Abstract
Background
The surgical treatment of osteoporotic vertebral fractures (OVF) is generally associated with a high risk of complications due to an aging population with osteoporosis; however, the detailed risk factors for systemic complications and mortality have not been clarified. We evaluated the risk factors for systemic complications and mortality in surgically treated OVF patients using a large national inpatient database.
Methods
Patients over 65 years old who were diagnosed with OVF and received either anterior fusion (AF) or posterior fusion (PF), from 2012 to 2016, were extracted from the diagnosis procedure combination (DPC) database. In each of the perioperative systemic complications (+) or (−) group, and the in-hospital death (+) or (−) group, we surveyed the various risk factors related to perioperative systemic complications and in-hospital death.
Results
The significant factors associated with systemic complications were older age (OR 1.38, 95% CI 1.09–1.74), a lower activity of daily living score upon admission (OR 1.52, 95%CI 1.19–1.94), atrial fibrillation (OR 2.14, 95%CI 1.25–3.65), renal failure (OR 2.29, 95%CI 1.25–4.20), and surgical procedure (AF, OR 1.73, 95%CI 1.35–2.22). The significant explanatory variables for in-hospital death were revealed to be male sex (OR 3.26, 95%CI 1.20–8.87), a lower body mass index (OR 3.97, 95%CI 1.23–12.86), unscheduled admission (OR 3.52, 95%CI 1.17–10.63), atrial fibrillation (OR 8.31, 95%CI 2.25–30.70), renal failure (OR 7.15, 95%CI 1.32-38.77), and schizophrenia (OR 8.23, 95%CI 1.66–42.02).
Conclusions
Atrial fibrillation and renal failure as preoperative comorbidities were common factors between perioperative systemic complications and mortality in elderly patients for OVF.
Similar content being viewed by others
Introduction
Thoracolumbar osteoporotic vertebral fractures (OVF) generally develop due to bone fragility, especially in elderly patients [1], and OVF are the most common type of fragile fractures [2]. The inducing mechanism of this type of fracture in elderly people is slight injury, such as a fall from a standing height [3]. OVF are deeply associated with difficulties in terms of activities of daily living (ADL) and poor quality of life (QOL) and high risks of hospitalization and mortality [4]. Due to the aging of the population, the prevalence of osteoporosis has increased markedly, resulting in increases in the number of patients with OVF [5, 6]. The increase in OVF and the subsequent high mortality will become serious socioeconomic problems [7].
OVF patients are usually prescribed conservative and nonsurgical treatments consisting of pain medication, bed rest, physiotherapy, and bracing, and most patients with OVF respond well to conservative management [8, 9]. This type of fracture occasionally requires operative treatment because of neurological dysfunction or kyphotic malalignment after severe vertebral collapse and/or instability [10, 11]. Several studies have investigated surgical methods for the treatment of OVF and the functional outcomes of each method [12, 13]. However, few studies have focused on perioperative complications with large sample sizes. As the surgical treatment of OVF generally has a high risk of complications due to the increase in age in the population with osteoporosis, it is quite important to clarify the detailed risk factors for systemic complications and mortality in patients undergoing surgery. Thus, in this study, we investigated a large national inpatient database that included numerous elderly patients undergoing surgical treatment for OVF and evaluated the perioperative complications, mortality, and risk factors.
Materials and methods
Data sources
The retrospective study was conducted using the diagnosis procedure combination (DPC), which was developed by the Ministry of Health, Labor and Welfare in Japan. All 82 academic and voluntary general hospitals in Japan participate in the database [14]. All patient data in this study were obtained from the multi-institutional DPC database as stated in previous literature [15,16,17,18]. This database contains the following items: age, sex, body mass index (BMI), smoking index, admission type, emergency transport, hospital type, ADL scores for admission and discharge by the Ministry of Health, surgical procedure, diagnosis with International Classification of Diseases, Tenth Revision (ICD-10) codes, comorbidities at admission and complications after admission, and in-hospital deaths. The database contains a separate registry of comorbidities at admission and postoperative complications. The institutional ethical committee at Tokyo Medical and Dental University permitted us to use all data in the DPC database.
Patient selection and data extraction
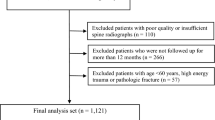
Patients over 65 years old and who were diagnosed with thoracic (ICD-10 code, S2200) or lumbar vertebral fracture (S3200) and osteoporosis (M800-805, 808-816, 818, 819) were eligible for inclusion in the DPC database. We selected patients who received operative treatment, either anterior fusion (AF, K142-1 according to the Japanese original surgical code; K-code) or posterior fusion (PF, K142-2), from April 1, 2012, to March 31, 2016. The use of anterior and posterior surgery upon the first admission was considered AF. Patients excluded from the current study were as follows: (1) patients less than 65 years of age, (2) patients without osteoporosis, (3) patients who received only vertebroplasty without spinal fusion (e.g., balloon kyphoplasty), (4) infectious spondylitis including pyogenic and tuberculosis, (5) metastatic or primary spinal tumors. Patient comorbidities at admission extracted in the current study were the following: diabetes mellitus (ICD-10 codes: E10-14), cardiovascular disease (I200, 201, 208-214, 219-221, 228, 229, 238), cardiac failure (I110, I500, 501, 509), atrial fibrillation (I48), hypertension (I10, 15), cerebrovascular disease (I614, 619, I630-639), chronic obstructive pulmonary disease (J441, 448, 449), pneumonia (J13, 14, 150-159, J180-182, 188, 189, J690, J958), renal failure (N17-19, N289, I120), hepatic failure (K704, 711, 719, 720, 729, 769), gastric ulcer and hemorrhage (K250-270, K279, K922), malignancy (C00-97), rheumatoid arthritis (M069), dementia (F000-002, 009, 010-012, 019, 03, G300-301, 308-309), depression (F313-315, 318-323, 328-334, 339), and schizophrenia (F200-209). Included perioperative systemic complications after admission were the following: cardiovascular disease, cardiac failure, atrial fibrillation, cerebrovascular disease, respiratory failure (J959-961, 969), pneumonia, dysphagia (K918, R13), renal failure, hepatic failure, gastric ulcer and hemorrhage, deep venous thrombosis (I801, 802, 828), pulmonary embolism (I269), sepsis (A394, 400-403, 409-415, 418, 419), delirium (F050, 051, 059), urinary tract infection (N390, T835), chylothorax (I898, S278, T812), hemothorax (J942, S271-272), pneumothorax (J930-931, 938-939, S270, T812), pleurisy (J90, R091, T812), and pyothorax (J869). We listed reoperations for systemic complications. The listed reoperations were as follows: cardiac (K codes; K538-605), vascular (K606-619, 621-623), pulmonary (K507-519), thoracic (K477-504), cerebral (K145-181), gastric (K520-533, 630-668), liver, gallbladder, pancreas (K669-709), and vena cava filter (K620), tracheoplasty (K403), or tracheostomy (K386).
Statistical analysis
First, all patients in this study were divided into either the perioperative systemic complications (+) or (−) group during hospitalization. In the two groups, we compared the following parameters: age, sex, BMI, smoking index, emergency transport, hospital type, ADL score upon admission, surgical procedure, and preoperative comorbidities between the complication (+) group and the complication (−) group. Fisher’s exact test and the chi-square test were used to compare proportions of categorical variables. All continuous variables were converted into categorical variables. We further performed multivariate logistic regression analysis to investigate the risk factors related to perioperative systemic complications using the explanatory variables that were significant in the univariate analysis as P < 0.05. Second, all patients in this study were also divided into either the in-hospital death (+) or (−) group. We similarly conducted univariate analysis to reveal the risk factors for hospital mortality in this study between the in-hospital death (+) group and the in-hospital death (−) group. Multivariate logistic regression analysis was also performed using the variables with P < 0.05 in the univariate analysis. All statistical analyses were performed with Stata/MP version 14 (StataCorp, College Station, TX, USA), and P < 0.05 was considered statistically significant. We also calculated variance inflation factor (VIF) for variables that seemed to influence each other (e.g., cardiac failure and atrial fibrillation), taking multicollinearity into account. As the VIF was below 10, we considered the effect of multicollinearity of the explanatory variables to be small.
Results
First, Table 1 describes whole demographics of total 2446 patients in this study. In total, the average age was 77.4 years old, BMI was 22.2 kg/m2, scheduled admission was 56.4%, emergency transport was 16.3%, and academic hospital was 5.4%. The common preoperative comorbidities were, in order of descending prevalence, hypertension (28.3%), diabetes mellitus (14.5%), and cardiovascular disease (5.6%).
Table 2 shows the demographics of all patients in terms of the perioperative systemic complications (+) or (−) group. Whole systemic complications were observed in 498 patients, which accounted for 20% of the total 2446 patients. The patients in the complication (+) group were characterized as follows: there were fewer elderly patients (over 85 years old, complication (+)/(−) group: 13.3%/11.6%, P < 0.001), more were unscheduled at admission (48.4%/42.4%, P = 0.016), they had a lower ADL score at admission (0 to 10 points: 47.8%/40.0%, P < 0.001), and more patients received AF (23.3%/16.4%, P < 0.001) (Table 2).
We also show the risk factors for perioperative systemic complications according to the multivariable analysis in Table 3. The significant factors proven to be associated with systemic complications were older age (75 to 84 years old, odds ratio [OR] 1.38, 95% confidence interval [CI] 1.09–1.74, P = 0.007), a lower ADL score upon admission (0 to 10 points, OR 1.52, 95%CI 1.19–1.94, P = 0.001), atrial fibrillation (OR 2.14, 95%CI 1.25–3.65, P = 0.006), renal failure (OR 2.29, 95%CI 1.25–4.20, P = 0.007), and surgical procedure (AF, OR 1.73, 95%CI 1.35–2.22, P < 0.001) (Table 3).
Figure 1 shows a list of systemic complications in this study. The incidence of systemic complications was approximately 20%, including gastrointestinal complications (6.1%), cardiovascular complications (2.8%), urinary tract infections (2.3%), and deep vein thrombosis (2.3%) (Fig. 1). We further listed reoperations for systemic complications in each organ (Additional Table 1).
Table 4 shows the demographic data for a total of 2446 patients, including 18 deceased patients. The patients in the in-hospital death (+) group had the following characteristics: there were more males (in-hospital death (+)/(−): 61.1%/24.6%, P < 0.001), they had a lower BMI (less than 18.5 kg/m2: 44.4%/14.0%, P = 0.001), more were unscheduled at admission (72.2%/43.4%, P = 0.014), more had cardiac failure (11.1%/3.1%, P = 0.009), more had atrial fibrillation (22.2%/2.4%, P < 0.001), more had renal failure (11.1%/1.9%, P = 0.006), and more had schizophrenia (11.1%/1.8%, P = 0.004) compared with patients in the in-hospital death (−) group (Table 4).
Finally, we demonstrate the risk factors for in-hospital death according to multivariable logistic regression analysis during hospitalization in Table 5. The significant explanatory variables revealed by this analysis were male sex (OR 3.26, 95%CI 1.20–8.87; P = 0.021), lower BMI (less than 18.5 kg/m2, OR 3.97, 95%CI 1.23–12.86, P = 0.021), unscheduled at admission (OR 3.52, 95%CI 1.17–10.63, P = 0.026), atrial fibrillation (OR 8.31, 95%CI 2.25–30.70, P = 0.001), renal failure (OR 7.15, 95%CI 1.32-38.77, P = 0.023), and schizophrenia (OR 8.23, 95%CI 1.66–42.02, P = 0.010) (Table 5).
In summary, the risk factors for perioperative systemic complications were high age, low ADL score, comorbidities of atrial fibrillation and renal failure, and anterior surgery. The risk factors for death during hospitalization were male, low BMI, unscheduled admission, comorbidities of atrial fibrillation, renal failure, and schizophrenia. Atrial fibrillation and renal failure were risk factors for both postoperative systemic complications and in-hospital death.
Discussion
We showed the risk factors for perioperative systemic complications and mortality in patients who underwent surgery for OVF using a large national inpatient database in Japan. The results obtained for the risk factors associated with systemic complications were older age, lower ADL score upon admission, atrial fibrillation, renal failure, and surgical procedure, i.e., AF. Moreover, we also revealed the risk factors significantly associated with in-hospital death for OVF: male sex, a lower BMI, unscheduled at admission, atrial fibrillation, renal failure, and schizophrenia. Among them, atrial fibrillation and renal failure were common factors for both mortality and perioperative systemic complications as preoperative comorbidities.
As shown in Table 3 and Fig. 2, age was found to be one of the risk factors for perioperative systemic complications. The incidence of systemic complications increased with age and was particularly pronounced with age over 75 years (Fig. 2). Hamel et al. reported that 20% of older patients who underwent major noncardiac surgery experienced one or more postoperative complications, which supports our results (498 cases of total 2446 cases, with an incidence rate of 20.4%) [19]. Recent studies on perioperative complications after spine surgery have suggested an association with sarcopenia [20] and poor nutritional status [21] in aged patients. These factors may also be associated with postoperative complications and mortality in surgeries for OVF, although they were not evident in the current study because of the lack of detailed information in the database.
The results of this study showed that preoperative ADL was significantly associated with postoperative systemic complications with an OR of 1.52. Patients with lower ADL levels are often unable to walk independently and thus need to move with wheelchairs or are even bedridden due to their leg pain, numbness, and/or paralysis before the surgery. This condition can be associated with various systemic complications during the perioperative period, such as pneumonia [22], urinary tract infections due to catheter use [23], and pulmonary embolism [24, 25]. Therefore, it is important to consider surgical intervention before the patient’s functioning and ADL are seriously deteriorated due to OVF and vertebral collapse.
Anterior fusion is an effective and reasonable method that can reconstruct the anterior column and decompress neural tissue in the spinal canal. However, anterior fusion is associated with serious perioperative systemic complications, including pulmonary embolism [26], urinary tract infection [27], and pleurisy. Anterior surgery generally necessitates longer operative times with large quantities of blood loss, which results in the demand for transfusion more than posterior surgery [26]. The use of blood transfusion after spinal surgery is associated with high risks of urinary tract infection and other types of infection owing to some immunological problems [27]. Furthermore, the anterior surgical approach for accessing the thoracolumbar spine sometimes injures the diaphragm [28] and pleura [29], and this type of injury can be closely associated with respiratory complications. In the aging population, postoperative respiratory disturbance is sometimes serious and life-threatening. Thus, less-invasive procedures such as vertebroplasty and/or posterior percutaneous pedicle screw fixation [30, 31] should be alternatively considered if applicable to the patient’s condition.
A previous study revealed that impaired renal function, in particular, an estimated glomerular filtration rate (eGFR) of < 60 mL/min/1.73 m2, was a significant predictor for mortality after vertebral fracture [32]. Puvanesarajah et al. reported that elderly patients suffering from renal disease treated with lumbar fusion had 5.0 times increased mortality within 90 days of surgery compared to the control group [33]. They presumed that advanced renal disease was deeply associated with experiencing pulmonary embolism, myocardial infarction, pneumonia, respiratory failure, or cerebrovascular accident, which can lead to in-hospital death. Regarding cardiac problems, Fineberg et al. demonstrated the association between cardiac complications and lumbar spine surgeries and that cardiac events resulted in increased lengths of hospitalization and mortality [34]. Patients with atrial fibrillation have a significantly higher risk of perioperative mortality than patients with coronary artery disease undergoing noncardiac surgeries [35]. Atrial fibrillation is profoundly pertinent to thromboembolic events, which may lead to fatal hemodynamic decompensation due to the dysfunction of correct atrial contraction [36]. For elderly OVF patients, atrial fibrillation may be particularly relevant to mortality and complication factors according to our results.
Nakano et al. further indicated that male sex and low nutritional status may cause increased mortality in vertebral fracture patients, even in addition to low renal function [32]. Their logic supports our results, as male sex and low BMI were associated with in-hospital systemic complication events and mortality in patients with OVF who underwent surgical treatment. Another study confirmed that serum albumin concentration, which can reflect patients’ nutritional condition and BMI, was a significant predictor of mortality in elderly patients with fractures [37]. In particular, they established that the cut-off BMI value was 18.9 kg/m2.
Concerning the relationship between mortality and schizophrenia, the average life expectancy of patients with schizophrenia has been reported to be shorter than that of the general population, and they have a mortality risk that is two to three times that of the general population [38]. Another study reported that the higher in-hospital mortality in patients with schizophrenia may have resulted from impaired access to and low-quality care for primary disease due to psychiatric problems and unmeasured physical factors other than psychiatric factors [39]. Interestingly, in regard to unscheduled admission, recent studies discovered the possibility of an increased risk of death associated with hospital admission on the weekend [40, 41]. Thomas et al. found that fracture patients were more likely to die as an inpatient when admitted on the weekend [40]. In another paper, patients admitted on the weekend were significantly less likely to receive early spinal intervention [42]. These findings suggest that increased mortality with weekend admission may be explained by limited orthopedic resources, reductions in medical staff in hospital wards, and decreased access to diagnostic tools [40].
This study has several limitations. This national database cannot reflect clinically important findings since the database system was diagnosed with coding using ICD-10 codes without radiological findings or laboratory data. For example, bone mineral density, mechanism and severity of injury, the neurologic condition-related Japanese Orthopedic Association score, the level of fusion, blood loss, and operation duration could not be verified in this database system. Any instances of mortality or perioperative complications after leaving the hospital could not be considered because the database only contains information during hospitalization. In addition, unmeasured confounding factors (e.g., surgeon experience) may have influenced the occurrence of systemic complications and in-hospital deaths. Further research would be needed using database that included more detailed information.
Even with these limitations, we ascertained the novel detailed predictors for surgically treated OVF patients in terms of mortality and perioperative systemic complications with a large national inpatient database.
Conclusions
We demonstrated the various risk factors related to perioperative systemic complications and in-hospital death in patients who underwent surgery for OVF using a large national inpatient database in Japan. Atrial fibrillation and renal failure as preoperative comorbidities were common factors between perioperative systemic complications and mortality. For patients at particularly high risk of complications, surgical indication should be carefully considered, and the efforts to minimize the perioperative complications are needed.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OVF:
-
Osteoporotic vertebral fractures
- ADL:
-
Activities of daily living
- QOL:
-
Quality of life
- DPC:
-
Diagnosis procedure combination
- BMI:
-
Body mass index
- ICD-10:
-
International classification of diseases, tenth revision
- AF:
-
Anterior fusion
- PF:
-
Posterior fusion
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- eGFR:
-
Estimated glomerular filtration rate
References
Arciero RA, Leung KY, Pierce JH. Spontaneous unstable burst fracture of the thoracolumbar spine in osteoporosis. A report of two cases. Spine (Phila Pa 1976). 1989;14:114–7.
Genant HK, Cooper C, Poor G, Reid I, Ehrlich G, Kanis J, et al. Interim report and recommendations of the World Health Organization Task-Force for Osteoporosis. Osteoporos Int. 1999;10:259–64.
Wasfie T, Jackson A, Brock C, Galovska S, McCullough JR, Burgess JA. Does a fracture liaison service program minimize recurrent fragility fractures in the elderly with osteoporotic vertebral compression fractures? Am J Surg. 2019;217:557–60.
Wáng YXJ, Che-Nordin N, Deng M, Leung JCS, Kwok AWL, He LC, et al. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int. 2019;30:897–905.
Kato T, Inose H, Ichimura S, Tokuhashi Y, Nakamura H, Hoshino M, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med. 2019;8:198. https://doi.org/10.3390/jcm8020198.
Li M, Law S, Cheng J, Kee H, Wong MS. A comparison study on the efficacy of SpinoMed®and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int. 2015;39:270–6.
Lee Y-K, Jang S, Jang S, Lee HJ, Park C, Ha Y-C, et al. Mortality after vertebral fracture in Korea. Osteoporos Int. 2012;23:1859–65.
Song D, Meng B, Gan M, Niu J, Li S, Chen H, et al. The incidence of secondary vertebral fracture of vertebral augmentation techniques versus conservative treatment for painful osteoporotic vertebral fractures: a systematic review and meta-analysis. Acta radiol. 2015;56:970–9.
Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the Medicare population. J Bone Miner Res. 2011;26:1617–26.
Abbasi Fard S, Skoch J, Avila MJ, Patel AS, Sattarov KV, Walter CM, et al. Instability in thoracolumbar trauma: is a new definition warranted? Clin spine Surg. 2017;30:E1046–9.
Lin CL, Chou PH, Fang JJ, Huang KY, Lin RM. Short-segment decompression and fixation for thoracolumbar osteoporotic fractures with neurological deficits. J Int Med Res. 2018;46:3104–13.
Sudo H, Ito M, Kaneda K, Abumi K, Kotani Y, Nagahama K, et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 2013;13:1726–32.
Uchida K, Nakajima H, Yayama T, Miyazaki T, Hirai T, Kobayashi S, et al. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine. 2010;13:612–21.
Fujiogi M, Michihata N, Matsui H, Fushimi K, Yasunaga H, Fujishiro J. Outcomes following laparoscopic versus open surgery for pediatric inguinal hernia repair: analysis using a national inpatient database in Japan. J Pediatr Surg. 2019;54:577–81.
Oichi T, Oshima Y, Matsui H, Fushimi K, Tanaka S, Yasunaga H. Can elective spine surgery be performed safely among nonagenarians? Spine (Phila Pa 1976). 2019;44:E273–81.
Kumamaru KK, Kumamaru H, Yasunaga H, Matsui H, Omiya T, Hori M, et al. Large hospital variation in the utilization of post-procedural CT to detect pulmonary embolism/deep vein thrombosis in patients undergoing total knee or hip replacement surgery: Japanese nationwide diagnosis procedure combination database study. Br J Radiol. 2019:92. https://doi.org/10.1259/bjr.20180825 Epub 2019 Mar 15.
Takada D, Kunisawa S, Fushimi K, Imanaka Y. Previously-initiated hemodialysis as prognostic factor for in-hospital mortality in pneumonia patients with stage 5 chronic kidney disease: retrospective database study of Japanese hospitals. PLoS One. 2019;14:e0213105. https://doi.org/10.1371/journal.pone.0213105 eCollection 2019.
Morishita S, Yoshii T, Okawa A, Fushimi K, Fujiwara T. Perioperative complications of anterior decompression with fusion versus laminoplasty for the treatment of cervical ossification of the posterior longitudinal ligament: propensity score matching analysis using a nation-wide inpatient database. Spine J. 2019;19:610–6.
Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: Morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53:424–9.
Bokshan SL, Han AL, De Passe JM, Eltorai AEM, Marcaccio SE, Palumbo MA, et al. Effect of sarcopenia on postoperative morbidity and mortality after thoracolumbar spine surgery. Orthopedics. 2016;39:e1159–64.
Puvanesarajah V, Jain A, Kebaish K, Shaffrey CI, Sciubba DM, De La Garza-Ramos R, et al. Poor nutrition status and lumbar spine fusion surgery in the elderly. Spine (Phila Pa 1976). 2017;42:979–83.
Bohl DD, Saltzman BM, Sershon RA, Darrith B, Okroj KT, Della Valle CJ. Incidence, risk factors, and clinical implications of pneumonia following total hip and knee arthroplasty. J Arthroplasty. 2017;32:1991–5.
Tominaga H, Setoguchi T, Ishidou Y, Nagano S, Yamamoto T, Komiya S. Risk factors for surgical site infection and urinary tract infection after spine surgery. Eur Spine J. 2016;25:3908–15.
Shem K. Phlegmasia cerulea dolens: Rare complication of vena cava filter placement in man with paraplegia. J Spinal Cord Med. 2008;31:398–402.
Masuda K, Chikuda H, Yasunaga H, Hara N, Horiguchi H, Matsuda S, et al. Factors affecting the occurrence of pulmonary embolism after spinal surgery: data from the national administrative database in Japan. Spine J. 2012;12:1029–34.
Kim HJ, Kepler C, Cunningham M, Rawlins B, Boachie-Adjei O. Pulmonary embolism in spine surgery: a comparison of combined anterior/posterior approach versus posterior approach surgery. Spine (Phila Pa 1976). 2011;36:177–9.
Kato S, Chikuda H, Ohya J, Oichi T, Matsui H, Fushimi K, et al. Risk of infectious complications associated with blood transfusion in elective spinal surgery-a propensity score matched analysis. Spine J. 2016;16:55–60.
Shi J, Yue X, Niu N, Zhao C, Qiu H, Wang Z. Application of a modified thoracoabdominal approach that avoids cutting open the costal portion of diaphragm during anterior thoracolumbar spine surgery. Eur Spine J. 2017;26:1852–61.
Theologis AA, Tabaraee E, Toogood P, Kennedy A, Birk H, McClellan RT, et al. Anterior corpectomy via the mini-open, extreme lateral, transpsoas approach combined with short-segment posterior fixation for single-level traumatic lumbar burst fractures: analysis of health-related quality of life outcomes and patient satisfaction. J Neurosurg Spine. 2016;24:60–8.
Niu J, Song D, Gan M, Liu B, Tan C, Yang H, et al. Percutaneous kyphoplasty for the treatment of distal lumbosacral pain caused by osteoporotic thoracolumbar vertebral fracture. Acta radiol. 2018;59:1351–7.
Zhao Q, Zhang H, Hao D, Guo H, Wang B, He B. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore). 2018;97:e11560.
Nakano T, Kuwabara A, Mizuta H, Tanaka K. Contribution of hypoalbuminemia and decreased renal function to the increased mortality after newly diagnosed vertebral fracture in Japanese subjects. Asia Pac J Clin Nutr. 2016;25:472–7.
Puvanesarajah V, Jain A, Hess DE, Shimer AL, Shen FH, Hassanzadeh H. Complications and mortality after lumbar spinal fusion in elderly patients with late stage renal disease. Spine (Phila Pa 1976). 2016;41:E1298–302.
Fineberg SJ, Ahmadinia K, Patel AA, Oglesby M, Singh K. Incidence and mortality of cardiac events in lumbar spine surgery. Spine (Phila Pa 1976). 2013;38:1422–9.
van Diepen S, Bakal JA, McAlister FA, Ezekowitz JA. Mortality and readmission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery. Circulation. 2011;124:289–96.
Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–64.
Miyanishi K, Jingushi S, Torisu T. Mortality after hip fracture in Japan: the role of nutritional status. J Orthop Surg (Hong Kong). 2010;18:265–70.
Brown S, Kim M, Mitchell C, Inskip H. Twenty-five year mortality of a community cohort with schizophrenia. Br J Psychiatry. 2010;196:116–21.
Ishikawa H, Yasunaga H, Matsui H, Fushimi K, Kawakami N. Differences in cancer stage, treatment and in-hospital mortality between patients with and without schizophrenia: retrospective matched-pair cohort study. Br J Psychiatry. 2016;208:239–44.
Thomas CJ, Smith RP, Uzoigwe CE, Braybrooke JR. The weekend effect. Bone Joint J. 2014;96-B:373–8.
Isogai T, Yasunaga H, Matsui H, Tanaka H, Ueda T, Horiguchi H, et al. Effect of weekend admission for acute myocardial infarction on in-hospital mortality: a retrospective cohort study. Int J Cardiol. 2015;179:315–20.
Dasenbrock HH, Pradilla G, Witham TF, Gokaslan ZL, Bydon A. The impact of weekend hospital admission on the timing of intervention and outcomes after surgery for spinal metastases. Neurosurgery. 2012;70:586–93.
Acknowledgements
Not applicable.
Funding
This work was supported by no funding.
Author information
Authors and Affiliations
Contributions
SM participated in the data collection, the data analysis and manuscript preparation, TY participated in the study design, the data collection, the data analysis and manuscript preparation. AO, HI, TH, MY, and KF participated in the data collection and data analysis. TF participated in the study design and manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was approved by the review board of Tokyo Medical and Dental University. The informed consent was not obtained for each patient, because all data in this study were completely anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
(XLS 28 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Morishita, S., Yoshii, T., Okawa, A. et al. Risk factors related to perioperative systemic complications and mortality in elderly patients with osteoporotic vertebral fractures—analysis of a large national inpatient database. J Orthop Surg Res 15, 518 (2020). https://doi.org/10.1186/s13018-020-02050-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-020-02050-5