Abstract
Background
Obesity is significant problem involving eating behavior and peripheral metabolic conditions. The effect of carbohydrate and fat restriction on appetite regulation, fibroblast growth factor 21 (FGF21) and leptin in children has not been defined. Our objective was to compare the effect of both diets.
Methods
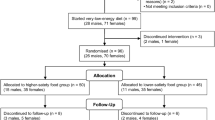
One hundred and twenty children with body mass index (BMI) higher than the equivalent of 30 kg/m2 for an adult, as corrected for gender and age were randomly assigned to (n = 60) a low-carbohydrate (L-CHO) diet or (n = 60) a low-fat (L-F) diet for 2 months. Fifty-three (88.3 %) subjects on the low-carbohydrate-diet and 45 (75 %) on the low-fat diet completed the study. Anthropometric measures, leptin and FGF21 levels were measured before and after the intervention. Comparison of the data for both of the diet groups was carried out using the t-test for independent variables. Intragroup comparisons before and after of each of the dietary treatments were performed using ANOVA for repeated measures. Factors associated with FGF21, leptin levels and satiety, were analyzed by multiple regression.
Results
After both of the diets, weight, leptin, food responsiveness, and enjoyment of food significantly decreased and high density lipoprotein cholesterol (HDL) increased, but FGF21 decreased. Before and after both of the interventions FGF21 was associated with triglycerides. Before the diet, satiety was associated with lower screen time (p < 0.04) and insulin levels (p < 0.05).
Conclusions
Both dietary restrictions improved the metabolic and hormonal parameters of obese children. FGF21 is an indicator of a beneficial metabolic response in younger children. After 2 months an adaptation of the eating behavior to food restriction was observed.
Similar content being viewed by others
Background
Childhood obesity is a health problem that is difficult to manage because the obesogenic environment hinders long-term adherence to a diet. Eating behavior and energetic balance are controlled by neural circuits in the hypothalamic and hindbrain centers, which have afferent pathways related to sensory and hedonic centers, metabolic hormones and nutrient and adiposity signals [1].
Several programs of caloric restriction have been designed. Among them, carbohydrate or lipid restrictions have been used extensively with limited long-term results. In children, carbohydrate restriction offers a satisfactory weight loss and improvement of adiponectin levels [2]. Lipid restriction may improve cardiometabolic risk factors such as triglycerides, low density lipoprotein cholesterol (LDL) and insulin levels [3]. Lipid restriction may also improve Homeostatic Model Assessment- Insulin Resistance (HOMA-IR) scores, and leptin and proinflammatory cytokines levels regardless of body weight [4].
In obese children, low-carbohydrate (L-CHO) diet may induce a better improvement of HOMA-IR and triglyceride levels compared to lipid restriction [5]; however, other reports have indicated that a low-fat (L-F) diet results in a better improvement of triglyceride levels [6].
For a better understanding of the effects of both types of macronutrient restriction, the impact on appetite-satiety mechanisms should be assessed. The Children’s Eating Behavior Questionnaire (CEBQ) is a validated tool to identify diverse signals related to satiety, enjoyment of food, response to different foods, and emotional components of appetite-satiety physiology in children [7].
In children food intake and attitudes toward meals, depend on maternal influences. Maternal feeding restriction is associated with a child’s food approach traits and responsiveness to food [8]; however, appetitive traits may respond differently to dietary restriction of carbohydrates or fats, and to our knowledge this subject has not been studied in children.
Leptin and fibroblast growth factor 21 (FGF21) are related to the regulation of food ingestion and energetic balance. Leptin is a key appetite-regulating hormone produced in the white adipose tissue that acts on the hypothalamus. Leptin suppresses food intake and increases energy expenditure by means of adrenergic stimulation [9] and stimulates peripheral fat oxidation and influences in glucose homeostasis by direct action on the pancreatic β cells [10]. Therefore, deficiency of leptin or its receptors facilitates obesity, increases insulin resistance and impairs glucose tolerance. In humans, a diet with fat [11] and carbohydrate [12] restriction decreases leptin levels.
FGF21 is a product of the liver and adipose tissue with important roles in food intake, and energy expenditure [13]. FGF21 mediates the metabolic response to starvation [14]. FGF21 enhances insulin sensitivity, decreases triglyceride concentrations, and ameliorates obesity-associated hyperglycemia and hyperlipidemia [15]. FGF21 also represses de novo lipogenesis by mediation of sterol regulatory element binding protein 1c transcription [16]. FGF21 is proposed as a mediator of glucagon regulation of glucose and lipid metabolism [17] and is an independent predictor of the metabolic syndrome in adults [18] but not in children [19].
In animal models, the effect of a L-CHO diet on FGF21 levels is controversial. In mice, a L-CHO diet increases as an adaptive response to malnutrition [20]; however, in another study FGF21 levels did not change [21]. In adults, overfeeding increases FGF21 levels [22], and an acute response was found with a fructose load [23].
In obese children who participated in exercise, behavior, and nutrition therapy over the course of 1 year, body mass index (BMI) diminution was accompanied by a decrease in FGF21 levels [24]; however, FGF21 did not change in adults on a ketogenic diet [25].
Surgical interventions in obese adults with intragastric balloon [26], laparoscopic sleeve gastrectomy [27] or gastric banding [28] decreases BMI and FGF21 levels; however in other studies, FGF21 levels did not change after intervention [29].
Carbohydrate or fat restrictions in the diet are strategies used to treat obesity with conflicting effects on appetite and satiety. Nevertheless, the effect on hormone and metabolic factors and the impact on long-term eating behavior are not well defined. Therefore, we examined the effect of restriction of carbohydrates or lipids, on diverse aspects of eating behavior and the metabolic and hormonal responses including leptin and FGF21 levels.
Subjects and methods
In a prospective clinical intervention, we recruited 120 obese children (58 boys and 62 girls) with a BMI higher than the equivalent of 30 kg/m2 for an adult, as corrected for gender and age according to the International tables of Cole et al. [30]. The participants were 6 to 12 years old and were recruited from grammar schools from the León City at the region central of Mexico. The participants did not have clinical evidence of hypothyroidism, chronic infections, congenital or metabolic diseases. The nature and purpose of the study was explained to the children and their parents and the confidentiality of individual results was guaranteed. All of the parents who accepted their children’s participation signed informed consent forms. The study was approved by the Institutional Ethics Committee, in compliance with the Declaration of Helsinki.
Data collection
All of the measurements were obtained at baseline and after the intervention. The children’s time of sleep (hours/day); exercise (minutes/week); and screen time, mainly spent on TV, computer and video games (minutes/week) were collected by direct questioning of the children and at least one of their parents. We collected the family history of obesity and diabetes as well as mother’s BMI.
Eating behavior scores were calculated using the CEBQ scale [7], as reported by one of the parents, which included 35 items to evaluate the following seven subscales: Satiety responsiveness/slowness in eating (nine items), Food fussiness (six items), Food responsiveness (five items), Enjoyment of food (four items), Desire to drink (three items), Emotional overeating (four items) and Emotional undereating (four items).
Weight and standing height were obtained while the children wore indoor clothing but no shoes using a roman type scale and a Harpenden stadiometer to determine the BMI value. The waist girth was measured while the children wore indoor clothes using a non-extendible flexible tape at the midpoint between the last rib and the iliac crest. The hip girth was measured at the point of maximum girth over the buttocks to obtain the waist-hip ratio (WHR). The skin fold thickness was obtained at bicipital, tricipital, suprailiac and subscapular sites to calculate body density as follows: For boys = 1.1533−(0.0643 × log ∑ (four measurements of skin fold thickness)), and for girls = 1.1369−(0.0598 × log ∑ (four measurements)). The percent body fat [31] was calculated as {4.95/body density - 4.5} × 100. The children were examined for pubertal development, scoring pubarche, adrenache, thelarche and menarche. The testicular volume was registered for the boys.
A venous blood sample was obtained after 12 h of fasting to measure hormones and metabolites. Serum glucose, triglycerides and total cholesterol concentrations were measured using enzymatic methods with a chemistry analyzer (Auto KEM II, Kontrollab, Italy). Serum insulin, leptin and adiponectin were analyzed by radioimmunoassay using a Millipore kit (St. Charles, Mo), with intra- and inter-assay variation coefficients of 4.4 and 6.0 % for insulin, 3.4 and 3.6 % for leptin, and 6.2 and 9.2 % for adiponectin. FGF21 was measured by ELISA, (Mediagnost, Reutlingen, Germany), with intra- and inter-assay variation coefficients of 3.5 and 5.2 %. Insulin resistance was estimated with HOMA-IR.
Intervention
The children were randomly assigned to two different dietary treatments: a L-F diet and a L-CHO diet (60 children each) for a 2-month period. The diets were elaborated according to the recommendations of the American Academy of Pediatrics [32] and the Official Mexican Norm 043 (NOM-043-SSA2-2005). The L-CHO diet was 50 % carbohydrate, 30 % fat and 20 % protein, while the L-F diet with 60 % carbohydrate, 25 % fat and 15 % protein. The caloric intake was calculated individually based on total energy expenditure for each child according to age requirements [33]. Then, the distribution of macronutrients, depending on the assigned dietary treatment was calculated. The diet prescribed was explained to the parents, indicating the choice of foods and procedures of measurements, to be carried out at home. Deviations from the indications were assessed in the collection of the compliance evaluation.
Statistical analysis
The data are shown as the means and standard deviations. The variables were tested for normality with the K-S test. Comparison of the data for both of the diet groups was carried out with the t-test for independent variables. Each group was compared before and after the dietary treatment using ANOVA for repeated measures, testing as covariates sex, age, pubarche and adrenarche.
Factors associated with FGF21, leptin levels and satiety were analyzed by multiple regression, with stepwise selection of significant variables. We used the same model for the analysis of serum FGF21 and leptin levels as dependent variables testing as candidate regressors BMI, percent body fat, age, sex, glucose, insulin, HOMA, total cholesterol, triglycerides, adiponectin, hours of sleep, exercise, screen time and the seven subscales of eating behavior. We analyzed the factors associated with satiety taking as candidate regressors BMI, age, sex, leptin, adiponectin, insulin, FGF21, time of exercise, screen time, and hours of sleep.
Results
One hundred and twenty children were included in the study. The children had a mean age of 9.8 ± 1.6 years, a mean BMI of 28.1 ± 3.6 kg/m2, a mean WHR of 0.96 ± 0.05, and a mean percent body fat of 41.01 ± 3.46. Their basal dietary consumption was as follows: kilocalories 2161 ± 606, lipids 31.6 ± 6.3 % and carbohydrates 54.1 ± 7.4 %. Initially the children were randomized into two groups. The data from both of the groups had a normal distribution and were similar compared with a t-test for independent variables.
The 2 months follow-up was completed by 53 (88.3 %) subjects on the L-CHO diet and 45 (75 %) with on the L-F diet. The children decreased their total caloric intake by a mean of 2436 kJ/day (582 kcal) after 8 weeks (p < 0.00003). The group on the L-CHO diet decreased 2554 kJ/day (616 kcal), t = 6.14, p < 0.0000001. The group on the L-F diet decreased 2457 kJ/day (587 kcal), t = 7.50, p < 0.0000001 a value within the range of expected dietary compliance.
Effect of low-carbohydrate diet
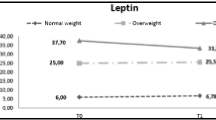
After 2 months on the L-CHO diet, the BMI, leptin and FGF21 levels decreased. An increase in total cholesterol was observed as a result of an increase in high density lipoprotein cholesterol (HDL) levels. No change was found for HOMA-IR. In regards to eating behavior, food responsiveness, enjoyment of food and emotional overeating decreased significantly, and satiety responsiveness increased marginally (Table 1).
Effect of low-fat diet
After 2 months on the L-F diet, the BMI, leptin levels, LDL-cholesterol and FGF21 levels decreased and HDL-cholesterol increased. Regarding eating behavior, food responsiveness and enjoyment of food decreased significantly and satiety responsiveness increased marginally (Table 2).
Comparison of changes between both dietary interventions
Table 3 compares the effect of both diets. The total and LDL-cholesterol levels significantly decreased with the L-F diet. A similar feeding behavior was observed in both of the groups.
Factors associated with the FGF21 levels
Using the multiple regression procedure, we found that before the diet, FGF21 was positively associated with total cholesterol, triglycerides and BMI. After the L-CHO and L-F diets FGF21 remained associated only with triglyceride levels (Table 4).
Considering this association we examined the possible relationship of FGF21 with pubertal development. ANOVA for adrenarche stages in both sexes did not show an association with FGF21 (f = 0.005, p = 0.94). With univariate regression analysis for young boys, testicular volume was not associated with FGF21 (p = 0.22).
Factors associated with leptin
For the basal study, the only factor associated with leptin was BMI. After dietary treatment with the L-CHO and L-F diets, the association with BMI remained significant (Table 4).
Factors associated with satiety
Before the treatment satiety was negatively associated with screen time and insulin levels. After the treatment no factor was associated (Table 4).
Influence of age on the response to macronutrient restriction
In the multiple regression analysis for hormones and satiety, gender and age were not included in the model. In an additional analysis we divided both of the groups by ages 6 to 10 (n = 76), and >10 to 12 years (n = 22). In the 6 to 10 years of age group, the factors associated with leptin, FGF21 and satiety were the same as in the total group (Table 4); however in the >10 to 12 years group, leptin was associated with BMI before intervention, and after either diet. No associations were found with FGF21 or satiety. This finding indicates that in our group early pubertal activation is not adequately represented to show its influence on satiety or hormone changes.
Discussion
A 2-month intervention may be limited by tolerance. A prolonged intervention may permit a further reduction of obesity. Adult obese people on a diet may have serious rebound effects. Whether problems of treatment in adults may be more manageable in children is important to clarify.
The balance of macronutrients in the design of dietary restriction for obesity in children is an important subject. To solve this point, the impact of different diet schemes on eating behavior, hormones and metabolic response must be studied in diverse populations. In adults, the comparison of carbohydrate or fat restriction during 8 weeks did not show differences in satiety [34]. Yet, another study showed a lower perception of hunger in the group on a L-CHO diet after 6 weeks [35].
Nonetheless in obese children, differences in feeding behavior, under fat or carbohydrate restriction have not been reported. In this study we found that changes in appetite traits were not different with carbohydrate or fat restriction. After 2 months on either diet, food responsiveness and enjoyment of food decreased, and satiety increased marginally, probably because of reduced feeding pleasure. Our results indicate that eating behavior in children is modified favorably with both diets. Emotional overeating decreased in a marginal manner only under the L-CHO diet. There is no previous information about this subject. An appetite adaptation to macronutrient restriction occurred for the children after the 2-month study and further supports the continuation of the dietary program. The decrease in appetite may also correlate with the bland diets.
Before the intervention, satiety was negatively associated with screen time and insulin levels. Previous reports showed that in children, a long time spent before a screen increases caloric intake by delaying normal mealtime satiation [36]. This finding supports the concept that entertainment before a screen may increase obesogenic behavior. A recent study in adults reported that satiety signals are related to ghrelin and triglycerides but not to insulin levels [37]. Nevertheless, no previous information about insulin and satiety in children exists, and therefore, this subject should be analyzed in future studies.
In our study LDL-cholesterol and total cholesterol had a greater decrease with the L-F diet. In adults the information about this subject is controversial because one report shows that a L-CHO diet for 8 weeks decreased LDL-cholesterol levels, showing a less atherogenic lipid profile compared to the L-F diet [34]; however, another study reported that both restriction diets induced a similar decrease of LDL-cholesterol [38]. HDL-cholesterol increased after both interventions in accordance with a previous report in adults [39].
We found that leptin decreases with both diets, and this hormone was positively associated with BMI. Leptin release is dependent on both adipose mass and nutrient flux, which is mainly represented by hexosamines in the adipocyte [40]; however, satiety increased marginally, and we must consider that appetite and satiety result from the interplay of several factors, included ghrelin and nutrient signaling [41] and factors related with leptin resistance [42].
Insulin levels showed a trend to a non-significant decrease. In adults, short-term food restriction induces a decrease in insulin levels [43]. In children, a significant insulin decrease has been reported with only 6-month [2] and 16-week diets [44]; however, in children insulin diminution may be observed after 2 weeks of diet and exercise [4]. This finding may indicate that in children, leptin is more sensitive to calorie restriction than insulin levels.
FGF21, which is proposed to be an important hormone for metabolic adaptation to starvation and food restriction [14], decreased with both diets. In humans, the decrease rather than the increase of FGF21 levels with dietary restriction is not congruent with that concept. This finding is in agreement with previous studies with food restriction in children [24] and adults [28]. Our findings are of interest because a similar response was found with the L-CHO and L-F diets. We are not aware of similar previous observations.
Before the diet, FGF21 was associated with BMI, total cholesterol and triglycerides. In regards to triglyceride levels, this association is in agreement with previous reports [45] and in accordance with the concept that FGF21 is a biomarker of metabolic conditions. In adults, the circulating levels of FGF21 increase under adverse lipid profiles, obesity, metabolic syndrome, impaired glucose tolerance, type 2 diabetes mellitus, or atherosclerosis [18], but in children its relationship with metabolic syndrome has not been confirmed [19].
Interestingly, the association of FGF21 with triglyceride levels remained after both diets. Transgenic mice with an overexpression of FGF21 have a reduction in plasma triglyceride levels [14]; however, in human subjects, FGF21 correlates positively with triglycerides suggesting that FGF21 is a result of obesity and may compensate for the metabolic stress in states of obesity and insulin resistance. Considering that the administration of FGF21 has an antilipolytic effect, the positive association between FGF21 and triglycerides levels may indicate a state of FGF21 resistance as proposed by Fisher et al. [46] in which FGF21 fails to maintain triglyceride levels within the normal range. FGF21 may act as a compensatory signal to mitigate metabolic stresses due to obesity [47].
Fgf21-null mice showed increased hepatic endoplasmic reticulum (ER) stress. Exposure of primary hepatocytes to palmitic acid elevated the mRNA levels encoding DNA damage-inducible transcript 3, an indicator of ER stress, and FGF21 in a peroxisome proliferator activated receptor alpha (PPARα) -independent manner. This finding suggests that lipid-induced ER stress can enhance hepatic FGF21 expression [48].
A closer examination of the results suggests that certain parameters trended down or up and were close to statistical significance, and thus, much larger cohorts need to be analyzed.
Conclusions
In conclusion, to our knowledge this is the first study to compare the effect of carbohydrate or lipid restriction on appetite traits in obese children. Both types of dietary restriction improved the metabolic parameters. Leptin and FGF21 decreased with both diets. Leptin was correlated with BMI and FGF21 was associated with triglycerides, total cholesterol and BMI, but after the L-CHO and L-F diets, only triglycerides remained associated with FGF21. Before the diet, satiety was associated with less screen time, but after the diet, appetite traits were not associated with life-style, hormonal or metabolic factors. In this study we did not find important behavioral, metabolic or hormonal differences between both types of diets. Further studies are required to properly identify changes induced with different amounts of macronutrients.
Abbreviations
- LDL:
-
Low density lipoprotein
- HOMA-IR:
-
Homeostatic Model Assessment- Insulin Resistance
- CEBQ:
-
Children’s eating behavior questionnaire
- FGF21:
-
Fibroblast growth factor 21
- BMI:
-
Body mass index
- WHR:
-
Waist-hip ratio
- L-F:
-
Low-fat diet
- L-CHO:
-
Low-carbohydrate diet
- HDL:
-
High density lipoprotein
- ER:
-
Endoplasmic reticulum
References
Ahima RS, Antwi DA. Brain regulation of appetite and satiety. Endocrinol Metab Clin N Am. 2008;37(4):811–23.
Partsalaki I, Karvela A, Spiliotis BE. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J Pediatr Endocrinol Metab. 2012;25(7–8):697–704.
Niinikoski H, Pahkala K, Ala-Korpela M, Viikari J, Rönnemaa T, Lagström H, et al. Effect of repeated dietary counseling on serum lipoproteins from infancy to adulthood. Pediatrics. 2012;129(3):e704–13.
Roberts CK, Izadpanah A, Angadi SS, Barnard RJ. Effects of an intensive short-term diet and exercise intervention: comparison between normal-weight and obese children. Am J Physiol Regul Integr Comp Physiol. 2013;305(5):R552–57.
Casazza K, Cardel M, Dulin-Keita A, Kolbe L. Reduced carbohydrate diet to improve metabolic outcomes and decrease adiposity in obese peripubertal African American girls. J Pediatr Gastroenterol Nutr. 2012;54(3):336–42.
Maffeis C, Bonadonna R, Maschio M, Aiello G, Tommasi M, Marigliano M, et al. Metabolic and hormonal consequences of two different meals after a moderate intensity exercise bout in obese prepubertal children. Eur J Clin Nutr. 2013;67(7):725–31.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children’s eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42(7):963–70.
Carnell S, Benson L, Driggin E, Kolbe L. Parent feeding behavior and child appetite: associations depend on feeding style. Int J Eat Disord. 2014;47(7):705–9.
Pellegrino MJ, McCully BH, Habecker BA. Leptin stimulates sympathetic axon outgrowth. Neurosci Lett. 2014;566:1–5.
Wolsk E, Mygind H, Grøndahl TS, Pedersen B, van Hall G. The role of leptin in human lipid and glucose metabolism: the effects of acute recombinant human leptin infusion in young healthy males. Am J Clin Nutr. 2011;94(6):1533–44.
Lasa A, Miranda J, Bulló M, Casas R, Salas-Salvadó J, Larretxi I, et al. Comparative effect of two Mediterranean diets versus a low-fat diet on glycaemic control in individuals with type 2 diabetes. Eur J Clin Nutr. 2014;68(7):767–72.
Ratliff J, Mutungi G, Puglisi MJ, Volek JS, Fernandez ML. Carbohydrate restriction (with or without additional dietary cholesterol provided by eggs) reduces insulin resistance and plasma leptin without modifying appetite hormones in adult men. Nutr Res. 2009;29(4):262–8.
Sarruf DA, Thaler JP, Morton GJ, German J, Fischer JD, Ogimoto K, et al. Fibroblast growth factor 21 action in the brain increases energy expenditure and insulin sensitivity in obese Rats. Diabetes. 2010;59(7):1817–24.
Inagaki T, Dutchak P, Zhao G, Ding X, Gautron L, Parameswara V, et al. Endocrine regulation of the fasting response by PPARalpha-mediated induction of fibroblast growth factor 21. Cell Metab. 2007;5(6):415–25.
Li H, Zhang J, Jia W. Fibroblast growth factor 21: a novel metabolic regulator from pharmacology to physiology. Front Med. 2013;7(1):25–30.
Zhang Y, Lei T, Huang JF. The link between fibroblast growth factor 21 and sterol regulatory element binding protein 1c during lipogenesis in hepatocytes. Mol Cell Endocrinol. 2011;342(1–2):41–7.
Habegger KM, Stemmer K, Cheng C, Müller TD, Heppner KM, Ottaway N, et al. Fibroblast growth factor 21 mediates specific glucagon actions. Diabetes. 2013;62(5):1453–63.
Jin QR, Bando Y, Miyawaki K, Shikama Y, Kosugi C, Aki N, et al. Correlation of fibroblast growth factor 21 serum levels with metabolic parameters in Japanese subjects. J Med Invest. 2014;61(1–2):28–34.
Ko BJ, Kim SM, Park KH, Park HS, Mantzoros CS. Levels of circulating selenoprotein P, fibroblast growth factor (FGF) 21 and FGF23 in relation to the metabolic syndrome in young children. Int J Obes ( Lond). 2014;38(12):1497–502.
Murata Y, Nishio K, Mochiyama T, Konishi M, Shimada M, Ohta H, et al. Fgf21 impairs adipocyte insulin sensitivity in mice fed a low-carbohydrate, high-fat ketogenic diet. PLoS ONE. 2013;8(7):e69330.
Badman MK, Kennedy AR, Adams AC, Pissios P, Maratos-Flier E. A very low carbohydrate ketogenic diet improves glucose tolerance in ob/ob mice independently of weight loss. Am J Physiol Endocrinol Metab. 2009;297(5):e1197–204.
Heilbronn LK, Campbell LV, Xu A, Samocha-Bonet D. Metabolically protective cytokines adiponectin and fibroblast growth factor-21are increased by acute overfeeding in healthy humans. PLoS ONE. 2013;8(10):e78864.
Dushay JR, Toschi E, Mitten EK, Fisher FM, Herman MA, Maratos-Flier E. Fructose ingestion acutely stimulates circulating FGF21 levels in humans. Mol Metab. 2014;4(1):51–7.
Reinehr T, Woelfle J, Wunsch R, Roth CL. Fibroblast growth factor 21 (FGF-21) and its relation to obesity, metabolic syndrome, and nonalcoholic fatty liver in children: a longitudinal analysis. J Clin Endocrinol Metab. 2012;97(6):2143–50.
Dushay J, Chui PC, Gopalakrishnan GS, Varela-Rey M, Crawley M, Fisher FM, et al. Increased fibroblast growth factor 21 in obesity and nonalcoholic fatty liver disease. Gastroenterology. 2010;139(2):456–63.
Bužga M, Evžen M, Pavel K, Tomáš K, Vladislava Z, Pavel Z, et al. Effects of the intragastric balloon medSil on weight loss, fat tissue, lipid metabolism, and hormones involved in energy balance. Obes Surg. 2014;24(6):909–15.
Haluzíková D, Lacinová Z, Kaválková P, Drápalová J, Křížová J, Bártlová M, et al. Laparoscopic sleeve gastrectomy differentially affects serum concentrations of FGF-19 and FGF-21 in morbidly obese subjects. Obesity (Silver Spring). 2013;21(7):1335–42.
Lips MA, de Groot GH, Berends FJ, Wiezer R, van Wagensveld BA, Swank DJ, et al. Calorie restriction and Roux-en-Y gastric bypass have opposing effects on circulating FGF2 in morbidly obese subjects. Clin Endocrinol (Oxf). 2014;81(6):862–70.
Woelnerhanssen B, Peterli R, Steinert RE, Peters T, Borbély Y, Beglinger C. Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy- a prospective randomized trial. Surg Obes Relat Dis. 2011;7(5):561–8.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–3.
Brook CGD. Composition of human adipose tissue from deep and subcutaneous sites. Br J Nutr. 1971;25(3):377–80.
Gidding SS, Dennison BA, Birch LL, Daniels SR, Gilman MW, Lichtenstein AH, et al. Dietary Recommendations for children and adolescents: A guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005;112(13):2061–75.
Report of a Joint FAO/WHO/UNU Expert Consultation. Title of subordinate document. Human energy requirements. 2001. http://www.fao.org/3/a-y5686e.pdf. Accessed 04 Aug 2015.
Stoernell CK, Tangney CC, Rockway SW. Short-term changes in lipoprotein subclasses and C-reactive protein levels of hypertriglyceridemic adults on low-carbohydrate and low-fat diets. Nutr Res. 2008;28(7):443–9.
Nickols-Richardson SM, Coleman MD, Volpe JJ, Hosig KW. Perceived hunger is lower and weight loss is greater in overweight premenopausal women consuming a low-carbohydrate/high-protein vs high-carbohydrate/low-fat diet. J Am Diet Assoc. 2005;105(9):1433–7.
Bellissimo N, Pencharz PB, Thomas SG, Anderson GH. Effect of television viewing at mealtime on food intake after a glucose preload in boys. Pediatr Res. 2007;61(6):745–9.
Sun X, Veldhuizen MG, Wray AE, de Araujo IE, Sherwin RS, Sinha R, et al. The neural signature of satiation is associated with ghrelin response and triglyceride metabolism. Physiol Behav. 2014;136:63–73.
Tay J, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert GA, et al. A very low-carbohydrate, low-saturated fat diet for type 2 diabetes management: a randomized trial. Diabetes Care. 2014;37(11):2909–18.
Schwingshackl L, Hoffmann G. Comparison of effects of long-term low-fat vs high-fat diets on blood lipid levels in overweight or obese patients: a systematic review and meta-analysis. J Acad Nutr Diet. 2013;113(12):1640–61.
Considine RV, Cooksey RC, Williams LB, Fawcett RL, Zhang P, Ambrosius WT, et al. Hexosamines regulate leptin production in human subcutaneous adipocytes. J Clin Endocrinol Metab. 2000;85(10):3551–6.
Van der Plasse G, van Zessen R, Luijendijk MC, Erkan H, Stuber GD, Ramakers GM, et al. Modulation of cue-induced firing of ventral tegmental area dopamine neurons by leptin and ghrelin. Int J Obes (Lond).2015; doi:10.1038/ijo.2015.131.
Crujeiras AB, Carreira MC, Cabia B, Andrade S, Amil M, Casanueva FF. Leptin resistance in obesity: An epigenetic landscape. Life Sci.2015; doi: 10.1016/j.lfs.2015.05.003.
Gower BA, Goss AM. A lower-carbohydrate, higher-fat diet reduces abdominal and intermuscular fat and increases insulin sensitivity in adults at risk of type 2 diabetes. J Nutr. 2015;145(1):177S–83S.
Armeno ML, Krochik AG, Mazza CS. Evaluation of two dietary treatments in obese hyperinsulinemic adolescents. J Pediatr Endocrinol Metab. 2011;24(9–10):715–22.
Lee Y, Lim S, Hong ES, Kim JH, Moon MK, Chun EJ, et al. Serum FGF21 concentration is associated with hypertriglyceridaemia, hyperinsulinaemia and pericardial fat accumulation, independently of obesity, but not with current coronary artery status. Clin Endocrinol (Oxf). 2014;80(1):57–64.
Fisher FM, Chui PC, Antonellis PJ, Bina HA, Kharitonenkov A, Flier JS, et al. Obesity is a fibroblast growth factor 21 (FGF21)-resistant state. Diabetes. 2010;59(11):2781–9.
Kim KH, Lee MS. FGF21 as a Stress Hormone: The Roles of FGF21 in stress adaptation and the treatment of metabolic diseases. Diabetes Metab J. 2014;38(4):245–51.
Tanaka N, Takahashi S, Zhang Y, Krausz KW, Smith PB, Patterson AD, et al. Role of fibroblast growth factor 21 in the early stage of NASH induced by methionine- and choline-deficient diet. Biochim Biophys Acta. 2015;1852(7):1242–52.
Acknowledgments
This work was supported in part by CONACYT grant CB 2007 – 84277 and by CONACYT GTO-2010-C02-145281.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LR IR participated in the recruitment of participants, clinical assessment, statistical analysis and drafting of the work. LP participated in the recruitment of participants, clinical assessment and drafting of the work. EL PL participated in the design, coordination of the study, supervision of laboratory procedures and drafting of the work. ME GS participated in the design, coordination of the study, supervision of laboratory procedures and drafting of the work. JM M participated in the study design, obtained the grant, coordinated the project, analyzed the data and drafted of the work. All of the authors approved the final version to be published.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ibarra-Reynoso, L.d.R., Pisarchyk, L., Pérez-Luque, E.L. et al. Dietary restriction in obese children and its relation with eating behavior, fibroblast growth factor 21 and leptin: a prospective clinical intervention study. Nutr Metab (Lond) 12, 31 (2015). https://doi.org/10.1186/s12986-015-0027-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-015-0027-0