Abstract
Background
Low back pain (LBP) is the leading cause of disability worldwide and a significant component of healthcare expenditures. Clinical practice guidelines (CPGs) have been highlighted as a key resource to improve the quality of care. This study aimed to develop a clinical pathway for LBP based on CPGs in an academic health system.
Methods
We conducted a modified Delphi study of clinicians caring for patients with LBP who were asked to rate 21 CPG-informed seed statements through an online survey. The goal was to identify statements that achieved a minimum of 80% consensus among panelists.
Results
Thirty-five healthcare providers participated as panelists. The majority of participants were male (68.6%), had MD or DO (62.9%) degrees, and were clinicians (73.8%) working in neurosurgery (36.1%), orthopedics (25.7%), emergency medicine (14.3%), or physical therapy (11.4%). Initially, consensus was reached on 20 of 21 seed statements. One statement did not reach consensus in the initial round and was revised into two separate statements based on feedback from panelists. One of these statements achieved consensus in the second review round. All statements reaching consensus were incorporated into a care pathway consisting of diagnosis, evaluation, and treatment for LBP.
Conclusion
Healthcare providers across various disciplines supported statements interpreting current CPGs related to care for LBP. This study represents a step toward supporting guideline-concordant care for LBP. Additional research is needed to assess how such pathways impact actual clinical care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Low back pain (LBP) is the leading cause of disability worldwide and a major component of healthcare expenditures [1, 2]. In the USA, more is spent on low back and neck pain ($134.6 billion in 2016) than any other condition [3]. Clinical practice guidelines (CPGs) have been highlighted as a key resource to help inform clinicians and health organizations about current evidence and improve the quality of care [4,5,6].
The existence of CPGs, however, does not ensure evidence-based care is routinely delivered. Clinicians may be unfamiliar with current CPGs, and some recommendations may conflict with clinical training or experience [7]. Clinicians may lack trust in CPGs due to insufficient transparency in reporting methods and concerns about quality [8,9,10]. Health organization characteristics and processes can also positively or negatively influence the extent to which CPGs are followed [11, 12].
CPGs are informed by subject matter experts and careful review of current scientific evidence, typically resulting in formal recommendations for clinical decision-making and care delivery [13]. Current CPG recommendations differ from traditional management approaches for LBP. For example, The American College of Physicians (ACP) recommends non-pharmacological care as the first option for people with LBP [14]. Several non-pharmacological therapies, such as exercise and various manual therapies, demonstrate similar benefits to pharmacological therapies with comparatively less risk [15,16,17,18,19,20,21,22,23] and lower healthcare costs [4,5,6].
Unfortunately, there is little evidence that CPG-recommended care for LBP is prevalent across health systems [24, 25]. Some evidence suggests treatments of unknown value and other high-cost, low-value care for LBP are increasing [26, 27]. Health organizations and providers play a vital role in guideline-concordant care. Therefore, providers caring for patients with LBP are essential stakeholders who offer key insight into applying clinical guidelines to clinical decision-making, diagnosis, treatment decisions, and referral pathways. Academic health centers, consistent with other health systems [28, 29], are determined to facilitate guideline-concordant care by creating care pathways aligned with guideline recommendations for LBP. This study aimed to develop an evidence-based care pathway for LBP for use in an academic health center and validated by a multidisciplinary panel of provider stakeholders.
Methods
We used a three-step process to accomplish study objectives. First, we worked with a librarian to conduct bibliographic searches in MEDLINE, EMBASE, CINAHL. The search strategy focused on LBP CPGs, systematic reviews focused on evidence-based care for LBP, and clinical trials published after the most recent systematic reviews. Authors (GB, DPD, and CG) independently conducted title/abstract and full text screening to identify relevant studies. The authors independently abstracted study characteristics and key findings from systematic reviews and clinical trials or recommendations for CPGs. We used these data, with an emphasis on CPG recommendations, to develop the seed statements. Second, we developed seed statements as individual components of a care pathway designed to support and facilitate the clinical application of evidence-based care for LBP. Seed statements were designed to address consistency in care delivery regardless of health profession and whether the patient presented with acute or chronic low back pain. Third, we recruited a multidisciplinary panel of Duke University Hospital System providers who care for patients with LBP (e.g., primary care, physical therapy, physiatrists, orthopedic surgery, chiropractic) to review and validate seed statements using modified Delphi methodology. This study was reviewed and found exempt by the Duke University Health System Institutional Review Board (IRB protocol number: Pro00109618).
Source document and seed statements
One investigator (RV), an experienced clinician, educator, and clinical researcher, initially developed seed statements. Other investigators (GB, DPD, CG, HG, JM) refined statements through an iterative process and facilitated statement formatting for Delphi panel review (GB, DPD). Topic areas included LBP assessment, referral pathways, and general clinical management. The investigative team then further reviewed, refined, and organized draft statements into thematic headings. Twenty-one statements were distributed to Delphi panelists for the initial review round.
Modified Delphi consensus process
Consensus was conducted using a modification of the RAND Corporation/University of California, Los Angeles methodology on appropriateness ratings [30]. Data were collected electronically using Qualtrics (v. 2020; Qualtrics, Provo, UT). Panelists were invited if they were providers with the Duke University Health System who commonly treat LBP and in the following disciplines: orthopedic and neurosurgery, primary care, physiatry, osteopathic medicine, physical therapy, nurse practitioner, physician assistant, and chiropractic. Panelists from these disciplines represented the majority of provider types who cared for people with LBP within the Duke University Health System and for whom the clinical care pathway for LBP was most applicable. A Qualtrics link containing an overview of the project, the purpose of recommendations included in seed statements, instructions on participating in the Delphi panel, participants’ expectations, and approximate time required to participate were sent to 44 potential participants via E-mail. Interested participants signed an electronic consent form before initiating the survey.
Demographic characteristics collected from panelists included profession, age, employment duration at Duke, race, and ethnicity. Panelists individually rated the content of each seed statement using the following ordinal scale: 1–3 “highly inappropriate,” 4–6 “undecided,” or 7–9 “highly appropriate.” Each seed statement contained text fields to provide an opportunity to comment on any statement rated below 7. Each statement also included embedded references supporting the statements, with electronic links to PubMed abstracts.
After the panelist review, two investigators (GB and DPD) entered the de-identified numerical ratings and panelist comments into Microsoft Excel. Consensus was defined as a minimum of 80% of participants rating a single seed statement as “highly appropriate” (a rating of 7–9). Statements not reaching consensus were revised and reassessed by panelists until consensus was obtained or the statement was removed. The consensus process took place between March and October 2022. The first round of seed statement review began in March 2022, lasting four weeks. The second round started in October 2022, lasting two weeks and consisting only of revised statements that did not reach consensus during the first review round.
Result
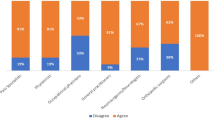
Thirty-five panelists rated seed statements. Demographic characteristics are reported in Table 1. Participants were predominantly male (n = 24, 68.6%) with a mean (SD) age of 44.8 (14.5). Members of several disciplines participated in the Delphi panel. The most commonly reported degrees were medicine (MD) or Osteopathic medicine (DO) (n = 22, 62.9%). The majority of participants identified as physicians/clinicians (n = 31, 73.8%) working in several different areas such as neurosurgery (n = 13, 36.1%), orthopedics (n = 9, 25.7%), emergency medicine (n = 5, 14.3%) and physical therapy (n = 4, 11.4%). The largest single group of participants were employed at Duke for 4 to 10 years (n = 16, 48.5%) and in their professions for over ten years (n = 15, 44.1%). After the first review round, 20 of 21 statements met the a-priori definition of consensus. The statement failing to reach a consensus was then revised into two separate statements based on panelist feedback. Eleven participants responded to the follow-up survey (31.4% response rate).
Twenty-one seed statements comprised topics relevant to evidence-based clinical management of LBP, including processes associated with diagnosis, diagnostic imaging, treatment approaches for initial and specific presentations, and referral pathways. Seed statements and panelist ratings are reported in Table 2. The single statement that did not reach consensus during the initial review was: “Secondary pharmacological management should include Tramadol or Duloxetine.” Panelist comments included an unwillingness to prescribe Tramadol, preferring non-opiate muscle relaxants, and a lack of conclusive evidence supporting duloxetine as a safe and effective therapy with a low risk for dependence.
Panelist comments suggested low ratings related to a single statement addressing two medications with different classifications, Tramadol and Duloxetine. Therefore, the statement was revised into two statements for a second review. In the second round, consensus was reached on one revised statement and failed to reach consensus on one revised statement (Table 3). The statement failing to reach consensus was “Secondary pharmacological management may consist of Duloxetine, when tolerated and in the absence of contraindication(s).” Although the statement was consistent with ACP guidelines, panelists did not reach a consensus on appropriateness due to remaining questions about Duloxetine’s efficacy (e.g., whether it functions primarily as a pain or antidepressant agent, concerns for dependency, and lack of experience with prescribing). Therefore, the statement was removed from the final care pathway.
Seed statements reaching consensus were used to develop the final care pathway (Fig. 1). The pathway describes general management processes beginning with a patient presenting with LBP. The first significant clinical management process indicated is an evaluation for red flags that suggest urgent referral to the emergency department or a surgeon for appropriate imaging and treatment. If patients do not present with red flags, they should be referred to a primary spine practitioner (PT or DC) for a clinical examination consisting of patient history, physical, and psychosocial examination. After clinical examination, treatment should consist of non-pharmacological care unless there is evidence of serious pathology, or severe radiculopathy (e.g., identified by reduced/absent nerve root signaling) is present. When a trial of non-pharmacological care is ineffective, referral for pharmacological treatment should be considered, followed by referral for evaluation by pain management specialist when there is a limited/no response. Finally, referral and consult with a spine surgeon is appropriate to determine if evidence-based criteria for surgical intervention are met in cases when there is a limited/no response to care.
Discussion
While prior LBP care pathways have been developed within academic health centers in Europe, to our knowledge, this is the first Delphi consensus process conducted to develop a LBP care management pathway using a multidisciplinary panel of providers with experience caring for patients within a US academic health system [31, 32]. Our findings are consistent with existing CPGs, [14, 33, 34] suggesting that the core components of the care pathway developed in this study may have broader applicability for other healthcare settings.
Participants arrived at consensus for 21 seed statements across two rounds, while one statement regarding the use of Tramadol and Duloxetine required three rounds to achieve consensus. Consistent with our findings that clinicians were less likely to agree with CPG recommendations regarding use of these two medications, there is considerable uncertainty regarding optimal pharmacological therapy for LBP [35]. Such uncertainty highlights the need for additional high-quality randomized controlled trials of pharmacological therapies for LBP to better inform CPGs and their resultant care pathways.
Core to the care pathway developed under this initiative is an acknowledgment that members of different health professions can appropriately conduct diagnostic evaluations for LBP. In summary, regardless of discipline, clinical evaluation should include a detailed history, red flag screening, and psychosocial screening. Consistent with CPGs from the American College of Radiology, initial evaluation of LBP typically should not include imaging unless red flags suggest serious underlying pathology [36]. Following diagnostic evaluation, first-line care is initiated by primary spine practitioners offering nonpharmacological care, with psychological co-management when indicated [37, 38]. When patients do not respond favorably, pharmacological therapy is considered, followed by interventional pain management, and finally, surgical evaluation if appropriate criteria are met.
Though evidence-based care pathways may be applicable in a given setting, improved outcomes do not necessarily follow. Three recent clinical trials compared risk-stratified care using the STarT Back tool with usual care for participants with LBP [39,40,41]. Each trial reported similar outcomes for both groups, suggesting referral pathways informed by risk stratification added no clinical benefit. However, two studies showed limited fidelity in implementing risk-stratified care. We attempted to address issues of implementation by working with an interdisciplinary team to conceptualize this project and using the Delphi process to incorporate input from clinicians across the broad range of disciplines for which the care pathway was intended. These methods leveraged the practical knowledge of providers, theoretically facilitating acceptance and laying a foundation for successful implementation.
The next logical step in this line of research is to assess the feasibility of implementation and, subsequently, the clinical effectiveness of pathway-driven care for low back pain. Consistent with this line of research, the academic health systems of Duke University, Dartmouth College, and the University of Iowa have recently begun recruiting participants for an NIH-funded pragmatic clinical trial designed to evaluate outcomes associated with asking patients to consider seeing a physical therapist or doctor of chiropractic before seeking care from a primary care physician [42].
This study has several important strengths. For example, seed statements were informed by current evidence, notably CPGs relevant to management for LBP. Further, we recruited experienced providers across disciplines (e.g., Medicine, Osteopathic Medicine, Physician Assistant, Physical Therapy, and Chiropractic) and care settings (e.g., emergency, orthopedics, neurosurgery, physical medicine and rehabilitation, and primary care), allowing for a broad perspective on best practices for clinical care. We also acknowledge several important limitations. We did not include professionals from every conceivable clinical discipline that may engage patients with LBP (e.g., pain psychologists). In addition, panelists in our study were all employed at one academic medical center, which could limit the extrapolation of findings to other settings. Finally, studies of this type are always limited by those who did and did not participate.
Conclusion
Healthcare providers across various disciplines within a large academic health center supported statements interpreting current clinical practice guidelines for low back pain care. This study represents a step toward supporting and coordinating guideline-concordant care among multiple health disciplines. Additional research is needed to assess how the care pathway developed in this study influences clinical management and outcomes. Fortunately, such investigation is already being initiated through the NIH Collaboratory.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ACP:
-
American College of Physicians
- CPGs:
-
Clinical practice guidelines
- LBP:
-
Low back pain
References
Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain—where to from here? Am J Public Health. 2019;109(1):35–40.
GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Lond Engl. 2017;390(10100):1260–344.
Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, et al. US Health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84.
Fritz JM, Cleland JA, Brennan GP. Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Med Care. 2007;45(10):973–80.
Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J, Oostendorp RA. Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther. 2010;90(8):1111–22.
Childs JD, Fritz JM, Wu SS, Flynn TW, Wainner RS, Robertson EK, et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res. 2015;15(1):150.
Baiardini I, Braido F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol. 2009;9(3):228–33.
Scott IA, Guyatt GH. Clinical practice guidelines: the need for greater transparency in formulating recommendations. Med J Aust. 2011;195(1):29–33.
Lin I, Wiles LK, Waller R, Goucke R, Nagree Y, Gibberd M, et al. Poor overall quality of clinical practice guidelines for musculoskeletal pain: a systematic review. Br J Sports Med. 2018;52(5):337–43.
Bejarano G, Csiernik B, Zadro JR, Ferreira GE. Analysis of comparator quality in trials included in the National Institute of Clinical Excellence (NICE) low back pain clinical practice guideline. Braz J Phys Ther. 2023;14: 100563.
Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83(4):691–729.
Ayanian JZ, Markel H. Donabedian’s lasting framework for health care quality. N Engl J Med. 2016;375(3):205–7.
Gurgel RK. Updating clinical practice guidelines: how do we stay current? Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2015;153(4):488–90.
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Clinical guidelines committee of the American college of physicians noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2017;166(7):514–30.
Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD009790.pub2/full.
Rubinstein SM, de Zoete A, van Middelkoop M, Assendelft WJJ, de Boer MR, van Tulder MW. Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: systematic review and meta-analysis of randomised controlled trials. BMJ. 2019;13(364): l689.
Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatol Oxf Engl. 2010;49(12):2346–56.
Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368–83.
Migliorini F, Maffulli N. Choosing the appropriate pharmacotherapy for nonspecific chronic low back pain. J Orthop Surg. 2022;17(1):556.
Baroncini A, Maffulli N, Eschweiler J, Molsberger F, Klimuch A, Migliorini F. Acupuncture in chronic aspecific low back pain: a Bayesian network meta-analysis. J Orthop Surg. 2022;17(1):319.
Migliorini F, Maffulli N, Eschweiler J, Tingart M, Baroncini A. Non-steroidal anti-inflammatory drugs and gabapentinoids for chronic lumbar pain: a Bayesian network meta-analysis of randomized controlled trials. Br Med Bull. 2021;138(1):85–95.
Migliorini F, Maffulli N, Eschweiler J, Betsch M, Catalano G, Driessen A, et al. The pharmacological management of chronic lower back pain. Expert Opin Pharmacother. 2021;22(1):109–19.
Baroncini A, Maffulli N, Al-Zyoud H, Bell A, Sevic A, Migliorini F. Nonopioid pharmacological management of acute low back pain: A level I of evidence systematic review. J Orthop Res Off Publ Orthop Res Soc. 2023;41(8):1781–91.
Zadro J, O’Keeffe M, Maher C. Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open. 2019;9(10): e032329.
Goertz CM, Long CR, English C, Meeker WC, Marchiori DM. Patient-reported physician treatment recommendations and compliance among US adults with low back pain. J Altern Complement Med N Y N. 2021;27(S1):S99-105.
Zadro JR, Ferreira G. Has physical therapists’ management of musculoskeletal conditions improved over time? Braz J Phys Ther. 2020;24(5):458–62.
Radomski TR, Zhao X, Lovelace EZ, Sileanu FE, Rose L, Schwartz AL, et al. Use and cost of low-value health services delivered or paid for by the veterans health administration. JAMA Intern Med. 2022;182(8):832–9.
Ding Y, Liu C. Alternative payment models and physician treatment decisions: evidence from lower back pain. J Health Econ. 2021;80: 102548.
Lisi AJ, Salsbury SA, Hawk C, Vining RD, Wallace RB, Branson R, et al. Chiropractic integrated care pathway for low back pain in veterans: results of a delphi consensus process. J Manipulative Physiol Ther. 2018;41(2):137–48.
Fitch K, editor. The Rand/UCLA appropriateness method user’s manual. Santa Monica: Rand; 2001. 109 p.
Bailly F, Trouvin AP, Bercier S, Dadoun S, Deneuville JP, Faguer R, et al. Clinical guidelines and care pathway for management of low back pain with or without radicular pain. Joint Bone Spine. 2021;88(6): 105227.
Lee J, Gupta S, Price C, Baranowski AP. Low back and radicular pain: a pathway for care developed by the British Pain Society. Br J Anaesth. 2013;111(1):112–20.
National Guideline Centre (UK). Low Back Pain and Sciatica in Over 16s: Assessment and Management [Internet]. London: National Institute for Health and Care Excellence (UK); 2016 [cited 2021 Jun 11]. (National Institute for Health and Care Excellence: Clinical Guidelines). Available from: http://www.ncbi.nlm.nih.gov/books/NBK401577/
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86.
Wewege MA, Bagg MK, Jones MD, Ferraro MC, Cashin AG, Rizzo RR, et al. Comparative effectiveness and safety of analgesic medicines for adults with acute non-specific low back pain: systematic review and network meta-analysis. BMJ. 2023;22(380): e072962.
Expert Panel on Neurological Imaging, Hutchins TA, Peckham M, Shah LM, Parsons MS, Agarwal V, et al. ACR Appropriateness Criteria® Low Back Pain: 2021 Update. J Am Coll Radiol JACR. 2021;11S:S361–79.
Murphy DR, Justice B, Bise CG, Timko M, Stevans JM, Schneider MJ. The primary spine practitioner as a new role in healthcare systems in North America. Chiropr Man Ther. 2022;9(30):6.
Goertz CM, Weeks WB, Justice B, Haldeman S. A proposal to improve health-care value in spine care delivery: the primary spine practitioner. Spine J Off J North Am Spine Soc. 2017;17(10):1570–4.
Rhon DI, Greenlee TA, Poehlein E, Beneciuk JM, Green CL, Hando BR, et al. Effect of risk-stratified care on disability among adults with low back pain treated in the military health system: a randomized clinical trial. JAMA Netw Open. 2023;6(7): e2321929.
Delitto A, Patterson CG, Stevans JM, Freburger JK, Khoja SS, Schneider MJ, et al. Stratified care to prevent chronic low back pain in high-risk patients: The TARGET trial. A multi-site pragmatic cluster randomized trial. eClinicalMedicine [Internet]. 2021 Apr 1 [cited 2023 Jul 9];34. Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00075-4/fulltext
Cherkin D, Balderson B, Wellman R, Hsu C, Sherman KJ, Evers SC, et al. Effect of low back pain risk-stratification strategy on patient outcomes and care processes: the MATCH randomized trial in primary care. J Gen Intern Med. 2018;33(8):1324–36.
UG3 Project: Implementation of the American College of Physicians Guideline for Low Back Pain (IMPACt-LBP) [Internet]. Rethinking Clinical Trials. [cited 2023 Apr 12]. Available from: https://rethinkingclinicaltrials.org/demonstration-projects/impact-lbp/
Acknowledgments
The authors want to acknowledge Wren Burton's contributions to the initial care pathway draft.
Funding
There was no funding provided for this project. The authors have no relevant funding to disclose.
Author information
Authors and Affiliations
Contributions
CG had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GB, RV, DPD, JM, HMG, and CG contributed to concept and design. GB, RV, DPD, JM, HMG, and CG were involved in acquisition, analysis, or interpretation of data. GB, DPD, and CG contributed to drafting of the manuscript. GB, RV, DPD, JM, HMG, and CG were involved in critical manuscript revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and found exempt by the Duke University Health System Institutional Review Board (IRB protocol number: Pro00109618). All participants consented to participate.
Consent for publication
The co-authors and institutions have consented to publication.
Competing interests
The authors declare no competing interests.
Data statement
The authors will provide the data for this study under reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bejarano, G., Vining, R., Desai, D.P. et al. Development of a low back pain care pathway in an academic hospital system: results of a consensus process. J Orthop Surg Res 19, 11 (2024). https://doi.org/10.1186/s13018-023-04492-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04492-z