Abstract
Background
Artificial intelligence (AI) is gaining traction in medicine and surgery. AI-based applications can offer tools to examine high-volume data to inform predictive analytics that supports complex decision-making processes. Time-sensitive trauma and emergency contexts are often challenging. The study aims to investigate trauma and emergency surgeons’ knowledge and perception of using AI-based tools in clinical decision-making processes.
Methods
An online survey grounded on literature regarding AI-enabled surgical decision-making aids was created by a multidisciplinary committee and endorsed by the World Society of Emergency Surgery (WSES). The survey was advertised to 917 WSES members through the society’s website and Twitter profile.
Results
650 surgeons from 71 countries in five continents participated in the survey. Results depict the presence of technology enthusiasts and skeptics and surgeons' preference toward more classical decision-making aids like clinical guidelines, traditional training, and the support of their multidisciplinary colleagues. A lack of knowledge about several AI-related aspects emerges and is associated with mistrust.
Discussion
The trauma and emergency surgical community is divided into those who firmly believe in the potential of AI and those who do not understand or trust AI-enabled surgical decision-making aids. Academic societies and surgical training programs should promote a foundational, working knowledge of clinical AI.
Similar content being viewed by others
Background
Artificial intelligence (AI) is defined as the development of algorithms that give machines the ability to act with human-like rationality in complex tasks, such as problem-solving and decision-making, and is poised to reshape medicine and surgery broadly [1].
Diagnostic and judgment errors are the second leading cause of preventable harm [2]. Decision-making is one of the most challenging and crucial tasks performed by trauma and emergency surgeons, where time constraints and high cognitive loads from high volumes of information demand reliance on cognitive shortcuts, leading to mistakes and preventable patient harm [3].
In recent years, decision support systems based on AI algorithms are receiving considerable attention in the literature [4,5,6]. In contrast to human cognitive capacities, AI can be used to examine high-complexity and high-volume data for predictive analytics to augment the precision of complex decision-making processes. Nonetheless, deploying medical AI systems in routine trauma and emergency surgery care presents a critical yet largely unfulfilled opportunity as the medical AI community steers the complex ethical, technical, and human-centered challenges required for safe and adequate translation [7,8,9,10]. Experienced surgeons are appropriately cautious of enthusiastic, novel solutions that are unsubstantiated by academic rigor and evidence of performance advantages in clinical settings [8]. Even when AI accurately predicts clinical outcomes hours or days in advance, its application in trauma and emergency surgery will remain marginal until the deployment proves trust in the accuracy and the lack of bias of the model, addresses target risk-sensitive decisions, and integrates with clinical workflows [11, 12].
The recently published artificial intelligence in Emergency and Trauma Surgery (ARIES) survey, endorsed by the World Society of Emergency Surgery (WSES) evaluated the knowledge, attitude, and practices in the application of AI in the emergency setting among international acute care and emergency surgeons. The investigation revealed how the implementation of AI in the emergency and trauma setting is highly anticipated but still in an early phase, with trauma and emergency surgeons enthusiastic about being involved [13].
Starting from these premises and research gaps, this article aims to assess surgeons’ understanding and knowledge about the role of new technologies like AI in clinical decision-making by employing an international survey endorsed by the WSES.
Methods
Design and setting
The exploratory study of the international trauma and emergency surgeons’ community used a population-based online questionnaire to gather demographic, knowledge, and practice-based information regarding the adoption of new technological tools to support clinical decision-making. The online questionnaire was generated in English through Google Forms [14, 15], and followed the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [16].
A steering committee within the WSES was appointed, involving a multidisciplinary panel of academics and practitioners in the fields of trauma and emergency surgery, healthcare management and policies, innovation, business and medical ethics, information technology, law, and organization science. No Institutional Review Board (IRB) approval was required. Starting from a review of the literature, a research protocol was conceived and shared by the principal investigators (LC and FDM) with the steering committee. The protocol was peer-reviewed and published [17]. The leading references to create the protocol and the survey structure were gathered from Dal Mas et al. [18], Loftus et al. [19, 20], Cobianchi et al. [21], Venkatesh et al. [22], and Bashshur, Shannon and Sapci [23]. Before the initiative's official launch, the research protocol and the online survey were reviewed by the steering committee and filled in by a sample of surgeons to avoid mistakes.
The poll was made available at the end of November 2021 and was open until the middle of August 2022. All 917 WSES members received an e-mail invitation to participate in the survey. The initiative was also shared on the society's website and Twitter account. Additionally, the members of the Team Dynamics Study Group [14, 15] were also invited via e-mail. Four e-mail reminders were sent. WSES membership was not required to answer the survey. Still, it may be assumed that the vast majority of the participants come from the 917 WSES members to whom the research initiative was publicized, yielding an approximate 70% response rate.
The invitation e-mail included comprehensive details on the initiative's goals and rationale, the anticipated time frame (about 10 min), and the option to join the Team Dynamics Study Group to carry out additional research and disseminate the results. The identities of the participants were kept secret. Additionally, the identity of the investigators and the research protocol were kept private.
Survey
The first group of questions aimed at understanding the participants’ features. The questions’ structure and list were derived from the previous Team Dynamics investigation [14, 15]. Surgeons were asked to disclose their gender, years of experience in trauma/emergency surgery, type of institution (academic versus non-academic), the country in which they work, role, eventual participation within a trauma team (institutionalized or not, and of which type), the kind of trauma leader, the educational training attended, and the eventual presence of diverse team members.
The second group of questions investigated the decision aids as reported by the surgical literature [18,19,20], by assessing the surgeons’ perception of 11 items using a 5-point Likert scale.
The third group of questions concerned the perceived challenges that surgeons need to face when making clinical decisions, assessing 13 items gathered from Loftus and colleagues [20] using a 5-point Likert scale.
The fourth section of the questionnaire aimed at assessing the surgeons’ feelings about AI by asking them if they were familiar with the term AI, their understanding of it through an open question, and the perceived importance of AI in surgery at the present time and in a five-year horizon. One last question aimed to assess the perceived benefits [21, 22] of the application of AI in surgery.
The survey’s questions related to clinical decision-making through new technological aids are reported in Appendix 1.
Statistical analysis
The statistical analysis was conducted using the software R (RStudio 2022.07.0 + 548 "Spotted Wakerobin" Release) [24].
Manual coding was also employed concerning the qualitative questions. Surgeons were required to express their understanding of AI through an open question. Results were manually coded by two researchers (LC and FDM), who rated each statement as concordant, discordant, or inconclusive, following the analysis of Woltz et al. [25] and Cobianchi et al. [14].
Results
Participants
650 surgeons responded to the questionnaire. Located on five continents, participants hailed from 71 different nations. The sample, however, was not evenly dispersed, with the majority of surgeons coming from Europe (477, or 73%), particularly Italy (251, or 39%). 465 responders (72%) were from the 10 nations with the most participants overall.
118 female surgeons (18%), 531 male surgeons (82%), and one person who would rather remain anonymous made up the sample. Surgeons' years of experience in the field ranged from 1 to 35, with a mean of 12. The majority of participants (499, or 77% of the sample) were from academic institutions, and 540 of them declared to be part of a formally-established emergency surgery team (83%). Although there were a variety of roles indicated, senior consultants made up the bulk of surgeons (233, or 36%). Department heads made up 114 (18%) of the sample.
Table 1 presents descriptive statistics about the individuals and institutions that participated in the study, whereas Table 2 reports some information about the number of respondents according to their locations.
Clinical decision-making facilitators
Surgeons were given a list of 11 items referred to clinical decision-making facilitators to be rated on a 5-point Likert scale according to their perceived importance. Clinicians underlined the importance of training, clinical guidelines, and multidisciplinary committees and meetings, with a mean of over 4 out of 5. Interestingly, the most modern tools (namely, risk stratification by additive scores using static variable thresholds, machine learning and artificial intelligence, regression modeling and calculations—with 3.87, 3.56, and 3.49, respectively) received the lowest scores, with machine learning and artificial intelligence recording the highest standard deviation (1.07). The following Table 3 reports the results.
The responses given to the item “Machine Learning and Artificial Intelligence” were analyzed by dividing the sample by institution, position held, and country. Interestingly, the institution (academic or non-academic) and the role did not show any significant difference. Major differences emerged when analyzing countries, with some of them (like Argentina) showing a high mean (4.5) and a low standard deviation (0.548), and others (like Switzerland) a very low mean (2.6) and a high standard deviation (0.89). Such results are reported in the following Table 4.
Moreover, the same responses were analyzed by considering the institution, position, and country simultaneously. Although numbers become smaller, some interesting findings emerge. For instance, all senior consultants belonging to Malaysian academic institutions firmly believed in AI, with all of them giving a rate of 5/5, compared to division chiefs working in the USA, who scored the item 2.5 with a standard deviation of 1.05. Despite being digital natives, residents do not appear in the top positions. Results are depicted in the following Table 5.
Challenges in clinical decision-making
Surgeons were asked to rate 13 items regarding the challenges that could arise when engaging in clinical decision-making. The items were adapted from Loftus et al. [20].
Results underline a perceived misalignment between the actual clinical scenario and the independent assessment, the lack of complete data availability, the risk of expecting specific outcomes grounded on inaccurate data, the presence of bias derived from the most recent experiences, and the possibility of making mistakes all along the clinical journey. Interestingly, surgeons rated the potential support granted by new technologies like AI as the lowest item (with a mean of 3.10 and the highest standard deviation of 1.14).
Findings are reported in the following Table 6.
Knowledge and understanding of AI
Surgeons were asked if they were familiar with the term AI. 451 out of 650 participants (69% of the sample) declared they were familiar with the term, while 199 (31%) admitted they were not.
The following question required surgeons to write their understanding of AI applied to surgery. Each given statement was rated by the two principal investigators (LC and FDM) as concordant, discordant, or inconclusive.
To be rated as concordant, definitions needed to somehow stress the capability of the machine to mimic human intelligence or, at least, to express the aims and potential of AI applied to surgical practice or its technological functioning. Only 112 surgeons (17% of the sample) provided a statement that fitted the criterion. 178 participants (27% of the sample) gave responses that were incomplete, showing only a partial view of the phenomenon, being so rated as inconclusive. The remaining 360 surgeons (55% of the participants) gave answers that were not fitting the concept of AI, its aims, and its potential. Most of these participants declared they had no idea about what AI could entail in surgical practice.
The following Table 7 reports some examples of answers that were rated as concordant, inconclusive, and discordant [14, 25].
The statements were also analyzed according to different keys, namely, the fact that they recalled the idea of AI supporting clinical decision-making and of learning/training, and the eventual other technologies linked to AI. Most surgeons (409, 63% of the sample) mentioned the impact on clinical decision-making, and 57 (9%) recalled the potential of AI for surgical training. Among the most cited technologies that may be linked with AI, there are Big Data (mentioned by 130 participants – 20% of the sample) and new technologies in general terms (107, 16%).
Table 8 highlights such results.
The potential of AI today and tomorrow
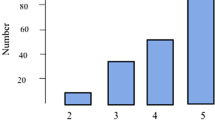
Surgeons were asked to express their opinion about the importance of AI-based applications to support clinical decision-making at the current time and on a five-year horizon, using a 5-point Likert scale.
Participants rated the importance today with a mean of 3.06 out of 5 and a standard deviation of 1.1. In the future, the sample rated the importance as 3.88 as an average with a standard deviation of 0.97.
The goals of AI
One last question referred to the perceived goals and benefits of AI-based in supporting clinical decision-making. Five items needed to be rated on a 5-point Likert scale.
Interestingly, surgeons rated all five items as equally relevant (ranging from a mean score of 3.51 to 3.78). The item with the highest score sees AI as a support tool to validate decisions that clinicians would make anyway.
The following Table 9 reports the results.
Discussion
The results of our survey are in line with previous studies [13], with trauma and emergency surgeons showing interest in AI but still having several doubts and concerns about its actual application and potential as a decision-making aid.
When enquired about the most effective tools to support clinical decision-making, surgeons declare to rely more on training, clinical guidelines, and the support of their multidisciplinary staff and colleagues. Interestingly, these three items represent central and “classical” elements in the trauma and emergency surgery context [14] and in the action of the leading scientific societies like the WSES, which promotes training modules for both physicians and nurses [26], clinical guidelines covering several aspects of the clinical profession [27], and studies on multidisciplinary team dynamics [14, 15]. AI and Machine Learning tools got one of the lowest rates (3.56), with the highest standard deviation (1.07). The broad standard deviation interval may represent a gap in the surgical community, with some surgeons firmly believing in the potential of such new technologies and others still having severe concerns about their practical application.
Interestingly, while no significant differences emerge when considering the institution and the position held, geographical differences occur in the sample, with some countries giving higher scores than others. It would be interesting to investigate further while such differences emerge, for instance, in terms of cultural mindset, training opportunities, availability of technology or tech partners, and presence of technological surgical leaders or ambassadors. Moreover, when analyzing the sample under different lenses simultaneously (institution, role, and country), residents do not appear to be technology enthusiasts and believers, despite their younger age and the definition of digital natives.
When considering the decision-making process dynamics, trauma and emergency surgeons underline the need for sound decision aids. Indeed, the most rated elements refer to the potential gap between reality and the surgeon's initial assessment and the lack of accurate data. Even in this case, most respondents did not believe that AI offers valuable support for decision-making. Like in the case of decision aids, the contribution of AI to decision-making got the highest standard deviation, depicting the two extreme views, with enthusiastic adopters in contrast with skeptics.
Regarding the knowledge about AI, while most surgeons declare to be familiar with the concept of AI, many exhibited only a partial understanding of AI. Interestingly, many surgeons recall big data technology, and some associate AI primarily with robotics. While robotic surgery may represent one promising application of AI in surgical science [13, 28, 29], AI in its current state offers sound decision-making support, like in the case of the POTTER algorithm as an emergency surgery risk calculator [5, 6].
The current general skepticism of trauma and emergency surgeons about AI is also confirmed by the given rate on the relevance of AI-based tools for decision-making as they appear today, with a mean of 3.06. One more time, a high standard deviation interval depicts divergent opinions and beliefs in the surgical community. Still, the future looks brighter, with a higher perceived relevance on a five-year horizon.
The same picture and the divergent trust in using AI-based decision tools emerge in the question about the goals and benefits. Interestingly, the degree of technology acceptance appears generally low, with surgeons being rather skeptical when it comes to AI ensuring better support and outcomes than traditional tools. Such a low degree of acceptance opens up new research avenues to investigate the main concerns in the practical adoption of AI or the ethical bias connected to it. In such a perspective, one primary concern may reside in the lack of technical knowledge regarding AI, which emerges from several questions, especially that on the understanding of AI. Moreover, when enquired about legal responsibility (a topic to which medical doctors are particularly sensitive), surgeons modestly rate the need to share their legal responsibility with either the manufacturer, those in charge of maintenance, or the data manager, and so the need to rethink the informed written consent when new technologies are involved.
Limitations
Although our survey got a reasonably high response rate and 650 participants (approximately 70%), the sample is not equally distributed geographically. Indeed, most participants work in Europe and, more specifically, in Italy. The specific situation of the Italian and European contexts, including the actual access to AI-based technology and the medical education related to it, may have biased some of our results. Our limitations, along with the international community's perceived interest in AI [13], may stimulate new in-depth studies and investigations.
Conclusion
In concluding our work, we return to the premises and research gaps that inspired it. AI-based applications are gaining traction in surgery as decision-making aids, and the surgical community is showing interest in them. Trauma and emergency contexts are often challenging, and surgeons perceive the need for sound decision-making tools.
Our results underline how the emergency surgical community seems to include surgeons who strongly believe in the potential contribution of AI technology and who may act as enthusiastic early adopters [19] and those who are reluctant, feeling more comfortable relying upon more classical aids like guidelines, traditional training, and multidisciplinary groups’ support. Some countries seem to have greater comprehension and trust of AI-based tools. Younger surgeons, who some presume to be keener on using new technologies, do not appear to have greater trust or understanding of AI compared with mid-career and senior surgeons.
Given the potential of AI in clinical practice [7, 20, 30] and the speed of development, the role of scientific societies like the WSES and surgical training programs are crucial to expanding knowledge regarding AI-enabled decision aids, disseminate new approaches, and encompass them in training modules and clinical guidelines, to bridge the gaps between technology enthusiasts and those who misunderstand and mistrust AI. In addition, AI-enabled decision aids in surgery should seek to gain the trust of surgeons by establishing transparency and by demonstrating performance advantages that improve patient care.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Change history
23 March 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13017-023-00493-9
Abbreviations
- AI:
-
Artificial intelligence
- WSES:
-
World society of emergency surgery
- CHERRIES:
-
Checklist for reporting results of internet e-surveys
- IRB:
-
Institutional review board
- SD:
-
Standard deviation
References
Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nat Med. 2022;28(1):31–8.
Healey MA, Shackford SR, Osler TM, Rogers FB, Burns E. Complications in surgical patients. Arch Surg. 2002;137(5):611–8.
Litvin A, Korenev S, Rumovskaya S, Sartelli M, Baiocchi G, Biffl WL, et al. WSES project on decision support systems based on artificial neural networks in emergency surgery. World J Emerg Surg. 2021;16(1):50.
Loftus TJ, Vlaar APJ, Hung AJ, Bihorac A, Dennis BM, Juillard C, et al. Executive summary of the artificial intelligence in surgery series. Surgery. 2022;171(5):1435–9.
Bertsimas D, Dunn J, Velmahos GC, Kaafarani HMA. Surgical Risk Is Not Linear: Derivation and Validation of a Novel, User-friendly, and Machine-learning-based Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) Calculator. Ann Surg [Internet]. 2018;268(4). https://journals.lww.com/annalsofsurgery/Fulltext/2018/10000/Surgical_Risk_Is_Not_Linear__Derivation_and.4.aspx
Maurer LR, Bertsimas D, Bouardi HT, El Hechi M, El Moheb M, Giannoutsou K, et al. Trauma outcome predictor: An artificial intelligence interactive smartphone tool to predict outcomes in trauma patients. J Trauma Acute Care Surg [Internet]. 2021;91(1). https://journals.lww.com/jtrauma/Fulltext/2021/07000/Trauma_outcome_predictor__An_artificial.15.aspx
Johnson-Mann CN, Loftus TJ, Bihorac A. Equity and artificial intelligence in surgical care. JAMA Surg. 2021;156(6):509.
Balch J, Upchurch GR, Bihorac A, Loftus TJ. Bridging the artificial intelligence valley of death in surgical decision-making. Surgery. 2021;169(4):746–8.
Loftus TJ, Upchurch GR, Bihorac A. Building an artificial intelligence-competent surgical workforce. JAMA Surg. 2021;156(6):511.
Ingraham NE, Jones EK, King S, Dries J, Phillips M, Loftus T, et al. Re-Aiming Equity Evaluation in Clinical Decision Support: A Scoping Review of Equity Assessments in Surgical Decision Support Systems. Ann Surg. 2022 Aug;Publish Ah(612).
Loftus TJ, Tighe PJ, Ozrazgat-Baslanti T, Davis JP, Ruppert MM, Ren Y, et al. Ideal algorithms in healthcare: explainable, dynamic, precise, autonomous, fair, and reproducible. In: Lu HH-S (ed.) PLOS Digit Heal. 2022;1(1):e0000006.
Loftus TJ, Shickel B, Ruppert MM, Balch JA, Ozrazgat-Baslanti T, Tighe PJ, et al. Uncertainty-aware deep learning in healthcare: a scoping review. In: Lai Y (ed.) PLOS Digit Heal. 2022;1(8):e0000085.
De Simone B, Abu-Zidan FM, Gumbs AA, Chouillard E, Di Saverio S, Sartelli M, et al. Knowledge, attitude, and practice of artificial intelligence in emergency and trauma surgery, the ARIES project: an international web-based survey. World J Emerg Surg. 2022;17(1):10.
Cobianchi L, Dal Mas F, Massaro M, Fugazzola P, Coccolini F, Kluger Y, et al. Team dynamics in emergency surgery teams: results from a first international survey. World J Emerg Surg. 2021;16:47. https://doi.org/10.1186/s13017-021-00389-6
Cobianchi L, Dal Mas F, Massaro M, Biffl W, Catena F, Coccolini F, et al. Diversity and ethics in trauma and acute care surgery teams: results from an international survey. World J Emerg Surg. 2022;17(1):44. https://doi.org/10.1186/s13017-022-00446-8.
Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6(3):1–6.
Cobianchi L, Dal Mas F, Catena F, Ansaloni A. Artificial intelligence and clinical decision-making in emergency surgery. A research protocol. In: Sousa MJ, Kumar PS, Dal Mas F, Sousa S (eds.) Advancements in artificial intelligence in the service sector. London: Routledge; 2023.
DalMas F, Garcia-Perez A, Sousa MJ, LopesdaCosta R, Cobianchi L. Knowledge translation in the healthcare sector. A structured literature review. Electron J Knowl Manag. 2020;18(3):198–211. https://doi.org/10.34190/EJKM.18.03.001
Loftus TJ, Filiberto AC, Balch J, Ayzengart AL, Tighe PJ, Rashidi P, et al. Intelligent, autonomous machines in surgery. J Surg Res. 2020;253:92–9. https://doi.org/10.1016/j.jss.2020.03.046.
Loftus TJ, Tighe PJ, Filiberto AC, Efron PA, Brakenridge SC, Mohr AM, et al. Artificial intelligence and surgical decision-making. JAMA Surg. 2020;155(2):148–58.
Cobianchi L, Verde JM, Loftus TJ, Piccolo D, Dal Mas F, Mascagni P, et al. Artificial Intelligence and Surgery: Ethical Dilemmas and Open Issues. J Am Coll Surg. 2022;235(2):268–75. https://journals.lww.com/journalacs/Fulltext/9900/Artificial_Intelligence_and_Surgery__Ethical.215.aspx
Venkatesh V, Morris M, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. Mis Q. 2003;27(3):425–78.
Bashshur R, Shannon G, Krupinski E, Grigsby J. The taxonomy of telemedicine. Telemed J e-health Off J Am Telemed Assoc. 2011;17(6):484–94.
R Development Core Team. The R Manuals [Internet]. R. 2021 [cited 2021 Mar 12]. https://cran.r-project.org/manuals.html
Woltz S, Krijnen P, Pieterse AH, Schipper IB. Surgeons’ perspective on shared decision making in trauma surgery. A national survey. Patient Educ Couns. 2018;101(10):1748–52. https://doi.org/10.1016/j.pec.2018.06.002.
World Society of Emergency Surgery. Wses courses [Internet]. Courses for physicians and nurses. 2022 [cited 2022 Oct 4]. https://www.wses.org.uk/courses
World Society of Emergency Surgery. Wses guidelines [Internet]. WSES Guidelines. 2022 [cited 2022 Oct 4]. https://www.wses.org.uk/guidelines
McBride KE, Steffens D, Duncan K, Bannon PG, Solomon MJ. Knowledge and attitudes of theatre staff prior to the implementation of robotic-assisted surgery in the public sector. PLoS One. 2019;14(3):e0213840. https://doi.org/10.1371/journal.pone.0213840.
O’Sullivan S, Nevejans N, Allen C, Blyth A, Leonard S, Pagallo U, et al. Legal, regulatory, and ethical frameworks for development of standards in artificial intelligence (AI) and autonomous robotic surgery. Int J Med Robot Comput Assist Surg. 2019;15(1):1–12.
Byerly S, Maurer LR, Mantero A, Naar L, An G, Kaafarani HMA. Machine learning and artificial intelligence for surgical decision making. Surg Infect (Larchmt). 2021;22(6):626–34. https://doi.org/10.1089/sur.2021.007.
Acknowledgements
Please see the list of the Team Dynamics Study Group members.
Kenneth Lyle Abbott1, Abubaker Abdelmalik2, Nebyou Seyoum Abebe3, Fikri Abu-Zidan4, Yousif Abdallah Yousif Adam5, Harissou Adamou6, Dmitry Mikhailovich Adamovich7, Ferdinando Agresta8, antonino Agrusa9, Emrah Akin10, Mario Alessiani11, Henrique Alexandrino12, Syed Muhammad Ali13, Vasilescu Alin Mihai14, Pedro Miguel Almeida15, Mohammed Mohammed Al-Shehari16, Michele Altomare17, Francesco Amico18, Michele Ammendola19, Jacopo Andreuccetti20, Elissavet Anestiadou 21, Peter Angelos22, Alfredo Annicchiarico23, Amedeo Antonelli24, Daniel Aparicio-Sanchez25, antonella Ardito26, Giulio Argenio27, Catherine Claude Arvieux28, Ingolf Harald Askevold29, Boyko Tchavdarov Atanasov30, Goran Augustin31, Selmy Sabry Awad32, Giulia Bacchiocchi 33, Carlo Bagnoli34, Hany Bahouth35, Efstratia Baili36, Lovenish Bains37, Gian Luca Baiocchi38, Miklosh Bala39, Carmen Balagué 40, Dimitrios Balalis41, Edoardo Baldini42, oussama Baraket43, Suman Baral44, Mirko Barone45, Alberto Gonzãlez Barranquero46, Jorge Arturo Barreras47, Gary Alan Bass48, Zulfu Bayhan49, Giovanni Bellanova50, Offir Ben-Ishay 51, Fabrizio Bert52, Valentina Bianchi 53, Helena Biancuzzi54, Chiara Bidoli55, Raluca Bievel Radulescu56, Mark Brian Bignell57, Alan Biloslavo58, Roberto Bini59, Daniele Bissacco60, Paoll Boati61, Guillaume Boddaert62, Branko Bogdanic63, Cristina Bombardini64, Luigi Bonavina65, Luca Bonomo66, Andrea Bottari67, Konstantinos Bouliaris68, Gioia Brachini69, Antonio Brillantino70, Giuseppe Brisinda71, Maloni Mamada Bulanauca72, Luis Antonio Buonomo73, Jakob Burcharth74, Salvatore Buscemi75, Francesca Calabretto76, Giacomo Calini77, Valentin Calu78, Fabio Cesare Campanile79, Riccardo Campo Dall’Orto80, Andrea Campos-Serra81, Stefano Campostrini82, Recayi Capoglu83, Joao Miguel Carvas84, Marco Cascella85, Gianmaria Casoni Pattacini86, Valerio Celentano87, Danilo Corrado Centonze88, Marco Ceresoli89, Dimitrios Chatzipetris90, Antonella Chessa91, Maria Michela Chiarello92, Mircea Chirica93, Serge Chooklin94, Christos Chouliaras95, Sharfuddin Chowdhury96, Pasquale Cianci97, Nicola Cillara98, Stefania Cimbanassi99, Stefano Piero Bernardo Cioffi100, Elif Colak101, Enrique Colás Ruiz102, Luigi Conti103, Alessandro Coppola104, Tiago Correia De Sa105, Silvia Dantas Costa106, Valerio Cozza107, Giuseppe Curro’108, Kirsten Felicia Ann-Sophie Aimee Dabekaussen109, Fabrizio D’acapito110, Dimitrios Damaskos111, Giancarlo D’Ambrosio112, Koray Das113, Richard Justin Davies114, Andrew Charles De Beaux115, Sara Patricia De Lebrusant Fernandez 116, Alessandro De Luca117, Francesca De Stefano118, Luca Degrate119, Zaza Demetrashvili120, Andreas Kyriacou Demetriades121, Dzemail Smail Detanac 122, Agnese Dezi123, Giuseppe Di Buono124, Isidoro Di Carlo125, Pierpaolo Di Lascio126, Marcello Di Martino127, Salomone Di Saverio128, Bogdan Diaconescu129, Jose J. Diaz130, Rigers Dibra131, Evgeni Nikolaev Dimitrov132, Vincenza Paola Dinuzzi133, Sandra Dios-Barbeito134, Jehangir Farman Ali Diyani135, Agron Dogjani136, Maurizio Domanin137, Mario D’Oria138, Virginia Duran Munoz-Cruzado139, Barbora East140, Mikael Ekelund141, Gerald Takem Ekwen142, Adel Hamed Elbaih143, Muhammed Elhadi144, Natalie Enninghorst145, Mairam Ernisova146, Juan Pablo Escalera-Antezana147, Sofia Esposito148, Giuseppe Esposito149, Mercedes Estaire150, Camilla Nikita Farè151, Roser Farre 152, Francesco Favi153, Luca Ferrario154, Antonjacopo Ferrario di Tor Vajana155, Claudia Filisetti156, Francesco Fleres157, Vinicius Cordeiro Fonseca158, Alexander Forero-Torres159, Francesco Forfori160, Laura Fortuna161, Evangelos Fradelos162, Gustavo P. Fraga163, Pietro Fransvea164, Simone Frassini165, Giuseppe Frazzetta166, Erica Pizzocaro 167, Maximos Frountzas168, Mahir Gachabayov169, Rita Galeiras170, Alain A. Garcia Vazquez171, Simone Gargarella172, Ibrahim Umar Garzali173, Wagih Mommtaz Ghannam174, Faiz Najmuddin Ghazi175, Lawrence Marshall Gillman176, Rossella Gioco177, Alessio Giordano178, Luca Giordano179, Carlo Giove180, Giorgio Giraudo181, Mario Giuffrida182, Michela Giulii Capponi183, Emanuel Gois Jr.184, Carlos Augusto Gomes185, Felipe Couto Gomes186, Ricardo Alessandro Teixeira Gonsaga187, Emre Gonullu188, Jacques Goosen189, Tatjana Goranovic190, Raquel Gracia-Roman191, Giorgio Maria Paolo Graziano192, Ewen Alexander Griffiths193, Tommaso Guagni194, Dimitar Bozhidarov Hadzhiev195, Muad Gamil Haidar196, Hytham K. S. Hamid197, Timothy Craig Hardcastle198, Firdaus Hayati199, Andrew James Healey200, Andreas Hecker201, Matthias Hecker202, Edgar Fernando Hernandez Garcia203, Adrien Montcho Hodonou204, Eduardo Cancio Huaman205, Martin Huerta206, Aini Fahriza Ibrahim207, Basil Mohamed Salabeldin Ibrahim208, Giuseppe Ietto209, Marco Inama210, Orestis Ioannidis211, Arda Isik212, Nizar Ismail213, Azzain Mahadi Hamid Ismail214, Ruhi Fadzlyana Jailani215, Ji Young Jang216, Christos Kalfountzos217, Sujala Niatarika Rajsain Kalipershad218, Emmanouil Kaouras219, Lewis Jay Kaplan220, Yasin Kara221, Evika Karamagioli222, Aleksandar Karamarkovia223, Ioannis Katsaros224, Alfie J. Kavalakat225, Aristotelis Kechagias226, Jakub Kenig227, Boris Juli Kessel 228, Jim S. Khan229, Vladimir Khokha230, Jae Il Kim231, Andrew Wallace Kirkpatrick232, Roberto Klappenbach233, Yoram Kluger234, Yoshiro Kobe236, Efstratios Kofopoulos Lymperis237, Kenneth Yuh Yen Kok238, Victor Kong239, Dimitris P. Korkolis 240, Georgios Koukoulis241, Bojan Kovacevic242, Vitor Favali Kruger243, Igor A. Kryvoruchko244, Hayato Kurihara245, Akira Kuriyama246, Aitor Landaluce-Olavarria 247, Pierfrancesco Lapolla248, Ari Leppäniemi249, Leo Licari250, Giorgio Lisi251, Andrey Litvin252, Aintzane Lizarazu253, Heura Llaquet Bayo254, Varut Lohsiriwat255, Claudia Cristina Lopes Moreira256, Eftychios Lostoridis257, Agustãn Tovar Luna258, Davide Luppi259, Gustavo Miguel Machain V.260, Marc Maegele261, Daniele Maggiore262, Stefano Magnone263, Ronald V. Maier264, Piotr Major266, Mallikarjuna Manangi267, Andrea Manetti268, Baris Mantoglu269, Chiara Marafante270, Federico Mariani271, Athanasios Marinis272, Evandro Antonio Sbalcheiro Mariot273, Gennaro Martines 275, Aleix Martinez Perez276, Costanza Martino278, Pietro Mascagni279, Damien Massalou280, Maurizio Massaro281, Belen Matías-García282, Gennaro Mazzarella283, Giorgio Mazzarolo284, Renato Bessa Melo285, Fernando Mendoza-Moreno286, Serhat Meric287, Jeremy Meyer288, Luca Miceli289, Nikolaos V. Michalopoulos290, Flavio Milana291, Andrea Mingoli292, Tushar S. Mishra293, Muyed Mohamed294, Musab Isam Eldin Abbas Mohamed295, Ali Yasen Mohamedahmed296, Mohammed Jibreel Suliman Mohammed297, Rajashekar Mohan298, Ernest E. Moore299, Dieter Morales-Garcia300, MÃ¥ns Muhrbeck301, Francesk Mulita 302, Sami Mohamed Siddig Mustafa303, Edoardo Maria Muttillo304, Mukhammad David Naimzada305, Pradeep H. Navsaria306, Ionut Negoi307, Luca Nespoli308, Christine Nguyen309, Melkamu Kibret Nidaw 310, Giuseppe Nigri311, Ioannis Nikolopoulos312, Donal Brendan O’Connor313, Habeeb Damilola Ogundipe314, Cristina Oliveri315, Stefano Olmi316, Ernest Cun Wang Ong317, Luca Orecchia318, Aleksei V. Osipov319, Muhammad Faeid Othman320, Marco Pace321, Mario Pacilli322, Leonardo Pagani323, Giuseppe Palomba324, Desire’ Pantalone325, Arpad Panyko326, Ciro Paolillo327, Mario Virgilio Papa328, Dimitrios Papaconstantinou329, Maria Papadoliopoulou330, Aristeidis Papadopoulos331, Davide Papis332, Nikolaos Pararas333, Jose Gustavo Parreira 334, Neil Geordie Parry335, Francesco Pata336, Tapan Patel 337, Simon Paterson-Brown338, Giovanna Pavone339, Francesca Pecchini340, Veronica Pegoraro341, Gianluca Pellino342, Maria Pelloni343, Andrea Peloso344, Eduardo Perea Del Pozo345, Rita Goncalves Pereira346, Bruno Monteiro Pereira347, Aintzane Lizarazu Perez348, Silvia Pérez349, Teresa Perra350, Gennaro Perrone351, Antonio Pesce352, Lorenzo Petagna353, Giovanni Petracca354, Vorapong Phupong 355, Biagio Picardi356, Arcangelo Picciariello 357, Micaela Piccoli358, Edoardo Picetti360, Emmanouil Pikoulis Pikoulis361, Tadeja Pintar362, Giovanni Pirozzolo363, Francesco Piscioneri364, Mauro Podda365, Alberto Porcu366, Francesca Privitera367, Clelia Punzo368, Silvia Quaresima369, Martha Alexa Quiodettis370, Niels Qvist371, Razrim Rahim372, Filipe Ramalho de Almeida373, Rosnelifaizur Bin Ramely374, Huseyin Kemal Rasa375, Martin Reichert376, Alexander Reinisch-Liese377, Angela Renne378, Camilla Riccetti379, Maria Rita Rodriguez-Luna380, Daniel Roizblatt381, Andrea Romanzi382, Luigi Romeo383, Francesco Pietro Maria Roscio384, Ramely Bin Rosnelifaizur 385, Stefano Rossi386, Andres M Rubiano387, Elena Ruiz-Ucar388, Boris Evgeniev Sakakushev389, Juan Carlos Salamea 390, Ibrahima Sall391, Lasitha Bhagya Samarakoon392, Fabrizio Sammartano393, Alejandro Sanchez Arteaga394, Sergi Sanchez-Cordero395, Domenico Pietro Maria Santoanastaso396, Massimo Sartelli397, Diego Sasia398, Norio Sato399, Artem Savchuk400, Robert Grant Sawyer401, Giacomo Scaioli402, Dimitrios Schizas403, Simone Sebastiani404, Barbara Seeliger405, Helmut Alfredo Segovia Lohse406, Charalampos Seretis407, Giacomo Sermonesi408, Mario Serradilla-Martin409, Vishal G. Shelat410, Sergei Shlyapnikov411, Theodoros Sidiropoulos 412, Romeo Lages Simoes413, Leandro Siragusa414, Boonying Siribumrungwong415, Mihail Slavchev416, Leonardo Solaini417, gabriele soldini418, Andrey Sopuev419, Kjetil Soreide420, Apostolos Sovatzidis421, Philip Frank Stahel422, Matt Strickland423, Mohamed Arif Hameed Sultan424, Ruslan Sydorchuk425, Larysa Sydorchuk426, Syed Muhammad Ali Muhammad Syed427, Luis Tallon-Aguilar428, Andrea Marco Tamburini429, Nicolò Tamini430, Edward C .T. H. Tan431, Jih Huei Tan432, Antonio Tarasconi433, Nicola Tartaglia434, Giuseppe Tartaglia435, Dario Tartaglia436, John Vincent Taylor437, Giovanni Domenico Tebala438, Ricardo Alessandro Teixeira Gonsaga439, Michel Teuben440, Alexis Theodorou441, Matti Tolonen442, Giovanni Tomasicchio443, Adriana Toro444, Beatrice Torre445, Tania Triantafyllou446, Giuseppe Trigiante Trigiante 447, Marzia Tripepi 448, Julio Trostchansky449, Konstantinos Tsekouras450, Victor Turrado-Rodriguez451, Roberta Tutino452, Matteo Uccelli453, Petar Angelov Uchikov454, Bakarne Ugarte-Sierra455, Mika Tapani Ukkonen456, Michail Vailas457, Panteleimon G. Vassiliu458, Alain Garcia Vazquez459, Rita Galeiras Vazquez460, George Velmahos461, Juan Ezequiel Verde462, Juan Manuel Verde463, Massimiliano Veroux464, Jacopo Viganò465, RAMON VILALLONGA466, Diego Visconti467, Alessandro Vittori468, Maciej Waledziak469, Tongporn Wannatoop470, Lukas Werner Widmer471, Michael Samuel James Wilson472, Sarah Woltz473, Ting Hway Wong474, Sofia Xenaki475, Byungchul Yu476, Steven Yule477, Sanoop Koshy Zachariah478, Georgios Zacharis479, Claudia Zaghi480, Andee Dzulkarnaen Zakaria481, Diego A. Zambrano482, Nikolaos Zampitis483, Biagio Zampogna484, Simone Zanghì485, Maristella Zantedeschi486, Konstantinos Zapsalis487, Fabio Zattoni488, Monica Zese489.
Affiliations: 1Department of Surgery, University of Florida, Gainesville, USA, 2General Surgery Dept., Misrata Medical Center, Misrata, Libya, 3Department of surgery college of health sciences, Addis Abeba University, Addis Abeba, Ethiopia, 4Research Office, College of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates, 5University Hospital in Waterford, Tullamore, Ireland, 6Department of surgery, Faculté des Sciences de la Santé, Zinder, Zinder, Niger, 7Department of Surgical Diseases II, Senior Lecturer at Gomel State Medical University, Gomel, Belarus, 8Dept. of General Surgery, AULSS2 Trevigiana del Veneto, Vittorio Veneto (TV), Italy, 9Department of Surgical, Oncological and Oral Sciences—University of Palermo, Palermo, Italy, 10Sakarya University Faculty of Medicine, Sakarya, Turkey, 11Department of Clinical Surgical Diagnostic and Pediatric Sciences, University of Pavia—Department of Surgery, ASST Pavia, Pavia, Italy, 12Faculty of Medicina, University of Coimbra, Coimbra, Portugal, 13Department of Acute Care Surgery, Hamad Medical Corporation, Doha, Qatar, 14Grigore T Popa University of Medicine and Pharmacy, Iasi Romania, First Surgical Clinic, St Spiridon University Hospital, Iasi, Romania, 15Centro Hospitalar e Universitario do Algarve—Hospital de Portimao, Portimão, Portugal, 16Sana'a University—College of medicine, Sana'a, Yemen, 17Sapienza University of Rome, Rome, Italy, 18Dept. of Trauma at John Hunter Hospital, School of Medicine and Public Health at University of Newcastle, Newcastle NSW, Australia, 19Health of Science Department, "Magna Graecia" University Medical School, Digestive Surgery Unit, "Mater Domini" Hopsital, Catanzaro, Italy, 20General Surgery 2, ASST Spedali Civili of Brescia, Brescia, Italy, 214th Department of Surgery, Aristotle University of Thessaloniki, Thessaloniki, Greece, 22Department of Surgery and MacLean Center for Clinical Medical Ethics, The University of Chicago, Chicago, IL, USA, 23Università di Parma, Italy, 24Università degli studi di Roma Tor Vergata, Rome, Italy, 25Emergency Surgery Unit (Virgen del Rocio Hospital), Sevilla, Spain, 26Departmento of general Surgery Asst-fbf-sacco, Milan, Italy, 27UOC Chirurgia Generale ed Oncologica, AO San Pio, Benevento, Italy, 28 Grenoble-Alpes University Hospital, GRENOBLE, France, 29Department of General, Visceral, Thoracic, Transplant and Pediatric Surgery, University Hospital of Giessen, Giessen, Germany, 30UMHAT EUROHOSPITAL, MEDICAL UNIVERSITY PLOVDIV, Plovdiv, Bulgaria, 31University Hospital Centre Zagreb, Zagreb, Croatia, 32Department of General surgery-Mansoura Faculty of Medicine, Mansoura, Egypt, 33Department of Surgical Science, University of Rome Tor Vergata, Rome, Italy, 34Department of Management, Ca' Foscari University of Venice, Venice, Italy, 35Trauma center, Rambam medical center, Haifa, Israel, Israel, 36UGI Surgery- Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom, 37Department of Surgery, Maulana Azad Medical College, New Delhi, India, India, 38Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy, 39Department of General Surgery, Hadassah Medical Center and Faculty of Medicine, Hebrew University of Jerusalem, Israel, Jerusalem, Israel, 40Digestive Surgery. Hospital Universitari Mutua Terrassa, Terrassa, Spain, 41Surgery, Saint Savvas Cancer Hospital, Halandri—Athens, Greece, 42Unità Operativa Complessa di Chirurgia—Ospedale Santa Maria delle Stelle, Melzo (Milano), Italy, 43Departement of general surgery. Bizerte hospital .faculty of Medecine of Tunis University Tunis El Manar, bizerte, Tunisia, 44Department of Surgery, Dirghayu Pokhara Hospital, Pokhara, Nepal, 45Department of General and Thoracic Surgery, "SS. Annunziata" University Hospital of Chieti, Chieti, Italy, 46General and Digestive Surgery Department, Ramón y Cajal University Hospital, Madrid, Spain, 47Secretaria de Salud, Hermosillo, Mexico, 48Division of Traumatology, Surgical Critical Care and Emergency Surgery, University of Pennsylvania, Philadelphia, United States, 49Sakarya University, Faculty of Medicine, Department of General Surgery, Sakarya, Turkey, 50UOC Chirurgia Generale PO D.Camberlingo Francavilla Fontana, Francavilla Fontana (BR), Italy, 51Department of General Surgery, Rambam health Care Campus, Haifa, Israel, 52University of Turin, Turin, Italy, 53Chirurgia d'Urgenza e del Trauma, Fondazione Policlinico Gemelli IRCCS, Roma, Italy, 54Department of Pain Medicine, National Cancer Center, Aviano, Rome, Italy, 55Department of Economics, Ca Foscari University, Venice, Italy, 56Banca degli occhi, Mestre, Italy, 57Surgical Emergency Unit, Oxford University NHS Trust, Oxford, United Kingdom, 58General Surgery Department, Cattinara University Hospital. ASUGI, Trieste, Trieste, Italy, 59Emergency Department Niguarda Hospital, Milano, Italy, 60Vascular Surgery Department IRCCS Ca Granda Ospedale Maggiore Policlinico, Milan, Italy, 61asst santi paolo carlo milano, milano, Italy, 62Thoracic and Vasular surgery Department—Percy military hospital, Clamart, France, 63School of Medicine University of Zagreb, Department of Surgery, University Hospital Centre Zagreb, Zagreb, Croatia, 64University Hospital of Ferrara, Surgical Department, Colorectal Unit, Ferrara, Italy, 65University of Milan, Department of Biomedical Sciences for Health, IRCCS Policlinico San Donato, Division of General Surgery, Milano (Italy), Italy, 66Department of General Surgery University Hospitals Dorset, Poole, United Kingdom, 67Digestive Surgery Unit, AOU Careggi, Firenze, Italy, 68General Surgery Department, Koutlimbaneio & Triantafylleio General Hospital of Larissa, Larissa, Greece, 69Dept of Surgery P. Valdoni—sapienza University, Rome, Italy, 70Department of Surgery, "A. Cardarelli" hospital, Naples, Italy, Napoli, Italy, 71Department of Surgery, Fondazione Policlinico Universitario A Gemelli, IRCCS, Roma, Italy, 72Labasa Hospital Fiji, Labasa, Fiji, 73Hopital "Dr. Alberto Balestrini". University of Buenos Aires, Buenos Aires, Argentina, 74Department of Gastrointestinal and Hepatic Diseases, Copenhagen University Hospitals Herlev and Gentofte; Emergency Surgery Research Group Copenhagen (EMERGE), Herlev, Denmark, 75Department of Surgical, Oncological and Oral Science, Policlinico “P.Giaccone” Palermo, Italy, 76University of Pavia, Corso Str. Nuova, 65, 27100, Pavia, Italy; Unit of General Surgery I, Fondazione I.R.C.C.S. Policlinico San Matteo, Viale Camillo Golgi, 19, 27100, Pavia, Italy., Pavia, Italy, 77University of Udine, Udine, Italy, 78Elias Emergency University Hospital, Department of Sugery, Bucharest, Romania, 79Ospedale San Giovanni Decollato—Andosilla, Civita Castellana, Italy, 80Vascular Surgery, University of Padua, Padua, Italy, 81Department of Surgery, Parc Tauli University Hospital, Sabadell, Spain, 82Department of Economics, Ca Foscari University, Venice, Italy, 83Sakarya University Training and Research Hospital General surgery, Sakarya, Turkey, 84Servicao de Cirurgia Geral, Hospital de Bragansa, Bragança, Portugal, 85IRCCS Pascale, Naples, Italy, 86Chirurgia Generale, d'urgenza e Nuove Tecnologie,Ospedale Civile di Baggiovara, Modena, Italy, 87Chelsea and Westminster Hospital, London, United Kingdom, 88Unità operativa complessa chirurgia generale ospedale Umberto I di Enna, Enna, Italy, 89General and Emergency Surgery, Milano-Bicocca University, School of Medicine and Surgery,, Monza, Italy, 90Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece, 91Chirurgia Generale uslsudesttoscana, Orbetello Grosseto, Italy, 92Asp Cosenza, Cosenza, Italy, 93service de chirurgie digestive, Centre Hospitalier Universitaire Grenoble Alpes, Grenoble, France, 94Department of Surgery, Lviv Regional Clinical Hospital, Lviv, Ukraine, 95Athens Medical Center, Athens, Greece, 96Trauma Center, King Saud Medical City, Riyadh, Saudi Arabia, 97University of Foggia-ASL BAT, Andria, Italy, 98UOC Chirurgia Generale ASL8 Cagliari, Cagliari, Italy, 99Acute Care Surgery and Trauma-ASST GOM Niguarda, Milano, Italy, 100General Surgery Trauma Team ASST GOM NIGUARDA MILAN, ITALY, Milano, Italy, 101University of Samsun, Samsun Training and Research Hospital, Department of General Surgery, Samsun, Turkey, 102General Surgery. Hospital Universitario Son Llatzer, Palma de Mallorca, Spain, 103Department of Surgery, Acute care surgery Unit, G. Da Saliceto hospital, Piacenza, Italy, 104General Surgey, Fondazione Policlinico Universitario Campus Bio-Medico, General Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Italy, 105General Surgery Department, Centro Hospitalar do Tâmega e Sousa, Penafiel, Portugal, 106General Surgery, CHVNG/E,EPE, V.N. Gaia, Portugal, 107Chirurgia d'urgenza e del trauma, Fondazione Policlinico Universitario A Gemelli IRCCS, Rome, Italy, 108Health Science Department, Magna Graecia University of Catanzaro, Catanzaro, Italy, 109Department of Surgery, Spaarne Gasthuis, Haarlem, Netherlands, 110General and Oncologic Surgery, Morgagni—Pierantoni Hospital, AUSL Romagna, Forlì, Italy, 111Deparyment of General Surgery, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom, 112Department of General Surgery. University Sapienza, Rome, Italy, 113University of Health Science Adana City Training and Research Hospital. General Surgery, Adana, Turkey, 114Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom, 115Royal Infirmary of Edinburgh, Department of General Surgery and Motol University Hospital, 3rd department of Surgery, EDINBURGH, United Kingdom, 116General and Digestive Surgery. Hospital Universitario de Jerez de la Frontera, Sevilla, Spain, 117General Surgery Unit, Molfetta Hospital, Molfetta, Italy, 118General surgery I, San Matteo Hospital, University of Pavia, Pavia, Italy, 119San Gerardo Hospital, Monza, Italy, 120Surgery Department, Tbilisi State Medical University, Georgia, 121Department of Neurosurgery, Royal Infirmary Edinburgh, Edinburgh, United Kingdom, 122Department of general surgery, General hospital Novi Pazar, Novi Pazar, Serbia and Montenegro, 123Department of Emergency and Organ Transplantation (DETO), University of Bari, Italy, Bari, Italy, 124Department of surgical, oncological and orale sciences—university of Palermo, Palermo, Italy, 125University of Catania, Catania, Italy, 126AOR San Carlo—Potenza—UOC Chirurgia Generale e Urgenza, POTENZA, Italy, 127AORN Cardarelli, ITALIA (IT), Italy, 128Dept of General Surgery, San benedetto del tronto Hospital, AV5, ASUR marche, San benedetto del tronto, Italy, 129Carol Davila University of Medicine and Pharmacy Bucharest, Emergency Hospital of Bucharest Romania, Bucharest, Romania, 130R Adams Cowley Shock Trauma, University of Maryland Medical Center, Baltimore, United States, 131Department of Emergency and Organ Transplant (DETO), University "Aldo Moro" Medical School of Bari, Bari, Italy, 132Department of Surgical Diseases, University Hospital "Prof. Dr. Stoyan Kirkovich", Stara Zagora, Bulgaria, 133Operative Unit of General Surgery Magenta Hospital, Milan, Italy, Magenta, Italy, 134University Hospital Virgen del Rocio, Seville, Spain, 135Sindh Institute of Urology and Transplant, Karachi, Pakistan, 136Department of Surgery, University of Medicine, Tirana, Albania, 137Department of logo Clinical Sciences and Community Health, University of Milan, Italy, 138Division of Vascular and Endovascular Surgery, Cardiovascular Department, University Hospital of Trieste ASUGI, Italy, Trieste, Italy, 139Department of General Surgery, Virgen del Rocao University Hospital, Seville, Spain, 1403rd Department of Surgery, 1st Medical Faculty of Charles University, Motol University Hospital, Prague, Czech Republic, 141Department of Surgery, Skane University Hospital, Lund & Malmö, Sweden, 142Surgery Lead. PIH Liberia, Harper, Liberia, 143Associate Professor of Emergency Medicine,Faculty of Medicine,Suez Canal University, Ismailia, Egypt, 144Tripoli University Hospital, Tripoli, Libya, 145University of Newcastle, Department of Traumatology John Hunter Hospital, Newcastle, Australia, 146Department of Hospital Surgery with the Course of Operative Surgery of KSMA named after I.K. Akhunbaeva, Bishkek, Kyrgyzstan, 147Emergency/Surgery department—Hospital Viedma, Cochabamba, Bolivia, 148General, Emergency surgery and New technologies, Baggiovara General Hospital,, Modena, Italy, 149ARNAS Brotzu, Cagliari, Italy, 150Hospital Universitario Severo Ochoa Leganes. Madrid. Spain, Madrid, Spain, 151Università degli studi di Pavia, Pavia, Italy, 152General Surgeon. Fundacia Althaia., Manresa, Spain, 153UOC Chirurgia Generale e d'Urgenza Ospedale M. Bufalini Cesena AUSL della Romagna, Cesena, Italy, 154General Surgery and Trauma Team, ASST Niguarda, Milan, Italy, 155Swiss Surgical Practice, Lugano, Switzerland, 156Pediatric Surgery Department, Vittore Buzzi Children's Hospital of Milan, Milan, Italy, 157Department of Human Pathology of the Adult and Evolutive Age "Gaetano Barresi", General and Emergency Surgery Unit, University of Messina, Messina, Italy, 158Acute Care Surgery Service of Hospital Vivalle, São José dos Campos, Brazil, 159General Surgery. La Paz University Hospital, Madrid, Spain, 160Università di Pisa, Pisa, Italy, 161AOU Careggi, Firenze, Italy, 162General Surgery Department, Saint Savvas Anticancer Hospital of Athens, Athens, Greece, 163Division of Trauma Surgery, University of Campinas, Campinas, Brazil, 164Chirurgia d'urgenza e del trauma. Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy, 165General Surgery I Unit, Fondazione IRCCS Policlinico San Matteo, Universita di Pavia, Pavia, Italy, 166Chirurgia oncologica ARNAS civico Palermo, Palermo, Italy, 167HPB Unit, Pederzoli Hospital, 37019 Peschiera del Garda, Italy, 168First Propaedeutic Department of Surgery, Medical School of Athens, National and Kapodistrian University of Athens, Hippocration General Hospital of Athens, Athens, Greece, 169Department of Abdominal Surgery, Vladimir City Emergency Hospital, Vladimir, Russia, 170Critical Care Unit, A Coruña, Spain, 171IHU Strasbourg, Strasbourg, France, 172Department of Medical Science, Oral and Biotecnology of University of Chieti-Pescara “G. d'Annunzio”, Chieti, Italy, 173Department of Surgery, Aminu Kano Teaching Hospital, Nigeria., Kano, Nigeria, 174Mansoura faculty of medicine, Man soura, Egypt, 175Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia, Kota Bharu, Malaysia, 176Department of surgery university of Manitoba, Winnipeg, Canada, 177Department of General Surgery Policlinico G.Rodolico, Catania, Italy, 178Department of Surgery, General Surgery Unit, S.Stefano Hospital, Prato, Italy, 179Department Valdoni; La Sapienza University of Rome, Roma, Italy, 180Università degli studi di Bari, Bari, Italy, 181Department of Surgery, AO Santa Croce e Carle, Cuneo, Italy, 182General Surgery Unit-Parma University Hospital, Parma, Italy, 183UOC Chirurgia Generale e d'Urgenza, Ospedale Santo Spirito in Sassia, Roma, Italy, 184Department of Surgery, State University of Londrina, Londrina, Brazil, 185Universidade Federal de Juiz de Fora, Minas Gerais, Juiz de Fora, Brazil, 186Surgery Unit, Faculdade de Ciências Médicas e da Saúde de Juiz de Fora – Suprema, Brazil, 187Centro Universitario Padre Albino, Catanduva—SP, Brazil, 188Sakarya university training and research hospital, Sakarya, Turkey, 189Department of Surgery, University of Witwatersrand, Johannesburg, South Africa, 190University Department of Anaesthesiology, Resuscitation and Intensive Care Medicine, Sveti Duh University Hospital, Zagreb, Croatia, 191General surgery, Hospital Universitari Parc Tauli, Sabadell, Spain, 192Dipartimento di Scienze Clinico-Chirurgiche, Diagnostiche e Pediatriche, Università degli studi di Pavia, Pavia, Italy, 193Department of Upper GI Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom, 194Emergency surgery department, Careggi University Hospital, Florence, Italy, 195 MU-Plovdiv- Prop. of Surgical Diseases, Plovdiv, Bulgaria, 196Aden university, Aden, Yemen, 197Department of Surgery, Kuwaiti Specialized Hospital, Khartoum, Sudan, 198Dept of Surgery, Nelson R Mandela School of Clinical Medicine, UKZN and Inkosi Albert Luthuli Central Hospital, Trauma and Burns Service, Durban, South Africa, 199Department of Surgery, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia, Kota Kinabalu, Malaysia, 200General Surgery, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom, 201Dept. of General & Thoracic Surgery, University Hospital of Giessen, Giessen, Germany, 202University Hospital Giessen, Germany, 203Cirugia de trauma, Hospital Central militar, Ciudad de México, Mexico, 204General surgery, CHUD, Universitu of Parakou, Parakou, Benin, 205Hospital Almenara—Lima, Lima, Peru, 206General and Digestive Surgery Unit, Hospital Universitari Vall d'Hebron, Barcelona, Spain, Barcelona, Spain, 207DEPARTMENT OF SURGERY, UNIVERSITI MALAYSIA SARAWAK, KUCHING, Malaysia, 208Manchester Foundation Trust, Manchester, United Kingdom, 209University of Insubria, Varese, Italy, 210General Surgery Department—Pederzoli Hospital, Peschiera del Garda, Italy, 2114th Department of Surgery, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece, 212General Surgery, Istanbul Medeniyet University, Istanbul, Turkey, 213Trauma and Orthopaedics Department, Royal Cornwall Hospital, Truro, United Kingdom, 214Queen Elizabeth Hospital-Birmingham, Department of Trauma&Orthopaedics, Birmingham, United Kingdom, 215Surgical Unit, Faculty of Medicine and Health Sciences, Universiti Sains Islam Malaysia, Nilai, Negeri Sembilan, Malaysia, 216Department of Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea, South, 217General Hospital of Larissa "Koutlimpaneio and Triantafylleio", Larissa, Greece, 218Department of Surgery, Tameside General Hospital, Manchester, United Kingdom, 219DDepartment of Surgery, Metaxa Cancer Hospital, Piraeus, Greece, 220University of Pennsylvania; Department of Surgery; Division of Trauma, Surgical Critical Care and Emergency Surgery, Philadelphia, United States, 221Health Sciences University, Kanuni Sultan Süleyman Training and Research Hospital, Istanbul, Turkey, 222School of Medicine, National and Kapodistrian University ofAthens, Greece, NKUA, Filothei, Greece, 223Surgical Clinic "Nikola Spasia", Faculty of Medicine University of Belgrade, Belgrade, Serbia and Montenegro, 224Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece, 225Department of General Surgery, Jubilee Mission Medical College & RI, Thrissur, India, 226Department of General and Digestive Surgery, Tampere University Hospital (TAUH), Hämeenlinna, Finland, 227Department of General, Gastrointestinal, Oncologic Surgery and Transplantology, Krakaw, Poland, 228Hillel Yaffe Medical Center, Hadera, Israel, 229Portsmouth Hospitals University NHS trust, Portsmouth, United Kingdom, 230Head surgeon, City Hospital, Mozyr, Belarus, 231Department of Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea, South, 232Departments of Surgery and Critical Care and the TeleMentored Ultrasound Supported Medical Interventions (TMUSMI) Research Group, Calgary, Canada, 233Fundacion Trauma, Ciudad AutÃ3noma de Buenos Aires, Argentina, 234Division of General Surgery, Rambam Health Care Campus, Haifa, Israel, 235Division of General Surgery, Rambam Health Care Campus, Haifa, 236Fujita Health University Hospital, Toyoake, Japan, 237Attikon hospital department of general surgery, Athens, Greece, 238Pengiran Anak Puteri Rashidah Saadatul Bolkiah Institute of Health Sciences, Universiti Brunei Darussalam, Bandar Seri Begawan, Brunei, 239Department of Surgery, University of KwaZulu Natal, Durban, South Africa, 240Department of Surgical Oncology Hellenic Anticancer Hospital, Athens, Greece, 241General Surgery, General Hospital of Larissa, Larissa, Greece, 242UMC Zvezdara, Clinic for Surgery, Belgrade, Serbia and Montenegro, 243Department of trauma surgery—University of Campinas, Campinas, Brazil, 244Kharkiv National Medical University, Department of Surgery No. 2, Kharkiv, Ukraine, 245Emergency Surgery and Trauma Unit, IRCCS Humanitas Research Hospital, Rozzano, Italy, 246Emergency and Critical Care Center, Kurashiki Central Hospital, Kurashiki, Japan, 247Surgery department. Urduliz Hospital, Urduliz, Spain, 248Department of Surgery "Pietro Valdoni", Sapienza University of Rome, Rome, Italy, 249Abdominal Center, Helsinki University Hospital and University of Helsinki, Finland, 250Department of Surgery. Buccheri La Ferla Hospital—Palermo, Palermo, Italy, 251Department of Surgery, Sant'Eugenio Hospital, Rome, Italy, 252Department of Surgical Disciplines, Immanuel Kant Baltic Federal University, Regional Clinical Hospital, Kaliningrad, Russia, 253General Surgery, Hospital Universitario Donostia, Donostia, Spain, 254General Surgery. Corporació Sanitària Parc Taulí, Sabadell, Spain, 255Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, 256Donostia University Hospital, San Sebastian, Spain, 257Department of Surgery, Kavala General Hospital, Kavala, Greece, 258Surgery Department, Mexico City, Mexico, 259General And Emergency Surgery—ASMN IRCCS Reggio Emilia, Reggio Emilia, Italy, 260Universidad Nacional de Asuncion, ASUNCIÓN, Paraguay, 261Department of Trauma and Orthopedic Surgery, Insitute for Research in Operative Medicine (IFOM), Cologne-Merheim Medical Center (CMMC), University Witten/Herdecke, Cologne, Germany, 262Nouvelle Clinique Vert, Geneve, Switzerland, 263General Surgery ASST Papa Giovanni XXIII, Bergamo, Italy, 264Surgery, Harborview Medical Center, University of Washington, Seatlle, WA, United States, 265Department of Sugery, Harborview Medical Center, University of Washington, Seattle, United States, 266Jagiellonian University Medical College, KrakÃ3w, Poland, 267General Surgery, Bangalore Medical College & Research Institute, Bangalore, India, 268University Hospital CAREGGI—Digestive Surgery Unit, Firenze, Italy, 269Sakarya University Research and Educational Hospital, Department of General Surgery, Sakarya, Turkey, 270Department of General Surgery, Ospedale degli Infermi, Rivoli, Rivoli, Italy, 271Gen and Emer Surg Department, Siena, Italy, 272Third Department of Surgery, Tzaneio General Hospital, Piraeus, Greece, 273Emergency Surgery Group—Departament of Surgery—University Hospital of Universidade Estadual de Ponta Grossa, Ponta Grossa, Brazil, 274Department of Architecture and Engineering, University of Pavia, Pavia, Italy, 275General Surgery Unit Azienda Ospedaliero Universitaria Policlinico, Bari, Italy, 276Department of General and Digestive Surgery. Hospital Universitario Doctor Peset., Valencia, Spain, 277Department of General and Digestive Surgery. Hospital Universitario Doctor Peset, Valencia, Spain, 278Cesena Hospital, Cesena, Italy, 279Institute of Image-Guided Surgery, IHU-Strasbourg, Strasbourg, France, 280Acute care surgery, Centre Hospitalier Universitaire de Nice, Universite Cote d'Azur, Nice, France, Nice, France, 281Department of Management, Ca' Foscari University of Venice, 282General Surgery of Princpe de Asturias Teaching, Alcalá de Henares, Spain, 283Department of Emergency Surgery, Sapienza University of Rome, Rome, Italy, 284UOC CHIRURGIA GENERALE, VITTORIO VENETO, Italy, 285Servisao Cirurgia Geral—Centro Hospitalar Universitario Sao Joao, Porto, Portugal, 286Hospital Universitario Principe de Asturias, Alcalá de Henares, Spain, 287Bagcilar training and research hospital / general surgery department, Ä°stanbul, Turkey, 288University Hospitals of Geneva, Geneva, Switzerland, 289IRCCS CRO di Aviano, Pain Medicine, Aviano (PN), Italy, 290Ass. Prof. of Surgery, Medical School, University of Athens, Greece, Athens, Greece, 291Department of Hepatobiliary and General Surgery, IRCCS Humanitas Research Hospital, Rozzano, Milan, Italy, 292Department of Surgery "Pietro Valdoni", Sapienza University of Rome, Rome, Italy, 293DEPARTMENT OF SURGERY AND DEPARTMENT OF TRAUMA AND EMERGENCY, ALL INDIA INSTITUTE OF MEDICAL SCIENCES, BHUBANESWAR, Bhubaneswar, India, 294Trauma and Orthopaedics, Raigmore Hospital, NHS Highlands, Inverness, United Kingdom, 295Trauma and Orthopaedic at Queen Elizabeth hospital, Birmingham, United Kingdom, 296Sandwell and West Birmingham NHS trust, Birmingham, United Kingdom, 297University Hospital Wishaw, Wishaw, United Kingdom, 298Department of Surgery, All India Institute of Medical Sciences, Mangalagiri, Guntur, Andhra Pradesh, India, 299Ernest E Moore Shock Trauma Center at Denver Health, Denver, United States, 300DEPARTMENT OF SURGERY. UNIVESITY HOSPITAL "MARQUES DE VALDECILLA", SANTANDER (CANTABRIA), Spain, 301Department of Surgery, and Department of Biomedical and Clinical Sciences, Linköping University, Norrköping, Sweden, 302Department of Surgery, General University Hospital of Patras, Patras, Greece, 303Northern Ireland medical and dental training, Belfast, United Kingdom, 304Sapienza University of Rome, Rome, Italy, 305Laboratory of Public Health Indicators Analysis and Health Digitalization, Moscow Institute of Physics and Technology, Dolgoprudniy, Russia, 306Trauma Center, Groote Schuur Hospital and University of Cape Town, Cape Town, South Africa, 307Carol Davila University of Medicine and Pharmacy Bucharest, Emergency Hospital of Bucharest Romania, Bucharest, Romania, 308Dipartimento di Medicina e Chirurgia Università di Milano Bicocca, Italy, 309Rocky Vista University, Parker, USA, 310General surgery and Pawi General Hospital, Pawi, Ethiopia, 311Department of Medical and Surgical Sciences and Translational Medicine, Sapienza University of Rome, Rome, Italy, 312Lewisham & Greenwich NHS Trust, London, United Kingdom, 313Department of Surgery Trinity College Dublin, Dublin, Ireland, 314Department of Surgery, University College Hospital, Ibadan, Ibadan, Nigeria, 315General surgery, Ospedale Borgomanero, Borgomanero (NO), Italy, 316Department of General and Oncologic Surgery. Policlinico San Marco, Zingonia (bg), Zingonia (Bg), Italy, 317Department of General Surgery, Hospital Bintulu, Bintulu, Malaysia, 318Urology Unit, Fondazione PTV Policlinico Tor Vergata, Rome, Italy, 319Research institute of emergency medicine n.a. I. I. Dzhanelidze, department of urgent surgery, Saint-Petersburg, Russia, 320Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kota Bharu, Kelantan, Malaysia, Kota Bharu, Malaysia, 321General Surgery, University of Sapienza, Rome, Italy, 322Department of Medical and Surgical Sciences University of Foggia, Foggia, Italy, 323Antimicrobial Stewardship Program; Bolzano Central Hospital, Bolzano, Italy, 324Department of clinical medicine and surgery, university of Naples, Federico II, Naples, Italy, 325Dept of Experimental and Clinical Medicine -University of Florence, Careggi University Hospital Florence, Italy, Florence, Italy, 3264th Department of Surgery, University Hospital Bratislava, Bratislava, Slovakia, 327Emergency Department ATTS Spedali Civili di Brescia, Brescia, Italy, 328Department of Medical and Surgical Sciences, University of Padova, Padova, Italy, 329Third Department of Surgery, Athens, Greece, 330Fourth Department of surgery,Attikon University Hospital, Athens, Greece, 3311st Surgical Department, General Hospital of Nikaia, Nikaia, Greece, 332General Surgery, Sant'Anna Hospital, Como, Italy, 333Dr Sulaiman Al Habib Hospital, Surgical Department, Riyadh, Saudi Arabia, 334Department of Surgery. Santa Casa School of Medical Sciences., Sao Paulo., Brazil, 335Department of Surgery, Western University, London, Canada, 336Nicola Giannettasio Hospital, Corigliano-Rossano, Italy, 337Department of surgery, Baroda Medical College and S.S.G. Hospital, Vadodara, India, 338Royal Infirmary University of Edinburgh, Edinburgh, United Kingdom, 339Department of Medical and Surgical Sciences—University of Foggia, Foggia, Italy, 340Division of General Surgery, of Emergency and New Technologies, Baggiovara Hospital, Modena, Italy, Modena, Italy, 341Department of Economics, Ca Foscari University, Venice, Italy, 342Department of Advanced Medical and Surgical Sciences, Università degli Studi della Campania "Luigi Vanvitelli", Naples, Italy, 343General and Digestive Surgery- University Hospital of Gran Canaria, Las Palmas de Gran Canaria, Spain, 344Divisions of Transplantation and Visceral Surgery, Department of Surgery, University of Geneva, Geneva, Switzerland, 345General Surgery Emergency and Trauma Surgery, Seville, Spain, 346Centro Hospitalar Barreiro Montijo, EPE, Barreiro, Portugal, 347Grupo Surgical, Campinas, Brazil, 348General surgery, Hospital Universitario Donostia, Donostia, Spain, 349Hospital Arnau de Vilanova . Colorrectal surgery, Lleida, Spain, 350Department of Medical, Surgical and Experimental Sciences, University of Sassari, Sassari, Italy, 351Depeartment of emergency surgery, Parma University Hospital, Parma, Italy, 352Delta Hospital, Azienda USL of Ferrara, Department of Surgery, University of Ferrara, Ferrara, Italy, 353General Surgery Residency Program, Tor Vergata University Rome, Rome, Italy, 354Azienda Sanitaria Provinciale di Vibo Valentia, Vibo Valentia, Italy, 355Department of Obstetrics and Gynecology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand, 356San Filippo Neri Hospital, ASL Roma 1, Roma, Italy, 357Department of Emergency and Organ Transplantation, University Aldo Moro of Bari, Bari, Italy, 358General surgery and emergency unit. Department of Surgery. AOU (azienda ospedaliero universitaria) of Modena, Modena, Italy, 359Neurosurgery Department, University of Padua, Padua, Italy, 360Department of Anesthesia and Intensive Care, Parma University Hospital, Parma, Italy, 361School of Medicine, National and Kapodistrian University of Athens (NKUA), Athens, Greece, 362Abdominal Surgery Dep., UMC Ljubljana and Medical Faculty Ljubljana, Ljubljana, Slovenia, 363Emergency and General Surgery—Ospedale dell'Angelo—ULSS3 Serenissima, Venezia, Italy, 364Calvary Public Hospital, Canberra, Australia, 365Department of Emergency Surgery, Cagliari University Hospital, Cagliari, Italy, 366Department of Medical, Surgical and Experimental Sciences, University of Sassari, Sassari, Italy, 367General Surgery, Ospedale Policlinico-Vittorio Emanuele, Catania, Italy, 368Department of Emergency and Organ Transplant (DETO), University "Aldo Moro" Medical School of Bari, Bari, Italy, 369Sapienza University of Rome, department of General Surgery and surgical specialties Paride Stefanini, Rome, Italy, 370Trauma Surgery, Hospital Santo Tomas, Panama, Panama, 371Research Unit fo Surgery, Odense University Hospital; Southern University of Denmark, Odense, Denmark, 372Universiti Sains Islam Malaysia, Nilai, Malaysia, 373Cirurgia, Hospital Prof Doutor Fernando Fonseca, Amadora, Portugal, 374Surgical Department, Universiti Sains Malaysia and Hospital USM, Kubang Kerian, Malaysia, 375Anadolu Medical Center, Kocaeli, Turkey, 376Department of General, Visceral, Thoracic, Transplant and Pediatric Surgery, University Hospital of Giessen, Giessen, Germany, 377Dep. of General, Visceral and Oncologic Surgery, Hospital and Clinics Wetzlar, Germany, Wetzlar, Germany, 378Division of Trauma, Emergency Surgery, and Surgical Critical Care, Boston, United States, 379University of Rome Tor Vergata, Roma, Italy, 380Surgical Research Fellow. Research Institute Against Digestive Cancer, IRCAD, Strasbourg, France, Strasbourg, France, 381Hospital del Trabajador, Surgery Department, Santiago, Chile, 382Department of General Surgery, Valduce Hospital, Como, Italy, 383UO Chirurgia Generale, Ospedale Ceccarini, Riccione, Italy, 384General Surgery, ASST Valle Olona, Busto Arsizio, Italy, 385Department of Surgery Universiti Sains Malaysia, Kota Bharu, Malaysia, 386Department of General and Emergency Surgery, San Filippo Neri Hospital, Rome, Italy, Roma, Italy, 387Neuroscience Institute, Universidad El Bosque, Cali, Colombia, 388Endocrine and Bariatric-Metabolic Surgery Department, Fuenlabrada Universitary Hospital, Madrid, Spain, 389Research Institute at Medical Institute Plovdiv, General Surgery Department, Plovdiv, 4000, Bulgaria, 390Hospital Vicente Corral Moscoso, Universidad del Azuay, Cuenca, Ecuador, 391Department of visceral surgery. Military teaching hospital., Dakar, Senegal, 392Consultant General surgeon,University hospitals, Leicester, United Kingdom, 393Trauma Team, San Carlo Borromeo Trauma Center, ASST Santi Paolo e Carlo, Milan, Italy, 394Hospital Universitario Virgen del Rocio, Sevilla, Spain, 395Consorci Sanitari Integral—Hospital Moises Broggi Sant Joan, Sant Joan DespÃ, Spain, 396Cesena Hospital, Cesena, Italy, 397Macerata hospital, 398General and Oncological Surgery Unit, Santa Croce and Carle Hospital, Cuneo, Cuneo, Italy, 399Ehime University Department of Emergency and Critical Care, TOON, Japan, 400Surgery Department, Putyla District Hospital, Putyla, Ukraine, 401Western michigan University Homer Stryker MD School of Medicine, Kalamazoo, United States, 402University of Turin, Turin, Italy, 403FIRST DEPARTMENT OF SURGERY, NATIONAL AND KAPODISTRIAN UNIVERSITY OF ATHENS, ATHENS, Greece, 404AOUI Verona Chirurgia Generale E dell'Esofago e dello Stomaco, Verona, Italy, 405IHU-Strasbourg, Institute of Image-Guided Surgery / Strasbourg University Hospitals, Department of General, Digestive and Endocrine Surgery, Strasbourg, France, 406Hospital de Clinicas. Universidad Nacional de Asuncion, San Lorenzo, Paraguay, 407Agios Andreas General Hospital of Patras, Patras, Greece, 408DIMEC, University of Bologna, Bologna, Italy, 409Department of Surgery. Miguel Servet University Hospital, Zaragoza, Spain, 410General Surgery, Tan Tock Seng Hospital, Singapore, Singapore, 411Surgical Infections Department Emergency Care Research Institute n.a. I.I.Djanelidze, Saint-Petersburg, Russia, 4124th Surgical Department, University Hospital Attikon, Athens, Greece, 413Universidade Federal de Juiz de Fora Campus Governador Valadares—UFJF/GV (Federal University of Juiz de Fora) and Universidade Vale do Rio Doce—Univale (Vale do Rio Doce University)., Governador Valadares—MG, Brazil, 414Department of Surgical Sciences, University of Roma Tor Vergata, Rome, Italy, 415Thammasat University Hospital, Pathum Thani, Thailand, 416University Hospital Eurohospital, Plovdiv, Bulgaria, 417Department of Medical and Surgical Sciences, University of Bologna, Forli, Italy, 418Ospedale Sacra Famiglia Fatebenefratelli, Erba, Italy, 419Department of Hospital Surgery with the Course of Operative Surgery of KSMA named after I.K. Akhunbaeva, Bishkek, Kyrgyzstan, 420Department of Gastrointestinal Surgery, Stavanger University Hospital, Norway, 421Surgical Department, Giannitsa General Hospital, Giannitsa, Pella, Greece, 422East Carolina University, Brody School of Medicine, Greenville, NC, United States, 423University of Alberta, Edmonton, Canada, 424Department of General Surgery, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia, Kota Kinabalu, Sabah, Malaysia, Malaysia, 425Chernivtsi Regional Emergency Hospital, Chernivtsi, Ukraine, 426Bukovinian State Medical University, Chernivtsi, Ukraine, 427Acute Care Surgery, Hamad Medical Corporation, Doha, Qatar, 428Surgery Department. Virgen del Rocio University Hospital, Sevilla, Spain, 429Gastrointestinal Surgery IRCCS San Raffaele Scientific Institute, Milan, Italy, 430Asst Monza—Ospedale San Gerardo, Colorectal surgery unit, Monza, Italy, 431Department of Surgery, Radboudumc, Nijmegen, Netherlands, 432HSAJB, Johor Bahru, Malaysia, 433Emergency Surgery Department, Parma University Hospital, Parma, Italy, 434Department of Medical and Surgical Sciences—University of Foggia, Foggia, Italy, 435Università degli studi di Pavia, Italy, 436Emergency Surgery Unit & Trauma Center, Pisa University Hospital, University of Pisa, Pisa, Italy, 437Department of Surgery. University Hospital Aintree, Liverpool, United Kingdom, 438Digestive and Emergency Surgery Unit, Azienda Ospedaliera S.Maria, Terni, Italy, 439Departamento de cirurgia—UNIFIPA, Catanduva—SP, Brazil, 440Dept. Of Trauma, University Hospital Zurich, Zurich, Switzerland, 441Department of Surgery, Aretaieio University Hospital Athens, Athens, Greece, 442Abdominal Center, Helsinki University Hospital and University of Helsinki, Helsinki, Finland, 443Department of Emergency and Organ Transplant (DETO), University "Aldo Moro" Medical School of Bari, Bari, Italy, 444General Surgery, Augusta Hospital, Syracusa, Italy, Italy, 445Chirurgia Tratto Alimentare, IRCCS Policlinico Sant'Orsola, Bologna, Italy, 446UGI Senior Clinical Fellow,Department of Surgery,Royal Infirmary of Edinburgh, Edinburgh, United Kingdom, 447General Surgery Unit, Azienda Ospedaliero Universitaria Policlinico di Bari, Italy, Italy, 448Azienda ospedaliera universitaria Verona, Verona, Italy, 449Hospital Maciel, Montevideo, Uruguay, 450Sismanoglio General Hospital, Athens, Athens, Greece, 451General and Digestive Surgery, Fundacio Sanitaria Mollet, Mollet del Valles, Spain, 452Chirurgia 3, AOU Città della Salute e della Scienza di Torino, Torino, Italy, 453San Marco Hospital GSD, Zingonia (BG), Italy, 454Department of Special surgery, Medical university Plovdiv, Plovdiv, Bulgaria, 455GENERAL SURGERY DEPARTMENT-GALDAKAO UNIVERSITY HOSPITAL/BIOCRUCES BIZKAIA HEALTH RESEARCH INSTITUTE, GALDAKAO-USANSOLO, Spain, 456Department of gastroenterology and alimentary tract surgery, Tampere University Hospital, Tampere, Finland, 4571st Department of surgery, Laiko General hospital, Athens, Greece, 4584th Surgical Department, Attikon Hospital, National and Kapodistrian University of Athens, Haidari-Athens, Greece, 459IHU-Strasbourg, Institute of Image-Guided Surgery, Strasbourg, France, 460Critical Care Unit. Complexo Hospitalario Universitario A Coruna, A Coruña, Spain, 461Harvard Medical School, Boston, USA, 462Hospital Universitario Austral, Pilar, Argentina, 463Institute of Image-Guided Surgery, IHU Strasbourg, Strasbourg, France, 464Department of Medical and Surgical Sciences and Advanced Technologies, University of Catania, Italy, Catania, Italy, 465General Surgery 1, Fondazione IRCCS Policlinico San Matteo, Pavia, Pavia, Italy, 466Professor of Surgery at Universitat autonoma de Barcelona Consultant Surgeon at Vall Hebron Hospital Endocrine-Metabolic and Bariatric Unit. Robotic Surgery. Vall Hebron Barcelona Hospital Campus. Pg. De la Vall d'hebron, 119-129 080035 Barcelona, BARCELONA, Spain, 467Chirurgia Generale d'Urgenza e PS—AOU Città della Salute e della Scienza, Torino (Turin), Italy, 468Department of Anesthesia and Critical Care, ARCO Roma, IRCCS Ospedale Pediatrico Bambino Gesù, Rome, Italy, 469Department of General, Oncological, Metabolic and Thoracic Surgery, Military Institute of Medicine, Warsaw, Poland, 470Department of Surgery, Faculty of Medicine Siriraj hospital, Mahidol university, Bangkok, Thailand, 471Department of Visceral Surgery and Medicine, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland, 472Department of General Surgery, Forth Valley Royal Hospital, Larbert, United Kingdom, 473Department of Surgery, Spaarne Gasthuis, Hoofddorp, The Netherlands, 474Duke-National University of Singapore, Singapore, Singapore, 475Department of Surgery. University Hospital of Heraklion Crete, Heraklion Crete, Greece, 476Trauma surgery, Gachon University Gil Medical center, Incheon, Korea, South, 477Royal Infirmary University of Edinburgh, Edinburgh, United Kingdom, 478Department of General & Minimal Access Surgery, KIMS-Kerala Institute of Medical Sciences, Trivandrum, India, 479General Surgery, St.Andrew Hospital, Patra, Greece, 480Chirurgia Generale, ospedale San Bortolo, Vicenza, Italy, 481Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Kelantan, Malaysia, 482Departamento de Cirugia, Sociedad de Lucha Contra el Cancer—SOLCA, Guayaquil, Ecuador, 483Third surgical department -Tzaneio hospital, Piraeus, Greece, 484Department of Orthopaedic and Trauma Surgery, Campus Bio-Medico University Hospital, Rome, Italy, 485Università di Pavia, Unit of general surgery, Pavia, Italy, 486Department of Economics, Ca Foscari University, Venice, Italy, 4874th Surgical Clinic Aristotle University of Thessaloniki, Thessaloniki, Greece, 488Department of Surgical, Oncological and Gastroenterological Sciences-Urological Clinic, University of Padua, Padua, Italy, 489ULSS5 Polesana Department of General Surgery, Santa Maria della Misericordia Hospital, Rovigo, Italy
Funding
There are no funds to be reported.
Author information
Authors and Affiliations
Consortia
Contributions
LC and FDM conceived the idea of the study. LC and FDM wrote the research protocol. LC, FDM, LA, FaCa, SD, HK, TJL, and PP reviewed the research protocol. LC and FDM took care of the data collection. LC, DP, and FDM took care of the data analysis. LC, FDM, DP, and TJL wrote the first draft of the manuscript. VA, LA, JB, WB, GB, FaCa, FeCo, SD, BDS, IF, PF, GiM, GRM, JM, MM, PP, FR, AV, and HK critically reviewed the manuscript. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Ethical approval and consent to participate.
Not needed.
Consent for publication
Not applicable. The manuscript does not contain data from any person.
Competing interests
The authors declare that they have no competing interests in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: in PubMed the author name Daniele Bissacco under Team Dynamics Study Group has not been tagged and now it has been rectified.
Appendix 1
Appendix 1


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cobianchi, L., Piccolo, D., Dal Mas, F. et al. Surgeons’ perspectives on artificial intelligence to support clinical decision-making in trauma and emergency contexts: results from an international survey. World J Emerg Surg 18, 1 (2023). https://doi.org/10.1186/s13017-022-00467-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-022-00467-3