Abstract
Purpose
The clinical outcomes of using a zero-profile for anterior cervical decompression and fusion were evaluated by comparison with anterior cervical plates.
Methods
All of the comparative studies published in the PubMed, Cochrane Library, Medline, Web of Science, EBSOChost, and EMBASE databases as of 1 October 2021 were included. All outcomes were analysed using Review Manager 5.4.
Results
Seven randomized controlled studies were included with a total of 528 patients, and all studies were randomized controlled studies. The meta-analysis outcomes indicated that the use of zero-profile fixation for anterior cervical decompression and fusion was better than anterior cervical plate fixation regarding the incidence of postoperative dysphagia (P < 0.05), adjacent-level ossification (P < 0.05), and operational time (P < 0.05). However, there were no statistically significant differences in intraoperative blood loss, Visual Analogue Scale, Neck Disability Index, or Japanese Orthopaedic Association scale (all P > 0.05) between the zero-profile and anterior cervical plate groups.
Conclusions
The systematic review and meta-analysis indicated that zero-profile and anterior cervical plates could result in good postoperative outcomes in anterior cervical decompression and fusion. No significant differences were found in intraoperative blood loss, Visual Analogue Scale, Neck Disability Index, or Japanese Orthopaedic Association scale. However, the zero-profile is superior to the anterior cervical plate in the following measures: incidence of postoperative dysphagia, adjacent-level ossification, and operational time.
PROSPERO registration CRD42021278214.
Similar content being viewed by others
Introduction
Cervical degenerative disc disease (CDDD) is a common spine disease, and patients with severe symptoms usually require surgical intervention [1]. The anterior cervical decompression and fusion (ACDF) was first described by Smith and Robinson [2] in 1958. The procedure has become the gold-standard operation for CDDD treatment. Traditional ACDF procedures can restore the height of the intervertebral disc and avoid the migration of the implant by applying the anterior cervical plate (ACP) [3]. However, ACDF-related complications such as postoperative dysphagia, adjacent-level degeneration, and soft tissue injury are not rare [4, 5]. In addition, sometimes, it seems to be related to the ACP. Thus, a new stand-alone cervical anterior interbody fusion device, Zero-profile (Zero-p), was designed and developed [6]. Zero-p has a lower profile than an ACP. This type of device can reduce the compression of prevertebral soft tissue and has similar stability and clinical efficacy as ACP. A few meta-analyses have demonstrated that Zero-p in ACDF can produce better or similar outcomes than ACP in ACDF [7,8,9]. However, all previously published meta-analysis studies had significant limitations, including the absence of randomized controlled studies (RCTs). There is still insufficient level-one evidence to prove the proposed advantages of Zero-p in ACDF. Therefore, we reviewed previous RCTs and conducted this meta-analysis to compare outcomes between Zero-p implants and ACP interbody fusion systems for ACDF.
Methods
Literature search strategy
We performed systematic literature searches in six electronic databases, including PubMed, Cochrane Library, Medline, Web of Science, EBSOChost, and EMBASE. We searched using the following combination of MeSH (Medical Subject Heading) terms and free text words: “Zero-profile”, “Zero-p”, “cage and plate”, “anterior cervical disectomy and fusion” and “ACDF”. The search date was from when databases were built to 1 October 2021. We did not restrict searches based on language or publication year. To prevent certain studies from being missed, we manually searched the bibliographies of RCTs, meta-analyses, and systematic reviews.
Selection of studies
The study inclusion and exclusion processes were divided into two groups. The selection was first based on the title and abstract, and if a decision could not be made from the summary, the full text was retrieved. When there was a disagreement between the two groups, the selection committee was discussed until a consensus was reached.
Inclusion and exclusion criteria
We included studies that met the following criteria: (1). Included studies were RCTs. (2). A comparative study on the efficacy of Zero-p and ACP in ACDF. (3). The comparison outcomes included at least one of the following: surgical time, intraoperative blood loss, Visual Analogue Scale (VAS), Neck Disability Index (NDI), Japanese Orthopaedic Association (JOA) scale, postoperative dysphagia, and adjacent-level ossification. Studies were excluded according to the following criteria: (1). Editorials, letters, reviews, case reports, and cadaver or animal experiments. (2). The patient was diagnosed with scoliosis, infection or tumour (3). Studies that did not meet the inclusion criteria. (4). The data of the comparison outcomes could not be extracted.
Data extraction
Two reviewers used standardized data extraction tables. The extracted data included authors, publication date, title, country, study design, follow-up duration, number of patients, mean age of patients, type of operation, and comparison outcomes. The comparison outcomes included surgical time, intraoperative blood loss, VAS, NDI, JOA scale, postoperative dysphagia, and adjacent-level ossification. All data were extracted from article texts, tables, and figures. The research author was contacted for missing data or further information. Two reviewers independently extracted the data; differences were resolved through discussion, and a consensus was reached by including third parties. The data extraction outcomes are shown in Table 1.
Data analysis
We used Review Manager Version 5.4 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration) to analyse the data of all outcomes and compare the Zero-p group with the ACP group. For continuous outcomes, such as operating time, intraoperative blood loss, VAS, NDI, and JOA, the means and standard deviations were pooled to a weighted mean difference (WMD) and 95% confidence interval (CI). Risk ratios (RRs) and 95% CIs were used to evaluate dichotomous outcomes, such as postoperative dysphagia and adjacent segment ossification. We used I2 to quantify heterogeneity. If I2 > 50%, the heterogeneity was significant, and the unstandardized mean difference was estimated using a random effects model. Otherwise, a fixed effects model was applied.
Quality assessment
For RCTs, the Cochrane Handbook for Systematic Reviews of Interventions was used [10], including seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias (Fig. 2). Two reviewers independently carried out the quality assessment and discussed disagreements with a third party.
Results
Literature search
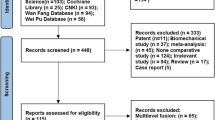
There were 9662 studies identified from five electronic databases (Fig. 1). Of those, 4639 studies were duplicates, and 4971 studies were excluded after title and abstract screening. After careful full-text evaluation, seven studies [11,12,13,14,15,16,17] were reviewed, and the data were extracted. The demographic and clinical characteristics of the seven studies are described in Table 1. A total of 267 patients who underwent Zero-p were compared with 261 patients who underwent ACP. The mean follow-up time was more than 6 months, and the mean age of the patients was 40–56 years old. Operating times were reported for four studies [13, 15,16,17]. Intraoperative blood loss was reported for three studies [12, 15, 16]. VAS was reported in three studies [14, 16, 17]. NDI and JOA scores were reported in three studies [11, 14, 17]. Postoperative dysphagia and adjacent segment ossification were reported in six studies [11,12,13,14,15, 17] and three studies [11, 12, 16], respectively (Fig. 2).
Intraoperative blood loss
Three studies [12, 15, 16] with 107 and 106 patients compared the mean intraoperative blood loss between the Zero-p and ACP groups. The meta-analysis indicated no significant differences between the Zero-p and ACP groups (WMD, − 7.71; 95% CI, − 17.03 to 1.61; P > 0.05). The heterogeneity test outcome (I2 = 81%) indicated significant heterogeneity (Fig. 3).
Operating time
Four studies [13, 15,16,17] with 185 and 183 patients compared the mean operating time between the Zero-p and ACP groups. We divided the operation time > 100 min and < 100 min into two subgroups for meta-analysis. In the > 100 min subgroup, the Zero-p group had significantly fewer operating times than the ACP group (WMD, − 10.69; 95% CI, − 16.10 to − 5.27; P < 0.05). In the < 100 min subgroup, the Zero-p group had significantly fewer operating times than the ACP group (WMD, − 18.83; 95% CI, − 23.64 to − 14.02; P < 0.05). The pooled outcomes showed that the Zero-p group had significantly fewer operating times than the ACP group (WMD, − 15.24; 95% CI, − 18.84 to − 11.65; P < 0.05). The heterogeneity test outcome (I2 = 45%) and the fixed effects model were applied. The results showed that the use of Zero-p in ACDF can significantly reduce the operating time compared with ACP (Fig. 4).
VAS
Three studies [14, 16, 17] with 94 and 91 patients, respectively, compared the mean VAS between the Zero-p and ACP groups. The meta-analysis indicated no significant differences between the Zero-p and ACP groups (WMD, − 1.82; 95% CI, − 4.12 to 0.48; P > 0.05). The heterogeneity test outcome (I2 = 98%) demonstrated significant heterogeneity. (Fig. 5).
NDI and JOA scores
Three studies [11, 14, 17] with 108 and 103 patients, respectively, compared mean NDI scores between the Zero-p and ACP groups. The meta-analysis concluded no significant differences between the Zero-p and ACP groups (WMD, − 9.45; 95% CI, − 20.9 to − 2.01; P > 0.05). The heterogeneity test outcome (I2 = 79%) has significant heterogeneity (Fig. 6).
Three studies [11, 14, 17] with 108 and 103 patients, respectively, compared mean JOA scores between the Zero-p and ACP groups. The meta-analysis indicated no significant differences between the Zero-p and ACP groups (WMD, 3.23; 95% CI, − 0.91 to 7.36; P > 0.05). The heterogeneity test outcome (I2 = 94%) indicated significant heterogeneity (Fig. 7).
Postoperative dysphagia
Six studies [11,12,13,14,15, 17] with 243 and 239 patients, respectively, compared the incidence of postoperative dysphagia between the Zero-p and ACP groups. The pooled outcomes indicated that the Zero-p group had a significantly lower incidence of postoperative dysphagia than the ACP group (RR, 0.56; 95% CI, 0.36 to 0.86; P < 0.05). The heterogeneity test outcome was I2 = 0, and the fixed effects model was applied (Fig. 8).
Adjacent-level ossification
Three studies [11, 12, 16] with 85 and 80 patients, respectively, compared the incidence of adjacent-level ossification between the Zero-p and ACP groups. The pooled outcomes noted that the Zero-p group had a significantly lower incidence of adjacent-level ossification than the ACP group (RR, 0.16; 95% CI, 0.06 to 0.42; P < 0.05). The heterogeneity test outcome was I2 = 0, and the fixed effects model was applied (Fig. 9).
Discussion
ACDF is a widely accepted surgical method for degenerative cervical spine diseases treatment [18]. This procedure can decompress the spinal cord, affect nerve roots and improve the stability of the cervical spine. During ACDF, an ACP is usually applied to enhance cervical stability, increase the interbody fusion rate and prevent graft dislocation or subsidence [19]. However, some postoperative complications seem to be related to ACP, such as oesophageal soft tissue damage, neurovascular injuries, and dysphagia [20]. The zero-profile implant is an independent anchoring spacer designed to minimize these complications, avoiding contact between the implant and the anterior soft tissue while providing the spine a stable biomechanical environment [21]. Several relevant studies comparing Zero-p and ACP in ACDF for degenerative cervical spondylosis patients have been reported. However, there is still a debate about whether Zero-p is better than ACP.
In our meta-analysis, the information of 528 patients was extracted from seven published RCTs using the Cochrane Handbook for Systematic Reviews of Interventions for quality assessment. The outcomes indicated that the included literature was of high quality. Our study demonstrated that the operation time, the incidence of postoperative dysphagia, and adjacent segment ossification of Zero-p in ACDF were significantly lower than those of ACP fixation. For intraoperative blood loss, VAS and NDI scores, and JOA scores, the meta-analysis outcomes have no significant differences between the Zero-p group and the ACP group.
Regarding the operating time, Chang et al. [22] reported that the operation time of Zero-p in ACDF is shorter than that of ACP fixation. Lan et al. indicated that there was no significant difference in terms of operation time between Zero-p and ACP [23]. We showed that the use of Zero-p can significantly reduce the operating time compared with ACP fixation, which is likely due to Zero-p saving time to harvest the autologous iliac graft. Moreover, since there is no steel plate, there is no need to polish the bone spurs on the anterior edge of the vertebral body, which reduces the operation time. Because Zero-p has no steel plate, there is no need to polish the bone spurs on the anterior vertebral body, thus reducing the operation time. Nemoto et al. [16] reported that Zero-p has a one-step locking mechanism with the simple insertion of the cage and tightening the screws, thus shortening the operation time.
Postoperative dysphagia is one of the most common complications after ACDF. Although we currently do not know the mechanism of dysphagia after ACDF, some hypotheses have been proposed. Lee et al. [24] noted a positive correlation between plate thickness and postoperative dysphagia rate. Joaquim et al. [25] showed that the causes of dysphagia after ACDF include postoperative soft tissue oedema, oesophageal injury, postoperative haematoma, and surrounding soft tissue adhesions. The Zero-p device can be inserted into the intervertebral space to avoid direct stimulation of the oesophagus and reduce oesophageal adhesions. Yang et al. noticed that the incidence and severity of dysphagia in the Zero-p group were lower than those in the ACP group [26]. Miao et al. [27] also obtained a similar outcome. Shao et al. meta-analysis [28] concluded that the Zero-p group was associated with a lower incidence of dysphagia at postoperative 1, 3, and 6 months and at the final follow-up than the ACP group. The meta-analysis of Sun et al. [29] also indicated that the incidence and severity of dysphagia in the Zero-p group were lower than those in the ACP group. However, most of the studies selected in their meta-analysis were not RCTs. In our meta-analysis, six randomized controlled studies reported dysphagia after the procedure. The results indicated that the Zero-p group had a significantly lower incidence of postoperative dysphagia than the ACP group (P < 0.05).
Another common complication of ACDF is adjacent-level ossification. Park et al. [30] indicated a positive association between adjacent-level ossification following anterior cervical plate procedures and the plate-to-disc distance. Huang et al. [31] also indicated that anterior plates with ACDF were associated with adjacent-level ossification. They reported that plate-to-disc distance < 5 mm was significantly associated with adjacent-level ossification. Yang et al. [26] demonstrated that Zero-p can reduce the incidence of adjacent-level ossification and the plate length, which also affects the incidence of adjacent-level ossification. Lee et al. [32] showed that using a shorter plate with longer angulated screws resulted in a significantly reduced incidence of adjacent-level ossification. In our meta-analysis, three randomized controlled studies reported dysphagia after the procedure. The results indicated that the Zero-p group had a significantly lower adjacent-level ossification incidence than the ACP group (P < 0.05). Kim et al. [33] indicated that adjacent-level ossification may be caused by ossification due to the inflammatory reaction between the plate and the anterior longitudinal ligament. Although the aetiology of adjacent-level ossification is not known, many scholars are still concerned and suggest avoiding adjacent-level ossification.
Conclusion
Based on our analysis, Zero-p implants can reduce the incidence of postoperative dysphagia and adjacent-level ossification and reduce the operation time compared with ACP implants. However, for intraoperative blood loss, VAS, JOA score and NDI score, Zero-p implant, and ACP implant achieved similar clinical outcomes. Based on current evidence, we suggest that the Zero-p implant should be used in ACDF if possible to reduce the incidence of postoperative dysphagia and adjacent-level ossification.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- CDDD:
-
Cervical degenerative disc disease
- Zero-p:
-
Zero-profile
- ACP:
-
Anterior cervical plate
- NDI:
-
Neck Disability Index
- VAS:
-
Visual Analogue Scale
- JOA:
-
Japanese Orthopaedic Association
- RCTs:
-
Randomized controlled trials
- WMD:
-
Weighted mean difference
- CI:
-
Confidence interval
- RRs:
-
Risk ratios
- ACDF:
-
Anterior cervical decompression and fusion
References
Davies BM, Mowforth OD, Smith EK, Kotter MR. Degenerative cervical myelopathy. BMJ. 2018;360:k186.
Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Jt Surg Am. 1958;40-A(3):607–24.
Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine. 2009;34(26):2886–92.
Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI. Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: 2-year results of a multi-centric, randomized, controlled study. Spine. 2009;34(7):641–6.
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS Jr. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32:2310–7.
Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, Marciano FF, Crawford NR. A new stand alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine. 2009;34:156–60.
Cheung ZB, Gidumal S, White S, Shin J, Phan K, Osman N, Bronheim R, Vargas L, Kim JS, Cho SK. Comparison of anterior cervical discectomy and fusion with a stand-alone interbody cage versus a conventional cage-plate technique: a systematic review and meta-analysis. Global Spine J. 2018;9:219256821877457.
Duan Y, Yang Y, Wang Y, Liu H, Hong Y, Gong Q. Comparison of anterior cervical discectomy and fusion with the Zero-profile device versus plate and cage in treating cervical degenerative disc disease: a meta-analysis. J Clin Neurosci. 2016;33:11–8.
Haiyu S, Jinping C, Bin R, Feifei Y, Jun Z, Shaonan X, Yazeng H. Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res Actions Search. 2015;10:148.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Yu C, Huajiang C, Xiaodong W, Xinwei W, Wenbo L, Wen Y. Comparative analysis of clinical outcomes between Zero-profile implant and cages with plate fixation in treating multilevel cervical spondilotic myelopathy: a 3-year follow-up. Clin Neurol Neurosurg. 2016;144:72–6.
Yibing L, Dingjun H, Baorong H, Xiaodong W, Liang Y. The efficiency of Zero-profile implant in anterior cervical discectomy fusion: a prospective controlled long-term follow-up study. Clin Spine Surg. 2013;28:398.
Shenghua H, Hualong F, Zhiming L, Juyi L, Zhitao S, Yeguang W, Jian W, Zhiqiang R, Feiqiang H, Fuguang X. A randomized trial comparing clinical outcomes between Zero-profile and traditional multi-level anterior cervical discectomy and fusion surgery for cervical myelopathy. Spine. 2018;43:E259–66.
Scholz M, Onal B, Schleicher P, Pingel A, Hoffmann C, Kandziora F. Two-level ACDF with a Zero-profile stand-alone spacer compared to conventional plating: a prospective randomized single-center study. Eur Spine J. 2020;29:2814–22.
Xiao Y, Shi Y, Li H, Xu K. Application of Zero-p on anterior cervical decompression and bone fusion. Int J Clin Exp Med. 2017;10:7077–83.
Nemoto O, Kitada A, Naitou S, Tachibana A, Ito Y, Fujikawa A. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol. 2015;25:127–34.
Bin Y, Lin N. Clinical comparison of Zero-profile interbody fusion device and anterior cervical plate interbody fusion in treating cervical spondylosis. Int J Clin Exp Med. 2015;8:13854–8.
Korinth M. Treatment of cervical degenerative disc disease—current status and trends. Zentralbl Neurochir. 2008;69:113–24.
Matz PG, Ryken TC, Groff MW, Vresilovic EJ, Anderson PA, Heary RF, Holly LT, Kaiser MG, Mummaneni PV, Choudhri TF, Resnick DK. Techniques for anterior cervical decompression for radiculopathy. J Neurosurg Spine. 2009;11:183–97.
Wang Z, Jiang W, Li X, Wang H, Shi J, Chen J, Meng B, Yang H. The application of Zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J. 2015;24:148–54.
Schollhorn B, Burki A, Stahl C, Howard J, Forterre F. Comparison of the biomechanical properties of a ventral cervical intervertebral anchored fusion device with locking plate fixation applied to cadaveric canine cervical spines. Vet Surg. 2013;42:825–31.
Chang H, Baek DH, Choi BW. Efficacy of Zero-profile implant in anterior fusion to treat degenerative cervical spine disease: comparison with techniques using bone graft and anterior plating. J Neurol Surg A Cent Eur Neurosurg. 2015;76:268–73.
Lan T, Lin JZ, Hu SY, Yang XJ, Chen Y. Comparison between Zero-profile spacer and plate with cage in the treatment of single level cervical spondylosis. J Back Musculoskelet Rehabil. 2018;31:299–304.
Lee CH, Hyun SJ, Kim MJ, Yeom JS, Kim WH, Kim KJ. Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, an cage plus plating. J Spinal Disord Tech. 2013;26:112–8.
Andrei FJ, Jozef M, Jason WS, Alpesh AP. Dysphagia after anterior cervical spine surgery: a systematic review of potential preventative measures. Spine J. 2014;14:2246–60.
Yang H, Chen D, Wang X, Yang L, He H, Yuan W. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg. 2015;135:781–7.
Miao J, Shen Y, Kuang Y, Yang L, Wang X, Chen Y, Chen D. Early follow-up outcomes of a new Zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech. 2013;26:193–7.
Shao H, Chen J, Ru B, Yan F, Zhang J, Xu S, Huang Y. Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res. 2015;10:148.
Sun Z, Liu Z, Hu W, Yang Y, Xiao X, Wang X. Zero-p versus cage-plate in anterior cervical discectomy and fusion with a minimum 2 years follow-up: a meta analysis. World Neurosurg. 2018;120:e551–61.
Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Jt Surg Am. 2005;87:558.
Huang C, Mobbs R, Selby M, Phan K, Rao P. Adjacent-level ossification development in single-level standalone anterior cervical discectomy and fusion versus anterior cervical discectomy and fusion with plate. Global Spine J. 2020;11:292–8.
Lee DH, Lee JS, Yi JS, Cho W, Zebala LP, Riew KD. Anterior cervical plating technique to prevent adjacent-level ossification development. Spine J. 2013;13:823–9.
Kim HJ, Kelly MP, Ely CG, Dettori JR, Riew KD. The risk of adjacent-level ossification development after surgery in the cervical. Spine. 2012;37:S65–74.
Acknowledgements
Not applicable in this section.
Funding
Ordos City Science and Technology Plan Project (2021YYSHE186-61).
Author information
Authors and Affiliations
Contributions
YW and WY conducted research design data extraction. GG, HL and YL conducted data extraction. FG, QZ and XT conducted data analysis and quality evaluation. TZ and NG made the final result judgement and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable in this section.
Consent for publication
Not applicable in this section.
Competing interests
The authors declare no competing interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, T., Guo, N., Gao, G. et al. Comparison of outcomes between Zero-p implant and anterior cervical plate interbody fusion systems for anterior cervical decompression and fusion: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res 17, 47 (2022). https://doi.org/10.1186/s13018-022-02940-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-02940-w