Abstract
Background
Primary Human herpesvirus-7 (HHV-7) infection usually occurs during childhood and causes several clinical manifestations: mainly exanthem subitum (roseola infantum), followed by a lifelong latent state with possible reactivation in case of immunodeficiency. Nevertheless, some considerably different approaches exist regarding the natural history of HHV-7 and the possible consequences of HHV-7 infection in immunocompetent adults. In particular, little is known about its pathogenic role in central nervous system (CNS) disease in nonimmunosuppressed adults. Specifically, in case of encephalitis, it is important to distinguish between infectious encephalitis and postinfectious encephalomyelitis for the management of patients
Case presentation
We describe here a case of encephalitis associated to human herpesvirus-7 with associated polymyeloradiculopathy in an immunocompetent patient which may contribute to the delineation of the approach to a patient profile with a similar clinical presentation and evolution to those presented in the literature.
Conclusions
This case may alert clinicians to consider this specific etiology in the differential diagnosis of encephalopathy in patients with suspected infectious encephalitis who do not respond to acyclovir or in patients who develop acute polymyeloradiculopathy, considering that HHV-7 may be a pathological factor and that a timely diagnosis is crucial for the early administration of specific treatment.
Similar content being viewed by others
Background
Human herpesvirus-7 (HHV-7) is a ubiquitous virus that belongs to the subfamily of β-herpesviruses (together with cytomegalovirus and human herpesvirus-6). Primary HHV-7 infection usually occurs during childhood and may cause several clinical manifestations: mainly exanthem subitum (roseola infantum), followed by a lifelong latent state with possible reactivation in case of immunodeficiency [1]. Nevertheless, some considerably different approaches exist regarding the natural history of this infectious agent and the possible consequences of HHV-7 infection in immunocompetent adults, pertaining both to late primary HHV-7 infection or reactivation of the virus from macrophages and/or CD4+ T cells. In particular, little is known about its pathogenic role in central nervous system (CNS) disease in nonimmunosuppressed adults. Specifically, in case of encephalitis, it is important to distinguish between infectious encephalitis and postinfectious encephalomyelitis for the management of patients. We describe here a case of HHV-7 encephalitis with associated polymyeloradiculopathy in an immunocompetent patient.
Case presentation
A 26-year-old immunocompetent male presented with dizziness, blurred vision, a 3-day history of fever, frontal headache, cervical and lumbar pain, and vomiting during the last 24 h. There was no significant personal history apart from animal exposure: contact with dogs and cats several days before the onset of symptoms and the presence of a tick on his back (information provided by his relatives). Physical examination revealed the presence of somnolence. On admission, the patient presented cranial nerve affectation (ophthalmoplegia), vertical nystagmus in attempted supra-version, mitigated osteotendinous reflexes, indifferent bilateral superficial cutaneous reflexes, and dysmetria, which was observed on the finger-to-nose test. A cerebrospinal fluid (CFS) sample contained 110 leucocytes/μl (lymphocytes + monocytes) and 100 red blood cells/μl, 82 mg/dl of protein, and 60 mg/dl of glucose (blood glucose, 108 mg/dl). A second CFS sample obtained 3 days after the collection of the first one contained 200 leucocytes/μl (95% monocytes), 61 mg/dl of protein, and 54 mg/dl of glucose (blood glucose, 88 mg/dl). Progressive deterioration of the level of consciousness with a Glasgow Coma Score (GCS) of 8 (V1, O1, M6) led to a requirement for mechanical ventilation.
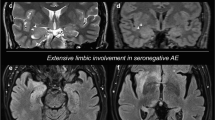
The patient was empirically treated with acyclovir, ceftriaxone, ampicillin, doxycycline, and corticoids. His level of consciousness improved (GCS 11 [O4, V1, M6]), although the ophthalmoplegia persisted. Electroencephalography (EEG) showed irregular slow activity with slow bilateral waves in the temporal and frontal areas, which was consistent with encephalitis. Magnetic resonance imaging (MRI) of the brain was normal. Normal findings were obtained for a wide spectrum of antibodies (anti-Jo-1, anti-Sm, anti-SS-A, anti-SS-B, anti-nRNP, anti-Scl-70, anti-c-ANCA, anti-p-ANCA, anti-dsDNA, anti-amphiphysin, anti-CV2, anti-PNMA2, anti-Yo (PCCA-1), anti-Hu (ANNA-1), anti-RI (ANNA-2), and anti-ganglioside). On the 5th evolution day, he developed flaccid paralysis of his right arm and lower limbs with abolishment of osteotendinous reflexes. Electromyography (EMG) performed on the 8th evolution day revealed an F-wave alteration in the upper and lower limbs that was indicative of the initial stage of polyradiculoneuritis. Cerebrospinal fluid (CFS), serum, and whole-blood samples were screened for the identification of possible etiologies. Follow-up MRI investigations performed in our patient revealed the presence of cervical and dorsolumbar myelitis. Intravenous immunoglobulins were administered to the patient, who was considered as having acute polymyeloradiculopathy. After treatment, the ophthalmoplegia disappeared, the strength of the upper-right limb was recovered, and the strength of the lower limbs was improved. The patient was subsequently discharged; however, urinary incontinence persisted. Four months later, the patient had recovered completely.
The results of the microbiological assessment, according to clinical and risk factors were as follows. First-line investigation: on day 1; gram stain and bacterial culture, alpha-herpesvirus (herpes simplex virus 1, herpes simplex virus 2, and varicella-zoster virus), and enterovirus were negative. On day 3; Treponema pallidum and Cryptococcal neoformans (serum and CFS), Mycoplasma pneumoniae, Epstein–Barr virus, and Cytomegalovirus were negative. Because of animal exposure and insect contact, Borrelia burgdorferi, Borrelia spp., Rickettsia spp., Bartonella, Coxiella burnetii, Anaplasma/Ehrlichia, Brucella, and Toxoplasma (serum and CFS) tests were performed and were negative. Screening for HIV (serology and RNA), hepatitis A, B, and C, and Mycobacterium tuberculosis (CSF) was also negative. Second-line investigation: on day 4; West Nile, Toscana, Choriomeningitis, Yellow fever, Dengue, and Chikungunya arbovirus were negative. Third-line investigation: on day 10, because of the deterioration of the patient and the lack of an etiologic cause for the symptoms, alpha-herpesvirus and enterovirus were screened again, with negative results. In addition, as vector-borne disease was the most likely explanation for the patient’s disease, on day 14 (early convalescent phase) he was tested for Borrelia burgdorferi, Rickettsia conorii, and Coxiella burnetii (serum and whole blood), as well as Rickettsia spp., Bartonella, Coxiella burnetii, and Anaplasma/Ehrlichia (whole blood; frozen on day 7 [acute phase]) in parallel, with negative results. Finally, human herpesvirus-6, HHV-7, and human herpesvirus-8 were suspected in the absence of positive outcomes and presence of deterioration despite treatment with acyclovir. HHV-7 DNA was detected in the first CSF sample by Multiplex Nested PCR, which detects DNA from HHV-6, HHV-7, and HHV-8 on day 18 [2]. Fluorescent anti-HHV-7 IgG testing in serum samples on day 3 and days 14 and 21 revealed an increase in anti-HHV-7 titers from 1:32 to 1:64, in a retrospective analysis. However, HHV-7 antibody avidity testing, to determine primary infection vs reactivation of HHV-7 in the nervous system, could not be performed. Details of the microbiological assessment performed on the patient’s samples are shown in the Additional file 1: Table S1. Acyclovir was discontinued after microbiological diagnosis and the patient was treated with ganciclovir over 3 weeks.
Discussion
Our approach to this patient included a differential diagnosis that excluded noninfectious CNS diseases such as structural lesions, brain abscesses, parameningeal infections, and metabolic and toxic encephalopathies; however, a definitive diagnosis could not be established that discriminated between HHV-7 encephalitis or postinfectious encephalomyelitis. The detection of HHV-7 DNA in the patient’s CSF concomitant with neurological disease in association with the exclusion of all alternative etiological causes (according to the clinical practice guidelines of the Infectious Diseases Society of America [3]) supported HHV-7 as the possible cause of the encephalitis, based on the criteria that were established by Schwartz et al. [4]. As a consequence of antibody avidity could not be determined in our laboratory to differentiate between primary and past infection, we can not certainly establish whether encephalitis associated to HHV-7 infection in our patient was secondary to late primary infection or reactivation. Conversely, HHV-7 is a virus that is highly prevalent and has been detected in normal brain tissue [5]. Therefore, CSF PCR has a low positive predictive value. In fact, the patient had already improved before ganciclovir therapy was administered. Thus, a combination of HHV-7 primoinfection or reactivation and immune response is believed to have contributed to the development of encephalomyelitis. It is likely that HHV-7 was the infecting microorganism that was responsible for the immunological response, taking into account our patient’s clinical improvement after treatment with intravenous immunoglobulin therapy.
The case presented here contributes to the delineation of the approach to a patient profile with a similar clinical presentation and evolution to those presented in the literature [6,7,8,9,10,11]. All relevant information about these cases is presented in Table 1. In our case, despite the administration of empirical antiviral therapy with acyclovir as the first line for viral encephalitis, the patient developed polymyeloradiculopathy consisting of urinary retention, respiratory failure, and flaccid paralysis of the limbs, progressing to quadriplegia. Notably, these findings are similar to those of the HHV-7 encephalitis cases published previously, which occurred in both immunocompetent and nonimmunocompetent adults; this may alert clinicians to consider this specific etiology.
Conclusions
It may be concluded, regarding the importance of the confirmed laboratory diagnosis, that HHV-7 should be considered in the differential diagnosis of encephalopathy in patients with suspected infectious encephalitis who do not respond to acyclovir or in patients who develop acute polymyeloradiculopathy, considering that HHV-7 may be a pathological factor and that a timely diagnosis is crucial for the early administration of specific treatment.
References
Caselli E, Di Luca D. Molecular biology and clinical associations of Roseoloviruses human herpesvirus 6 and human herpesvirus 7. New Microbiol. 2007;30:173–87. Review.
Pozo F, Tenorio A. Detection and typing of lymphotropic herpesviruses by multiplex polymerase chain reaction. J Virol Methods. 1999;79:9–19.
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL, Hartman BJ, Kaplan SL, Scheld WM, Whitley RJ. Infectious Diseases Society of America. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;1(47):303–27.
Schwartz KL, Richardson SE, Ward KN, Donaldson C, MacGregor D, Banwell B, Mahant S, Bitnun A. Delayed primary HHV-7 infection and neurologic disease. Pediatrics. 2014;133:e1541–7.
Chan PK, Ng HK, Cheung JL, Ng KC, Cheng AF. Prevalence and distribution of human herpesvirus 7 in normal brain. J Med Virol. 2000;62:345–8.
Ward KN, Kalima P, MacLeod KM, Riordan T. Neuroinvasion during delayed primary HHV-7 infection in an immunocompetent adult with encephalitis and flaccid paralysis. J Med Virol. 2002;67:538–41.
Ward KN, White RP, Mackinnon S, Hanna M. Human herpesvirus-7 infection of the CNS with acute myelitis in an adult bone marrow recipient. Bone Marrow Transplant. 2002;30:983–5.
Mihara T, Mutoh T, Yoshikawa T, Yano S, Asano Y, Yamamoto H. Postinfectious myeloradiculoneuropathy with cranial nerve involvements associated with human herpesvirus 7 infection. Arch Neurol. 2005;62:1755–7.
Ginanneschi F, Donati D, Moschettini D, Dominici F, Cermelli C, Rossi A. Encephaloradiculomyelitis associated to HHV-7 and CMV co-infection in immunocompetent host. Clin Neurol Neurosurg. 2007;109:272–6.
Miranda CM, Torres TJP, Larrañaga LC, Acuña LG. Meningomyelitis associated with infection by human herpes virus 7: report of two cases. Rev Med Chil. 2011;139:1588–91.
Escobar-Villalba A, Sainz de la Maza S, Pérez Torre P, Galán JC, Rodríguez-Domínguez M, Monreal Laguillo E, Martínez Ulloa PL, Buisán Catevilla J, Corral I. Acute myelitis by human herpes virus 7 in an HIV-infected patient. J Clin Virol. 2016;77:63–5.
Kidd IM, Clark DA, Bremner JA, Pillay D, Griffiths PD, Emery VC. A multiplexPCR assay for the simultaneous detection of human herpesvirus 6 and human herpesvirus 7, with typing of HHV-6 by enzyme cleavage of PCR products. J Virol Methods. 1998 Jan;70(1):29-36.
Acknowledgements
The authors would like to acknowledge the staff at the Institute of Health Carlos III (National Centre for Microbiology, Madrid, Spain) for their support.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors’ contributions
MP carried out the collection of the patient’s microbiological data and drafted the manuscript. AA and CA carried out the collection of the patient’s clinical data and drafted the manuscript. CA and VS reviewed the literature and interpreted the data. AB acquired the data and contributed to draft the manuscript. MAG discussed the scientific issues regarding the patient’s management. DT carried out molecular genetic studies and AG carried out the fluorescent anti-HHV-7 IgG testing in serum samples. VS coordinate the management of the case and wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this report.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Elche University Hospital.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Microbiological assessment performed on the patient’s samples. (ODT 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Parra, M., Alcala, A., Amoros, C. et al. Encephalitis associated with human herpesvirus-7 infection in an immunocompetent adult. Virol J 14, 97 (2017). https://doi.org/10.1186/s12985-017-0764-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-017-0764-y