Abstract
Background
A displaced left B1 + 2 accompanied by an anomalous pulmonary vein is a rare condition involving complex structures. There is a risk of unexpected injuries to bronchi and blood vessels when patients with such anomalies undergo surgery for lung cancer.
Case presentation
A 59-year-old male with suspected lung cancer in the left lower lobe was scheduled to undergo surgery. Chest computed tomography revealed a displaced B1 + 2 and hyperlobulation between S1 + 2 and S3, while the interlobar fissure between S1 + 2 and S6 was completely fused. Three-dimensional computed tomography (3D-CT) revealed an anomalous V1 + 2 joining the left inferior pulmonary vein and a branch of the V1 + 2 running between S1 + 2 and S6. We performed left lower lobectomy via video-assisted thoracic surgery, while taking care with the abovementioned anatomical structures. The strategy employed in this operation was to preserve V1 + 2 and confirm the locations of B1 + 2 and B6 when dividing the fissure.
Conclusion
The aim of the surgical procedure performed in this case was to divide the fissure between S1 + 2 and the inferior lobe to reduce the risk of an unexpected bronchial injury. 3D-CT helps surgeons to understand the stereoscopic positional relationships among anatomical structures.
Similar content being viewed by others
Background
Due to the development and spread of imaging technology, thoracic surgeons are able to obtain a precise understanding of the anatomical structures of patients’ lungs before surgery [1]. Surgeons should plan surgical procedures using imaging modalities to avoid unexpected injuries to anatomical structures because the pulmonary anatomy exhibits numerous variations and anomalies. Herein, we report an exceedingly rare case involving a patient with a displaced B1 + 2 accompanied by an anomalous V1 + 2, which joined the left inferior pulmonary vein. We were able to safely perform left lower lobectomy using video-assisted thoracic surgery (VATS) after preoperatively identifying these complex anatomical structures.
Case presentation
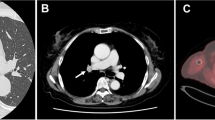
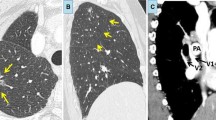
A 59-year-old male with no history of smoking exhibited a slightly increased carcinoembryonic antigen level (5.6 ng/mL) during a health check. Chest computed tomography (CT) revealed a tumor (maximum diameter: 13 mm) in the left lower pulmonary lobe (Fig. 1a). He was referred to our hospital with suspected left lower lobe lung cancer (cT1bN0M0 stage1A2). CT and three-dimensional CT (3D-CT), which was performed using the Fujifilm Synapse Vincent system (Fujifilm Corporation, Tokyo, Japan), revealed the following anatomical anomalies in the left lung: 1) a displaced B1 + 2 running behind the main pulmonary artery, 2) an anomalous V1 + 2 joining the left inferior pulmonary vein (Fig. 2b), and 3) hyperlobulation between S1 + 2 and S3 with a completely fused interlobar fissure between S1 + 2 and S6 (Fig. 1b and c). 3D-CT also indicated that the interlobar plane between S1 + 2 and S6 ran perpendicular to the cranio-caudal direction because the volume of S1 + 2 was relatively large (Fig. 2a). Bronchoscopy revealed that three bronchi branched from the left main bronchus (Fig. 1d).
Preoperative chest computed tomography images and bronchoscopic image. Chest computed tomography (CT) revealed a tumor in the left inferior lobe (a) and hyperlobulation between S1 + 2 and S3 (red arrow), while the interlobar fissure between S1 + 2 and S6 was completely fused (b). CT revealed a displaced B1 + 2 running behind the main pulmonary artery (c). Bronchoscopy revealed that three bronchi branched from the left main bronchus (d).
We planned VATS for surgical diagnosis and treatment. Hyperlobulation between S1 + 2 and S3 and a fused fissure between S1 + 2 and S6 were observed (Fig. 3a). At first, we performed non-anatomical wedge resection of the lesion to achieve a rapid pathological diagnosis. The patient was diagnosed with adenocarcinoma, and left lower lobectomy and systematic nodal dissection were performed.
Intraoperative findings. Hyperlobulation was seen between S1 + 2 and S3, and a largely fused fissure was observed between S1 + 2 and S6 (a). The inferior pulmonary vein (IPV) was identified on the posterior side of the mediastinal pleura (b). In the process of peeling away the proximal V1 + 2, we were able to clearly distinguish between B1 + 2 and B6 on the posterior side (c). The branch of V1 + 2 running between S1 + 2 and S6 was used as a landmark when dividing the fissure between S1 + 2 and the inferior lobe (d)
The major pitfalls that we had to pay attention to during this surgery were as follows: 1) to avoid injuring the displaced B1 + 2 running behind the main pulmonary artery and 2) to avoid cutting the anomalous V1 + 2.
The inferior pulmonary vein was identified on the posterior side of the hilum, and the anomalous V1 + 2 joined it (Fig. 3b). To prevent B1 + 2 from being mistaken for B6, we distinguished B1 + 2 from the distal section of B6 on the posterior side (Fig. 3c). The distal branch of A8 was identified using the interlobar fissure. After A8 was divided, we peeled away the pulmonary artery in the proximal direction to identify A6 and V1 + 2, which ran near A,6 and a branch of V1 + 2, which ran between S1 + 2 and S6 (Figs. 2b and 3d). This branch was used as a landmark when we divided the fissure between S1 + 2 and the inferior lobe. Forceps were passed from the anterior to posterior side between a branch of V1 + 2 and A,6 and the largely fused fissure between S1 + 2 and the inferior lobe was divided using a stapler. After dividing the fissure, A6 and A9 + 10 were identified and divided. The inferior bronchus branched from the left main bronchus at the level of the branches of B3 + B4 + 5 and the displaced B1 + 2, which was located at a more proximal site than normal; therefore, we needed to peel away the bronchus while holding down the pulmonary artery and identified the station 11 lymph nodes. Forceps were passed from the anterior to the posterior side along the station 11 lymph nodes, and the incomplete fissure between S5 and inferior lobe was divided using the stapler. After dividing the fissure, the inferior bronchus was divided, which completed the lobectomy ND2a-2 procedure.
The operation time was 185 min, and 30 mL intraoperative blood loss occurred. Pathologically, the tumor was diagnosed as an invasive mucinous adenocarcinoma with a maximal diameter of 15 mm, and the pathological stage was p-T1aN0M0 stage I A1. The patient’s postoperative course was uneventful, and he was discharged from hospital 6 days after the surgery.
Discussion and conclusion
In lung surgery, numerous variations in anatomical structures can be encountered, and they can cause serious complications if surgeons do not identify them preoperatively. Foster-Carter reported that bronchial anomalies are present in 0.64% of patients and classified them into displaced bronchi; i.e., bronchi that branch away from their normal positions, and supernumerary bronchi; i.e., excess bronchi that occur in addition to the normal bronchi [2]. Eighty percent of displaced bronchi occur in the right upper lobe, and 11% are displaced B1 + 2 arising from the left main bronchus [3]. In our case, a displaced left B1 + 2 accompanied by an anomalous V1 + 2 of the left pulmonary vein was seen, which is even rarer than the abovementioned variation. In addition, a case involving a displaced left B1 + 2, in which there were accessory fissures between the segment containing the displaced bronchus and an incomplete fissure between the upper lobe and lower lobe, was reported [4]. Thus, in the present case we needed to consider how we should create a fissure. Three surgical cases involving displaced B1 + 2, in which unexpected B1 + 2 injuries occurred when a region of lobulation between S1 + 2 and S6 was divided, even though two cases were recognized anomalies before surgery, have been reported (Table 1) [7,8,9]. The injuries were caused by the displaced B1 + 2 being misidentified as B6 when the fissure between S1 + 2 and the inferior lobe was divided using a stapler. Since excision of the upper lobe was scheduled in both cases, the injuries did not have adverse effects on the surgical procedures. However, unexpected injuries to the upper lobe can be serious complications during lower lobectomy. The aim of the surgical procedure performed in the present case was to divide the fissure between S1 + 2 and the lower lobe. It was necessary to take great care during this procedure because there was an anomalous V1 + 2 that passed from S1 + 2 to the inferior pulmonary vein in this case. In such cases, it is important to be aware not only of the existence of the anomaly, but also to understand the stereoscopic positional relationships between the pulmonary veins and bronchi. In the present case, 3D-CT revealed a displaced B1 + 2 arising from the left main bronchus and running along the left edge of the main pulmonary artery. In addition, an anomalous V1 + 2 was found to run between B1 + 2 and B6 and the dorsal side of the inferior bronchus. The branch of V1 + 2 running between S1 + 2 and S6 was used as a landmark when dividing the fissure between S1 + 2 and S6. By peeling away the distal part of V1 + 2 using a posterior approach, we were able to clearly identify B6, B1 + 2, and A.6 These anatomical findings matched the preoperative 3D-CT findings [1].
In this case, 3D-CT helped us to share information across the surgical team, which allowed the surgeons to become familiar with the patient’s rare anatomical structures. It is imperative for surgeons to acquire complete information about patients’ pulmonary anatomies before surgery, including a full understanding of any rare anomalies or complicated anatomies, before performing lobectomy.
In conclusion, during left lower lobectomy for patients with displaced B1 + 2, dividing the fissure between S1 + 2 and S6 carries a risk of injuring a bronchus. 3D-CT helped us to obtain information about the patient’s anatomy, leading to an optimal preoperative assessment and appropriate strategic planning.
Availability of data and materials
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- 3D-CT:
-
Three-dimensional computed tomography
- VATS:
-
Video-assisted thoracic surgery
References
Ikeda N, Yoshimura A, Hagiwara M, Akata S, Saji H. Three dimensional computed tomography lung modeling is useful in simulation and navigation of lung cancer surgery. Ann Thorac Cardiovasc Surg. 2013;19:1–5.
Foster-Carter AF. Broncho-pulmonary abnormalities. Br J Tuberc Dis Chest. 1946;40:111–24.
Yaginuma H. Investigation of displaced bronchi using multidetector computed tomography: associated abnormalities of lung lobulations, pulmonary arteries and veins. Gen Thorac Cardiovasc Surg. 2020;68:342–9.
Oshiro Y, Murayama S, Ohta M, Teruya T. CT findings of a displaced left upper division bronchus in adults: its importance for performing safe left pulmonary surgery. Eur J Radiol. 2013;82:1347–52.
Shimamoto A, Takao M, Kodama H, et al. A case of left apicoposterior segmentectomy for lung cancer occurring in a displaced anomalous bronchus. J Jpn Soc Respir Endoscopy. 2008;30:210–4 (in Japanese).
Tsukioka T, Yamamoto R, Takahama M, et al. A case of lung cancer arising from abnormal bronch. J Jpn Assoc Chest Surg. 2011;25:460–4 (in Japanese).
Osawa J, Ito H, Samejima J, Nagashima T, Nakayama H, Ikeda N. S1+2+6 segmentectomy for a case of lung cancer arising in a displaced anomalous bronchus. J Jpn Assoc Chest Surg. 2018;32:847–52 (in Japanese).
Asakura K, Imanishi N, Matsuoka T, Nagai S, Matsuoka K, Ueda M, et al. Video-assisted thoracic surgery lobectomy for lung cancer with displaced B1+2. Ann Thorac Cardiovasc Surg. 2014;20(Suppl):486–9.
Hayashi K, Motoishi M, Horimoto K, Sawai S, Hanaoka J. Left upper division segmentectomy with a simultaneous displaced bronchus and pulmonary arteriovenous anomalies: a case report. J Cardiothorac Surg. 2018;13:40.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SS performed the data collection and wrote the manuscript. SS and NK played major roles in the creation of the 3D-CT images. HT and AT supported the writing of the manuscript. All of the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient provided written informed consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sakamoto, S., Takizawa, H., Kawakita, N. et al. Lobectomy for lung cancer with a displaced left B1 + 2 and an anomalous pulmonary vein: a case report. J Cardiothorac Surg 16, 15 (2021). https://doi.org/10.1186/s13019-021-01392-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01392-3