Abstract
Objectives
Surgical correction of skeletal maxillary retroposition is often associated with changes in the morphology of the nose. Unwanted alar flaring of the nose is observed in many cases. The aim of the present study was therefore to investigate the influence of surgical advancement of the maxilla on changes in the soft-tissue morphology of the nose. Having a coefficient that allows prediction of change in the nasal width in Caucasian patients after surgery would be helpful for treatment planning.
Materials and methods
All 33 patients included in this retrospective study were of Caucasian descent and had skeletal Class III with maxillary retrognathia. They were all treated with maxillary advancement using a combination of orthodontic and maxillofacial surgery methods. Two cone-beam computed tomography (CBCT) datasets were available for all of the study's participants (16 female, 17 male; age 24.3 ± 10.4 years): the first CBCT imaging was obtained before the planned procedure (T0) and the second 14.1 ± 6.4 months postoperatively (T1). Morphological changes were recorded three-dimensionally using computer-aided methods (Mimics (Materialise NV, Leuven/Belgium), Geomagic (Geomagics, Morrisville/USA)). Statistical analysis was carried out using SPSS 21 for Mac.
Results
The mean sagittal advancement of the maxilla was 5.58 mm. The width of the nose at the alar base (Alb) changed by a mean of + 2.59 mm (±1.26 mm) and at the ala (Al) by a mean of + 3.17 mm (±1.32 mm). Both of these changes were statistically highly significant (P = 0.000). The increase in the width of the nose corresponded to approximately half of the maxillary advancement distance in over 80 % of the patients. The nasolabial angle declined by an average of −6.65° (±7.71°).
Conclusions
Maxillary advancement correlates with a distinct morphological change in nasal width. This should be taken into account in the treatment approach and in the information provided to patients.
Similar content being viewed by others
Introduction
Changes in the position of the maxilla and/or mandible are associated with corresponding changes in the soft tissue overlying the bone [1]. After surgical correction of maxillary retrognathia with maxillary advancement or bimaxillary surgery, with maxillary advancement and mandibular setback, undesirable changes in the nose have been observed in some cases. For many patients, a disturbing aesthetic appearance is the reason for undergoing surgery, in addition to functional problems [2]. It has been clinically and scientifically proven that the external nose undergoes changes in the context of surgical relocation of the maxilla [3]. This aspect should be examined in greater detail, and it would be of interest to know in what way advancement of the maxilla leads to alar flaring. Measurement of a coefficient capable of relating the skeletal displacement to nasal changes might be helpful for surgical planning and patient education.
The effect of maxillofacial surgery on the facial soft tissue has been investigated in many studies in the past [1, 4–16]. However, there is a lack of research on the relationship between the advancement distance and the amount of alteration measured [10, 17, 16]. A wide variety of analyses have been used for the purpose. The methods most often used in the past have included photography and two-dimensional lateral cephalography [18–21]. Recently, various optical procedures such as laser projection, glancing-light projection, and stereophotogrammetry have made it possible to capture spatial, three-dimensional parameters [18, 22, 23]. In radiography, computed tomography (CT) and cone-beam computed tomography (CBCT) can be used [18, 22–24]. In contrast to optical procedures, radiographic methods are not limited to depicting only the surface of the body; deeper bone structures can also be captured. Three-dimensional changes in the osseous structures and the resulting changes in the soft tissues can be analyzed using CBCT.
Only patients of Asian descent have previously been investigated in connection with this topic [8, 11, 13, 15, 16, 25–27, 14]. Due to ethnic differences in facial structure, it is not possible to transfer the findings to Caucasian patients [26]. It is regarded as clinically and scientifically proven that the external nose is subject to flattening and widening when surgical repositioning is carried out in the maxilla.
The aim of the present study was therefore to use three-dimensional CBCT data to detect dependencies between skeletal advancement of the maxilla and alterations in the morphology of the nose. In the case of a confirmed association, the aim was to evaluate whether any dependency on the extent of the advancement could be identified.
Materials and methods
Two CBCT datasets for each of 33 patients (16 female, 17 male) — i.e., a total of 66 CBCTs — were examined retrospectively. The patients’ mean age was 24.3 ± 10.4 years. All of the patients had an Angle class III anomaly with maxillary retrognathia preoperatively. They were examined clinically and radiographically in the Department of Oral and Maxillofacial Surgery in Bad Homburg, Germany, and were of Caucasian descent.
Weight variations of more than 5 kg were not permitted during the study period. This information was obtained from the anesthesia protocol. The following inclusion and exclusion criteria were set. The criteria for inclusion in the patient group were:
-
Caucasian descent
-
Maxillary retrognathia (SNA < 80°)
-
Surgical advancement of the maxilla
-
During the preoperatively conducted model operation, available current plaster jaw models had to allow stable occlusion in Angle class I
The criteria for exclusion from the patient group were:
-
No maxillary retrognathia (SNA > 80°)
-
Not of Caucasian descent
-
Additional intraoperative augmentation of the midface
-
Craniofacial anomalies or syndromes, or any form of cheilognathouranoschisis
Surgically, a Le Fort I osteotomy of the maxilla in combination with bridle sutures for the bases of the two ala was used [16, 17, 28, 29]. The Le Fort I osteotomy method used by the surgeon (exclusively W.K.) is based on the fracture line described by René Le Fort in 1901 [30]. The osteotomy starts at the piriform aperture cranial to the anterior nasal spine and passes through the facial maxillary sinus wall, the zygomaticoalveolar crest, and the maxillary tuberosity to the dorsal surface of the maxillary sinus, separates the caudal tip of the pterygoid process of the sphenoid bone, bends forward to the nasal cavity, runs through the lateral nasal wall in its basal portion, and from there returns to the piriform aperture [30]. After repositioning of the maxilla using the face-bow and glabella support, or with a surgical splint prepared in advance to determine the occlusal relationship of the maxilla to the mandible, the maxilla is fixed in its final position using an adapted titanium mini-plate and accompanying screws. In addition, alar cinch sutures are created for the bases of the two nostrils and attached with this technique at the anterior nasal spine [17, 3, 29, 28]
All 33 patients underwent maxillary advancement. A bimaxillary operation with maxillary advancement and mandibular setback was carried out in the majority of the patients. Table 1 presents an overview of the additional surgical procedures used and their frequencies.
The first CBCT imaging procedure was carried out 2–3 weeks before the planned procedure (T0). The second images were obtained after surgery (T1; 14.1 ± 6.4 months postoperatively), but not before the completion of soft-tissue healing. Completion of soft-tissue healing was defined as 6 months after surgery, based on the results of earlier studies [31, 32].
Identical parameters were used for all CBCT imaging procedures. All of the CBCT images were taken with a KaVo 3D eXam device (KaVo Dental Ltd., Bieberach/Riss, Germany). This CBCT device has a high-frequency X-ray source with a constant potential of 120 kVp (kilovolt peak) and pulsed 3–8 mA. The settings used for all of the CBCT imaging procedures were identical, with a scanning time of 26.9 s, a voxel size of 0.25 × 0.25 × 0.25 mm, an effective irradiation period of 7 s, anode voltage of 120 kV, and tube current of 5 mA (for details, see KaVo). The maximum field of view (FOV) of the device was 16 × 13 cm. Depending on the issue and indication, the height of the FOV was 6, 8, or 11 cm and the image had to include all relevant points.
All of the patients provided written informed consent to the inclusion of their data in the study. The data were pseudonymized. The CBCT datasets were given identifiers numbered 1–66 and the underlying names of the patients were deleted. Deallocation was only permissible for the director of the study (HKS).
Collection and analysis of the soft-tissue datasets were carried out using the Mimics 15.0 (Materialise NV, Leuven/Belgium) computer program. Table 2 shows all of the relevant points, distances, planes, and angles.
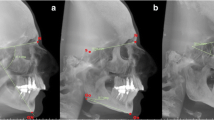
The nasolabial angle (NLA [33]), alar base width (Alb), and alar width (Al) were measured to assess changes in the nasal soft tissues. The soft-tissue points shown in Fig. 1 were used for measurements. The following distances and angles were formed from the measurement points:
-
Alar base width (Alb): from Albr to Albl: Alb distance
-
Alar width (Al): from All to Alr: Al distance
-
Nasolabial angle (NLA): angle between Ls to Co and Sn
Soft-tissue points and distances. The nasolabial angle (NLA) is the angle between the labrale superius (Ls), the columellar tangential point (Co), and the subnasal point (Sn). The alar base width (Alb) is the distance from the alar base on the right (Albr) to the alar base on the left (Albl). The alar width (Al) is the distance from the right ala (Alr) to the left ala (All)
For measurement of the skeletal repositioning of the maxilla, the CBCT for T0 and T1 were superimposed using Geomagic Control 2014.0 (Geomagics, Morrisville, USA). Superimposition was carried out at the foramen magnum with surrounding bone and at the anterior skull base at 100,000 polygons [34, 35] (Fig. 2). Figure 3 shows the user interface in Geomagic Control after completion of the superimposition. A level parallel with the Frankfurt plane was placed through the A point (Fig. 4). At this level, individual measurement values were collected in regions 13, 11, 21, and 23 in the needle view, and a mean was calculated (Fig. 5). The calculated repositioning of these points represents the skeletal advancement of the maxilla. All of the measurements were repeated by the same operator after an interval of 2 weeks.
Statistics
Statistical analysis was performed using IBM SPSS Statistics for Mac, version 21.0 (IBM Corporation, Armonk, New York, USA). Methodological error was estimated using Spearman rank correlation. As the Shapiro-Wilk test showed significant deviations from the normal distribution, Student’s t-test and the Wilcoxon test were carried out. The significance level was set at P < 0.05.
Using SPSS, a formula was generated to calculate the amount of change in the width of the nose. A regression between the amount of maxillary advancement and the widening of the ala and alar base was prepared by transformation of the sagittal displacement distance with the square root and soft-tissue enlargement with the logarithm. The transformed variables followed a sufficiently Gaussian normal distribution. The relation of the transformed values was not purely linear, but curved. A second-degree polynomial was used to calculate the regression.
Results
The reproducibility of the measurement values represented by Spearman rank correlation showed highly significant correlations (P = 0.000) (Tables 3). The mean sagittal repositioning of the maxilla was 5.58 mm. The calculated smallest repositioning distance was 2.02 mm and the largest distance was 10.84 mm (Table 4).
The width of the nose increased highly significantly between T0 and T1 as a result of the maxillary advancement (P = 0.000). As Table 5 shows, highly significant changes in the alae (Al), alar base (Alb), and nasolabial angle (NLA) were observed (P = 0.000). The alar width Al (mean + 3.17 ± 1.32 mm) increased in all 33 patients. The alar base width Alb (mean + 2.59 ± 1.26 mm) also increased. The nasolabial angle declined in 28 patients and increased in five patients (mean −6.65° ± 7.71°). As Table 6 shows, the increases in the width of the alar base and alar width correlated highly significantly with the skeletal advancement of the maxilla (P = 0.000).
The change in the nasolabial angle was not entirely independent of the sagittal repositioning, but this was not statistically significant (P > 0.05).
Based on the results, the following formulas were developed to allow prediction of soft-tissue changes relative to skeletal advancement:
Alar base width:
-
Patients (n = 33), regression coefficient R2 = 0.4764, standard deviation s = 0.1338959
-
Formula for y = ∆Alb in the course of x = maxillary advancement:
-
log(ΔAlb) = 0.4558889 + 0.124167 × z + 0.010571 × z2, where z = (√(maxillary advancement) – 2.305)/0.5255
-
Alar width:
-
Patients (n = 33), regression coefficient R2 = 0.5281, standard deviation s = 0.1403169
-
Formula for y = ∆Alin the course of x = maxillary advancement:
-
log (ΔAl) = 0.3704371 + 0.1435941 × z − 0.001474 × z2, where z = (√(maxillary advancement) – 2.305) / 0.5255
-
Advancement by 5 mm would thus lead to a mean widening of the alar base of ≈ 2.8 mm. Ninety percent of the patients would have widening of between ≈ 1.7 mm and ≈ 4.6 mm (Table 7). As Table 8 shows, advancement of 5 mm would lead to a mean widening of the ala of ≈ 2.2 mm. Ninety percent of the patients could expect widening of between ≈ 1.3 mm and ≈ 3.8 mm.
Discussion
Investigations have been carried out since the 1980s to analyze associations between changes occurring in the facial soft tissue in connection with Le Fort I osteotomies in dysgnathia surgery. A correlation between sagittal repositioning of the maxilla and the amount of alar flaring was not identified at that time [36]. Preoperative and postoperative lateral cephalograms or photographs were used for measurements in the early studies [10]. However, these techniques did not allow any conclusions to be drawn regarding correlations with the changing width of the nose [11].
Three-dimensional measurement of hard-tissue models obtained from CBCT and CT imaging is now increasingly being used, mainly for the planning of dental implants in dental medicine [37]. The amount of correlation between the initial measurements and control measurements of the soft tissue after 2 weeks is highly significant. Discussion is needed on mistakes during the reproducibility of these measurements. The reproducibility and reliability of different measurement points on lateral cephalograms has been frequently investigated in the past and has also been classified [38–40]. Similar findings were obtained with measurement points derived from lateral cephalograms created with CBCT [41]. The measurement points created on three-dimensional surfaces using CBCT scans are thus regarded as being highly reliable [42–44].
The sagittal movement of the maxilla was registered on a plane parallel to the Frankfurt plane. In 2012, Daboul et al. reported that the reproducibility and reliability of the Frankfurt plane on 3D multiplanar reformatting (MPR) images was excellent [45]. Similar results were described by Ludlow et al. in 2009, who found amongst other things that identification of cephalometric landmarks is significantly more precise with MPR views of CBCT landmarks [46].
The first analysis of soft-tissue areas on the basis of three-dimensional CBCT reconstructions was reported by Han et al. in 2005. However, the patients included in the study were all of Asian descent [25]. In 2010, Kim et al. also investigated 3D reconstructions from CBCT images after repositioning of the maxilla at the Le Fort I level [47]. However, transverse changes in the size of the nose were not investigated. In 2012, the topic was again addressed by Park et al. using a new method, and transverse changes in the size of the nose were measured. The study also only included patients of Asian descent [14]. Farkas et al. noted that Asian individuals tend to have a nasal morphology that is very different from that in Caucasians [26, 48]. Direct comparison thus does not appear useful. In contrast to other publications, the present study therefore only includes patients of Caucasian descent and exclusively patients with maxillary retrognathic position. The results of the measurements of the width of the nose before surgical intervention were also compared with the results presented by Farkas. The T0 results were very similar to those of Farkas et al. in relation to the anthropometric measurements of Caucasian noses.
Measurement of soft-tissue models obtained from CBCTor CT imaging using Mimics has been confirmed as a valid method in various studies [49, 50]. Correlation of the initial measurements and follow-up measurements in the present study also showed that the measurement method is extremely accurate.
Using 3D radiographic evaluation, the present study shows that the transverse size of the nose increases when the maxilla is advanced during Class III surgical correction of occlusion anomalies. This result is also supported by the 3D photographic studies reported by Honrado et al. in 2006 [5]. A considerable disadvantage with the use of methods based on conventional light is that only the skin is detected as a surface, with no information about the underlying structures. In addition, the undercutting (“shadow”) that is produced by conventional light during detection of a three-dimensional surface can make evaluation impossible in some areas [23, 24]. These problems can be avoided with three-dimensional radiographic methods such as CBCT. Thanks to the different physical properties of skin and bone, the skin remains in the field of view when the underlying bone is being examined. In addition, CBCT produces an image that is true to scale, and undercutting does not occur.
The use of ionizing radiation for evaluation of a problem that is primarily aesthetic in nature may be questioned. It should be noted here that there is no indication for CBCT in the evaluation of soft tissue. Instead, when CBCT is required in any case for another indication, its findings can be enhanced using the techniques described here.
Overall, the results appear to be of major importance for everyday clinical purposes, since according to Göz et al., a poor aesthetic appearance is the most important reason why patients decide to undergo surgery for dysgnathia [2]. Subsequent widening of the nose is often regarded as an undesirable aesthetic change [2, 51]. If functional aspects allow it, the initial shape of the nose and the amount of maxillary advancement should be taken into account during the planning of the operation [27, 52, 28].
In addition to the usual information provided before surgery, it should therefore also be drawn to the patient’s attention that the morphology of the external nose changes postoperatively and that surgical correction of the nose may become necessary later on [27, 52, 53]. The three-dimensional alteration coefficient of approximately 50 % calculated in the present study (with 1 mm of sagittal advancement of the maxilla equaling an increase in the width of the nose by 0.5 mm) could be used for preoperative assessment of the potential change.
The nasolabial angle decreases in most cases after sagittal repositioning, but there was no statistically significant correlation.
Conclusions
Maxillary advancement has effects on nasal morphology in individuals of Caucasian descent. The widening of the nose and narrowing of the nasolabial angle demonstrated in the present study may have a negative influence on the postoperative aesthetic result and should therefore be taken into account both in treatment planning and also in the information provided to patients. The correlation coefficient calculated between sagittal advancement and soft-tissue changes in the nose may make prediction easier.
Ethical considerations
The study was compiled with the rules laid down by the Declaration of Helsinki. It was explained to the patients that inclusion of their data in the study was voluntary and that confidentiality and anonymity were guaranteed. They were also able to withdraw from the study at any time before publication without needing to give any reason. Written informed consent was obtained from all of the participants.
Abbreviations
- Al:
-
Alar width
- Alb:
-
Alar base width
- Albl:
-
Alar base on the left
- Albr:
-
Alar base on the right
- All:
-
Left ala
- Alr:
-
Right ala
- CBCT:
-
Cone-beam computed tomography
- Co:
-
Columellar tangential point
- CT:
-
Computed tomography
- FOV:
-
Field of view
- Ls:
-
Labrale superius
- MPR:
-
Multiplanar reformatting
- NLA:
-
Nasolabial angle
- Sn:
-
Subnasal point
- SNA:
-
Sella-nasion-A point angle
References
Baik HS, Kim SY. Facial soft-tissue changes in skeletal Class III orthognathic surgery patients analyzed with 3-dimensional laser scanning. Am J Orthod Dentofacial Orthop. 2010;138(2):167–78. doi:10.1016/j.ajodo.2010.02.022.
Göz G. Die Motivation bei kieferorthopädischen Operationen. Freiburg i. Br: Albert-Ludwigs-Universität Freiburg i. Br; 1981.
Guymon M, Crosby DR, Wolford LM. The alar base cinch suture to control nasal width in maxillary osteotomies. Int J Adult Orthodon Orthognath Surg. 1988;3(2):89–95.
Choi JW, Lee JY, Oh TS, Kwon SM, Yang SJ, Koh KS. Frontal soft tissue analysis using a 3 dimensional camera following two-jaw rotational orthognathic surgery in skeletal class III patients. J Craniomaxillofac Surg. 2013. doi:10.1016/j.jcms.2013.05.004.
Honrado CP, Lee S, Bloomquist DS, Larrabee Jr WF. Quantitative assessment of nasal changes after maxillomandibular surgery using a 3-dimensional digital imaging system. Arch Facial Plast Surg. 2006;8(1):26–35. doi:10.1001/archfaci.8.1.26.
Hwang DS, Kim YI, Park SB, Lee JY. Midfacial soft tissue changes after leveling Le Fort I osteotomy with differential reduction. Cone-beam computed tomography volume superimposition. Angle Orthod. 2012;82(3):424–31. doi:10.2319/052411-342.1.
Johnson BM, McNamara JA, Bandeen RL, Baccetti T. Changes in soft tissue nasal widths associated with rapid maxillary expansion in prepubertal and postpubertal subjects. Angle Orthod. 2010;80(6):995–1001. doi:10.2319/033110-179.1.
Kim YI, Park SB, Son WS, Hwang DS. Midfacial soft-tissue changes after advancement of maxilla with Le Fort I osteotomy and mandibular setback surgery: comparison of conventional and high Le Fort I osteotomies by superimposition of cone-beam computed tomography volumes. J Oral Maxillofac Surg. 2011;69(6):e225–33. doi:10.1016/j.joms.2010.12.035.
Lee JY, Kim YI, Hwang DS, Park SB. Effect of setback Le Fort I osteotomy on midfacial soft-tissue changes as evaluated by cone-beam computed tomography superimposition for cases of skeletal Class III malocclusion. Int J Oral Maxillofac Surg. 2013;42(6):790–5. doi:10.1016/j.ijom.2012.11.012.
Radney LJ, Jacobs JD. Soft-tissue changes associated with surgical total maxillary intrusion. Am J Orthod. 1981;80(2):191–212.
Mansour S, Burstone C, Legan H. An evaluation of soft-tissue changes resulting from Le Fort I maxillary surgery. Am J Orthod. 1983;84(1):37–47.
McCance AM, Moss JP, Fright WR, James DR, Linney AD. A three dimensional analysis of soft and hard tissue changes following bimaxillary orthognathic surgery in skeletal III patients. Br J Oral Maxillofac Surg. 1992;30(5):305–12.
Mommaerts MY, Lippens F, Abeloos JV, Neyt LF. Nasal profile changes after maxillary impaction and advancement surgery. J Oral Maxillofac Surg. 2000;58(5):470–5. discussion 5–6.
Park SB, Yoon JK, Kim YI, Hwang DS, Cho BH, Son WS. The evaluation of the nasal morphologic changes after bimaxillary surgery in skeletal class III maloccusion by using the superimposition of cone-beam computed tomography (CBCT) volumes. J Craniomaxillofac Surg. 2012;40(4):e87–92. doi:10.1016/j.jcms.2011.05.008.
Ryckman MS, Harrison S, Oliver D, Sander C, Boryor AA, Hohmann AA, et al. Soft-tissue changes after maxillomandibular advancement surgery assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S86–93. doi:10.1016/j.ajodo.2009.03.041.
Westermark AH, Bystedt H, Von Konow L, Sallstrom KO. Nasolabial morphology after Le Fort I osteotomies. Effect of alar base suture. Int J Oral Maxillofac Surg. 1991;20(1):25–30.
Collins PC, Epker BN. The alar base cinch: a technique for prevention of alar base flaring secondary to maxillary surgery. Oral Surg Oral Med Oral Pathol. 1982;53(6):549–53.
Rustemeyer J, Martin A. Soft tissue response in orthognathic surgery patients treated by bimaxillary osteotomy: cephalometry compared with 2-D photogrammetry. Oral Maxillofac Surg. 2013;17(1):33–41. doi:10.1007/s10006-012-0330-0.
Kajikawa Y. Changes in soft tissue profile after surgical correction of skeletal class III malocclusion. J Oral Surg. 1979;37(3):167–74.
Lin SS, Kerr WJ. Soft and hard tissue changes in Class III patients treated by bimaxillary surgery. Eur J Orthod. 1998;20(1):25–33.
Kinzinger G, Frye L, Diedrich P. Class II treatment in adults: comparing camouflage orthodontics, dentofacial orthopedics and orthognathic surgery--a cephalometric study to evaluate various therapeutic effects. J Orofac Orthop. 2009;70(1):63–91. doi:10.1007/s00056-009-0821-2.
Verze L, Bianchi FA, Schellino E, Ramieri G. Soft tissue changes after orthodontic surgical correction of jaws asymmetry evaluated by three-dimensional surface laser scanner. J Craniofac Surg. 2012;23(5):1448–52. doi:10.1097/SCS.0b013e31824e25fc.
Holberg C, Heine AK, Geis P, Schwenzer K, Rudzki-Janson I. Three-dimensional soft tissue prediction using finite elements. Part II: Clinical application. J Orofac Orthop. 2005;66(2):122–34. doi:10.1007/s00056-005-0422-7.
Holberg C, Schwenzer K, Rudzki-Janson I. Three-dimensional soft tissue prediction using finite elements. Part I: Implementation of a new procedure. J Orofac Orthop. 2005;66(2):110–21. doi:10.1007/s00056-005-0421-8.
Han SY, Baik HS, Kim KD, Yu HS. Facial soft tissue measuring analysis of normal occlusion using three-dimensional CT imaging. Korean J Orthod. 2005;35(6):409–19.
Farkas LG, Katic MJ, Forrest CR, Alt KW, Bagic I, Baltadjiev G, et al. International anthropometric study of facial morphology in various ethnic groups/races. J Craniofac Surg. 2005;16(4):615–46.
Altman JI, Oeltjen JC. Nasal deformities associated with orthognathic surgery: analysis, prevention, and correction. J Craniofac Surg. 2007;18(4):734–9. doi:10.1097/SCS.0b013e3180684328.
Rauso R, Freda N, Curinga G, Del Pero C, Tartaro G. An alternative alar cinch suture. Eplasty. 2010;10, e69.
Millard Jr DR. The alar cinch in the flat, flaring nose. Plast Reconstr Surg. 1980;65(5):669–72.
Tessier P. The classic reprint: experimental study of fractures of the upper jaw. 3. Rene Le Fort, M.D., Lille, France. Plast Reconstr Surg. 1972;50(6):600–7.
Kau CH, Cronin A, Durning P, Zhurov AI, Sandham A, Richmond S. A new method for the 3D measurement of postoperative swelling following orthognathic surgery. Orthod Craniofac Res. 2006;9(1):31–7. doi:10.1111/j.1601-6343.2006.00341.x.
Oh KM, Seo SK, Park JE, Sim HS, Cevidanes LH, Kim YJ, et al. Post-operative soft tissue changes in patients with mandibular prognathism after bimaxillary surgery. J Craniomaxillofac Surg. 2013;41(3):204–11. doi:10.1016/j.jcms.2012.09.001.
Legan HL, Burstone CJ. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38(10):744–51.
Cevidanes LH, Motta A, Proffit WR, Ackerman JL, Styner M. Cranial base superimposition for 3-dimensional evaluation of soft-tissue changes. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S120–9. doi:10.1016/j.ajodo.2009.04.021.
Gkantidis N, Halazonetis DJ. Morphological integration between the cranial base and the face in children and adults. J Anat. 2011;218(4):426–38. doi:10.1111/j.1469-7580.2011.01346.x.
O'Ryan F, Schendel S. Nasal anatomy and maxillary surgery. I. Esthetic and anatomic principles. Int J Adult Orthodon Orthognath Surg. 1989;4(1):27–37.
Neugebauer J, Ritter L, Mischkowski R, Zoller JE. Three-dimensional diagnostics, planning and implementation in implantology. Int J Comput Dent. 2006;9(4):307–19.
Baumrind S, Frantz RC. The reliability of head film measurements. 1. Landmark identification. Am J Orthod. 1971;60(2):111–27.
Miethke RR. Zur Lokalisationsgenauigkeit kephalometrischer Referenzpunkte. Prakt Kieferorthop. 1989;3:107–22.
Stabrun AE, Danielsen K. Precision in cephalometric landmark identification. Eur J Orthod. 1982;4(3):185–96.
Navarro Rde L, Oltramari-Navarro PV, Fernandes TM, Oliveira GF, Conti AC, Almeida MR, et al. Comparison of manual, digital and lateral CBCT cephalometric analyses. J Appl Oral Sci. 2013;21(2):167–76. doi:10.1590/1678-7757201302326.
Fourie Z, Damstra J, Gerrits PO, Ren Y. Accuracy and repeatability of anthropometric facial measurements using cone beam computed tomography. Cleft Palate Craniofac J. 2011;48(5):623–30. doi:10.1597/10-076.
Naji P, Alsufyani NA, Lagravere MO. Reliability of anatomic structures as landmarks in three-dimensional cephalometric analysis using CBCT. Angle Orthod. 2013. doi:10.2319/090413-652.1.
Oz U, Orhan K, Abe N. Comparison of linear and angular measurements using two-dimensional conventional methods and three-dimensional cone beam CT images reconstructed from a volumetric rendering program in vivo. Dentomaxillofac Radiol. 2011;40(8):492–500. doi:10.1259/dmfr/15644321.
Daboul A, Schwahn C, Schaffner G, Soehnel S, Samietz S, Aljaghsi A, et al. Reproducibility of Frankfort horizontal plane on 3D multi-planar reconstructed MR images. PLoS One. 2012;7(10), e48281. doi:10.1371/journal.pone.0048281.
Ludlow JB, Gubler M, Cevidanes L, Mol A. Precision of cephalometric landmark identification: cone-beam computed tomography vs conventional cephalometric views. Am J Orthod Dentofacial Orthop. 2009;136(3):312 e1–10. doi:10.1016/j.ajodo.2008.12.018. discussion −3.
Kim YI, Kim JR, Park SB. Three-dimensional analysis of midfacial soft tissue changes according to maxillary superior movement after horizontal osteotomy of the maxilla. J Craniofac Surg. 2010;21(5):1587–90. doi:10.1097/SCS.0b013e3181edc5c9.
Farkas LG, Phillips JH, Katic M. Anthropometric anatomical and morphological nose widths in Canadian Caucasian adults. Can J Plast Surg. 1998;6(3):149–51.
Gorgulu S, Gokce SM, Olmez H, Sagdic D, Ors F. Nasal cavity volume changes after rapid maxillary expansion in adolescents evaluated with 3-dimensional simulation and modeling programs. Am J Orthod Dentofacial Orthop. 2011;140(5):633–40. doi:10.1016/j.ajodo.2010.12.020.
Shaw K, McIntyre G, Mossey P, Menhinick A, Thomson D. Validation of conventional 2D lateral cephalometry using 3D cone beam CT. J Orthod. 2013;40(1):22–8. doi:10.1179/1465313312Y.0000000009.
Honn M, Goz G. The ideal of facial beauty: a review. J Orofac Orthop. 2007;68(1):6–16. doi:10.1007/s00056-007-0604-6.
Mitchell C, Oeltjen J, Panthaki Z, Thaller SR. Nasolabial aesthetics. J Craniofac Surg. 2007;18(4):756–65. doi:10.1097/scs.0b013e3180684360.
Rauso R, Tartaro G, Tozzi U, Colella G, Santagata M. Nasolabial changes after maxillary advancement. J Craniofac Surg. 2011;22(3):809–12. doi:10.1097/SCS.0b013e31820f3663.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AH carried out the design and drafted the first manuscript. BK, MS, and RD carried out the measurements and helped with the design and coordination of the study and the drafting of the manuscript. WK performed the surgery and helped with the coordination of the study. HKS helped with the study design, the translation into English and the illustrations. All of the authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hellak, A.F., Kirsten, B., Schauseil, M. et al. Influence of maxillary advancement surgery on skeletal and soft-tissue changes in the nose — a retrospective cone-beam computed tomography study. Head Face Med 11, 23 (2015). https://doi.org/10.1186/s13005-015-0080-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13005-015-0080-y