Abstract
Background
Robot-assisted platforms in spine surgery have rapidly developed into an attractive technology for both the surgeon and patient. Although current literature is promising, more clinical data is needed. The purpose of this paper is to determine the effect of robot-related complications on clinical outcomes
Methods
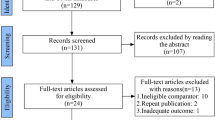
This multicenter study included adult (≥18 years old) patients who underwent robot-assisted lumbar fusion surgery from 2012-2019. The minimum follow-up was 1 year after surgery. Both bivariate and multivariate analyses were performed to determine if robot-related factors were associated with reoperation within 1 year after primary surgery.
Results
A total of 320 patients were included in this study. The mean (standard deviation) Charlson Comorbidity Index was 1.2 (1.2) and 52.5% of patients were female. Intraoperative robot complications occurred in 3.4% of patients and included intraoperative exchange of screw (0.9%), robot abandonment (2.5%), and return to the operating room for screw exchange (1.3%). The 1-year reoperation rate was 4.4%. Robot factors, including robot time per screw, open vs. percutaneous, and robot system, were not statistically different between those who required revision surgery and those who did not (P>0.05). Patients with robot complications were more likely to have prolonged length of hospital stay and blood transfusion, but were not at higher risk for 1-year reoperations. The most common reasons for reoperation were wound complications (2.2%) and persistent symptoms due to inadequate decompression (1.5%). In the multivariate analysis, robot related factors and complications were not independent risk factors for 1-year reoperations.
Conclusion
This is the largest multicenter study to focus on robot-assisted lumbar fusion outcomes. Our findings demonstrate that 1-year reoperation rates are low and do not appear to be influenced by robot-related factors and complications; however, robot-related complications may increase the risk for greater blood loss requiring a blood transfusion and longer length of stay.
Similar content being viewed by others
Introduction
Robotic surgery has rapidly developed into an attractive option for spine surgeons as evidenced by the growing literature in the last few years [1,2,3,4]. Numerous reports demonstrate excellent pedicle screw accuracy and early studies have explored the impact of robot-assisted spine surgery on reducing radiation exposure, length of hospital stay, operative time, and perioperative complications in comparison to conventional freehand technique [5,6,7,8,9,10]. However, current literature has been derived from mostly single-center or single-surgeon studies [11,12,13,14,15]. Furthermore, the impact of robot-related complications on clinical outcomes remains unclear.
Reoperation rates are particularly important in spine surgery because they imply disease progression or surgical complications. Complete reoperation data in robotic spine surgery remains to be elucidated as most studies only report intraoperative revisions due to screw misplacement and rates are exceedingly low. In a large, retrospective study of 359 patients, Keric et al. reported a reoperation rate of 1.7% [8]. Other authors in smaller, prospective randomized control trials have reported reoperation rates of 0.0% at up to 2 years [14, 16]. Additional reported post-operative complications in robotic surgery that have led to revision surgery include wound healing issues, new neurological deficits, and infections [7, 8].
The purpose of this study is to examine the influence of robot-related complications on clinical outcomes, including 1-year reoperations, after robot-assisted lumbar fusion. To the authors’ knowledge, this is the first multicenter assessment of complications related to robot-assisted lumbar fusion with a minimum 1-year follow-up. We hypothesize that robot-related factors do not influence reoperation risk, but may prolong operative time. Our study’s findings may further contribute to the acceptance of robotic-assisted spine surgery as an excellent surgical option for surgeons and patients alike.
Materials and Methods
Patient selection
We reviewed a multicenter database of adult patients (≥18 years old) who underwent robot-assisted lumbar arthrodesis between 2012 and 2019. All surgeries were performed by either the Renaissance (Renaissance, Mazor Robotics Ltd., Israel) or Mazor X system (Mazor Robotics Ltd.). Patients with missing data or who underwent spinal fusion at unrelated levels (cervical, thoracic) were excluded from our study. The minimum follow-up was 1 year after the date of surgery. This study was approved by the institutional review board.
Data collection
Several perioperative factors were collected and included patient demographics, comorbidity profile, smoking status, body mass index, and primary preoperative diagnosis. Robot factors included open vs. percutaneous surgery, robot time spent per screw, robot screws placed per patient, and robot system (Renaissance or Mazor X). Other operative factors included primary vs. revision surgery, number of instrumented levels per patient, pelvic fixation, and total operative time.
Robot-related complications included intraoperative exchange of robot screw due to breach, robot abandonment due to registration issues or unreachable anatomy, intraoperative loss of motor/sensory function, and return to the operating room during the same inpatient stay for screw removal and/or exchange. Even though surgeons generally would not characterize an intraoperative redirection of a screw using freehand, flouro-assist or navigation as a “complication,” we wanted to have strict criteria when assessing any variance with the planned surgery. We evaluated the impact of each robot-related factor on reoperation risk as well as the composite of all robot-related complications, which was defined as the variable, “any robot-related complication.” A reoperation was defined as any return to the operating room during a subsequent hospital encounter. In other words, a return to the operating room during the same index hospital stay was not considered a reoperation.
Data analysis
The primary outcome of our study was reoperation within 1 year after the index surgery. Secondary outcomes of interest included estimated blood loss, perioperative blood transfusion, total operative time, and length of hospital stay. The chi-square test and t test were used to compare categorical and continuous variables, respectively. Both bivariate and multivariate logistic regression analyses were performed to determine if robot-related complications were associated with reoperation within 1 year after primary surgery. Statistical significance was defined as a P value <0.05. SAS Studio Version 3.4 (SAS Institute Inc., Cary, NC) was used for all statistical analyses.
Results
A total of 320 patients were included in this study. The mean (standard deviation) Charlson Comorbidity Index (CCI) was 1.2 (1.2), 44.7% (N=143) of patients were obese, 10% (N=32) were prior/current smokers, and 52.5% (N=168) of patients were female. The most common preoperative primary diagnoses included high-grade spondylolisthesis (60.3%, N=193), degenerative disk disease (18.1%, N=58), and spinal stenosis (9.7%, N=31). The mean number of instrumented levels was 2.8 (0.9), 17.5% (N=56) of surgeries were open (vs. percutaneous), 48.8% (N=156) were performed with the X robot (vs. Renaissance), 6.6% (N=21) of patients had pelvic fixation, the mean robot time was 28.7 (21.3) minutes, and the mean total operative time was 126 (92) minutes (Table 1).
Intraoperative robot complications occurred in 3.4% (N=11) of patients. These included robot abandonment (2.5%, N=8), return to the operating room during the same inpatient stay for screw removal and/or exchange (1.3%, N=4), and intraoperative exchange of screw for breach (0.9%, N=3). No intraoperative loss of motor/sensory function was observed in this study’s cohort. Intraoperative dural tear occurred in 3 patients (0.9%), but these occurred during decompression during revision laminectomy and were not directly related to robot factors (Table 1).
The 1-year reoperation rate was 4.4% (N=14) [1 to 90 days = 2.5%, N=8; 91 days to 1 year = 1.9%, N=6]. Robot characteristics were not statistically different between those who required revision surgery and those who did not (P>0.05). These factors included open surgery [vs. percutaneous] (no reoperation = 17.6%, N=54 vs. reoperation = 14.3%, N=2), robot time (seconds) per screw (no reoperation = 6.6 vs. reoperation = 6.1), and robot system (Renaissance: no reoperation = 52.3%, N=160 vs. reoperation = 28.6%, N=4; Mazor X: no reoperation = 47.7%, N=146 vs. reoperation = 71.4%, N=10). Intraoperative robot complications such as exchange of a breached screw and robot abandonment for either registration errors or unreachable anatomy did not appear to influence reoperation risk. Interestingly, return to the operating room during the same inpatient stay for screw removal and/or exchange was a significant risk factor for reoperation (no reoperation 1.0% (N=3) vs. reoperation 7.1% (N=1)) (P=0.042) in the bivariate analysis (Table 1).
In the secondary outcome analysis, patients with robot complications were more likely to have prolonged length of hospital stay (any robot complication: 5.9 days vs. no robot complication: 4.8 days, P=0.019), a higher estimated blood loss (any robot complication: 324 mL vs. no robot complication: 78 mL, P<0.001), and an increased blood transfusion rate (any robot complication: 21.4% vs. no robot complication: 1%, P<0.001). Robot complications did not appear to be associated with longer operative time or robot time (Table 2).
The most common reasons for reoperation were wound complications (2.2%, N=7) and persistent symptoms due to inadequate decompression (1.5%, N=5). In this study cohort, no reoperations were due to screw malposition or implant failure (Table 3). In the multivariate analysis for 1-year reoperations, robot-related factors and any robot-related complications were not independent risk factors (Table 4).
Discussion
Over the last two decades, there has been an increasing amount of literature in support for robot-assisted spine surgery. Most of this literature has focused on pedicle screw accuracy, and recent meta-analyses on randomized controlled trials have found robot-guided spine cases to be more accurate in pedicle screw placement with fewer proximal facet violations than conventional freehand techniques [17, 18]. However, other intraoperative robot complications, such as robot abandonment due to registration issues, are important to identify since they may have a negative impact on operative time and complications; however, their true incidence is not known since they are rarely mentioned in current literature. Furthermore, the consequence of robot-related complications on clinical outcomes, including post-discharge reoperations, has not been examined.
Using the Renaissance robot from 2011 to 2016, Keric et al. examined the outcomes for 406 patients who underwent thoracolumbar robot-assisted spine surgery [8]. Intraoperative robot complications included conversion to freehand due to registration failure (1.7%, N=7), dural tears (6.4%, N=26), and screw misplacement requiring revision surgery (0.48%, N=2 screws). The registration issues were seen in patients with severe osteopenia and obese patients whose significant soft tissue resulted in poor radiographic quality. All dural tears occurred during decompression or cage implantation. Screw breach most often occurred due to skiving or platform displacements. The overall revision rate was 9.4%, and included wound complications (4.9%, N=20), durotomy repair (0.49%, N=2), new neurologic deficits (0.49%, N=2), and screw misplacement or screw loosening (3.4%, N=14). Although these authors provided an excellent, detailed assessment of their robot-related complications, it is unclear what the consequence of these errors had on other clinical outcomes, including operative time and length of stay. In addition, Keric et al. report that their study used data from two different neurosurgical departments; however, follow-up data was only reported for one hospital and the mean follow up was only 75.5 days. Furthermore, it is unclear if the rate of screw exchange included intraoperative screw revision during the index surgery.
In a single-center, retrospective analysis, Zhang et al. examined robot failure with the Renaissance system in 76 patients (874 screws) [19]. There were 39 screws (4.5%) which were adjusted during the operation, and registration failed in two patients (2.8%), both of whom had congenital scoliosis. In their multivariate analysis, they found that osteoporosis, obesity, vertebral rotation, and congenital scoliosis were independent risk factors for inaccurate pedicle screw placement (Gertzbein and Robbins—grades C, D, and E). Registration failure typically occurs when there are differences between the intraoperative positioning or imaging and the preoperative CT scan. These authors hypothesized that this can occur in patients with non-rigid scoliosis where their deformities may change after muscle relaxation with anesthesia. It is also possible that robots have more difficulty matching preoperative and intraoperative imaging in patients with poor bone mineral density. Other instances of robot failure can occur due to unreachable anatomy, which may be observed in obese patients or those with severe rotation in their vertebral bodies. Zhang et al. provided significant insight on their intraoperative robot complications and emphasized the importance of appropriate patient selection when considering robot-assisted spine surgery. However, the aim of this study was to perform risk factor analysis and the impact of these intraoperative complications on other outcomes was not addressed.
The literature on reoperations after robot-assisted spine surgery is sparse and rates are variable. Kantelhardt et al. performed a retrospective analysis on 55 patients (250 screws) who underwent robot-assisted spine surgery with a mean follow up of 3 months [7]. They reported an intraoperative complication rate of 4.7% (major hemorrhage, dural tears), wound healing issues in 13.5%, and reoperation for screw malposition in 1% of robotic-guided cases. Jiang et al examined 28 patients who underwent robot-assisted short lumbar (1 level or 2 level) fusions and reported a 30-day reoperation of 3.6% (N=1) [11]. Schroder and Staartjes reported on 72 patients who underwent robot-guided lumbar fusion for spondylolisthesis with a minimum 1-year follow up. None of their pedicle screws required intraoperative repositioning, and the authors denied any implant-related revisions or complications during the study’s follow-up period. The overall non-screw-related reoperation rate was 4.2% (2 patients with facet cyst removal, 1 patient with adjacent segment disease) [20]. Much of the current literature on reoperation rates after robot-assisted spine surgery is limited by short follow-up, single center series, and relatively small sample sizes.
In comparison to prior literature, this is the first multicenter study to examine robot-related complications and their potential influence on other clinical outcomes after robot-assisted spine surgery. We observed that robot complications are not uncommon (3.4%) and included screw breach, robot abandonment due to either unreachable anatomy or registration issues, and return to the operating room for screw exchange. Although robot abandonment and screw exchange, especially where there is no injury to motor/sensory function, may appear benign, these were associated with greater blood loss requiring blood transfusion and significantly longer length of hospital stay (more than 1 day), which can be costly. The reoperation rate within 1 year after the index surgery was 4.4%. The most common reasons for reoperation were wound complications (2.2%) and persistent symptoms due to inadequate decompression (1.5%). Robot factors, including robot time per screw, open vs. percutaneous, and robot system, were not statistically significant for reoperation risk. Furthermore, patients with robot-related complications at the index surgery were not at higher risk for 1-year reoperations.
Several limitations should be considered in this study. First, the minimum follow-up was 1 year after the index surgery. It is possible that complications, such as implant failure, can occur beyond this follow-up period. Second, the data collection for patient-reported outcomes was sporadic for this patient population and precluded further analysis of this important outcome variable. It is possible that patients who require multiple surgeries during the same hospital encounter or have prolonged hospital stays due to robot-related complications may have worse patient-reported outcomes. Third, cost data was not available at the time of our study and should be included in future studies to examine factors that may improve cost efficiency.
Despite these limitations, this is the first and largest multicenter study to focus on robot-assisted lumbar fusion outcomes. Our study demonstrates that robot-related complications and 1-year reoperation rates are low. Robot-related factors and complications do not increase reoperation risk; however, robot-related complications may increase the risk for greater blood loss requiring a blood transfusion and prolonged length of hospital stay. These findings can be included during the preoperative decision-making discussions with the patient.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CCI:
-
Charlson Comorbidity Index
- BMI:
-
Body mass index
- SD:
-
Standard deviation
References
Joseph JR, Smith BW, Liu X, et al. Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus. 2017;42(5):E2.
Li J, Fang Y, Jin Z, et al. The impact of robot-assisted spine surgeries on clinical outcomes: a systemic review and meta-analysis. Int J Med Robot. 2020;16(6):e2143.
Siccoli A, Klukowska AM, Schröder ML, et al. A systematic review and meta-analysis of perioperative parameters in robot-guided, navigated, and freehand thoracolumbar pedicle screw instrumentation. World Neurosurg. 2019;127:576–587.e575.
Staartjes VE, Klukowska AM, Schröder ML. Pedicle screw revision in robot-guided, navigated, and freehand thoracolumbar instrumentation: a systematic review and meta-analysis. World Neurosurg. 2018;116:433–443.e438.
Ghasem A, Sharma A, Greif DN, Alam M, Maaieh MA. The arrival of robotics in spine surgery: a review of the literature. Spine (Phila Pa 1976). 2018;43(23):1670–7. https://doi.org/10.1097/BRS.0000000000002695.
Lieber AM, Kirchner GJ, Kerbel YE, Khalsa AS. Robotic-assisted pedicle screw placement fails to reduce overall postoperative complications in fusion surgery. Spine J. 2019;19(2):212–7. https://doi.org/10.1016/j.spinee.2018.07.004.
Kantelhardt SR, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20(6):860–8. https://doi.org/10.1007/s00586-011-1729-2.
Keric N, Doenitz C, Haj A, et al. Evaluation of robot-guided minimally invasive implantation of 2067 pedicle screws. Neurosurg Focus. 2017;42(5):E11.
Keric N, Eum DJ, Afghanyar F, Rachwal-Czyzewicz I, Renovanz M, Conrad J, et al. Evaluation of surgical strategy of conventional vs. percutaneous robot-assisted spinal trans-pedicular instrumentation in spondylodiscitis. J Robot Surg. 2017;11(1):17–25. https://doi.org/10.1007/s11701-016-0597-5.
Feng S, Tian W, Sun Y, Liu Y, Wei Y. Effect of robot-assisted surgery on lumbar pedicle screw internal fixation in patients with osteoporosis. World Neurosurg. 2019;125:e1057–62. https://doi.org/10.1016/j.wneu.2019.01.243.
Jiang B, Pennington Z, Azad T, Liu A, Ahmed AK, Zygourakis CC, et al. Robot-assisted versus freehand instrumentation in short-segment lumbar fusion: experience with real-time image-guided spinal robot. World Neurosurg. 2020;136:e635–45. https://doi.org/10.1016/j.wneu.2020.01.119.
Khan A, Meyers JE, Siasios I, Pollina J. Next-generation robotic spine surgery: first report on feasibility, safety, and learning curve. Oper Neurosurg (Hagerstown). 2019;17(1):61–9. https://doi.org/10.1093/ons/opy280.
Kim HJ, Jung WI, Chang BS, Lee CK, Kang KT, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot. 2017;13(3). https://doi.org/10.1002/rcs.1779.
Kim HJ, Kang KT, Chun HJ, et al. Comparative study of 1-year clinical and radiological outcomes using robot-assisted pedicle screw fixation and freehand technique in posterior lumbar interbody fusion: a prospective, randomized controlled trial. Int J Med Robot. 2018;14(4):e1917.
Laudato PA, Pierzchala K, Schizas C. Pedicle screw insertion accuracy using O-arm, robotic guidance, or freehand technique: a comparative study. Spine (Phila Pa 1976). 2018;43(6):E373–e378. https://doi.org/10.1097/BRS.0000000000002449.
Park SM, Kim HJ, Lee SY, Chang BS, Lee CK, Yeom JS. Radiographic and clinical outcomes of robot-assisted posterior pedicle screw fixation: two-year results from a randomized controlled trial. Yonsei Med J. 2018;59(3):438–44. https://doi.org/10.3349/ymj.2018.59.3.438.
Li HM, Zhang RJ, Shen CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine (Phila Pa 1976). 2020;45(2):E111–e119. https://doi.org/10.1097/BRS.0000000000003193.
Peng YN, Tsai LC, Hsu HC, et al. Accuracy of robot-assisted versus conventional freehand pedicle screw placement in spine surgery: a systematic review and meta-analysis of randomized controlled trials. Ann Transl Med. 2020;8(13):824.
Zhang JN, Fan Y, Hao DJ. Risk factors for robot-assisted spinal pedicle screw malposition. Sci Rep. 2019;9(1):3025.
Schröder ML, Staartjes VE. Revisions for screw malposition and clinical outcomes after robot-guided lumbar fusion for spondylolisthesis. Neurosurg Focus. 2017;42(5):E12.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception: NJL, RAL. Design of work: NJL, RAL. Acquisition of data: EL, ALB, JP, EJ, CH, TCS, CRG, JML, RAL. Analysis and interpretation of data: NJL, EL. Creation of new software used in the work: Not applicable. Drafted the work: NJL, IAB, VB, JM, GM, PJP, EL, ALB, JP, EJ, CH, TCS, CRG, JML, RAL. Approved submitted version: NJL, IAB, VB, JM, GM, PJP, EL, ALB, JP, EJ, CH, TCS, CRG, JML, RAL. Agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature: NJL, IAB, VB, JM, GM, PJP, EL, ALB, JP, EJ, CH, TCS, CRG, JML, RAL. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Yes. This project was approved by the hospital’s IRB AAAT1470.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, N.J., Buchanan, I.A., Boddapati, V. et al. Do robot-related complications influence 1 year reoperations and other clinical outcomes after robot-assisted lumbar arthrodesis? A multicenter assessment of 320 patients. J Orthop Surg Res 16, 308 (2021). https://doi.org/10.1186/s13018-021-02452-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02452-z