Abstract
Objective
The purpose of the present study was to estimate complications and other outcomes associated with staple and suture closure after hip arthroplasty through meta-analysis techniques and a systematic review.
Methods
We searched for articles in EMBASE, PubMed, Medline, Web of Science and the Cochrane Library. To determine the eligibility of the searched trials, Cochrane Collaboration's Review Manager software was used to perform the meta-analysis.
Results
Five randomized controlled trials and one retrospective cohort trial were included in our study. Our study indicated that for skin closure after hip arthroplasty, the risks of superficial infection and prolonged discharge were higher with staples than with sutures. There was no significant difference between the two groups in terms of allergic reaction, dehiscence, inflammation, abscess formation, the Hollander Wound Evaluation Scale or patient's satisfaction with skin closure methods. However, suturing required a longer operating time.
Conclusions
Closure with sutures is associated with lower risks of superficial infection and prolonged discharge than closure with staples following hip arthroplasty, but it may take more time.
Similar content being viewed by others
Introduction
Hip arthroplasty is the final treatment for degenerative and traumatic hip disease. With the ageing of the population and the progress of medical technology, the rate of arthroplasty has consistently been rising over the past decades [1, 2]. Hip arthroplasty includes total hip arthroplasty and hemiarthroplasty [3]. It is estimated that by 2030, major total hip arthroplasty operations in the USA will be performed 572,000 times a year, an increase of 174% since 2005 [4].
Wound complications are one of the main morbidities of hip arthroplasty and can prolong hospitalization duration or lead to readmission, increase costs and reduce patient satisfaction [5, 6]. Surgical site infections (SSIs) are one of the most common and important complications after hip arthroplasty. Patients with early incision infections after hip arthroplasty have poor clinical scores in terms of postoperative pain and function. Some incision infections may spread inward, leading to deep infections and failure of the prosthesis [7]. Good skin closure in hip arthroplasty can achieve appropriate closure and rapid healing, with acceptable cosmesis and minimal complications such as infection, delayed dehiscence and haematoma[5]; in addition, the stress of early activities and accelerated wound rehabilitation programmes highlight the importance of skin closure [8].
Many materials have been used for skin closure in hip arthroplasty, among which sutures and staples are the most common [9]. However, there seems to be no consensus in the literature on which method of skin closure is superior in hip arthroplasty. Some studies show that the incidence of complications between skin staples and sutures is similar; however, studies also report that sutures can reduce costs and that sutures are less painful to remove [6, 10,11,12]. In addition, Yao Lu et al. found that the incidence of complications with suture closure was significantly lower than that with staple closure [13]. The main disadvantage of sutures is that it takes a longer time to suture a wound, and sutures require surgeons to have better suture skills [14]. Unlike sutures, the surface of the staples rarely touches the edge of the wound, and staples do not penetrate to the depth of the incision. Staplers do much less damage to wound defence and reduce the immune response. In the process of wound closure and removal, staples are also considered faster than sutures [15, 16]. However, Singh et al. [6] showed that using staples was more than three times costlier than using sutures. Therefore, further critical evidence is needed to prove which skin closure method is more suitable for surgical wound closure after hip arthroplasty.
Until recently, some meta-analyses and systematic reviews comparing staples with sutures for skin closure in orthopaedic procedures or total knee arthroplasty have been published [17,18,19,20]. However, after extensive searching through a large number of studies in the past, we found no related study comparing the wound complications, perioperative details and resource utilization of patients whose wound was closed with staples or sutures after hip arthroplasty. Meanwhile, some randomized controlled trials comparing staples and sutures for wound closure in hip arthroplasty have been published in recent years. The purpose of the present study was to estimate complications and other outcomes associated with staple and suture closure after hip arthroplasty through meta-analysis and systematic review. We hypothesized that skin staples would be associated with better outcomes in the assessment of all relevant variables.
Materials and methods
Literature search
Two investigators (ZL, BL) independently conducted an extensive search of electronic databases such as EMBASE, PubMed, Medline, Web of Science and the Cochrane Library on studies published between 1996 and October 2021. When searching, we used the following keywords and their combinations: staples, clips, suture, arthroplasty, hip, wound, closure, and skin. Our study included only English-language publications on human trials. In addition, the bibliographies of the included studies and dissertations were searched for additional sources. A manual search of relevant trials, reviews and related articles was also performed. Authors were contacted, when possible, to obtain missing information.
Inclusion and exclusion criteria
To be included in this study, the trials had to meet the following inclusion criteria: (1) be full-text randomized controlled trials and high-quality retrospective cohort studies; (2) compare staples versus sutures; (3) include patients treated with primary hip arthroplasty, including total hip arthroplasty or hemiarthroplasty; (4) include at least one of the key outcomes. The exclusion criteria were as follows: (1) studies on skin adhesives used for skin closure; (2) studies on barbed sutures; (3) studies were case reports, discourses, basic research, conference papers, non-English articles and other studies that did not contain results to our interest; (4) study data that could not be extracted. How deeper tissues were closed and the type of suture or stitch technique used were not considered exclusion criteria. The two authors independently assessed whether each article met the criteria for inclusion and then discussed their differences until they reached a consensus.
Selection of the literature
After eliminating duplicates, two independent researchers (ZL, BL) scanned the titles and abstracts according to predetermined selection criteria and selected randomized controlled trials that might be relevant. The researchers retrieved hard copies of all relevant articles and read the full texts for further identification. Relevant data were extracted through a predetermined standardized procedure involving the first author, the year of publication, the demographic characteristics of countries, the participants and the treatment options for each group.
Quality assessment
The Cochrane collaboration tool for assessing risk of bias was used to evaluate the methodological quality of the included randomized controlled trials [21]. This tool focuses on the internal validity of the trial and assessment of risk for possible bias in different phases of the trial. The details are as follows: random sequence generation, allocation concealment, blinding of outcome assessment, blinding of participants and personnel, incomplete outcome data, selective reporting, and other bias. Each item was classified according to a high, low, or unclear risk of bias that is represented as high (H), low (L), and unclear (U), respectively. The Newcastle–Ottawa Scale (NOS) was used to assess the quality of cohorts and case–control studies [22]. NOS ranges from 0 to 9 stars; research scores above 5 are considered high quality. All the assessments were conducted by the two independent reviewers (ZL, BL).
Data extraction
The relevant data from the eligible papers were subjected to double extraction by two authors (ZL, HY) according to a predefined standardized protocol. We extracted the baseline of each included study from trials that included the following information: design, closure material, age (mean and range), sex, BMI, closure length, stitch technique for suture, cohort size, follow-up, and information on the study objective. When inadequate information existed in the studies, contacting the study authors to obtain and clarify the relevant data was essential, as specified by the standardized protocol.
Outcome assessment
We extracted data on superficial infection, deep infection, prolonged discharge, abscess, wound dehiscence, allergic reaction, and inflammation as our primary evaluated outcomes. The secondary outcomes evaluated included wound closure time, length of stay in the hospital, the Hollander Wound Evaluation Scale (HWES), and the visual analogue scale (VAS).
Statistical analysis
The Review Manager Software Package (RevMan Version 5.3, The Cochrane Collaboration, Copenhagen, 2014) was used to generate forest plots. The overall effect of staples or sutures on wound closure was calculated as the weighted average of the inverse variance adjusted individual effects and 95% confidence interval (95% CI). The statistical heterogeneity among the individual studies was evaluated based on the Cochrane Q test and the I2 index [23], and statistical heterogeneity was confirmed if I2 was > 50% and P < 0.10 [24]. A variance-based fixed effect model was applied to calculate the pooled effect; otherwise, a random effect model was used in the presence of statistically significant heterogeneity [25]. If appropriate, the heterogeneity was identified and explained using a subgroup analysis [23]. Evidence grading was evaluated according to the Grading of Recommendations, Assessment, Development and Evaluation system [26].
Ethical statement
As all analyses were grounded on previously published studies, ethical approval was not necessary.
Results
Literature search
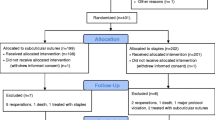
There were 2197 articles in the initial literature search. According to the inclusion and exclusion criteria, 188 articles were retained after removing duplicates and screening the title and abstract. Finally, after careful reading of the full text, five randomized controlled trials [6, 11, 12, 27, 28] and one retrospective cohort trial [13] were included in our study. The flowchart of the studies included is presented in Fig. 1.
Characteristics of the trials
A total of 1286 patients, 627 in the staples group and 659 in the sutures group were included in our study. Every patient we selected from this eligible study had undergone total hip replacement or hemiarthroplasty. One RCT[27] was divided into three groups: the skin clips group, OCA (2-octylcyanoacrylate) group, and sutures group. The OCA group was excluded from this meta-analysis. The retrospective cohort trial [13] was also divided into three groups: the subcuticular sutures group, the staples group and the interrupted sutures group. Because the subcuticular sutures group used staples as a supplementary means of skin closure, we also removed the subcuticular sutures group from this study. The mean age of the participants ranged from 55.7 years to 71 years in the staples group and from 57.8 years to 70 years in the sutures group. The sample sizes of the studies included ranged from 17 to 268. More detailed baseline characteristics of the eligible studies are shown in Table 1.
Risk of bias assessment
Based on the Cochrane Collaboration recommendation, four RCTs [11, 12, 27, 28] reported the detailed methods of random sequence generation. Two RCTs [12, 27] reported allocation concealments. The participants and personnel were blinded in 3 RCTs [6, 12, 27]. In addition, full details of withdrawals and dropouts were described in all studies. In some studies, the follow-up rate was 100%. Details of deviation risk are shown in Fig. 2. The bias risk of the retrospective cohort trial assessed with NOS is shown in Table 2.
Superficial infection
All six trials included in our study compared the superficial infection rates between the staples group and the suture group. Twenty out of 627 patients in the staples group were infected, while 6 out of 659 patients in the sutures group were infected. The fixed-effects meta-analysis of the 6 trials showed that the risk of superficial infection was higher with staples than with sutures for skin closure after hip arthroplasty. The odds ratio of superficial infection was 2.88 (95% CI 1.27–6.54; P = 0.01), and there was no heterogeneity (χ2 = 2.31; I2 = 0%; P = 0.81). The forest plots are illustrated in Fig. 3. In addition, we further compared the superficial infection rate between staples and sutures for skin closure after total hip arthroplasty. Data regarding superficial infection after total hip arthroplasty were reported in four studies[11, 12, 27, 28]. After total hip arthroplasty, 16 out of 499 patients in the staples group were infected, while 5 out of 501 patients in the sutures group were infected. The fixed-effects meta-analysis showed that the risk of superficial infection was higher with staples than with sutures for skin closure after total hip arthroplasty, with an OR (odds ratio) of 2.73 (95% CI 1.10 to 6.80; p = 0.03), and there was no heterogeneity (χ2 = 2.11; I2 = 0%; P = 0.55). The forest plots are illustrated in Fig. 4. All pooled outcomes comparing staples to sutures for skin closure after arthroplasty are listed in Table 3.
Deep Infection
Three of the trials compared the deep infection rates between the staples group and the sutures group. Seven out of 491 patients in the staples group were infected, while 4 out of 527 patients in the sutures group were infected. The fixed-effects meta-analysis of the 6 trials showed that the risk of deep infection was higher with staples than with sutures for skin closure after hip arthroplasty. The odds ratio of deep infection was 1.70 (95% CI 0.56–5.21; P = 0.35), and there was no heterogeneity (χ2 = 1.67; I2 = 0%; P = 0.43). The forest plots are illustrated in Fig. 5. Similarly, we further compared the deep infection rates between staples and sutures for skin closure after total hip arthroplasty. Data regarding deep infection after total hip arthroplasty were reported in four studies [11, 12, 27, 28]. After total hip arthroplasty, 5 out of 380 patients in the staples group were infected, while 4 out of 386 patients were infected in the sutures group. The fixed-effects meta-analysis showed that the risk of deep infection was higher with staples than with sutures for skin closure after total hip arthroplasty, with an OR (odds ratio) of 1.24 (95% CI 0.35–4.35; P = 0.74) and no heterogeneity (χ2 = 0.76; I2 = 0%; P = 0.38). The forest plot is illustrated in Fig. 6.
Prolonged discharge
Overall, 5 studies [6, 11, 13, 27, 28] reported on discharge after hip arthroplasty. Wound discharge lasting at least 4 days was recorded as ‘prolonged discharge’ in these studies; 55 out of 544 patients in the staples groups had prolonged discharge, while 21 out of 577 patients in the sutures groups had prolonged discharge. The fixed-effects meta-analysis of all 5 trials revealed that the risk of prolonged discharge was lower with sutures than with staples for skin closure after hip arthroplasty. The odds ratio of prolonged discharge was 2.88 (95% CI, 1.72 to 4.83; P < 0.0001), and there was no heterogeneity (χ2 = 1.48; I2 = 0%; P = 0.83). The forest plot is listed in Fig. 7.
Abscess
Two studies [13, 27] compared the number of participants who developed wound abscesses after hip arthroplasty. From a total of 321 patients, only one patient from the sutures group developed an abscess. The OR-based models revealed that the incidence of abscesses was similar between skin staples and sutures (OR = 0.30; 95% CI 0.01–7.54; P = 0.46), with no heterogeneity. The forest plots are illustrated in Fig. 8.
Wound dehiscence
Three studies [12, 13, 28] reported data on wound dehiscence. Four out of 462 patients in the staples group experienced wound dehiscence, while 2 out of 499 patients in the sutures group experienced wound dehiscence. The fixed-effects meta-analysis of 3 trials revealed that there was no significant difference in the risk of wound dehiscence between the two groups after hip arthroplasty (OR = 0.42; 95% CI 0.02–10.41; P = 0.60), with no heterogeneity. The forest plots are illustrated in Fig. 8.
Allergic reaction
Two trials [11, 27] reported allergic reactions. Two out of 300 patients had allergic reactions, and our findings showed that there was no significant difference in the risk of allergic reaction between the staples groups and the sutures groups after hip arthroplasty (OR = 0.39; 95% CI 0.09–1.69; P = 0.21; heterogeneity: χ2 = 0.03, P = 0.86, I2 = 0%). The forest plots are illustrated in Fig. 8.
Inflammation
A total of two trials [6, 13] reported inflammation. In the staples groups, there were signs of inflammation in 12 out of 128 participants, while in the sutures groups there were only seven out of 158 participants with signs of inflammation. However, our pooled result revealed that the differences noted between the staples group and sutures group were not statistically significant (OR = 3.78; 95% CI 0.05–317.93; P = 0.56; heterogeneity: χ2 = 7.43, P = 0.006, I2 = 87%). Because the heterogeneity was more than 50%, we chose the fixed-effects model. In addition, there are no additional data to support our further sensitivity or subgroup analysis. The forest plots are illustrated in Fig. 9.
Systematic review
In addition to the six outcomes assessed in our study, four other secondary outcomes (length of stay, Holland Wound Evaluation Score, closure time, and visual analogue score) were compared in the systematic review section of this study. The included trials did not provide appropriate data types to conduct a meta-analysis.
Wound closure time
Two studies reported the time required for wound closure. Khan et al. [27] and Rui et al. [12] both showed that wound closure with staples was significantly faster than with sutures. The data on wound closure time with staples or sutures are listed in Table 4.
Length of stay
Three studies indicated the length of stay in the hospital for wound closure with skin staples or sutures after hip arthroplasty. Khan et al. [27] and Lu et al. [13] both showed that there were no significant differences in the median length of stay in the hospital. However, Rui et al. [12] reported the length of stay in the hospital in the staples group compared with the sutures group. The median and interquartile ranges of length of stay in the hospital are listed in Table 4.
HWES (Hollander Wound Evaluation Score)
The HWES is a scoring rule to evaluate surgical wounds and predict wound healing. The HWES evaluates the wound for steps, irregular contour, edge separation, edge inversion, excessive deformation and overall appearance. Each category is graded with a score of 0 or 1. The total score is 0–6, and wounds with a score of 6 have the best prognosis. Two studies used the Hollander Wound Evaluation Score to evaluate wounds after hip arthroplasty. In the two studies [12, 27], the HWES of the staples groups was lower than that of the sutures groups, but there was no significant difference in Holland's wound evaluation score. The Hollander Wound Evaluation Scores are listed in Table 4.
VAS (visual analogue scale)
Two studies [12, 27] used the visual analogue scale (VAS) to evaluate the satisfaction of patients according to skin wound closure methods. The study by Khan et al. judged patient satisfaction with skin closure technology with a VAS score between 0 and 100, of which 100 denotes the greatest satisfaction, while Rui, M et al. assessed patient satisfaction with a VAS score between 0 and 10, with 10 denoting the greatest satisfaction. Both of these studies reported that there was no significant difference between the satisfaction of patients in the staples group and those in the sutures group after hip arthroplasty. The Visual Analogue Scale (VAS) scores are listed in Table 4.
Discussion
Hip arthroplasty is the final treatment for debilitating hip joint disease. In recent years, the number of hip replacements has been increasing. [2]. The main purpose of skin closure in hip arthroplasty is to obtain sufficient closure, to promote rapid healing with an acceptable appearance, and to reduce complications such as delayed healing, dehiscence, haematoma and infection [10, 29]. There are many kinds of skin closure materials used in hip arthroplasty, and staples and sutures have served as primary materials for superficial skin closure [30]. At present, there are no clear clinical guidelines for skin closure after hip arthroplasty. Overall, our goal of this systematic review and meta-analysis was to provide valuable information about sutures versus staples for wound closure in hip arthroplasty. In the present study, we evaluated superficial infection, deep infection, prolonged discharge, abscess, wound dehiscence, allergic reaction, inflammation, wound closure time, length of stay in the hospital, Hollander Wound Evaluation Score, and patient satisfaction with skin closure methods from five eligible RCTs and one retrospective cohort trial that compared outcomes with staples or sutures for skin wound closure after hip arthroplasty.
In the present study, we found that the risk of superficial infection with sutures was less than twice that with staples. We found that our pooled result was similar to that of a previous meta-analysis by Smith et al. [19], who reported that after orthopaedic surgery, the risk of wound infection was significantly higher when the wound was closed with staples than with sutures, especially in patients who underwent hip surgery. Shetty et al. [31] also showed that the incidence of superficial wound infection was significantly higher when metal staples were used to suture skin wounds after hip fractures. In addition, our meta-analysis showed that the risk of superficial infection with staples was higher than that with sutures for skin closure after total hip arthroplasty. However, regardless of hip arthroplasty or total hip arthroplasty, there was no significant difference between the staples group and the sutures group in the comparison of deep infection which may be related to the use of antibiotics and deep tissue sutures. Surgical site infection increases the burden on the health care system, increases the length of stay, rehospitalization rate and cost of health care, and adversely affects the quality of life and function of patients [32]. Therefore, our meta-analysis results may be helpful to practitioners in making the choice between staples and sutures for wound closure following hip arthroplasty. However, there are still some potential prognostic factors that remain uncertain. For example, surgical techniques, expertise, aseptic techniques, antibiotic time and patient-specific prognostic factors may also influence surgical site infection risk [33]. Therefore, we need more high-quality randomized, blind, and long-lasting follow-up RCTs to be published and subsequently included in our analysis to help us choose the best wound closure method following hip arthroplasty. In the meantime, our findings suggest that the prolonged wound discharge rate was significantly lower in the sutures group. Our results and those of previous studies show that skin wounds closed with sutures are more resistant to infection, which then affects wound healing and wound discharge [34]. However, many potential factors affect the use of sutures as well, such as the accuracy aligning dermal margins and the doctor's skill, which may also affect the exudation of wound discharge [35].
In addition, we compared the incidence of abscess, wound dehiscence, allergic reaction and inflammation between the two groups, and our analysis showed that there were no significant differences in the outcomes between the staples group and sutures group. Our results lend support to the conclusions of Krishnan et al. [18], who reported no significant difference in allergic reaction, inflammation, dehiscence, or abscess formation between the two groups after orthopaedic surgery. However, it is important to note that only two RCTs analysed LOS (length of stay), allergic reaction, inflammation, dehiscence, and abscess formation between the two groups. Finally, our systematic review results show that there was no significant difference in HWES and patient satisfaction with skin wound closure methods after hip arthroplasty. Therefore, this is not a factor that affects our choice of skin closure methods after hip arthroplasty. Khan et al. [27] and Lu et al. [13] both showed that there were no significant differences in the median length of stay in the hospital. However, Rui et al. [12] reported that the median (interquartile range) length of hospital stay (days) in the staples groups was 12 (11–13) days versus 6.0 (5–8) days in the sutures group. The results suggest that the length of hospitalization following staple closure may be slightly longer than that following suture closure. Khan et al. [27] reported an estimated two-minute savings in time using staples for skin closure. Rui, M[12] also reported that the use of staples for skin closure compared with sutures can save approximately five minutes. The results suggest that the use of staples may be slightly faster than the use of skin sutures after hip arthroplasty.
Although this analysis was performed on 6 studies, and these different studies compared outcomes with different methods, we tried our best to analyse the data that could be included. The limitations of this meta-analysis and systematic review include the small number of included high-quality RCTs, unified surgical management programmes and rehabilitation programmes as well as publishing language. Some studies or guides have documented the distorting effects of location bias and publication bias on system evaluation and meta-analysis [36,37,38]. The poor quality of evidence in original studies reduces the quality of evidence in meta-analysis. Because of some characteristics of surgical techniques, orthopaedic surgeons cannot carry out blinded studies. Therefore, attention should be given to interpreting the conclusions of this meta-analysis. Due to the small number of studies included in this meta-analysis, we expect more high-quality RCTs to be published in the future, and future research should focus on high-quality randomized controlled trials. Detailed baseline characteristics and detailed patient recruitment flowcharts should be provided.
Conclusion
In summary, our meta-analyses and systematic review suggest that the risks of superficial infection and prolonged discharge are higher with staples than with sutures for skin closure after hip arthroplasty. However, there was no significant difference in allergic reaction, inflammation, dehiscence, abscess formation, the Hollander Wound Evaluation Score or satisfaction among patients who received either wound closure technique after hip arthroplasty. However, the suture technique may require a longer operating time.
Availability of data and materials
All data and material generated or analysed during this study are included in this published article.
Abbreviations
- SSIs:
-
Surgical site infections
- RCTs:
-
Randomized controlled trials
- H:
-
High
- L:
-
Low
- U:
-
Unclear
- NOS:
-
Newcastle–Ottawa scale
- 95% CIs:
-
95% Confidence intervals
- OCA:
-
2-Octylcyanoacrylate
- OR:
-
Odds ratio
- HWES:
-
Hollander Wound Evaluation Score
- VAS:
-
Visual analogue scale AR Androgen receptor
- LOS:
-
Length of stay
References
Han Y, Yang W, Pan J, Zeng L, Liang G, Lin J, et al. The efficacy and safety of knotless barbed sutures in total joint arthroplasty: a meta-analysis of randomized-controlled trials. Arch Orthop Trauma Surg. 2018;138(10):1335–45.
Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(8):624–30.
Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010;340:c2332.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5.
Clayer M, Southwood RT. Comparative study of skin closure in hip surgery. Aust N Z J Surg. 1991;61(5):363–5.
Singh B, Mowbray MAS, Nunn G, Mearns S. Closure of hip wound, clips or subcuticular sutures: does it make a difference? Eur J Orthop Surg Traumatol. 2006;16(2):124–9.
Gaine WJ, Ramamohan NA, Hussein NA, Hullin MG, McCreath SW. Wound infection in hip and knee arthroplasty. J Bone Joint Surg Br. 2000;82(4):561–5.
Dowsey MM, Kilgour ML, Santamaria NM, Choong PF. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust. 1999;170(2):59–62.
Patel RM, Cayo M, Patel A, Albarillo M, Puri L. Wound complications in joint arthroplasty: comparing traditional and modern methods of skin closure. Orthopedics. 2012;35(5):e641–6.
Slade Shantz JA, Vernon J, Morshed S, Leiter J, Stranges G. Sutures versus staples for wound closure in orthopaedic surgery: a pilot randomized controlled trial. Patient Saf Surg. 2013;7(1):6.
Buttaro MA, Quinteros M, Martorell G, Zanotti G, Comba F, Piccaluga F. Skin staples versus intradermal wound closure following primary hip arthroplasty: a prospective, randomised trial including 231 cases. Hip Int. 2015;25(6):563–7.
Rui M, Zheng X, Sun SS, Li CY, Zhang XC, Guo KJ, et al. A prospective randomised comparison of 2 skin closure techniques in primary total hip arthroplasty surgery. Hip Int. 2018;28(1):101–5.
Lu Y, Wang C, Lin L, Qin Q, Li Q. Complication rate of different wound closures after primary hip arthroplasty - A survey of 373 patients. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2018;11:15–8.
Ranaboldo CJ, Rowe-Jones DC. Closure of laparotomy wounds: skin staples versus sutures. Br J Surg. 1992;79(11):1172–3.
Kanegaye JT, Vance CW, Chan L, Schonfeld N. Comparison of skin stapling devices and standard sutures for pediatric scalp lacerations: a randomized study of cost and time benefits. J Pediatr. 1997;130(5):808–13.
Barrow J, Divecha H, Board T. Skin closure in arthroplasty surgery: current practice. Int Wound J. 2018;15(6):966–70.
Kim KY, Anoushiravani AA, Long WJ, Vigdorchik JM, Fernandez-Madrid I, Schwarzkopf R. A meta-analysis and systematic review evaluating skin closure after total knee arthroplasty-what is the best method? J Arthroplasty. 2017;32(9):2920–7.
Krishnan R, MacNeil SD, Malvankar-Mehta MS. Comparing sutures versus staples for skin closure after orthopaedic surgery: systematic review and meta-analysis. BMJ Open. 2016;6(1):e009257.
Smith TO, Sexton D, Mann C, Donell S. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199.
Krishnan RJ, Crawford EJ, Syed I, Kim P, Rampersaud YR, Martin J. Is the risk of infection lower with sutures than with staples for skin closure after orthopaedic surgery? A meta-analysis of randomized trials. Clin Orthop Relat Res. 2019;477(5):922–37.
Michaelis R, Tang V, Wagner JL, Modi AC, Curt LaFrance W, Jr., Goldstein LH, et al. Cochrane systematic review and meta-analysis of the impact of psychological treatments for people with epilepsy on health-related quality of life. Epilepsia. 2018;59(2):315–32.
G.A. Wells, B. Shea, D. O'Connell, J. Peterson, V. Welch, M. Losos. The NewcastleeOttawa Scale (NOS) for Assessing the Quality of Non-randomized Studies in Meta-analysis.
Melsen WG, Bootsma MC, Rovers MM, Bonten MJ. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20(2):123–9.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–45.
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Khan RJ, Fick D, Yao F, Tang K, Hurworth M, Nivbrant B, et al. A comparison of three methods of wound closure following arthroplasty: a prospective, randomised, controlled trial. J Bone Joint Surg Br. 2006;88(2):238–42.
Mallee WH, Wijsbek AE, Schafroth MU, Wolkenfelt J, Baas DC, Vervest TMJS. Wound complications after total hip arthroplasty: a prospective, randomised controlled trial comparing staples with sutures [published online ahead of print, 2020 Jul 7]. Hip Int. 2020;1120700020939075.
Ercole FF, Chianca TC, Duarte D, Starling CE, Carneiro M. Surgical site infection in patients submitted to orthopedic surgery: the NNIS risk index and risk prediction. Rev Lat Am Enfermagem. 2011;19(2):269–76.
Livesey C, Wylde V, Descamps S, Estela CM, Bannister GC, Learmonth ID, et al. Skin closure after total hip replacement: a randomised controlled trial of skin adhesive versus surgical staples. J Bone Joint Surg Br. 2009;91(6):725–9.
Shetty AA, Kumar VS, Morgan-Hough C, Georgeu GA, James KD, Nicholl JE. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticular vicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong). 2004;12(2):191–3.
Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23(4):183–9.
de Jonge SW, Gans SL, Atema JJ, Solomkin JS, Dellinger PE, Boermeester MA. Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection: A systematic review and meta-analysis. Medicine (Baltimore). 2017;96(29):e6903.
Thakore RV, Greenberg SE, Shi H, Foxx AM, Francois EL, Prablek MA, et al. Surgical site infection in orthopedic trauma: A case-control study evaluating risk factors and cost. J Clin Orthop Trauma. 2015;6(4):220–6.
Meiring L, Cilliers K, Barry R, Nel CJ. A comparison of a disposable skin stapler and nylon sutures for wound closure. S Afr Med J. 1982;62(11):371–2.
Egger M, Smith GD. Bias in location and selection of studies. BMJ. 1998;316(7124):61–6.
Ernst E, Pittler MH. Alternative therapy bias. Nature. 1997;385(6616):480.
Sood A, Knudsen K, Sood R, Wahner-Roedler DL, Barnes SA, Bardia A, et al. Publication bias for CAM trials in the highest impact factor medicine journals is partly due to geographical bias. J Clin Epidemiol. 2007;60(11):1123–6.
Acknowledgements
This work was supported by 2018 Key scientific and technological projects in Henan Province (ID: 2018020041).
Funding
This study was funded by Key scientific and technological projects in Henan Province (ID: 2018020041).
Author information
Authors and Affiliations
Contributions
ZL and BL contributed to the study design, data analysis and writing. HY contributed to the data collections and data analysis. LZ contributed to the study design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Z., Liu, B., Yang, H. et al. Staples versus sutures for skin closure in hip arthroplasty: a meta-analysis and systematic review. J Orthop Surg Res 16, 735 (2021). https://doi.org/10.1186/s13018-021-02870-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02870-z