Abstract
Background
Previous reports regarding the predictive power of adiposity indices remain inconsistent, and longitudinal studies on this top are limited. The associations of hyperuricemia risk with changes in obesity status, as well as the joint effects of baseline adiposity indices and body adiposity change on hyperuricemia risk are not fully elucidated. This study aimed to explore the independent and joint associations of baseline adiposity indicators and body adiposity change with hyperuricemia risk among middle-aged and older population in China.
Methods
A total of 2895 participants aged ≥ 45 years from the baseline survey of the China Health and Retirement Longitudinal Study were followed up for 4 years. Anthropometric parameters (weight, height, and waist circumference) and serum uric acid were obtained using standard devices. Adjusted odds ratio and 95% confidential interval were calculated to estimate the associations between predictor variables and hyperuricemia risk using multivariate logistic regression.
Results
Of the 2895 participants, 293 (10.12%) cases of hyperuricemia were identified. Increased baseline body mass index (BMI), waist circumference, and waist-height ratio (WHtR) were significantly associated with higher risks of hyperuricemia. A slightly greater but non-significant area under the curve value was observed for waist circumference (0.622) than for BMI (0.611) and WHtR (0.614) (P = 0.447). Compared to subjects with stable adiposity status, participants with weight loss of ≥ 4 kg or waist circumference loss of ≥ 6 cm had a 56% or 55% lower risk of hyperuricemia, and those with weight gain of > 4 kg had a 1.62-fold higher risk of hyperuricemia. Compared to those without obesity, participants with incident or persistent obesity were more likely to develop hyperuricemia. Additionally, regardless of stable or increased weight/waist circumference during follow-up, individuals with obesity at baseline had a higher risk of incident hyperuricemia.
Conclusion
This study demonstrates that BMI, waist circumference, and WHtR equally predict the development of hyperuricemia, and weight loss and waist circumference reduction are favorable in preventing hyperuricemia.
Similar content being viewed by others
Background
Hyperuricemia, a metabolic disease due to disorder of purine metabolism, affects 13.3% of the general population in China [1], 21.3% in the U.S. [2], and 25.8% in Japan [3]. Both genetic and environmental factors may account for the development and progression of hyperuricemia [4], nevertheless, the underlying pathological mechanisms remain incompletely elucidated. Furthermore, long-term treatment of hyperuricemia carries both risks and costs. Hence, a better understanding of risk factors for hyperuricemia and early initiation of prevention are crucial to reduce the disease burden.
Uric acid, the major end product of purine metabolism, is primarily excreted by the kidney. Accordingly, the imbalance between production and excretion of uric acid contributes to hyperuricemia [5]. Growing evidence has shown that higher body mass index (BMI) increases the risks of renal impairment, leading to a decrease in uric acid clearance [6, 7]. Furthermore, higher BMI can disrupt the glucose and insulin metabolism [8], which may subsequently impair the renal handing of uric acid and alter SUA concentration [9]. In addition, visceral fat accumulation along with increased body weight promotes the synthesis of uric acid [10]. Notably, adipose tissue has also been reported to be a site of hypoxanthine secretion and uric acid production [5, 11]. Therefore, interventions aiming to reduce BMI and waist-height ratio (WHtR) might be effective in lowering the incidence of hyperuricemia.
Previous studies have found a positive association of hyperuricemia with BMI, waist circumference, and WHtR [12,13,14]. However, which adiposity indicator may better predict incident hyperuricemia remains inconsistent [15, 16]. Additionally, most of these studies are cross-sectional, and there is a lack of longitudinal studies with a nationally representative sample to validate these findings in the Chinese population. Although previous reports showed a significant association of serum uric acid (SUA) concentration with changes in weight and waist circumference [17], evidence regarding the impacts of changes in obesity status on hyperuricemia risk is limited and not fully elucidated. Furthermore, no study has explored the joint effects of BMI, waist circumference, and changes in body weight or waist circumference on hyperuricemia risk.
Therefore, the present study aims to investigate the independent and joint effects of BMI, waist circumference, WHtR, and their changes on risks of hyperuricemia in middle-aged and older Chinese population.
Methods
Study population and procedure
The data used in this study are from the China Health and Retirement Longitudinal Study (CHARLS), a nationally representative longitudinal survey of the Chinese population aged ≥ 45 years. A detailed description is available in a previous study [18]. Briefly, participants were randomly recruited through a four-stage probability sampling approach, which involved the selection of county-level units, primary sampling units within each selected county (administrative villages in rural areas and neighborhoods in urban areas), household units, and individual units. The baseline survey was carried out between 2011 and 2012 (wave 1), three subsequent follow-ups were conducted in 2013 (wave 2), 2015 (wave 3), and 2018 (wave 4), respectively. In the present study, information collected at wave 1 and wave 3 was used due to the availability of laboratory data on SUA. The inclusion criteria included: (a) aged ≥ 45 years; (b) without hyperuricemia, kidney diseases, or undertaking chemotherapy for malignancies; (c) no missing data on BMI, waist circumference, WHtR; (d) completed the questionnaire and blood sample collection; (e) successfully followed up to wave 3. The CHARLS was approved by the Institutional Review Board of Peking University (IRB00001052-11015, IRB00001052-11014), and written informed consent was obtained from all participants.
Data collection
Face-to-face interviews were administrated to collect data on demographic information (age, gender, residence, marital status, and education), smoking history, and drinking status. The information on comorbidities (hypertension, dyslipidemia, diabetes mellitus, and stroke) was also obtained by self-reports. Depression was evaluated using the Center for Epidemiologic Studies Depression Scale (CES-D), a 10-item questionnaire assessing the depressive feelings and behaviors in the last week [19]. The CES-D scale exhibited a good consistency in the present study, with Cronbach’s coefficient of 0.80. A total score of ≥ 10 was used to identify depression [20].
Weight, height, and waist circumference were objectively measured by trained investigators using standard devices, and were recorded to one decimal place (0.1 kg or 0.1 cm). BMI was calculated as weight in kilograms divided by height in meters squared, and was divided into four groups: underweight (< 18.5 kg/m2), normal weight (18.5–23.9 kg/m2), overweight (24–27.9 kg/m2), and obesity (≥ 28 kg/m2) [21]. WHtR was calculated as waist circumference in centimeters divided by height in centimeters [22]. General obesity was defined as a BMI value of ≥ 28 kg/m2. Abdominal obesity was determined if meeting one of the following criteria: (a) a waist circumference value of ≥ 90 cm for men, and a value of ≥ 85 cm for women [23]; (b) a WHtR value of ≥ 0.5 [24]. Change in weight or waist circumference was calculated as weight or waist circumference at follow-up minus the corresponding values at baseline. Weight change was divided into five groups: “loss of ≥ 4 kg (≤ −4 kg)”, “loss of ≥ 2 kg to loss of < 4 kg (> −4 to ≤ −2 kg)”, “loss of < 2 kg to gain of ≤ 2 kg (> −2 to ≤ 2 kg)”, “gain of > 2 kg to gain of ≤ 4 kg (> 2 to ≤ 4 kg)”, and “gain of > 4 kg (> 4 kg)”. Waist circumference change was also divided into five groups: “loss of ≥ 6 cm (≤ −6 cm)”, “loss of ≥ 3 cm to loss of < 6 cm (> −6 to ≤ −3 cm)”, “loss of < 3 cm to gain of ≤ 3 cm (> −3 to ≤ 3 cm)”, “gain of > 3 cm to gain of ≤ 6 cm (> 3 to ≤ 6 cm)”, and “gain of > 6 cm (> 6 cm)”.
All participants were asked to fast overnight before blood sample collection. Blood samples were transported to Beijing and stored at − 80℃ in the Chinese Center for Disease Control and Prevention. Bioassay was carried out at the laboratory of Capital Medical University. Fasting plasma glucose and total cholesterol were measured using enzymatic colormetric test. SUA, glycated hemoglobin, C-reactive protein, blood urea nitrogen, and serum creatinine were measured using UA Plus method, boronate affinity high-performance liquid chromatography, immunoturbidimetric assay, enzymatic ultraviolet method with urease, rate-blanked and compensated Jaffe creatinine method, respectively. Hyperuricemia was defined as a SUA value of ≥ 7 mg/dL for men, and a value of ≥ 6 mg/dL for women [25].
Statistical analysis
Data analysis was performed using STATA software version 15.1 (StataCorp., T.X., USA). Data were described as mean (SD) or median (IQR) for continuous variables, frequency (percentage) for categorical variables. The normality of data was verified by Kolmogorov–Smirnov test. The between-group comparison was conducted using one-way analysis of variance (ANOVA) or Wilcoxon rank-sum test for continuous variables, and Pearson χ2 test was used for categorical variables. Adjusted odds ratio (OR) and corresponding 95% confidential interval (CI) were calculated using multivariate logistic regression to estimate the associations between predictor variables and hyperuricemia. Test for linear trend was performed by treating ordinal categorical variables as continuous variables in the logistic regression model. Area under the curve (AUC) was calculated through the receiver operating characteristic (ROC) curve analysis to compare the predictive power of different adiposity indicators for hyperuricemia. A P value of < 0.05 indicated a significant difference.
To further evaluate the joint effects of baseline BMI and weight change, baseline BMI and waist circumference change on risks of hyperuricemia, baseline BMI was recategorized into “ < 24 kg/m2”, “24–27.9 kg/m2”, and “≥ 28 kg/m2”. Weight change was recategorized into “loss of ≥ 4 kg (≤ −4 kg)”, “loss of < 4 kg to gain of ≤ 4 kg (> −4 to ≤ 4 kg)”, and “gain of > 4 kg (> 4 kg)”. Similarly, waist circumference change was recategorized into “loss of ≥ 6 cm (≤ −6 cm)”, “loss of < 6 cm to gain of ≤ 6 cm (> −6 to ≤ 6 cm)”, and “gain of > 6 cm (> 6 cm)”. Adjusted OR for incident hyperuricemia was also calculated under different combined statuses of baseline BMI/waist circumference and weight change or waist circumference change. Participants with baseline BMI of < 24 kg/m2 and weight change of > −4 to ≤ 4 kg, participants with baseline BMI of < 24 kg/m2 and waist circumference change of > −6 to ≤ 6 cm, participants with baseline waist circumference of < 90 cm (men)/85 cm (women) and weight change of > −4 to ≤ 4 kg, participants with baseline waist circumference of < 90 cm (men)/85 cm (women) and waist circumference change of > −6 to ≤ 6 cm were selected as the reference groups, respectively.
Results
Figure 1 shows the flow chart for study population, and a total of 2895 participants were enrolled in the current study. The mean baseline age of participants was 59.08 years old, with males accounting for 49.36%. Of 2895 participants, 293 (10.12%) developed incident hyperuricemia. Individuals who developed hyperuricemia were more likely to be older, male, current drinkers; were more likely to have hypertension, dyslipidemia, and stroke; were more likely to have greater BMI, waist circumference, WHtR; and were more likely to have a higher concentration of SUA, total cholesterol, C-reactive protein, and serum creatinine at baseline (Table 1).
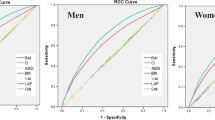
Multivariate logistic regression (Model 3) revealed that participants with obesity (BMI of ≥ 28 kg/m2) were at higher risk of hyperuricemia (OR 1.76; 95% CI 1.18–2.64) compared to those with BMI of 18.5–23.9 kg/m2, whereas there was no significant association between BMI and hyperuricemia risk in individuals with underweight (BMI of < 18.5 kg/m2) or overweight (BMI of 24–27.9 kg/m2). A linear trend toward higher risks of hyperuricemia as BMI increased was detected (P for trend = 0.022, Table 2). When waist circumference was applied, a significantly increased risk of hyperuricemia was observed in the third and fourth quartile compared to the first quartile (OR 1.84; 95% CI 1.20–2.83 and OR 2.12; 95% CI 1.38–3.27, respectively) (P for trend < 0.001, Table 2). In comparison with the first quartile of WHtR, the adjusted OR (Model 3) for incident hyperuricemia in the second, third and fourth quartile were 1.51 (95% CI 0.97–2.36), 1.61 (95% CI 1.03–2.51), and 2.75 (95% CI 1.75–4.31), respectively (P for trend < 0.001, Table 2). Compared to participants without abdominal obesity [waist circumference of < 90 cm (men)/85 cm (women)] or with low WHtR (< 0.5), individuals with abdominal obesity or high WHtR had a 1.57-fold (95% CI 1.17–2.10) or a 1.78-fold (95% CI 1.24–2.55) increased risk of hyperuricemia (Table 2). The adjusted OR (Model 3) for incident hyperuricemia per SD increase in BMI, waist circumference, and WHtR were 1.36 (95% CI 1.17–1.57), 1.34 (95% CI 1.17–1.53), and 1.42 (95% CI 1.22–1.65), respectively. In addition, ROC curve analysis showed a slightly higher AUC value for waist circumference (0.622) than BMI (0.611) and WHtR (0.614), but the intergroup difference was not statistically significant (P = 0.447, Fig. 2), demonstrating the comparable predictive ability of these indicators for incident hyperuricemia.
Compared to those with stable weight during follow-up (> −2 to ≤ 2 kg), there was a 56% or 37% lower risk of hyperuricemia (Model 3) in participants with weight loss of ≥ 4 kg or weight loss of ≥ 2 to < 4 kg. Besides, a 1.62-fold increased OR in participants with weight gain of > 4 kg was found (P for trend < 0.001). Similarly, participants with waist circumference loss of ≥ 6 cm had a reduced risk of hyperuricemia in comparison with those with waist circumference loss of < 3 cm to gain of ≤ 3 cm (OR 0.45; 95% CI 0.27–0.73; P for trend = 0.001). The adjusted OR (Model 3) for incident hyperuricemia per SD increase in weight change and waist circumference change was 1.37 (95%CI 1.21–1.55) and 1.27 (95% CI 1.11–1.46), respectively (Table 3). Further, we also explored the impact of changes in obesity status on hyperuricemia risk. Compared to those without obesity both at baseline and at follow-up, individuals with incident or persistent general obesity had a 3.04-fold (95% CI 1.66–5.59) or a 2.22-fold (95% CI 1.49–3.31) higher risk of hyperuricemia. Similarly, incident or persistent abdominal obesity was associated with higher risks of hyperuricemia, with an adjusted OR of 1.88 (95% CI 1.18–2.98) or 2.14 (95% CI 1.54–2.97) (Table 4).
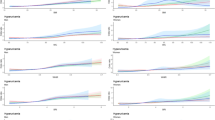
In addition, this study explored the joint effects of baseline BMI and changes in weight or waist circumference, baseline waist circumference and changes in weight or waist circumference on risks of hyperuricemia. Participants with obesity and had weight gain of > 4 kg exhibited a 4.29-fold (95% CI 1.66–11.09) increased risk of hyperuricemia in comparison with those who had BMI of < 24 kg/m2 and had stable weight (> −4 to ≤ 4 kg). Participants with obesity and had waist circumference gain of > 6 cm exhibited a 2.48-fold (95% CI 1.11–5.55) increased risk of hyperuricemia in comparison with those who had BMI of < 24 kg/m2 and had stable waist circumference (> −6 to ≤ 6 cm). Similarly, we found a significant association of increased hyperuricemia risk with a combined status of abdominal obesity [waist circumference of ≥ 90 cm (men)/85 cm (women)] and weight gain of > 4 kg compared to those without abdominal obesity and had stable weight (OR 3.49; 95% CI 2.06–5.91). Also, there was a significant association of increased hyperuricemia risk with a combined status of abdominal obesity and waist circumference gain of > 6 cm compared to those without abdominal obesity and had stable waist circumference (OR 2.74; 95% CI 1.57–4.77) (Fig. 3).
Adjusted OR for incident hyperuricemia was calculated, with a combined status of a BMI of < 24 kg/m2 and weight change of > −4 to ≤ 4 kg, b BMI of < 24 kg/m2 and waist circumference change of > −6 to ≤ 6 cm, c non-abdominal obesity [< 90 cm (men)/85 cm (women)] and weight change of > −4 to ≤ 4 kg, and d non-abdominal obesity and waist circumference change of > −6 to ≤ 6 cm as the reference groups, respectively. *P < 0.05, **P < 0.01, ***P < 0.001
Discussion
The present study demonstrated that indicators of both general obesity and abdominal obesity were related to a higher risk of hyperuricemia in middle-aged and older Chinese population, and loss of weight or waist circumference may help reduce the risk. Also, both development of obesity and persistent obesity were found to be risk factors for incident hyperuricemia. BMI, waist circumference, and WHtR exhibited comparable predictive power for incident hyperuricemia. Additionally, we found for the first time a significant joint association of hyperuricemia risk with a combined status of baseline BMI and weight change or waist circumference change, as well as the combined status of baseline waist circumference and weight change or waist circumference change.
The present study showed that the cumulative incidence of hyperuricemia was 10.12% in middle-aged and older Chinese population, with a follow-up duration of 4 years. The hyperuricemia incidence is comparable with that reported in a study by Dong et al. (10.24%) [26], but less than another finding (20.6%) [25], which is possibly due to different durations of follow-up. Previous studies have shown a positive relationship between obesity and SUA [27,28,29], which is in line with our findings. In this study, we found that both general obesity and abdominal obesity were associated with a higher risk of hyperuricemia, and this association maintained even further adjusted for baseline SUA. ROC curve analysis showed a slightly greater but non-significant AUC value for waist circumference compared with BMI and WHtR, indicating the equal predictive value of these adiposity indices for incident hyperuricemia. Furthermore, we did not observe a notable difference in the adjusted OR (Model 3) per SD increase in BMI, waist circumference, and WHtR, which were 1.36, 1.34, and 1.42, respectively. Similar to our findings, a study [30] involving 5685 Chinese individuals aged ≥ 60 years reported that there was no significant difference in the AUC of BMI and waist circumference for predicting elevated SUA in both males and females. However, another cross-sectional study [31] conducted in China suggested that WHtR was a better predictor of hyperuricemia than BMI and waist circumference. The discrepancy may be partially explained by two aspects. First, abdominal fat accumulation leads to weight gain, subsequently contributing to an increase in BMI. Through post hoc analysis, we found that a huge overlap existed between participants with BMI ≥ 28 kg/m2 and those with abdominal obesity in this study. Second, it is not feasible to delineate the temporal relationship between risks of hyperuricemia and these predictors in previous studies for their cross-sectional study design. Higher SUA level has been shown to induce abdominal obesity [32], this might account for a stronger association between WHtR and hyperuricemia reported in previous studies.
Previous studies have mainly focused on the relationship between changes in weight or waist circumference and changes in SUA [17, 33, 34], but whether such changes can indeed lead to the development of hyperuricemia remains inconclusive. The current study showed that loss of weight or waist circumference was favorable in reducing risks of hyperuricemia, and individuals with a gain in weight or waist circumference showed a higher propensity to develop hyperuricemia. In line with our results, a study with a ten-year follow-up period analyzed the data of 2611 participants aged 17–35 years from the Coronary Artery Risk Development in Young Adults (CARDIA) Study, and found that a decrease in BMI and waist circumference was associated with a lower SUA level after multivariate adjustments [34]. Similar findings have also been reported in another study by Heyden et al. and colleagues [33]. In our study, the results indicated that participants who developed obesity during follow-up were more inclined to suffer hyperuricemia, and persistent obesity also facilitated the development of hyperuricemia, further supporting the above findings. Also, a trend toward a lower risk of hyperuricemia for those with remittent obesity was observed, but this association was not statistically significant. The findings in this group should be verified by future research given the limited number of hyperuricemia cases (general obesity, n = 8; abdominal obesity, n = 10). Joint association analysis revealed that weight maintenance and waist circumference maintenance among individuals with general obesity were not enough to reduce risks of hyperuricemia, and a gain in weight or waist circumference may significantly increase the risk. Similar findings were also detected in subjects with abdominal obesity.
Decreased excretion and increased production of SUA may explain the high risk of incident hyperuricemia in obese individuals [35]. SUA concentration is highly dependent on renal excretion [34], while obesity leads to an increase in glucose concentration and blood pressure, risk factors for renal functions [36, 37]. In addition, insulin resistance intrigued by higher BMI can cause damage to urinary tract function, leading to a decrease in excretion of uric acid [9]. Additionally, visceral fat promotes the synthesis of very low-density lipoprotein and ribose-5-phosphate to phosphoribosyl pyrophosphate, which contribute to overproduction of uric acid [38]. Furthermore, greater catalytic activity of xanthine oxidoreductase is observed in obese individuals, facilitating the synthesis of uric acid [39, 40]. However, the underlying mechanisms have not been fully understood and warrant further explorations.
The present study has several strengths. First, this study was conducted using the data from the CHARLS, a population-based nationwide survey, ensuring sufficient representativeness of our study population. Second, we compared the predictive value of BMI, waist circumference, and WHtR using a longitudinal data set, and elucidated the relationship of changes in obesity status (general obesity and abdominal obesity) with risks of hyperuricemia. Third, we explored the joint associations of baseline adiposity indices and body adiposity change with hyperuricemia risk for the first time. However, this study also has some limitations. First, although our analysis made adjustments for a variety of confounding variables, the influence of other variables, like intake of dairy, meat, microelements, and use of allopurinol [41,42,43], cannot be ruled out since these data were not collected in the survey. Second, the participants in this study are Chinese population aged ≥ 45 years, thus it should be cautious when interpreting our findings in younger population and other ethnic individuals. Third, the follow-up duration is 4 years, impeding a further exploration of long-term associations between predictor variables and risks of hyperuricemia.
Conclusion
The present study demonstrates that BMI, waist circumference, and WHtR are comparable predictors of hyperuricemia in middle-aged and older Chinese population, and weight loss and waist circumference reduction are favorable in reducing the risk. Avoiding excessive gain in weight and waist circumference is an effective approach to prevent hyperuricemia, especially for individuals with overweight or obesity.
Availability of data and materials
The datasets generated and/or analyzed during the current study are publicly available on the following website: http://charls.pku.edu.cn/en.
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CES-D:
-
The Center for Epidemiologic Studies Depression Scale
- CHARLS:
-
The China Health and Retirement Longitudinal Study
- CI:
-
Confidential interval
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- SUA:
-
Serum uric acid
- WHtR:
-
Waist-height ratio
References
Liu R, Han C, Wu D, Xia X, Gu J, Guan H, et al. Prevalence of hyperuricemia and gout in mainland china from 2000 to 2014: a systematic review and meta-analysis. Biomed Res Int. 2015;2015:762820.
Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011;63:3136–41.
Nagahama K, Iseki K, Inoue T, Touma T, Ikemiya Y, Takishita S. Hyperuricemia and cardiovascular risk factor clustering in a screened cohort in Okinawa. Japan Hypertens Res. 2004;27:227–33.
Tanaka K, Ogata S, Tanaka H, Omura K, Honda C, Hayakawa K. The relationship between body mass index and uric acid: a study on Japanese adult twins. Environ Health Prev Med. 2015;20:347–53.
Kim IY, Han KD, Kim DH, Eun Y, Cha HS, Koh EM, et al. Women with metabolic syndrome and general obesity are at a higher risk for significant hyperuricemia compared to men. J Clin Med. 2019;8:837–50.
Xu H, Kuja-Halkola R, Chen X, Magnusson PKE, Svensson P, Carrero JJ. Higher body mass index is associated with incident diabetes and chronic kidney disease independent of genetic confounding. Kidney Int. 2019;95:1225–33.
Cai H, Zhan Y, Lu J, Zhu M, Liu S, Mei J, et al. Body mass index combined with waist circumference can predict moderate chronic kidney disease: a retrospective study. Medicine. 2021;100:e25017.
Walsh EI, Shaw J, Cherbuin N. Trajectories of BMI change impact glucose and insulin metabolism. Nutr Metab Cardiovasc Dis. 2018;28:243–51.
Facchini F, Chen YD, Hollenbeck CB, Reaven GM. Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration. JAMA. 1991;266:3008–11.
Matsuura F, Yamashita S, Nakamura T, Nishida M, Nozaki S, Funahashi T, et al. Effect of visceral fat accumulation on uric acid metabolism in male obese subjects: visceral fat obesity is linked more closely to overproduction of uric acid than subcutaneous fat obesity. Metabolism. 1998;47:929–33.
Nagao H, Nishizawa H, Tanaka Y, Fukata T, Mizushima T, Furuno M, et al. Hypoxanthine secretion from human adipose tissue and its increase in hypoxia. Obesity. 2018;26:1168–78.
de Oliveira EP, Moreto F, Silveira LV, Burini RC. Dietary, anthropometric, and biochemical determinants of uric acid in free-living adults. Nutr J. 2013;12:11–20.
Madala ND, Dubula T, Assounga AGH, Naicker S. Association of kidney function and waist circumference with uric acid levels in South Africans. Metab Syndr Relat Disord. 2017;15:500–6.
Wang YY, Li L, Cui J, Yin F, Yang F, Yuan DM, et al. Associations between anthropometric parameters (body mass index, waist circumference and waist to hip ratio) and newly diagnosed hyperuricemia in adults in Qingdao, China: a cross-sectional study. Asia Pac J Clin Nutr. 2020;29:763–70.
Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27:610–6.
Zhang ZQ, Deng J, He LP, Ling WH, Su YX, Chen YM. Comparison of various anthropometric and body fat indices in identifying cardiometabolic disturbances in Chinese men and women. PLoS ONE. 2013;8:e70893.
Ishizaka N, Ishizaka Y, Toda A, Tani M, Koike K, Yamakado M, et al. Changes in waist circumference and body mass index in relation to changes in serum uric acid in Japanese individuals. J Rheumatol. 2010;37:410–6.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–8.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84.
Xie Y, Ma M, Wu W, Zhang Y, Zhang Y, Tan X. Factors associated with depressive symptoms among the elderly in China: structural equation model. Int Psychogeriatr. 2020;4:1–11.
Wang J, Taylor AW, Zhang T, Appleton S, Shi Z. Association between body mass index and all-cause mortality among oldest old Chinese. J Nutr Health Aging. 2018;22:262–8.
Ashwell M, Lejeune S, McPherson K. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ. 1996;312:377.
Zhai Y, Fang HY, Yu WT, Yu DM, Zhao LY, Liang XF, et al. Changes in waist circumference and abdominal obesity among chinese adults over a ten-year period. Biomed Environ Sci. 2017;30:315–22.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
Zhang Y, Zhang M, Yu X, Wei F, Chen C, Zhang K, et al. Association of hypertension and hypertriglyceridemia on incident hyperuricemia: an 8-year prospective cohort study. J Transl Med. 2020;18:409–16.
Dong X, Zhang H, Wang F, Liu X, Yang K, Tu R, et al. Epidemiology and prevalence of hyperuricemia among men and women in Chinese rural population: the Henan Rural Cohort Study. Mod Rheumatol. 2020;30:910–20.
Ali N, Perveen R, Rahman S, Mahmood S, Rahman S, Islam S, et al. Prevalence of hyperuricemia and the relationship between serum uric acid and obesity: a study on Bangladeshi adults. PLoS ONE. 2018;13:e0206850.
Chen MY, Zhao CC, Li TT, Zhu Y, Yu TP, Bao YQ, et al. Serum uric acid levels are associated with obesity but not cardio-cerebrovascular events in Chinese inpatients with type 2 diabetes. Sci Rep. 2017;7:40009–16.
Duan Y, Liang W, Zhu L, Zhang T, Wang L, Nie Z, et al. Association between serum uric acid levels and obesity among university students (China). Nutr Hosp. 2015;31:2407–11.
Gu Z, Li D, He H, Wang J, Hu X, Zhang P, et al. Body mass index, waist circumference, and waist-to-height ratio for prediction of multiple metabolic risk factors in Chinese elderly population. Sci Rep. 2018;8:385–90.
Huang ZP, Huang BX, Zhang H, Zhu MF, Zhu HL. Waist-to-height ratio is a better predictor of hyperuricemia than body mass index and waist circumference in Chinese. Ann Nutr Metab. 2019;75:187–94.
Yadav D, Lee ES, Kim HM, Choi E, Lee EY, Lim JS, et al. Prospective study of serum uric acid levels and incident metabolic syndrome in a Korean rural cohort. Atherosclerosis. 2015;241:271–7.
Heyden S, Borhani NO, Tyroler HA, Schneider KA, Langford HG, Hames CG, et al. The relationship of weight change to changes in blood pressure, serum uric acid, cholesterol and glucose in the treatment of hypertension. J Chronic Dis. 1985;38:281–8.
Rathmann W, Haastert B, Icks A, Giani G, Roseman JM. Ten-year change in serum uric acid and its relation to changes in other metabolic risk factors in young black and white adults: the CARDIA study. Eur J Epidemiol. 2007;22:439–45.
Yamashita S, Matsuzawa Y, Tokunaga K, Fujioka S, Tarui S. Studies on the impaired metabolism of uric acid in obese subjects: marked reduction of renal urate excretion and its improvement by a low-calorie diet. Int J Obes. 1986;10:255–64.
Nurdiantami Y, Watanabe K, Tanaka E, Pradono J, Anme T. Association of general and central obesity with hypertension. Clin Nutr. 2018;37:1259–63.
Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89:309–19.
Hikita M, Ohno I, Mori Y, Ichida K, Yokose T, Hosoya T. Relationship between hyperuricemia and body fat distribution. Intern Med. 2007;46:1353–8.
Chiney MS, Schwarzenberg SJ, Johnson LA. Altered xanthine oxidase and N-acetyltransferase activity in obese children. Br J Clin Pharmacol. 2011;72:109–15.
Glantzounis G, Tsimoyiannis E, Kappas A, Galaris D. Uric acid and oxidative stress. Curr Pharm Des. 2005;11:4145–51.
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med. 2004;350:1093–103.
Zhang Y, Qiu H. Dietary magnesium intake and hyperuricemia among US adults. Nutrients. 2018;10:296–307.
Fan M, Liu J, Zhao B, Wu X, Li X, Gu J, et al. Comparison of efficacy and safety of urate-lowering therapies for hyperuricemic patients with gout: a meta-analysis of randomized, controlled trials. Clin Rheumatol. 2021;40:683–92.
Acknowledgements
The authors would like to thank the National School of Development at Peking University for providing the CHARLS data.
Funding
This work was sponsored by Shanghai Sailing Program (Grant Number: 20YF1448700), Key Construction Project of Health and Family Planning Commission of Baoshan District, Shanghai City (Grant Number: BSZK-2018-A01), Youth Programs of Shanghai Municipal Commission of Health and Family Planning (Grant Number: 20184Y0179).
Author information
Authors and Affiliations
Contributions
ZZ, RL, and RZ contributed to the conception and design of this study. ZZ, KL, and XL contributed to literature review. ZZ and XL contributed to data analyses. KL and RL contributed to data interpretation. ZZ drafted the article while RL and RZ critically appraised it and revised it. All authors have made substantial contributions to the preparation of this manuscript and approved its final version for submission. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The CHARLS was approved by the Institutional Review Board of Peking University (IRB00001052-11015, IRB00001052-11014). Before participation, written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, Z., Li, K., Li, X. et al. Independent and joint associations of body mass index, waist circumference, waist-height ratio and their changes with risks of hyperuricemia in middle-aged and older Chinese individuals: a population-based nationwide cohort study. Nutr Metab (Lond) 18, 62 (2021). https://doi.org/10.1186/s12986-021-00590-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-021-00590-z