addition, dietary supplement and adequate physical exercise are non-pharmacological healthy ways, and different dietary composition may affect gut microbiota structure [64, 89, 90]. Studies have confirmed the connection between high consumption of meat and fat and the development of lung disease and tumors [91,92,93,94]. The short-chain fatty acid cycle regulates the immune response through the intestinal flora and contributes to the maintenance of stasis in different organs, including the lungs. Consumption of a high-fiber diet and yogurt, rich in prebiotics and probiotics reduces the risk of lung cancers [95,96,97,98]. Numerous clinical studies suggest that the treatment of lung cancer must be considered in the context of the whole organism, with special emphasis on the impact of gastrointestinal micro-ecological regulation on lung cancer treatment.
The theory of “The lung and gastrointestinal tract are external and internal” is an important part of the doctrine of visceral manifestation theory. Qingfeiyin decoction can reduce the viral load, partially recover the colon atrophy caused by H1N1 virus, down-regulate the MAPK, tumor necrosis factor α(TNFα)and other inflammatory pathways, reduce lung injury, and improve the survival rate, which fully reflects the effectiveness of “lung-gut co-treatment”, and this theory has been applied to guide the treatment of refractory lung and intestinal diseases such as COVID-19 and ulcerative colitis, and reliable results have been obtained [99, 100].In the treatment of lung cancer, it should not only consider the lung but also the physiological function of the large intestine, and the treatment of intestinal diseases should take into account the physiological function of the lung [101,102,103,104], which is called “lung-gut co-treatment”. The physio-pathological relationship between the lung and gastrointestinal tract was shown in the Inner Canon of Yellow Emperor more than 3000 years ago, and modern studies have shown that decoctions named “Xuanbai Chengqi”, “Gegen Qinlian”, and tonic herbs such as ginseng, gardenia, angelica, and astragalus can improve acute lung tissue injury and pathological colon tissue damage caused by lipopolysaccharide (LPS) by regulating lung-intestinal mucosal immune function [105,106,107].Research on the mechanism of traditional Chinese medicine in the treatment of lung cancer has also made progress. Yiqi Yangyin Decoction (YYD) inhibits the proliferation of NSCLC cells. With the increase of YYD concentration, the expression of cell cycle-related proteins p53 and p21 increased, and the expression of cyclin D1 decreased. YYD inhibited the proliferation of NSCLC cells by inhibiting the EGFR-PI3K-AKT signaling pathway [108]. Feiyiliu Mixture could reduce the phosphorylation of EGFR and down-regulate the expression of cyclin, and up-regulate the level of cleaved Caspase-3 protein to promote cell apoptosis [109]. Therefore, lung cancer treatment should consider modulating intestinal function as well. The concept of lung-gut co-treatment could serve as the foundation for exploration of novel drugs.
Conclusions
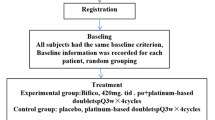
Traditional medicine has elaborated the pathophysiological characteristics of the lung and the gastrointestinal tract, and proposed the theory that the lung and gastrointestinal tract are external and internal. Growing evidence of modern medical research indicates an important and complex interaction between the lung and the intestine, as well as between the intestinal microbiota and host immunity, which is the lung-gut axis. The imbalance of lung and intestinal microecology and immunological barrier is closely related to lung cancer formation, metastasis, and prognosis. Based on the ancient theory of Chinese medicine and the modern findings of the lung-gut axis, we propose that treatment of lung cancer must be “lung-gut co-treatment”. The choice of “lung-gut co-treatment” should be made according to the characteristics of the patient’s disease, symptoms and signs, pathological types and clinical stages. According to the guidelines, surgical treatment is preferred for early stage lung cancer, and postoperative western medical treatment such as radiotherapy and chemotherapy is not needed. Generally, Chinese herb and patent medicine, acupuncture, and Daoyin can be recommended. For patients with advanced stage lung cancer who need radiotherapy and chemotherapy after surgery or are inoperable, interventional therapy, radiotherapy and chemotherapy, targeted therapy and immunotherapy can be selected according to their conditions. Probiotics and dietary modulation can be added. For patients who can not tolerate surgery, radiotherapy, chemotherapy or other western medicine treatment (or have poor efficacy), traditional Chinese medicine treatment should be given priority and combine with fecal microbiota transplantation, probiotics and dietary modulation (Fig. 6). Using “lung-gut co-treatment” to modify intestinal flora and improve the gut-lung immune imbalance provides a new strategy for the comprehensive treatment of lung cancer.
Availability of data and materials
Not applicable.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, Wender RC. Cancer screening in the United States, 2019: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2019;69(3):184–210.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Oliver AL. Lung cancer: epidemiology and screening. Surg Clin North Am. 2022;102(3):335–44.
Rami-Porta R, Bolejack V, Giroux DJ, Chansky K, Crowley J, Asamura H, Goldstraw P, International Association for the Study of Lung Cancer, Prognostic Factors Committee S, Participating ABM. The IASLC lung cancer staging project: the new database to inform the eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2014;9(11):1618–24.
Nagasaka M, Sexton R, Alhasan R, Rahman S, Azmi AS, Sukari A. Gut microbiome and response to checkpoint inhibitors in non-small cell lung cancer-a review. Crit Rev Oncol Hematol. 2020;145:102841.
Li LJ, Chen X, Yang WN, Xu XM, Lu LY, Wang J, Kong YX, Zheng JH. Traditional chinese medicine for the treatment of pulmonary fibrosis: a protocol for systematic review and meta-analysis of overview. Med (Baltim). 2020;99(31):e21310.
Pan MH, Zhu SR, Duan WJ, Ma XH, Luo X, Liu B, Kurihara H, Li YF, Chen JX, He RR. Shanghuo” increases disease susceptibility: modern significance of an old TCM theory. J Ethnopharmacol. 2020;250:112491.
Li LC, Kan LD. Traditional chinese medicine for pulmonary fibrosis therapy: progress and future prospects. J Ethnopharmacol. 2017;198:45–63.
He Q, Liu C, Shen L, Zeng L, Wang T, Sun J, Zhou X, Wan J. Theory of the exterior-interior relationship between the lungs and the large intestine to explore the mechanism of Eriobotrya japonica leaf water extract in the treatment of cough variant asthma. J Ethnopharmacol. 2021;281:114482.
Wang JY, Wang XY, Wu HY, Sun HY, Liu DM, Zhang W, Jin CX, Wang SR. The association between pulmonary function impairment and colon inflammation in ulcerative colitis patients: a scientific basis for exterior-interior correlation between lung and large intestine. Chin J Integr Med. 2016;22(12):894–901.
Yin LM, Zhang GQ, Yan XK, Wang Y, Xu YD, Yang YQ. An in vivo and in Vitro evaluation of the mutual interactions between the lung and the large intestine. Evid Based Complement Alternat Med. 2013;2013:695641.
Xue NZ, Fang RM, Lin LZ. Application of response evaluation criteria of traditional Chinese medicine for solid tumor in advanced non-small cell lung cancer. Chin J Integr Med. 2014;20(12):910–6.
Li Z, Feiyue Z, Gaofeng L. Traditional chinese medicine and lung cancer–from theory to practice. Biomed Pharmacother. 2021;137:111381.
Song Y, Miao L, Wang Z, Shi M. Combination of apatinib and docetaxel in treating advanced non-squamous non-small cell lung cancer patients with wild-type EGFR: a multi-center, phase II trial. J Thorac Dis. 2020;12(5):2450–8.
Unger SA, Bogaert D. The respiratory microbiome and respiratory infections. J Infect. 2017;74(Suppl 1):84–S88.
Gensollen T, Iyer SS, Kasper DL, Blumberg RS. How colonization by microbiota in early life shapes the immune system. Science. 2016;352(6285):539–44.
Gollwitzer ES, Saglani S, Trompette A, Yadava K, Sherburn R, McCoy KD, Nicod LP, Lloyd CM, Marsland BJ. Lung microbiota promotes tolerance to allergens in neonates via PD-L1. Nat Med. 2014;20(6):642–7.
Sze MA, Dimitriu PA, Hayashi S, Elliott WM, McDonough JE, Gosselink JV, Cooper J, Sin DD, Mohn WW, Hogg JC. The lung tissue microbiome in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1073–80.
Maddi A, Sabharwal A, Violante T, Manuballa S, Genco R, Patnaik S, Yendamuri S. The microbiome and lung cancer. J Thorac Dis. 2019;11(1):280–91.
Martin-Loeches I, Dickson R, Torres A, Hanberger H, Lipman J, Antonelli M, de Pascale G, Bozza F, Vincent JL, Murthy S, et al. The importance of airway and lung microbiome in the critically ill. Crit Care. 2020;24(1):537.
Frati F, Salvatori C, Incorvaia C, Bellucci A, Di Cara G, Marcucci F, Esposito S. The role of the microbiome in asthma: the gut(-)lung axis. Int J Mol Sci. 2018;20(1):123.
Dickson RP, Erb-Downward JR, Freeman CM, McCloskey L, Beck JM, Huffnagle GB, Curtis JL. Spatial variation in the healthy human lung microbiome and the adapted Island model of lung biogeography. Ann Am Thorac Soc. 2015;12(6):821–30.
Mur LA, Huws SA, Cameron SJ, Lewis PD, Lewis KE. Lung cancer: a new frontier for microbiome research and clinical translation. Ecancermedicalscience. 2018;12:866.
Garcia BA, Acosta NC, Tomar SL, Roesch LFW, Lemos JA, Mugayar LRF, Abranches J. Association of Candida albicans and Cbp(+) Streptococcus mutans with early childhood caries recurrence. Sci Rep. 2021;11(1):10802.
Metwalli KH, Khan SA, Krom BP, Jabra-Rizk MA. Streptococcus mutans, Candida albicans, and the human mouth: a sticky situation. PLoS Pathog. 2013;9(10):e1003616.
Enaud R, Prevel R, Ciarlo E, Beaufils F, Wieers G, Guery B, Delhaes L. The gut-lung axis in health and respiratory diseases: a place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. 2020;10:9.
Hong S, Mok Y, Jeon C, Jee SH, Samet JM. Tuberculosis, smoking and risk for lung cancer incidence and mortality. Int J Cancer. 2016;139(11):2447–55.
Lee CS, Shu CC, Chen YC, Liao KM, Ho CH. Tuberculosis treatment incompletion in patients with lung cancer: occurrence and predictors. Int J Infect Dis. 2021;113:200–6.
Pilaniya V, Gera K, Kunal S, Shah A. Pulmonary tuberculosis masquerading as metastatic lung disease. Eur Respir Rev. 2016;25(139):97–8.
Liang HY, Li XL, Yu XS, Guan P, Yin ZH, He QC, Zhou BS. Facts and fiction of the relationship between preexisting tuberculosis and lung cancer risk: a systematic review. Int J Cancer. 2009;125(12):2936–44.
Vandeputte D, Joossens M. Effects of low and high FODMAP diets on human gastrointestinal microbiota composition in adults with intestinal diseases: a systematic review. Microorganisms. 2020;8(11):1638.
Lee SH, Sung JY, Yong D, Chun J, Kim SY, Song JH, Chung KS, Kim EY, Jung JY, Kang YA, et al. Characterization of microbiome in bronchoalveolar lavage fluid of patients with lung cancer comparing with benign mass like lesions. Lung Cancer. 2016;102:89–95.
Marchesi JR, Ravel J. The vocabulary of microbiome research: a proposal. Microbiome. 2015;3:31.
Cheng C, Wang Z, Wang J, Ding C, Sun C, Liu P, Xu X, Liu Y, Chen B, Gu B. Characterization of the lung microbiome and exploration of potential bacterial biomarkers for lung cancer. Transl Lung Cancer Res. 2020;9(3):693–704.
Jin C, Lagoudas GK, Zhao C, Bullman S, Bhutkar A, Hu B, Ameh S, Sandel D, Liang XS, Mazzilli S, et al. Commensal microbiota promote lung cancer development via gammadelta T cells. Cell. 2019;176(5):998-1013e1016.
Ge Y, Wang X, Guo Y, Yan J, Abuduwaili A, Aximujiang K, Yan J, Wu M. Correction to: gut microbiota influence tumor development and alter interactions with the human immune system. J Exp Clin Cancer Res. 2021;40(1):334.
Cameron SJS, Lewis KE, Huws SA, Hegarty MJ, Lewis PD, Pachebat JA, Mur LAJ. A pilot study using metagenomic sequencing of the sputum microbiome suggests potential bacterial biomarkers for lung cancer. PLoS ONE. 2017;12(5):e0177062.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillere R, Fluckiger A, Messaoudene M, Rauber C, Roberti MP, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359(6371):91–7.
Man WH, de Steenhuijsen Piters WA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol. 2017;15(5):259–70.
Budden KF, Shukla SD, Rehman SF, Bowerman KL, Keely S, Hugenholtz P, Armstrong-James DPH, Adcock IM, Chotirmall SH, Chung KF, et al. Functional effects of the microbiota in chronic respiratory disease. Lancet Respir Med. 2019;7(10):907–20.
Ece F, N FH, Erdal N, Gedik C, Guney C, Aksoy F. Does helicobacter pylori infection play a role in lung cancer? Respir Med. 2005;99(10):1258–62.
Oster P, Vaillant L, Riva E, McMillan B, Begka C, Truntzer C, Richard C, Leblond MM, Messaoudene M, Machremi E, et al. Helicobacter pylori infection has a detrimental impact on the efficacy of cancer immunotherapies. Gut. 2022;71(3):457–66.
Tap J, Mondot S, Levenez F, Pelletier E, Caron C, Furet JP, Ugarte E, Munoz-Tamayo R, Paslier DL, Nalin R, et al. Towards the human intestinal microbiota phylogenetic core. Environ Microbiol. 2009;11(10):2574–84.
Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017;474(11):1823–36.
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14(8):e1002533.
He Y, Wen Q, Yao F, Xu D, Huang Y, Wang J. Gut-lung axis: the microbial contributions and clinical implications. Crit Rev Microbiol. 2017;43(1):81–95.
Schuijt TJ, Lankelma JM, Scicluna BP, de Sousa e Melo F, Roelofs JJ, de Boer JD, Hoogendijk AJ, de Beer R, de Vos A, Belzer C, et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut. 2016;65(4):575–83.
Hufnagl K, Pali-Scholl I, Roth-Walter F, Jensen-Jarolim E. Dysbiosis of the gut and lung microbiome has a role in asthma. Semin Immunopathol. 2020;42(1):75–93.
Vaughan A, Frazer ZA, Hansbro PM, Yang IA. COPD and the gut-lung axis: the therapeutic potential of fibre. J Thorac Dis. 2019;11(Suppl 17):2173–S2180.
Liu F, Li J, Guan Y, Lou Y, Chen H, Xu M, Deng D, Chen J, Ni B, Zhao L, et al. Dysbiosis of the gut microbiome is associated with tumor biomarkers in lung cancer. Int J Biol Sci. 2019;15(11):2381–92.
Srikanth CV, McCormick BA. Interactions of the intestinal epithelium with the pathogen and the indigenous microbiota: a three-way crosstalk. Interdiscip Perspect Infect Dis. 2008;2008:626827.
Tremaroli V, Backhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489(7415):242–9.
Macfarlane S, Macfarlane GT. Regulation of short-chain fatty acid production. Proc Nutr Soc. 2003;62(1):67–72.
Sanmamed MF, Carranza-Rua O, Alfaro C, Onate C, Martin-Algarra S, Perez G, Landazuri SF, Gonzalez A, Gross S, Rodriguez I, et al. Serum interleukin-8 reflects tumor burden and treatment response across malignancies of multiple tissue origins. Clin Cancer Res. 2014;20(22):5697–707.
Biagi E, Nylund L, Candela M, Ostan R, Bucci L, Pini E, Nikkila J, Monti D, Satokari R, Franceschi C, et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS ONE. 2010;5(5):e10667.
Bingula R, Filaire M, Radosevic-Robin N, Berthon JY, Bernalier-Donadille A, Vasson MP, Thivat E, Kwiatkowski F, Filaire E. Characterisation of gut, lung, and upper airways microbiota in patients with non-small cell lung carcinoma: study protocol for case-control observational trial. Med (Baltim). 2018;97(50):e13676.
Zhuang H, Cheng L, Wang Y, Zhang YK, Zhao MF, Liang GD, Zhang MC, Li YG, Zhao JB, Gao YN, et al. Dysbiosis of the gut microbiome in lung cancer. Front Cell Infect Microbiol. 2019;9:112.
Laroumagne S, Salinas-Pineda A, Hermant C, Murris M, Gourraud PA, Do C, Segonds C, Didier A, Mazieres J. [Incidence and characteristics of bronchial colonisation in patient with lung cancer: a retrospective study of 388 cases]. Rev Mal Respir. 2011;28(3):328–35.
Tsay JJ, Wu BG, Sulaiman I, Gershner K, Schluger R, Li Y, Yie TA, Meyn P, Olsen E, Perez L, et al. Lower airway dysbiosis affects lung cancer progression. Cancer Discov. 2021;11(2):293–307.
Chang SH, Mirabolfathinejad SG, Katta H, Cumpian AM, Gong L, Caetano MS, Moghaddam SJ, Dong C. T helper 17 cells play a critical pathogenic role in lung cancer. Proc Natl Acad Sci U S A. 2014;111(15):5664–9.
Bernicker EH, Quigley EMM. The gut microbiome influences responses to programmed death 1 therapy in Chinese lung cancer patients—the benefits of diversity. J Thorac Oncol. 2019;14(8):1319–22.
Bingula R, Filaire M, Radosevic-Robin N, Bey M, Berthon JY, Bernalier-Donadille A, Vasson MP, Filaire E. Desired turbulence? Gut-lung axis, immunity, and lung cancer. J Oncol. 2017;2017:5035371.
Dickson RP, Erb-Downward JR, Martinez FJ, Huffnagle GB. The Microbiome and the respiratory tract. Annu Rev Physiol. 2016;78:481–504.
Yan X, Yang M, Liu J, Gao R, Hu J, Li J, Zhang L, Shi Y, Guo H, Cheng J, et al. Discovery and validation of potential bacterial biomarkers for lung cancer. Am J Cancer Res. 2015;5(10):3111–22.
Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, Hoke AV, Levangie MW, Kumar R, Chakraborty N, et al. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol. 2017;312(6):G559–71.
Samuelson DR, Welsh DA, Shellito JE. Regulation of lung immunity and host defense by the intestinal microbiota. Front Microbiol. 2015;6:1085.
Bassis CM, Erb-Downward JR, Dickson RP, Freeman CM, Schmidt TM, Young VB, Beck JM, Curtis JL, Huffnagle GB. Analysis of the upper respiratory tract microbiotas as the source of the lung and gastric microbiotas in healthy individuals. mBio. 2015;6(2):e00037.
Jayawardena R, Sooriyaarachchi P, Chourdakis M, Jeewandara C, Ranasinghe P. Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. Diabetes Metab Syndr. 2020;14(4):367–82.
Santacroce L, Charitos IA, Ballini A, Inchingolo F, Luperto P, De Nitto E, Topi S. The human respiratory system and its microbiome at a glimpse. Biology (Basel). 2020;9(10):318.
Santacroce L, Charitos IA, Carretta DM, De Nitto E, Lovero R. The human coronaviruses (HCoVs) and the molecular mechanisms of SARS-CoV-2 infection. J Mol Med (Berl). 2021;99(1):93–106.
Santacroce L, Inchingolo F, Topi S, Del Prete R, Di Cosola M, Charitos IA, Montagnani M. Potential beneficial role of probiotics on the outcome of COVID-19 patients: an evolving perspective. Diabetes Metab Syndr. 2021;15(1):295–301.
Brown RL, Sequeira RP, Clarke TB. The microbiota protects against respiratory infection via GM-CSF signaling. Nat Commun. 2017;8(1):1512.
Herbst T, Sichelstiel A, Schar C, Yadava K, Burki K, Cahenzli J, McCoy K, Marsland BJ, Harris NL. Dysregulation of allergic airway inflammation in the absence of microbial colonization. Am J Respir Crit Care Med. 2011;184(2):198–205.
Grayson MH, Camarda LE, Hussain SA, Zemple SJ, Hayward M, Lam V, Hunter DA, Santoro JL, Rohlfing M, Cheung DS, et al. Intestinal microbiota disruption reduces regulatory T cells and increases respiratory viral infection mortality through increased IFNgamma production. Front Immunol. 2018;9:1587.
Cait A, Hughes MR, Antignano F, Cait J, Dimitriu PA, Maas KR, Reynolds LA, Hacker L, Mohr J, Finlay BB, et al. Microbiome-driven allergic lung inflammation is ameliorated by short-chain fatty acids. Mucosal Immunol. 2018;11(3):785–95.
Keely S, Talley NJ, Hansbro PM. Pulmonary-intestinal cross-talk in mucosal inflammatory disease. Mucosal Immunol. 2012;5(1):7–18.
Gong J, Chehrazi-Raffle A, Placencio-Hickok V, Guan M, Hendifar A, Salgia R. The gut microbiome and response to immune checkpoint inhibitors: preclinical and clinical strategies. Clin Transl Med. 2019;8(1):9.
Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, Hansbro PM. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017;15(1):55–63.
Ramakrishna C, Kujawski M, Chu H, Li L, Mazmanian SK, Cantin EM. Bacteroides fragilis polysaccharide a induces IL-10 secreting B and T cells that prevent viral encephalitis. Nat Commun. 2019;10(1):2153.
Ladinsky MS, Araujo LP, Zhang X, Veltri J, Galan-Diez M, Soualhi S, Lee C, Irie K, Pinker EY, Narushima S, et al. Endocytosis of commensal antigens by intestinal epithelial cells regulates mucosal T cell homeostasis. Science. 2019;363(6431):eaat4042.
Elkrief A, Derosa L, Kroemer G, Zitvogel L, Routy B. The negative impact of antibiotics on outcomes in cancer patients treated with immunotherapy: a new independent prognostic factor? Ann Oncol. 2019;30(10):1572–9.
Chansky K, Detterbeck FC, Nicholson AG, Rusch VW, Vallieres E, Groome P, Kennedy C, Krasnik M, Peake M, Shemanski L, et al. The IASLC lung cancer staging project: external validation of the revision of the TNM stage groupings in the eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2017;12(7):1109–21.
Wahbah M, Boroumand N, Castro C, El-Zeky F, Eltorky M. Changing trends in the distribution of the histologic types of lung cancer: a review of 4,439 cases. Ann Diagn Pathol. 2007;11(2):89–96.
Kong L, Wu Z, Zhao Y, Lu X, Shi H, Liu S, Li J. Qigesan reduces the motility of esophageal cancer cells via inhibiting Gas6/Axl and NF-kappaB expression. Biosci Rep. 2019;39(6):BSR20190850.
Kan H, Stevens J, Heiss G, Rose KM, London SJ. Dietary fiber, lung function, and chronic obstructive pulmonary disease in the atherosclerosis risk in communities study. Am J Epidemiol. 2008;167(5):570–8.
Jin Y, Dong H, Xia L, Yang Y, Zhu Y, Shen Y, Zheng H, Yao C, Wang Y, Lu S. The diversity of gut microbiome is associated with favorable responses to anti-programmed death 1 immunotherapy in Chinese patients with NSCLC. J Thorac Oncol. 2019;14(8):1378–89.
Gill N, Wlodarska M, Finlay BB. The future of mucosal immunology: studying an integrated system-wide organ. Nat Immunol. 2010;11(7):558–60.
Nakayama J, Watanabe K, Jiang J, Matsuda K, Chao SH, Haryono P, La-Ongkham O, Sarwoko MA, Sujaya IN, Zhao L, et al. Diversity in gut bacterial community of school-age children in Asia. Sci Rep. 2015;5:8397.
Gnagnarella P, Caini S, Maisonneuve P, Gandini S. Carcinogenicity of high consumption of meat and lung cancer risk among non-smokers: a comprehensive meta-analysis. Nutr Cancer. 2018;70(1):1–13.
Lippi G, Mattiuzzi C, Cervellin G. Meat consumption and cancer risk: a critical review of published meta-analyses. Crit Rev Oncol Hematol. 2016;97:1–14.
Yan L, Sundaram S, Mehus AA, Picklo MJ. Time-restricted feeding attenuates high-fat diet-enhanced spontaneous metastasis of Lewis lung carcinoma in mice. Anticancer Res. 2019;39(4):1739–48.
Huerta-Yepez S, Tirado-Rodriguez A, Montecillo-Aguado MR, Yang J, Hammock BD, Hankinson O. Aryl Hydrocarbon receptor-dependent inductions of omega-3 and omega-6 polyunsaturated fatty acid metabolism act inversely on tumor progression. Sci Rep. 2020;10(1):7843.
Ratajczak W, Ryl A, Mizerski A, Walczakiewicz K, Sipak O, Laszczynska M. Immunomodulatory potential of gut microbiome-derived short-chain fatty acids (SCFAs). Acta Biochim Pol. 2019;66(1):1–12.
Serini S, Trombino S, Oliva F, Piccioni E, Monego G, Resci F, Boninsegna A, Picci N, Ranelletti FO, Calviello G. Docosahexaenoic acid induces apoptosis in lung cancer cells by increasing MKP-1 and down-regulating p-ERK1/2 and p-p38 expression. Apoptosis. 2008;13(9):1172–83.
Zajdel A, Wilczok A, Tarkowski M. Toxic effects of n-3 polyunsaturated fatty acids in human lung A549 cells. Toxicol In Vitro. 2015;30(1 Pt B):486–91.
Yin Y, Sui C, Meng F, Ma P, Jiang Y. The omega-3 polyunsaturated fatty acid docosahexaenoic acid inhibits proliferation and progression of non-small cell lung cancer cells through the reactive oxygen species-mediated inactivation of the PI3K /Akt pathway. Lipids Health Dis. 2017;16(1):87.
Li X, Wang M, Liu C, Xiao Y, Li M, Ban C, Huang Y, Cheng M, Song L, Liu G, et al. Qingfeiyin decoction inhibits H1N1 virus infection via modulation of gut microbiota and inflammatory pathways in a murine model. Front Pharmacol. 2022;13:874068.
Lou Z, Zhao H, Lyu G. [Mechanism and intervention of mucosal immune regulation based on “lung and large intestine being interior-exteriorly related” theory of traditional chinese medicine]. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(6):665–78.
He W, Cheng M. [Meta-analysis on effectiveness and safety of traditional chinese medicine combined with first-generation EGFR-TKI in treating advanced non-small cell lung cancer]. Zhongguo Zhong Yao Za Zhi. 2017;42(13):2591–8.
Tao WW, Jiang H, Tao XM, Jiang P, Sha LY, Sun XC. Effects of acupuncture, Tuina, Tai Chi, Qigong, and traditional chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: a Meta-analysis. J Pain Symptom Manage. 2016;51(4):728–47.
Li Z, Zhang R, Yin X, Li N, Cui S, Wang T, Tan X, Shen M, Guo Y, Wang J, et al. Realgar (as(4)S(4)), a traditional chinese medicine, induces acute promyelocytic leukemia cell death via the Bcl-2/Bax/Cyt-C/AIF signaling pathway in vitro. Aging. 2022;14(17):7109–25.
Liao YH, Li CI, Lin CC, Lin JG, Chiang JH, Li TC. Traditional chinese medicine as adjunctive therapy improves the long-term survival of lung cancer patients. J Cancer Res Clin Oncol. 2017;143(12):2425–35.
Adesso S, Russo R, Quaroni A, Autore G, Marzocco S. Astragalus membranaceus extract attenuates inflammation and oxidative stress in intestinal epithelial cells via NF-kappaB activation and Nrf2 response. Int J Mol Sci. 2018;19(3):800.
Cui Y, Wang Q, Sun R, Guo L, Wang M, Jia J, Xu C, Wu R. Astragalus membranaceus (Fisch.) bunge repairs intestinal mucosal injury induced by LPS in mice. BMC Complement Altern Med. 2018;18(1):230.
Su KL, Xiong XJ. [Treatment strategy and thought on classical herbal formulae for coronavirus disease 2019]. Zhongguo Zhong Yao Za Zhi. 2021;46(2):494–503.
Jiao P, Wang Y, Ren G, Chu D, Li Y, Sang T. Integrating network pharmacology and experimental validation to elucidate the mechanism of Yiqi Yangyin decoction in suppressing non-small-cell lung cancer. Biomed Res Int. 2023;2023:4967544.
Shi J, Hao S, Liu X, Li Y, Zheng X. Feiyiliu mixture sensitizes EGFR(Del19/T790M/C797S) mutant non-small cell lung cancer to osimertinib by attenuating the PRC1/Wnt/EGFR pathway. Front Pharmacol. 2023;14:1093017.
Funding
This study was supported by Tianjin University and The Fourth Affiliated Hospital of Tianjin University of Traditional Chinese Medicine.
Author information
Authors and Affiliations
Contributions
LYK wrote the manuscript. XYC and XL collected relevant information and helped with the writing. QC and DHY jointly conceived the study and revised the final draft of the manuscript, which was approved by all authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, LY., Chen, XY., Lu, X. et al. Association of lung-intestinal microecology and lung cancer therapy. Chin Med 18, 37 (2023). https://doi.org/10.1186/s13020-023-00742-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-023-00742-8