Abstract
Background
Synchronous bilateral lung lesions are emerging as a common but tricky disease for surgical management. Whether one or two-stage surgery should be taken remains in debate. We retrospectively analysed 151 patients who underwent one and two-stage Video Assisted Thoracic Surgery (VATS) to investigate the safety and feasibility of the two surgical approaches.
Methods
A total of 151 patients were included in the study. Propensity score matching was performed to minimize the baseline characteristics difference between one and two-stage groups. Clinical factors including in-hospital days after surgery, chest tube drainage days, types and severity of post-operative complications were compared between the two groups. Logistic univariate and multivariate analyses were used to find the risk factors for post-operative complications. Nomogram was built to select the low risk candidates for the one-stage VATS.
Results
After propensity score matching, 36 one-stage and 23 two-stage patients were enrolled. The age (p = 0.669), gender (p = 0.3655), smoking status (p = 0.5555), pre-operative comorbidity (p = 0.8162), surgical resection (p = 0.798) and lymph node dissection (p = 9036) were balanced between the two groups. There was no difference in post-surgery hospital days (8.67 ± 2.68 versus 8.46 ± 2.92, p = 0.7711) and chest tube retaining days (5.47 ± 2.20 versus 5.46 ± 1.95, p = 0.9772). Moreover, post-operative complications also showed no difference between one-stage and two-stage groups (p = 0.3627). Univariate and multivariate analysis revealed that advanced age (p = 0.0495), pre-surgical low haemoglobin (p = 0.045) and blood loss (p = 0.002) were risk factors for post-operative complications. Nomogram built with the three risk factors showed reasonable predictive value.
Conclusions
One-stage VATS for synchronous bilateral lung lesion patients was proved to be a safety procedure. Advanced age, pre-surgical low haemoglobin and blood loss may predict complications after surgery.
Similar content being viewed by others
Background
Low dose computed tomography (LDCT) is widely used in lung cancer screening. As a result, an increasing number of small nodules that appear as ground-glass opacities and solid nodules are found [1]. There has been numerous research on the diagnosis and treatment of solitary lung lesions, but very few on synchronous bilateral lung lesions (SBLL). SBLL patients, however, are not rarely seen. It is often confusing for the surgeons to make clinical decision on whether these patients should receive surgical treatment. As there is no consensus on the surgical management of bilateral lung lesions, the treatment often varies among surgeons.
In recent decades, video-assisted thoracic surgery (VATS) has become the standard of care for patients with pulmonary nodules. With the maturation of VATS technique in solitary nodules surgery, some surgeons are applying it in SBLL patients. However, considering the risk of post-operative pulmonary dysfunction and complications, one-stage bilateral VATS lung resection is not used routinely [2]. Some surgeons made exploratory investigation on the one-stage VATS and achieved inspiring results [3, 4]. In this study, we retrospectively reviewed perioperative data of 151 patients who underwent VATS for SBLL in our centre and compared the outcomes after propensity score matching (PSM). Furthermore, we also investigated the potential risk factors for post-operative complications in one-stage surgery. To our knowledge, this is the first study that demonstrate the safety and feasibility of one-stage VATS for SBLL treatment.
Methods
Medical records of lung surgeries performed at Hebei Medical University Fourth Hospital between December 2014 and December 2020 were collected. To protect the privacy of the patients, their names and IDs were desensitized. During this period, a total of 10,711 patients underwent lung resections, with 109 synchronous bilateral lung lesions (SBLL) receiving one-stage bilateral VATS lung resection. Meanwhile, two-stage VATS surgery was performed on 42 SBLL patients. Medical data including sex, age, pre-operation comorbidity, laboratory test, pulmonary function test, surgery type, lymph node dissection, chest tube duration, post-operative days and complications were all collected. Complications after surgery were defined according to the Clavien–Dindo classification [5].
Surgery procedures
General anaesthesia was implemented with intravenous remifentanil and inhalational sevoflurane. Double-lumen tracheal intubation or single-lumen intubation with bronchus blocker was used to maintain the contralateral ventilation to the surgery side. Surgeries were performed by experienced surgeons who routinely perform VATS surgery for over 5 to 10 years. The one- or two-stage VATS were at the choice of the surgeon, according to the patient physical and psychological condition, performance status, tumour size and planned resection scope, etc. For younger, better performance status patients, some surgeons tended to resect all the lesions at one time. Whereas, for some older patients, if the lesions were small and located peripherally, wedge resections were suitable, and one-stage bilateral VATS could be chose by the surgeons. Some cases showed typical invasive adenocarcinoma which requires lobectomy at one side, and at the other side the lesion may need complex segmentectomy. A two-stage VATS surgery may be selected by most surgeons. Uni-portal, bi-portal or tri-portal VATS approaches were decided by the surgeon’s preference. Normally, in one-stage bilateral surgery, wedge resection and frozen biopsy were performed for the major lesion located at the peripheral of the lung. Anatomical segmentectomy or wedge resection was performed for small lesions less than 2 cm in diameter, depending on their location: central or peripheral. Lobectomy was performed for lesions larger than 2 cm in diameter or pathologically reported as adenocarcinoma in the frozen biopsy. Two-stage surgery was defined as that a planned second resection was performed within one year from the first surgery. In two-stage surgery, the major lesion was resected in the first stage, which normally needed lobectomy. In the second stage, the resection plan was determined by the lesion characteristics and pulmonary function. Chest tubes were routinely placed on each surgical side. Among all the subjects, one case was converted to thoracotomy intraoperatively due to difficult lymph node dissection.
Postoperative management
Antibiotics and analgesics were prescribed routinely. Chest radiography and laboratory test were issued within 2 days after surgery. Early ambulation and coughing were encouraged. Enteral nutrition was conducted on the first day after surgery. The chest tube was removed when there was no sign of air leak in X-ray and drainage was less than 200mL per day.
Statistical analysis
Continuous variables were presented as mean values ± standard deviation. Categorical variables were presented as numbers. Continuous variables with normal distribution were compared using two sample t test. Categorical variables were compared by chi-square test. For the patients who were planned to have bilateral lung surgery, surgeons tended to choose younger ones for the one-stage surgery. To resolve this potential bias, propensity score matching was introduced to balance the baseline characteristics between one- and two-stage group. While the analysis for the one-stage group complications was performed in the pre-matched “whole” data, as there was no comparation between one- and two-stage group. Logistic regression was performed to identify the risk factors of post-operative complications in one-stage surgery. Chi square test and Mann-Whitney-U test was performed to investigate the difference in number and grade of the complications between the two groups. The receiver operating characteristics (ROC) curves were plotted for the risk factors of one-stage VATS complications A nomogram was established to predict the risk of complications of one-stage VATS. Harrell Consistency Index (C-Index) and area under ROC curve (AUC) were used to evaluate the nomogram, and calibration curve were used to validate the nomogram performance. Statistical analysis was performed with R (version 4.2.0) in R Studio software (Version 1.4.1717, Boston, MA). For propensity score matching analysis, package “MatchIt” was used. Significance level was set at 5%.
Results
Patient characteristics
A total of 109 patients underwent one-stage bilateral VATS lung resection, while 42 received two-stage treatment during this time. For the two-stage patients, values of “post-surgery days” and “chest tube days” were the average of the two operations. Systematic lymph node dissection was marked if it was performed on either side of the mediastinal during the operations. Lymph node sampling was recorded when it was performed on both sides, or only one side but without systematic lymph node dissection on the other side. The baseline of patient characteristics was shown in Table 1.
Although the gender, age, and smoking status were not statistically different before propensity matching (PSM), the percentage of smokers in one-stage surgery was higher than that in two-stage group. Moreover, there were significantly more patients with comorbidities such as hypertension, coronary artery disease, and diabetes in two-stage group, which could possibly be the reason for their two-stage operations. Some variables such as neutrophils/lymphocyte ratio (NLR), platelet (PLT), haemoglobin (HB), surgery duration, and blood loss were not included into the PSM, because the first operation had a remarkable influence on these factors, making them pointless to compare.
Overall surgery results
Most patients recovered quickly without any complications. Bedside chest x-ray was routinely taken on the first or the second post-operative day and 86.1% of patients showed well-inflated lungs with clear thoracic cavities (94 in 109 one-stage and 36 in 42 two-stage). The average chest tube removal days were 5.64 in one-stage and 5.56 in two-stage. The average discharge days were 8.72 in one-stage and 8.4 in two-stage. (Table 1)
Propensity score matching and outcomes
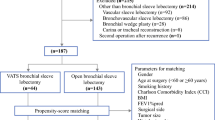
To minimize the difference of patients’ characteristics between two groups, propensity score matching (PSM) was adopted. The process was summarized in Fig. 1 as mentioned above. PSM was conducted using “MatchIt” package with nearest-neighbour method and a caliper of 0.03. Figure 2 showed the propensity score matching of raw data and matched data. After matching, the control and treated groups achieved well-balanced results. Finally, 36 one-stage patients and 23 two-stage patients were included in the analysis set.
In the post-match set, there was no significant difference in post-operative hospital days (8.67 ± 2.68 versus 8.46 ± 2.92, p = 0.7711) and chest tube retaining days (5.47 ± 2.20 versus 5.46 ± 1.95, p = 0.9772). More importantly, post-operative complications also showed no difference in number of cases between one-stage and two-stage groups, statistically (p = 0.3627). Further analysis according to the Clavien–Dindo classification was performed. The grade of the complications between the two groups also showed no significant difference (p = 0.3961) (Table 2). No perioperative death occurred.
Risk factors of post-operative complications in one-stage surgery
Results showed that the complications of one-stage surgery were no more common and severe than that of two-stage surgery. Hence, one-stage VATS may be an optimal choice for SBLL patients. However, lung resection was still a major procedure with potential complications, and some may even lead to life threatening consequence. Therefore, risk factor analysis was subsequently performed on the all 151 one-stage patients to reveal those which may possibly be correlated to adverse conditions. As shown in Table 3, univariate analysis showed that age, HB, surgery duration, and blood loss may be related to post-operative complications in one-stage surgery (p < 0.05). Furthermore, in multivariate analysis, results demonstrated that advanced age (p = 0.04951, OR 1.07, 95% CI 1–1.15), pre-surgical low HB (p = 0.045, OR 1.04, 95% CI 1–1.08) and increased blood loss (p = 0.002, OR 1.02, 95% CI 1.01–1.04) were risk factors for complications in one-stage surgery. Receiver operating characteristics curves were plotted for the risk factors. (Fig. 3). Area under the ROC curve and its 95% CI were also calculated.
Nomogram and its evaluation
We combined the risk factors from multivariate analysis, age, HB and blood loss, into the building of the nomogram for the prediction of one-stage surgery complications (Fig. 4). The line on the bottom indicates the probability that complications may occur after one-stage surgery. Area under the ROC curve of the nomogram was 0.705 (95% CI 0.600–0.811) in the model from the one-stage surgery data, with a sensitivity of 83.8% and a specificity of 56.1% (Fig. 5). The calibration curve for the nomogram demonstrated reasonable consistency between actual and predicted results (Fig. 6). These findings indicated that the nomogram could provide suggestions for the risk of one-stage surgery complications.
Discussion
Choosing a proper surgical plan for synchronized bilateral lung lesion patients has been emerging as a critical problem for thoracic surgeons. Moreover, there is still no consensus on whether one-stage or two-stage surgery should be adopted. Originally, bilateral pulmonary resection was performed mostly on a two-stage basis in our centre. As the VATS technique developed, one-stage surgery cases were also growing. In this study, we retrospectively reviewed 151 cases of such patients who underwent one-stage and two-stage bilateral VATS pulmonary resections. To our knowledge, this is the largest cohort of bilateral pulmonary resection research comparing one- and two- stage surgery after bias balanced with propensity score matching method. We found that most patients in both one and two-stage group had an uneventful postoperative recovery. Among all the 151 VATS cases, there was only one intraoperative thoracotomy conversion due to lymph node adhesion. Post-operative complications were observed in 33 out of 109 one-stage surgery (30.28%) and 14 out of 42 two-stage surgery (33.33%). Our results were similar to other researches, which indicated that one-stage VATS surgery had comparable outcomes and relatively low morbidities for SBLL patients with two-stage surgery [6]. In addition, we developed a nomogram with three risk factors that related to the one-stage surgery complications. The nomogram had reasonable prediction value and could be incorporated into surgical decision making for SBLL patients.
Complications after surgery were often the major concern for surgeons and patients. Our findings may reduce the concern for these complications. Similarly, some other study also reached the same conclusion. For example, Fu reported one-stage VATS surgery for 18 bilateral pulmonary nodules and all patients recovered well without major complications [7]. Tong and his colleagues studied 16 cases of their centre who received one-stage surgery in single-utility port VATS. Minor complications including air leakage, atrial fibrillation and poor healing of the surgical site occurred [8]. Yao also reported 29 one-stage VATS included lobar-lobar resections, lobar and sub-lobar resections, and sub-lobar-sub-lobar resections. Most of the patients had uneventful postoperative course except for one severe dyspnoea. There was no significant difference in complications and chest tube days between one-stage and two-stage patients at the same time [9]. However, there were some slight differences in the recommendations on the resection scope. For example, Kohno recommended at least one side sub-lobectomy for safe reasons after studying 19 one-stage bilateral surgery patients [10], which is in accordance with Yao’s paper. Another study directly compared one-stage bilateral VATS and unilateral resection. One-stage surgery showed similar post-operative complication incidence and hospital stays and achieved a safe postoperative recovery as long as wedge resection was performed on one side [11]. Table 4 summarises the peri-operative results of previous research [2, 4, 7, 12]. Overall, our study and previous investigations all favoured one-stage approach and suggested at least one sub-lobectomy in one-stage bilateral resection.
One-stage VATS was proved to be an equally safe procedure with two-stage VATS, though, it was still a major procedure with around 30% of post-operative complication rate. Although not life threatening in most cases, some complications would nevertheless bring extra sufferings for the patients. In order to select the best candidates for one-stage surgery, we developed a nomogram based on the multivariate logistic regression for the risk factors to predict those who may experience post-operative complications. Moreover, efforts must be made to reduce the risk for patients even they are predicted to be “low risk” candidates. Careful preoperative evaluation, meticulous operation, and advanced post-operative management all contribute to good recovery. We noticed that patients in one-stage group had significantly more hydrothorax (40%) than those in two-stage group (11.1%). The reason might be that the coughing movement was weakened as wound pain was sever in the one-stage bilateral surgery group. Enough analgesic should be prescribed to relief the postoperative pain.
In this study, both wedge resection (WR) and anatomical segmentectomy (AS) were categorized as sub-lobectomy (SL), as they are similar in the surgical trauma. It is generally recommended that lobectomy should be performed for large, progressing, and invasive lesions, while sub-lobectomy for the small, non-invasive ones. The choice of sub-lobectomy (AS or WR) was determined by the location, size, and consolidation/tumour ratio (CTR) of the lesion. If two-stage resection is planned, lobectomy is preferred in the first stage, and an interval of 3–4 months before the next surgery is recommended. Some researchers also claimed that in the one-stage surgery, wedge resection should be performed on at least one side to reduce the surgical trauma [11]. Meanwhile, for malignant lesions diagnosed before operation, systematic lymph node dissection should be considered as long as the patients could tolerate the surgery [13]. For patients who could not tolerate or refuse surgery, and those with multifocal malignant lesions which could not be resected radically, some investigators proposed that epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKI) treatment may be an alternative as long as the biopsy reported positive EGFR mutation [14].
Overall, one-stage VATS surgical treatment achieved favourable results for the SBLL patients, with acceptable postoperative complications. The nomogram would further help select patients with lower “risk”. However, our study is not without limitations. First, this was a retrospective study with inevitable selection bias. Future investigation in a larger cohort multicentre prospective study is required. Also, as an analysis focusing on the safety and feasibility of one-stage surgery, both benign and malignant lesion were included. As a consequence, long-term survival analysis for cancer patients was absent. In the cancer subset of the bilateral patients, it would be more powerful if prognostic results of 5-year overall survival and recurrence-free survival were presented to determine whether one- or two-stage bilateral surgery is appropriate. Last, the nomogram for the prediction of postoperative complications did not get a perfect predictive value. Large sample size is required to build a more powerful model.
Conclusion
One-stage VATS for synchronous bilateral lung lesion patients was proved to be a safety procedure. The risk and severity of postoperative complications in one-stage VATS were comparable to the two-stage VATS, but less surgical trauma and cost, thus one-stage VATS could be a possible choice for the treatment of synchronous bilateral lung lesion patients. Advanced age, pre-surgical low haemoglobin and blood loss may predict complications after surgery. Patients with those risk factors should be paid more attention postoperatively.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VATS:
-
Video assisted thoracic surgery
- SBLL:
-
Synchronous bilateral lung lesions
- PSM:
-
Propensity score matching
- LDCT:
-
Low dose computed tomography
- AUC:
-
Area under ROC curve
- ROC:
-
Receiver operating characteristics
- C-index:
-
Harrell Consistency Index
- NLR:
-
Neutrophils/lymphocyte ratio
- PLT:
-
Platelet
- HB:
-
Haemoglobin
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- WR:
-
Wedge resection
- AS:
-
Anatomical segmentectomy
- SL:
-
Sub-lobectomy
- CTR:
-
Consolidation/tumour ratio
- EGFR:
-
Epidermal growth factor receptor
- TKI:
-
Tyrosine kinase inhibitors
References
Bak SH, Lee HY, Kim JH, Um SW, Kwon OJ, Han J, et al. Quantitative CT scanning analysis of pure ground-glass opacity nodules predicts further CT scanning change. Chest. 2016;149(1):180–91.
Qu R, Hao Z, Zhang Y, Bie L, Fu X, Zhang N. Single-center experience of simultaneous bilateral uni-portal video-assisted thoracoscopic surgery for multiple ground-glass opacities. J Cardiothorac Surg. 2020;15(1):69.
Yang X, Wang L. Subxiphoid uniportal video-assisted thoracoscopic surgery for synchronous bilateral lung resection. Postgrad Med. 2018;130(1):142–5.
Zhang Y, Wang Y, Lv C, Shu X, Wang J, Yang Q. Clinical analysis of 56 cases of simultaneous bilateral video-assisted thoracoscopic surgery for bilateral synchronous multiple primary lung adenocarcinoma. J Thorac Dis. 2018;10(12):6452–7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Yang H, Sun Y, Yao F, Yu K, Gu H, Han B, et al. Surgical therapy for bilateral multiple primary lung cancer. Ann Thorac Surg. 2016;101(3):1145–52.
Xu G, Fu X. One-stage video-assisted thoracic surgery for bilateral multiple pulmonary nodules. J Thorac Dis. 2019;11(2):535–41.
Huang C, Sun Y, Wu Q, Ma C, Jiao P, Wang Y, et al. Simultaneous bilateral pulmonary resection via single-utility port VATS for multiple pulmonary nodules: a single-center experience of 16 cases. Thorac Cancer. 2021;12(4):525–33.
Yao F, Yang H, Zhao H. Single-stage bilateral pulmonary resections by video-assisted thoracic surgery for multiple small nodules. J Thorac Dis. 2016;8(3):469–75.
Mun M, Kohno T. Single-stage surgical treatment of synchronous bilateral multiple lung cancers. Ann Thorac Surg. 2007;83(3):1146–51.
Matsubara T, Toyokawa G, Kinoshita F, Haratake N, Kozuma Y, Akamine T, et al. Safety of simultaneous bilateral pulmonary resection for metastatic lung tumors. Anticancer Res. 2018;38(3):1715–9.
Fourdrain A, Bagan P, Georges O, Lafitte S, De Dominicis F, Meynier J, et al. Outcomes after contralateral anatomic surgical resection in multiple lung cancer. Thorac Cardiovasc Surg. 2021;69(4):373–9.
Han L, Gao S, Tan F, Zhao Z, Song P. Experience and progress processing policy of simultaneous multiple primary lung cancer. Zhongguo Fei Ai Za Zhi. 2018;21(3):180–4.
Cheng B, Deng H, Zhao Y, Zhu F, Liang H, Li C, et al. Management for residual ground-glass opacity lesions after resection of Main Tumor in Multifocal Lung Cancer: a Case Report and Literature Review. Cancer Manag Res. 2021;13:977–85.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
JL concepted, designed the study, and approved the manuscript. ZW collected, assembled, analysed and interpreted the data. XZ analysed the data. XS collected the data. All authors contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by ethics board of Hebei Medical University Fourth Hospital (No.: 2021KY318).
Consent for publication
Individual consent for this retrospective analysis was waived due to the retrospective nature.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Z., Zhang, X., Sun, X. et al. One-stage VATS surgery for synchronous bilateral lung lesion: a safe and feasible procedure. J Cardiothorac Surg 18, 126 (2023). https://doi.org/10.1186/s13019-023-02215-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02215-3