Abstract
Background
The surgical treatment of end-stage tibiotalar arthritis continues to be a controversial topic. Advances in surgical technique and implant design have lead to improved outcomes after both ankle arthrodesis (AA) and total ankle arthroplasty (TAA), yet a clear consensus regarding the most ideal form of treatment is lacking. In this study, the outcomes and complications following AA and TAA are compared in order to improve our understanding and decision-making for care and treatment of symptomatic tibiotalar arthritis.
Methods
Studies reporting on outcomes and complications following TAA or AA were obtained for review from the PubMed database between January 2006 and July 2016. Results from studies reporting on a minimum of 200 total ankle arthroplasties or a minimum of 80 ankle arthrodesis procedures were reviewed and pooled for analysis. All studies directly comparing outcomes and complications between TAA and AA were also included for review. Only studies including modern third-generation TAA implants approved for use in the USA (HINTEGRA, STAR, Salto, INBONE) were included.
Results
A total of six studies reporting on outcomes following TAA and five reporting on outcomes following AA met inclusion criteria and were included for pooled data analysis. The adjusted overall complication rate was higher for AA (26.9%) compared to TAA (19.7%), with similar findings in the non-revision reoperation rate (12.9% for AA compared to 9.5% for TAA). The adjusted revision reoperation rate for TAA (7.9%) was higher than AA (5.4%). Analysis of results from ten studies directly comparing TAA to AA suggests a more symmetric gait and less impairment on uneven surfaces after TAA.
Conclusions
Pooled data analysis demonstrated a higher overall complication rate after AA, but a higher reoperation rate for revision after TAA. Based on the existing literature, the decision to proceed with TAA or AA for end-stage ankle arthritis should be made on an individual patient basis.
Similar content being viewed by others
Background
End-stage arthritis of the tibiotalar joint is a disabling condition that causes substantial functional impairment and decreased quality of life [1]. The most common etiology is post-traumatic arthritis, with other causes including rheumatoid arthritis, idiopathic arthritis, neuropathic arthritis, osteonecrosis, hemophilic arthritis, septic arthritis, and gout [2]. Total ankle arthroplasty (TAA) and ankle arthrodesis (AA) are the two primary surgical options for patients who fail conservative measures.
Ankle arthrodesis has long been considered the gold standard for treatment of end-stage arthritis. Critics of arthrodesis, however, cite high complication rates and altered function as reasons to justify alternative forms of joint-sparing treatment [3]. For example, nonunion rates as high as 43% in some high-risk sub-groups have been reported after ankle arthrodesis [4]. There is also concern that elimination of tibiotalar motion accelerates adjacent joint degeneration due to the loss of a major motion segment [5, 6]. Still, despite successful arthrodesis, loss of normal ankle motion has been shown to negatively affect functional status at long-term follow-up [7]. Greater attention to soft tissue management and newer fixation options has resulted in fewer complications, higher fusion rates, and more predictable pain relief [8,9,10,11,12].
Total ankle arthroplasty was developed as an alternative to ankle arthrodesis. While first-generation implants were fraught with unacceptably high complication rates, current third-generation designs have led to more favorable outcomes [13,14,15,16,17,18,19]. Still, long-term survivorship of third-generation implants remains unknown. Proponents of TAA believe the advent of current generation designs and refined surgical techniques have the potential to offer long-term outcomes equivalent to that of arthrodesis, with benefits including preservation of ankle motion, improved gait, and preservation of adjacent joints.
The majority of existing studies comparing AA to TAA show equivocal or conflicting results. In addition, many of these studies focus on older techniques and early generation implants, which further complicate interpretation of the literature. The purpose of this study is to compare the outcomes of AA and TAA using pooled results from studies published in the past 10 years that include only modern third-generation TAA implants.
Methods
Search strategy
An electronic search for publications available in the English language from January 2006 to July 2016 using the PubMed database was performed. The keywords used included “ankle arthritis,” “tibiotalar,” “ankle arthroplasty,” and “ankle arthrodesis.” Two independent authors (CL and BB) reviewed all abstracts from the PubMed search results. This was supplemented with a manual review of references in all review articles and primary full-text studies identified in the PubMed database to verify the inclusion of all relevant publications. Our literature search decision flow chart for study inclusion is depicted in Fig. 1.
Total ankle arthroplasty study selection
Eligibility for study inclusion from the PubMed database search was assessed independently by two different authors (CL and BB). The review sought to identify primary research reporting outcomes and complications from third-generation total ankle arthroplasty designs approved for use in the USA (HINTEGRA, STAR, Salto, INBONE). Articles with a minimum of 200 ankles reporting complication, reoperation, and/or revision data were included for analysis in this review. Exclusion criteria included studies published prior to January 2006; abstracts, review articles, and surgical technique articles which did not report primary research outcomes; use of implants other than one of the four third-generation implants listed above; publications reporting only on restricted patient cohorts selected from a larger and more generalizable population; and studies reporting on revision TAA (Table 1).
Ankle arthrodesis study selection
A similar identification and screening strategy was used to analyze the PubMed database search results for ankle arthrodesis publications. The review sought to identify primary research reporting outcomes and complications for ankle arthrodesis. Studies with a minimum of 80 ankles reporting complication, reoperation, and/or revision data were included for analysis in this review. A cutoff of 80 ankles was chosen to identify studies reporting on larger cohorts with a goal of identifying a similar number of articles to use for comparison to the TAA articles in pooled data analysis. Exclusion criteria included studies published prior to January 2006; abstracts, review articles, and surgical technique articles which do not report primary research outcomes; articles reporting only on restricted patient cohorts selected from a larger and more generalizable population; and studies reporting solely on fusion accomplished with external fixation techniques or revision AA (Table 1).
Total ankle arthroplasty versus ankle arthrodesis study selection
A similar identification and screening strategy was used to analyze the PubMed database search results for publications reporting data directly comparing TAA to AA. The review sought to identify primary research reporting data directly comparing an AA cohort to a cohort of patients treated with a third-generation total ankle arthroplasty design approved for use in the USA. There was no cutoff for minimum number of ankles or data reported for inclusion in this review to provide a more comprehensive analysis of the literature directly comparing the two treatment options. Exclusion criteria included studies published prior to January 2006; abstracts, review articles, and surgical technique articles which do not report primary research outcomes; use of implants other than one of the four third-generation implants described above; and studies reporting on revision TAA or AA (Table 1).
Data collection and analysis
The total ankle arthroplasty and ankle arthrodesis studies included for analysis in this review can be seen in Table 1. Demographic information including study design, recruitment period, number of ankles, TAA prosthesis or AA operative technique, mean follow-up, and mean patient age was collected. The totals and adjusted means were then reported. Adjusted means were calculated for mean follow-up and mean age in the TAA and AA studies by summing each studies’ mean follow-up or mean age multiplied by the number of ankles in their study and dividing this sum by the total number of ankles in all studies reporting the variable of interest.
Complications, non-revision reoperations, and revisions were recorded for each study as seen in Table 2. There was significant heterogeneity between studies with respect to reporting complications. When a complication of interest, non-revision reoperation rate, or revision rate was not explicitly stated within an article, attempts were made to calculate these rates using data reported in the study. The studies reviewed did not consistently report on all of the same types of complications. Therefore, an adjusted rate was calculated by taking the number of specific complications divided by the sum of all cases for only those studies reporting the outcome of interest. Perioperative and postoperative fractures were combined in our analysis and reported as an overall fracture rate. During interpretation of revision rates, revision of TAA was defined as removal of either the tibial or talar component or both components with subsequent placement of an antibiotic spacer, reimplantation of metal components, conversion to an arthrodesis, or amputation. Revision of AA was defined as return to the operating room for a revision fusion in the setting of a nonunion.
Studies comparing TAA to AA included for analysis in this review can be seen in Table 3. Demographic information was collected including study design, number of ankles, TAA prosthesis or AA operative technique, mean and/or minimum follow-up, outcome measures used, and major study conclusions.
Results
Total ankle arthroplasty
There were six studies that met the inclusion criteria for pooled data analysis of outcomes after total ankle arthroplasty (Table 2) [14,15,16,17,18,19]. Five of the studies were prospective and one was retrospective. The studies report on a total of 2239 ankles operated on from 1993 to 2013. INBONE was used in 682 ankles, STAR in 455 ankles, Salto in 380 ankles, and HINTEGRA in 722 ankles. The adjusted mean follow-up was 4.8 years (range 3.3–7.3 years). The mean patient age at the time of arthroplasty was 61.3 years (range 56.8–63.2 years).
Ankle arthrodesis
A total of five studies met the inclusion criteria for pooled data analysis of outcomes after ankle arthrodesis (Table 2) [8,9,10,11,12]. All studies were retrospective in nature. The studies report on a total of 635 ankles operated on from 1993 to 2013. Arthrodesis was preformed through an open approach in 577 ankles and through an arthroscopic approach in 58 ankles. Three of the studies reported mean follow-up with an adjusted mean follow-up of 4.3 years (range 3.5–5.9 years). The mean patient age at the time of arthrodesis was 53.4 years (range 49–56.1 years).
Complications, reoperations, and revisions
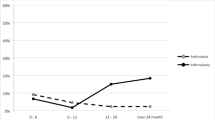
Table 3 lists the complication, reoperation, and revision rates in the selected studies. The most frequently reported complication in the arthroplasty group was aseptic loosening (5.8%), followed by wound complications (5.4%), fracture (4.9%), and deep infection (0.9%). Patients who underwent arthrodesis experienced mainly wound complications (9.8%), followed by nonunion (7.9%), deep infection (3.6%), and fracture (0.8%). Overall complication rate was reported in two arthroplasty studies with a mean rate of 19.7% compared to a mean of 26.9% reported in four arthrodesis studies. The pooled mean non-revision reoperation rate was higher in the arthrodesis studies (12.9%) compared to the arthroplasty studies (9.5%). Revision rate was higher in the arthroplasty group (7.9%) compared to the arthrodesis group (5.4%). Kaplan-Meier survivorship analysis was reported in four of the arthroplasty studies as seen in Table 3.
Total ankle arthroplasty versus ankle arthrodesis
There were ten studies that met the inclusion criteria for direct comparison of total ankle arthroplasty to ankle arthrodesis (Table 4) [20,21,22,23,24,25,26,27,28,29]. Three studies were prospective and seven were retrospective. The number of ankles included in the studies ranged from 36 to 672 ankles. The total ankle prosthesis and arthrodesis techniques used for each study are listed in Table 4.
Gait analysis was compared in seven studies. Two reported no significant difference between the TAA and AA cohorts [20, 22]. The remaining five studies found that patients performed better on gait analysis after TAA [21, 23,24,25, 29]. Clinical outcomes were collected in six studies [20, 23, 25,26,27,28]. Jastifer et al. reported improved Beuchel-Pappas scale (p = 0.036) and AOFAS (p = 0.03) in the TAA cohort over the AA cohort [23]. Saltzman et al. reported significantly greater efficacy (p < 0.001) and overall success (p < 0.001) in the Pivotal STAR group over the AA group [26]. Saltzman et al. reported improved outcome in TAA over AA for SF-36 MCS (p = 0.011) and AOS-pain scale (p = 0.001) [27]. The remaining three studies reported no significant difference in clinical outcomes between study cohorts. Two studies reported on radiographic outcomes showing no significant difference between TAA and AA in adjacent joint arthritis at the final follow-up [20, 27].
Discussion
End-stage arthritis of the tibiotalar joint is a disabling condition resulting in decreased functionality and quality of life [1]. Ankle arthrodesis has traditionally been considered the gold standard surgical option for tibiotalar arthritis, but total ankle arthroplasty is emerging as a viable alternative for certain patient cohorts. Over the past few decades, improved surgical techniques in AA and advancements in TAA prosthesis design have led to improved outcomes with both procedures. Many of the existing studies reporting outcomes following AA and TAA focus on outdated techniques and older generation TAA implants. This review focused on outcomes following AA and TAA with modern techniques and third-generation TAA implants.
Analysis of pooled data revealed that the overall complication rate of AA (26.9%) was higher than that of TAA (19.7%), as seen in Table 3. Issues with wound healing were the most common complication reported after AA (9.8%), followed by nonunion (7.9%) and deep infection (3.6%). The adjusted rate of deep infection after TAA was 0.9%, with fractures being the most infrequent complication seen in the AA cohort at 0.8%. The most frequent complication in the TAA studies was aseptic loosening with an adjusted rate of 5.8%, followed by wound complications (5.4%) and fracture (4.9%).
The adjusted non-revision reoperation rate was also higher for AA (12.9 versus 9.5%). Chalayon et al. reported on 215 ankle fusions with the most common reason for non-revision reoperation being hardware removal (6%) followed by incision and drainage for presumed infection (5%) [8]. Nielsen et al. reported on 107 ankle fusions and demonstrated reoperation rates similar to Chalayon et al., with hardware removal (21%) and incision and drainage for deep infection (3%) as the most common reasons for non-revision reoperation [11]. The two TAA studies with the highest non-revision reoperation rates did not provide detailed analysis of their indications for reoperation [15, 16].
The adjusted revision rate, however, was higher for TAA (7.9%) compared to AA (5.4%). In their study, Wood et al. reported a 12% revision rate for a cohort of 200 total ankles with a mean follow-up of 7.3 years. The majority of patients required revision for aseptic loosening (7%) [19]. Chalayon et al. reported a 7.4% revision rate in an AA cohort of 215 ankles, primarily for nonunion [8].
Studies directly comparing TAA to AA reported a wide range of outcome measures. Seven studies comparing the two treatments examined gait analysis. Common findings included improved walking ability upstairs, downstairs, and on uneven surfaces. Most notably, patients who received a TAA demonstrated a more symmetric gait compared to those who underwent AA.
Only two studies examined adjacent joint degeneration after surgical treatment. Braito et al. discussed radiographic findings in 101 TAA patients and 40 AA patients concluding an increase in degeneration of adjacent joints following both TAA and AA with no significant difference between the two cohorts at a mean observation period of 4.2 years in the TAA group and 3.4 years in the AA group [20]. Saltzman et al. found similar results on radiographic analysis, concluding no significant difference in the change of adjacent joint arthritis between the TAA and AA cohorts [27].
Arthroscopic ankle arthrodesis has the advantage of achieving fusion with less soft tissue dissection than what is required with open arthrodesis techniques, with the literature reporting promising initial outcome data. Myerson and Quill reported a retrospective study comparing open and arthroscopic arthrodesis concluding a shorter time to fusion in the arthroscopic group [30]. O’Brien et al. reported a retrospective study demonstrating similar fusion rates with less morbidity, shorter operative times, and shorter hospital stays with arthroscopic fusion [31]. Arthroscopic ankle arthrodesis has gained increasing popularity over the past decade [32, 33]. In a recent study, Duan et al. reported a wound complication rate of 1.5% in 68 arthroscopic ankle fusions, which is much less than the adjusted wound complication seen in this study [34]. As arthroscopic fusion techniques continue to develop, the potential for improved fusion rates with fewer complications in fusion cohorts may be seen; however, more large quality outcome studies are needed.
Terrell et al. assessed practice patterns in TAA and AA in the USA, reporting an increase in the percent of TAA cases performed between 2004 and 2009 [35]. The growing popularity of TAA combined with the higher failure rates, especially at long-term follow-up, are resulting in an increasing number of TAA patients requiring revision fusion procedure. Salvage fusion for failed TAA presents challenges of bone loss and poor soft tissue envelope quality when compared to primary fusion patients. As a result, salvage arthrodesis for failed TAA has shown worse outcomes over those seen after primary fusion [36, 37]. This should be considered when deciding between TAA and AA for the treatment of tibiotalar arthritis.
Previously published systematic reviews comparing results following TAA to AA are limited, largely focusing on clinical outcomes and revision rates. Jordan et al. concluded that a few studies report functional improvement following TAA over AA; however, the lack of high-quality evidence limits a definitive conclusion on which treatment is superior [38]. Haddad et al. report a 7% revision rate following TAA compared to 9% following AA [39]. van Heiningen et al. found a similar revision rate with TAA compared to AA (11 versus 12%) in rheumatoid arthritis patients, concluding both interventions show clinical improvement, with neither procedure showing superior outcomes [40]. Our current review focuses on modern techniques and implant designs to more accurately compare the current status of these treatment options.
The current literature does not support significant advantages of one procedure over the other in the general population. Knowledge of each procedure perioperative complication profile is important to help guide treatment recommendations, which should be made on a case-by-case basis. Appropriate patient selection plays a key role in successful treatment, where one method might be preferred over the other for specific case conditions. Krause et al. suggest age less than 50 years old, arthritis secondary to trauma or neuromuscular disease, unilateral ankle arthritis, ankle range of motion less than 10 degrees, absence of arthritis in adjacent joints, severe ankle instability, and coronal deformity greater than 15 degrees as major criteria to consider and suggest AA is the favored treatment in such cases [41].
The authors acknowledge that the present study is not without limitation. Foremost, this study was limited by the lack of randomized controlled trials published in the current literature on outcomes after TAA and AA. In addition, existing studies present significant clinical heterogeneity making comparison difficult. It should be noted that our ankle fusion studies included both open and arthroscopic techniques. Studies have reported improved fusion rates and lower complication rates with arthroscopic fusion; however, this was not a focus in our current study and therefore was not separated in our analysis of complications, reoperations, and revision for the fusion studies. Further, variations existed pertaining to the manner in which outcomes, complications, and revisions were reported. Various complications were inconsistently reported, with definitions of non-revision reoperation and implant failure differing between studies. Lastly, differences in length of follow-up and lack of consistent long-term follow-up likely underestimate the true complication and failure rates reported.
Conclusions
Total ankle arthroplasty and ankle arthrodesis are two surgical treatment options for end-stage tibiotalar arthritis supported in the literature. Currently, there is a lack of high-quality randomized controlled trials comparing these treatments in their modern form, utilizing current techniques and implant designs. The cohort studies and case series identified by this review were difficult to interpret as a whole due to heterogeneous populations and inconsistent reporting of complications and outcomes. However, pooled analysis of the data suggests that although AA may have a higher total complication rate, TAA may have a higher revision rate. Therefore, until a greater degree of current data is available demonstrating a significant advantage between the two treatment options, the decision to proceed with TAA or AA should be made on a case-by-case basis, accounting for appropriate patient selection, discussions regarding pros and cons of each treatment choice, and knowledge of perioperative complication profiles with each procedure. Individual patient goals, expectations, and understanding of the differences between the respective treatment options are vital to guide the decision between treatment with TAA or AA.
Abbreviations
- AA:
-
Ankle arthrodesis
- TAA:
-
Total ankle arthroplasty
References
Saltzman CL, Zimmerman MB, O’Rourke M, Brown TD, Buckwalter JA, Johnston R. Impact of comorbidities on the measurement of health in patients with ankle osteoarthritis. J Bone Joint Surg Am. 2006;88:2366–72.
Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–6.
Raikin SM. Arthrodesis of the ankle: arthroscopic, mini-open, and open techniques. Foot Ankle Clin. 2003;8:347–59.
Frey C, Halikus NM, Vu-Rose T, Ebramzadeh E. A review of ankle arthrodesis: predisposing factors to nonunion. Foot Ankle Int. 1994;15:581–4.
Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83-A:219–28.
Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg (Br). 2003;85:994–8.
Muir DC, Amendola A, Saltzman CL. Long-term outcome of ankle arthrodesis. Foot Ankle Clin. 2002;7:703–8.
Chalayon O, Wang B, Blankenhorn B, Jackson 3rd JB, Beals T, Nickisch F, Saltzman CL. Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int. 2015;36:1170–9.
Gordon D, Zicker R, Cullen N, Singh D. Open ankle arthrodeses via an anterior approach. Foot Ankle Int. 2013;34:386–91.
Zwipp H, Rammelt S, Endres T, Heineck J. High union rates and function scores at midterm followup with ankle arthrodesis using a four screw technique. Clin Orthop Relat Res. 2010;468:958–68.
Nielsen KK, Linde F, Jensen NC. The outcome of arthroscopic and open surgery ankle arthrodesis: a comparative retrospective study on 107 patients. Foot Ankle Surg. 2008;14:153–7.
Muckley T, Hofmann G, Buhren V. Tibiotalar arthrodesis with the tibial compression nail. Eur J Trauma Emerg Surg. 2007;33:202–13.
Gougoulias NE, Khanna A, Maffulli N. History and evolution in total ankle arthroplasty. Br Med Bull. 2009;89:111–51.
Gross CE, Lampley A, Green CL, DeOrio JK, Easley M, Adams S, Nunley 2nd JA. The effect of obesity on functional outcomes and complications in total ankle arthroplasty. Foot Ankle Int. 2016;37:137–41.
Demetracopoulos CA, Adams Jr SB, Queen RM, DeOrio JK, Nunley 2nd JA, Easley ME. Effect of age on outcomes in total ankle arthroplasty. Foot Ankle Int. 2015;36:871–80.
Lewis Jr JS, Green CL, Adams Jr SB, Easley ME, DeOrio JK, Nunley JA. Comparison of first- and second-generation fixed-bearing total ankle arthroplasty using a modular intramedullary tibial component. Foot Ankle Int. 2015;36:881–90.
Barg A, Zwicky L, Knupp M, Henninger HB, Hintermann B. HINTEGRA total ankle replacement: survivorship analysis in 684 patients. J Bone Joint Surg Am. 2013;95:1175–83.
Schenk K, Lieske S, John M, Franke K, Mouly S, Lizee E, Neumann W. Prospective study of a cementless, mobile-bearing, third generation total ankle prosthesis. Foot Ankle Int. 2011;32:755–63.
Wood PL, Prem H, Sutton C. Total ankle replacement: medium-term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg (Br). 2008;90:605–9.
Braito M, Dammerer D, Kaufmann G, Fischler S, Carollo J, Reinthaler A, Huber D, Biedermann R. Are our expectations bigger than the results we achieve? A comparative study analysing potential advantages of ankle arthroplasty over arthrodesis. Int Orthop. 2014;38:1647–53.
Chopra S, Rouhani H, Assal M, Aminian K, Crevoisier X. Outcome of unilateral ankle arthrodesis and total ankle replacement in terms of bilateral gait mechanics. J Orthop Res. 2014;32:377–84.
Flavin R, Coleman SC, Tenenbaum S, Brodsky JW. Comparison of gait after total ankle arthroplasty and ankle arthrodesis. Foot Ankle Int. 2013;34:1340–8.
Jastifer J, Coughlin MJ, Hirose C. Performance of total ankle arthroplasty and ankle arthrodesis on uneven surfaces, stairs, and inclines: a prospective study. Foot Ankle Int. 2015;36:11–7.
Piriou P, Culpan P, Mullins M, Cardon JN, Pozzi D, Judet T. Ankle replacement versus arthrodesis: a comparative gait analysis study. Foot Ankle Int. 2008;29:3–9.
Rouhani H, Favre J, Aminian K, Crevoisier X. Multi-segment foot kinematics after total ankle replacement and ankle arthrodesis during relatively long-distance gait. Gait Posture. 2012;36:561–6.
Saltzman CL, Mann RA, Ahrens JE, Amendola A, Anderson RB, Berlet GC, Brodsky JW, Chou LB, Clanton TO, Deland JT, et al. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. 2009;30:579–96.
Saltzman CL, Kadoko RG, Suh JS. Treatment of isolated ankle osteoarthritis with arthrodesis or the total ankle replacement: a comparison of early outcomes. Clin Orthop Surg. 2010;2:1–7.
Schuh R, Hofstaetter J, Krismer M, Bevoni R, Windhager R, Trnka HJ. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop. 2012;36:1207–14.
Singer S, Klejman S, Pinsker E, Houck J, Daniels T. Ankle arthroplasty and ankle arthrodesis: gait analysis compared with normal controls. J Bone Joint Surg Am. 2013;95:e191. 191-110.
Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res. 1991:84–95.
O’Brien TS, Hart TS, Shereff MJ, Stone J, Johnson J. Open versus arthroscopic ankle arthrodesis: a comparative study. Foot Ankle Int. 1999;20:368–74.
Townshend D, Di Silvestro M, Krause F, Penner M, Younger A, Glazebrook M, Wing K. Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Joint Surg Am. 2013;95:98–102.
Gougoulias NE, Agathangelidis FG, Parsons SW. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007;28:695–706.
Duan X, Yang L, Yin L. Arthroscopic arthrodesis for ankle arthritis without bone graft. J Orthop Surg Res. 2016;11:154.
Terrell RD, Montgomery SR, Pannell WC, Sandlin MI, Inoue H, Wang JC, SooHoo NF. Comparison of practice patterns in total ankle replacement and ankle fusion in the United States. Foot Ankle Int. 2013;34:1486–92.
Kamrad I, Henricson A, Magnusson H, Carlsson A, Rosengren BE. Outcome after salvage arthrodesis for failed total ankle replacement. Foot Ankle Int. 2016;37:255–61.
Gross C, Erickson BJ, Adams SB, Parekh SG. Ankle arthrodesis after failed total ankle replacement: a systematic review of the literature. Foot Ankle Spec. 2015;8:143–51.
Jordan RW, Chahal GS, Chapman A. Is end-stage ankle arthrosis best managed with total ankle replacement or arthrodesis? A systematic review. Adv Orthop. 2014;2014:986285.
Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89:1899–905.
van Heiningen J, Vliet Vlieland TP, van der Heide HJ. The mid-term outcome of total ankle arthroplasty and ankle fusion in rheumatoid arthritis: a systematic review. BMC Musculoskelet Disord. 2013;14:306.
Krause FG, Schmid T. Ankle arthrodesis versus total ankle replacement: how do I decide? Foot Ankle Clin. 2012;17:529–43.
Acknowledgements
Not applicable.
Funding
There was no funding provided in conjunction with this manuscript.
Availability of data and materials
Not applicable.
Authors’ contributions
CL assisted with the project design, literature review, and manuscript drafting. BB assisted with the literature review and manuscript revisions. RD assisted with the manuscript drafting and manuscript revisions. AP assisted with the literature review, table construction, and manuscript revisions. AK assisted with the project design and manuscript revisions. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lawton, C.D., Butler, B.A., Dekker, R.G. et al. Total ankle arthroplasty versus ankle arthrodesis—a comparison of outcomes over the last decade. J Orthop Surg Res 12, 76 (2017). https://doi.org/10.1186/s13018-017-0576-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-017-0576-1