Abstract
Background
Although the use of highly active antiretroviral therapy in HIV positive individuals has proved to be effective in suppressing the virus to below detection limits of commonly used assays, virological failure associated with drug resistance is still a major challenge in some settings. The prevalence and effect of pre-treatment resistance associated variants on virological outcomes may also be underestimated because of reliance on conventional population sequencing data which excludes minority species. We investigated long term virological outcomes and the prevalence and pattern of pre-treatment minority drug resistance mutations in individuals initiating HAART at a local HIV clinic.
Methods
Patient’s records of viral load results and CD4 cell counts from routine treatment monitoring were used and additional pre-treatment blood samples for Sanger sequencing were obtained. A selection of pre-treatment samples from individuals who experienced virological failure were evaluated for minority resistance associated mutations to 1 % prevalence and compared to individuals who achieved viral suppression.
Results
At least one viral load result after 6 months or more of treatment was available for 65 out of 78 individuals followed for up to 33 months. Twenty (30.8 %) of the 65 individuals had detectable viremia and eight (12.3 %) of them had virological failure (viral load > 1000 RNA copies/ml) after at least 6 months of HAART. Viral suppression, achieved by month 8 to month 13, was followed by low level viremia in 10.8 % of patients and virological failure in one patient after month 20. There was potentially reduced activity to Emtricitabine or Tenofovir in three out of the eight cases in which minority drug resistance associated variants were investigated but detectable viremia occurred in one of these cases while the activity of Efavirenz was generally reduced in all the eight cases.
Conclusions
Early viral suppression was followed by low level viremia for some patients which may be an indication of failure to sustain viral suppression over time. The low level viremia may also be representing early stages of resistance development. The mutation patterns detected in the minority variants showed potential reduced drug sensitivity which highlights their potential to dominate after treatment initiation.
Trial registration
Not applicable.
Similar content being viewed by others
Background
Highly active antiretroviral therapy (HAART) has resulted in improved quality of life among people infected with human immunodeficiency virus (HIV) including reduced mortality and morbidity rates. However, virological failure caused by emergence of drug resistant variants still occurs in some individuals on HAART [1]. Some individuals experience virological failure after HAART initiation as they may harbour pre-treatment drug resistant viral species [2–4]. HIV treatment guidelines from developed countries recommend drug resistance testing before initiation of HAART [5, 6]. In developing countries pre-treatment screening for drug resistant species is however not done as part of treatment optimization due to limited resources. Pre-treatment drug resistance data are usually obtained through conventional population sequencing methods which do not detect low level viral species with a frequency of less than 20 % [7, 8] and this may underestimate prevalence figures and the effect that these variants have on treatment outcomes.
The effect of pre-treatment resistance associated minority variants on treatment outcomes is a subject of many studies [7–14]. While some studies have reported lack of strong association between drug resistance minority variants and treatment outcomes [9, 10], there is also strong evidence suggesting otherwise. Patients with no detectable drug resistance mutations using the Sanger method but with low level resistance mutations detected by sensitive methods were shown to have a more than double increased risk of virological failure after initiating HAART [11]. Minority drug resistant species have been shown to reduce the effectiveness of first line non-nucleoside reverse transcriptase inhibitor (NNTRI) based regimens which are the widely used regimens in developing countries [12].
Viral load (VL) testing in individuals on HAART is the method used to detect HIV replication and virological failure. The measure of a successful HAART program would be a sustained viral suppression over time in individuals on the program. The South Africa HIV management guidelines recommend VL testing 6 months after HAART initiation followed by VL testing at 12 months and every 12 months thereafter [15]. Baseline drug resistance testing is not recommended but pre-treatment drug resistance prevalence figures of less than 5 % have been reported in South Africa [16]. We investigated long term virological outcomes and the pattern of pre-treatment minority drug resistance mutations in individuals initiating HAART at a local HIV clinic.
Methods
Participants
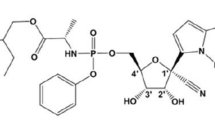
Participants were recruited from Tshwane District Hospital HIV clinic in Pretoria central, South Africa between July 2013 and May 2014 after written informed consent and followed up for at least 12 months and up to 33 months. Eligible participants were HIV infected treatment naïve adults with CD4 cell counts < 350 cells/μl and/or World Health Organization (WHO) clinical stage 3 or stage 4. Participants were initiated on a NNRTI based regimen consisting of Efavirenz (EFV), Emtricitabine (FTC) and Tenofovir (TDF).
Sample collection and RNA extraction
Samples were obtained before treatment initiation. Plasma was isolated from 10 to 15 ml of whole blood collected in EDTA tubes by centrifugation at 1600 g for 10 min and stored at −70 °C until required for RNA extraction. RNA was extracted from 210 μl of plasma using the QIAamp Viral RNA Mini kits (Qiagen) and eluted with 60 μl elution buffer.
Viral load monitoring
Follow up HIV-1 VLs for treatment monitoring were done after at least 6 months of treatment using Abbott Real Time HIV-1 test (Abbott laboratories, Illinois, USA) with a detection limit of 40 RNA copies/ml. Suppression was defined as a VL < 50 RNA copies/ml. Virological failure was defined as a VL ≥ 1000 RNA copies/ml after at least 6 months of HAART.
HIV genotypic resistance testing
A previously described method and primers was used for nucleic acid amplification and sequencing [17]. Superscript III reverse transcriptase enzyme (Life Technologies Corporation, California, USA) was used for cDNA synthesis and Platinum Taq enzyme (Life Technologies Corporation, California, USA) was used for the polymerase chain reaction (PCR). PCR primers targeted the protease (PR) gene and the first 300 codons of the reverse transcriptase (RT) gene (HXB2 nucleotide 2166–3440). BigDye Terminator V3.1 Cycle Sequencing Ready Reaction Kit (Applied Biosystems, Foster City, CA, USA) was used for sequencing reactions with two forward and two reverse primers and sequencing was done on the 3100 Automatic capillary sequencer (Applied Biosystems, Foster City, CA, USA). Sequences were edited and assembled on Sequencher V 4.5 (Gene Codes Corporation, USA). The Stanford HIVdb algorithm Version 7.0. (http://hivdb.stanford.edu/) was used for subtyping, resistance mutations interpretation and quality assessment.
HIV deep sequencing
For ultra-deep sequencing (UDS) amplicons obtained from pre-treatment samples from four individuals who experienced virological failure were sent to Inqaba Biotechnical industries in Pretoria South Africa for sequencing up to 1 % prevalence. Additional samples from three individuals who virally suppressed and one sample from an individual who experienced low level viremia were also deep sequenced to provide comparison.
Briefly, cDNA samples were fragmented using an ultrasonication approach and the resulting fragments were purified and size selected, end repaired and an illumina specific adapter sequence ligated. Following quantification, the samples were individually indexed and a second size selection step was performed using AMPure XP Beads. Libraries were quality controlled on a DNA chip (Agilent 2100 Bioanalyzer) and then sequenced on illumina’s MiSeq platform, using a MiSeq v3 kit according to the manufacturer’s protocol. Fifty (50) Mb of data (2 × 300bp long paired end reads) were produced for each sample. This was followed by HIV sequence analysis and quality check, genotyping and drug resistance interpretations using Deepchek 1.4 HIV analysis software. A minimum of 461 sequences was required for 99 % confidence at 1 % threshold and a Q30 score measure was applied for basecalling.
Pre-treatment drug resistance determination
Pre-treatment drug resistance was defined as identification of a mutation that is known to cause a reduced susceptibility to at least one prescribed drug.
Adherence monitoring
Adherence was monitored using a combination of measures including checking for missed clinic visits, participant interviews and investigating reasons for which participants had been sent for counselling sessions.
Statistical analysis
Differences between mean CD4 cell counts were calculated in excel using the t-test Two sample assuming equal variances.
Results
Enrolled participants characteristics and follow up
A total of 78 participants were recruited into the study. At least one follow up viral load result was available for 65 participants. Follow up viral loads were not available for 13 participants (16.6 %) due to loss to follow up. Participant characteristics are shown in Table 1.
Treatment initiation to first viral load monitoring
After treatment initiation, participants came for the first viral load monitoring at different time points (Fig. 1).
Time of first viral load testing after HAART initiation. The majority of participants (46) had at least one viral load (VL) test done by month 12 after HAART initiation. The first viral load test was done after month 12 in 15 (24.5 %) individuals. No viral load tests had been done by month 30 in 13 individuals
Virological outcomes
There were 20 participants (30.8 %) with detectable viremia at some point after at least 6 months of HAART (Fig. 2). Virological failure (>1000 RNA copies/ml) was detected in eight participants (12.3 %) with the following identification codes (IDs): L013, L029, L031, L037, L039, L054, L064 and L069 while the rest of the participants had low level viral loads < 1 000 RNA copies/ml. Virological failure occurred at 6–12 months after HAART initiation in six individuals (accounting for 9.2 % overall and 75 % in virological failure group) while virological failure occurred at 22 months in one individual (L039) who had initially achieved viral suppression.
There were eight participants (12.3 %), L022, L038, L039, L049, L058, L061, L063 and L067, who had initially suppressed the virus to below detection limits by month 8 to month 13 followed by detectable viremia at month 20 or after in all cases. The detected VLs after initial suppression were < 1 000 RNA copies/ml except for L039 with a VL of 21 646 RNA copies/ml. Subsequent viral load results after the initial rebound were available for two of these individuals, L038 and L039, and were done 10 and 3 months later respectively. The detectable viremia was shown to persist in both cases.
Immunological outcomes of participants with detectable viremia
There were no differences in mean baseline CD4 cell counts between the group that managed to achieve viral suppression and the groups with detectable viremia (Table 2). The same pattern was observed in CD4 cell counts done after 6–12 months of treatment. However, there was a significant difference between mean baseline CD4 cell counts and mean CD4 cell counts at 6–12 months after treatment initiation for the virally suppressed group and the low level viremia group. The virological failure group did not achieve a significant change in mean CD4 cell counts between these two time points. CD4 cell counts at time of virological failure were < 500 cells/μl (range = 21–441 cells/ μl) for six out of the eight participants while participant L013 who was virally suppressed at some point had a CD4 cell count > 500 cells/μl (Fig. 2). Of the eight participants who initially suppressed the virus but later had detectable viremia, three had CD4 cell counts < 350 cells/μl at the time of viral suppression, while four participants had CD4 cell counts > 350 (range = 427–746 cells/μl) (Fig. 2).
Baseline minority resistance mutations in participants with detectable viremia
Detection of baseline minority resistance associated mutations using ultra deep sequencing to 1 % threshold was done for eight participants. The coverage and basis for excluding some mutations from analysis is shown in Fig. 3 and Additional file 1: Figure S1. Of these eight participants: four had virological failure (>1000 RNA copies/ml), one had low level viremia < 1 000 RNA copies/ml and three had suppressed viremia (<50 RNA copies/ml) after at least 6 months of HAART. The mutations list and patterns are shown in Table 3.
Deep sequencing coverage of analysed samples. a Showing L013 (virological failure) and (b) showing L001 (virally suppressed). Mutations were excluded from analysis for any of the following: noisy mutations filtering, coverage filtering, forward/reverse unbalanced frequency and forward/reverse unbalanced coverage. Additional file 1: Figure S1 shows the rest of the samples. C – E (virological failure, L031, L054 and L064 respectively) and F – H (detectable viremia, L009 and virally suppressed L074 and L075 respectively)
Impact of treatment efficacy of initiated drugs
NRTI drugs TDF or FTC had potentially reduced activity in three out of the eight cases in which minority drug resistance associated variants were detected but detectable viremia occurred in one of these cases. The activity of EFV was reduced in all the eight cases ranging from low level resistance (two cases) to high level resistance (1 case). Taken together, the pattern of minority variants detected showed potentially reduced EFV treatment efficacy and were generally susceptible to the NRTI drugs TDF and FTC at 1 % prevalence.
Discussion
The goal of HIV antiretroviral therapy is to achieve sustained viral suppression in individuals on treatment. Virological failure due to development of drug resistance is still a challenge for many HIV treatment programmes in developing countries due to lack of resources for effective treatment monitoring and treatment optimization among other challenges. Furthermore, the effect of pre-treatment resistance associated minority variants on virological outcomes is still not well understood and largely underestimated because of reliance on conventional population sequencing data which do not include minority species. In this long term follow up study, baseline samples showed a high prevalence of pre-treatment resistance associated minority variants although their clinical relevance requires further study. There was high prevalence (30.8 %) of detectable viremia of any kind after at least 6 months of HAART and in 40 % of these cases detectable viremia occurred after previous viral suppression to below detection limits.
Virological failure occurred in 12.3 % of the participants compared to an overall 15 % virological failure rate (range 0–43 %) calculated from 19 studies done in sub-Saharan Africa countries [18]. However the duration of treatment at time of failure detection was not mentioned for most of these studies. We detected virological failure at month 6 to 12 after initiation of HAART except where virological failure was detected after previous viral suppression. Viral load testing at month 6 and month 12 after HAART initiation, which is recommended in South African public health institutions caring for HIV positive patients, seems adequate to detect early virological failure as was shown in our participants. However, up to 23.1 % of participants as indicated in Fig. 1 had their first post HAART initiation viral load after more than 12 months which may affect the detection of early virological failure. South Africa HIV management guidelines [15] use a cut off value of VL > 1000 RNA copies/ml to define virological failure, however HIV treatment guidelines from some developed countries are more stringent and define virological failure as confirmed VL > 50 RNA copies/ ml [5, 6]. Using this criterion, our frequency of virological failure would increase by more than 50 % from 12.3 to 30.8 %.
We noted that viral suppression had been achieved by month 8 to month 13 and viral rebound occurred after month 20 in a subset of individuals indicating failure to sustain viral suppression over time. Although the rebound resulted in low level viremia ranging from 83 RNA copies/ml to 579 RNA copies/ml in seven of the cases, detection of low level viremia after previous viral suppression should be monitored as these detections may be early stages of resistance development.
The association of pre-treatment minority drug resistance associated HIV variants of < 1 % frequency or greater with increased risk of virological failure for individuals on NNRTI based regimens has been highlighted [12]. The mutation patterns detected in the minority variants showed potentially reduced sensitivity to EFV and to a lesser extent TDF and FTC which highlights their potential to dominate after treatment initiation. However, the comparison of the pre-treatment pattern of minority variants detected between the virological failure group and the suppressed group did not show a specific pattern associated with virological failure at this stage indicating that other factors might be involved. Factors such as mutation linkages and mutational loads also need to be investigated. A single TAM D67E was found to be highly prevalent but TDF-based regimens have been shown to be effective in the presence of other single TAMs such as M41L at baseline [19]. Pre-treatment minority TAMs M41L and K70R have been reported in other studies [20] including multiple TAMs of up to six in another study [13].
Pre-treatment HIV drug resistance has been shown to increase regimen switches in developing countries [2] which results in increased treatment costs and exhaustion of treatment options. Recent studies have also demonstrated strong association between low level viremia of 200–499 RNA copies/ml with virological failure [21] while some studies have associated virological failure with lower levels of less than 50 copies per ml [22] after a follow up period of up to 2 years. This compares with our results where viremia after initial suppression was detected at month 20 and after and shown to persist on subsequent testing. Low level viremia may also be viewed in light of the correlation between viral persistence and the viral reservoir size which may require several years of HAART to reduce [23, 24].
We noted that 43 % of individuals who experienced low level viral rebound after initially suppressing the virus generally had poor immunological outcomes with a CD4 cell count < 350 cells/μl after more than 6 months of HAART. The same poor immunological outcome pattern was observed in individuals who experienced virological failure where 75 % of them had a CD4 cell count < 350 cells/μl. However CD4 cell count monitoring in isolation has been shown to be a poor marker for treatment failure [25, 26] and in our case we had a minority of individuals with CD4 cell counts > 500 experiencing virological failure or viral rebound.
The study has a number of limitations in particular the absence of resistance data at the time of virological failure. Additional samples taken at the time of routine viral load testing were not always available since the researchers were not part of the routine patient care personnel at the clinic where participants accessed care. The small number of samples that were deep sequenced also limited the information and conclusions that could be derived from this data. The data obtained however provide a basis for further investigation using larger sample sizes and comparison of baseline minority mutations with sequences dominating at time of failure. We also relied on self-reported information on treatment adherence to monitor participant’s treatment adherence levels. Poor adherence to treatment may have been the cause of virological failure in some individuals given that there was a high loss to follow up of 20 % in our cohort. Many studies have shown that poor treatment adherence is associated with virological failure in resource limited settings [27–30] and that an adherence of at least 95 % in individuals with minority variants significantly lowers the risk of virological failure [12].
Conclusions
While the development of low level viremia or virological failure after previously suppressing the virus that we noticed in a subgroup of our participants could be due to viral persistence emanating from established viral reservoirs, there is need to establish if such occurrences might be due to resistant minority variants beginning to take over and dominate following suppression of the treatment sensitive population. These data therefore highlight the need for a better understanding of the role played by pre-treatment HIV drug resistance associated minority variants under various clinical settings.
References
Bulteel N, Bansi-Matharu L, Churchill D, et al. The emergence of drug resistant HIV variants at virological failure of HAART combinations containing efavirenz, tenofovir and lamivudine or emtricitabine within the UK Collaborative HIV Cohort. J Infect. 2014;68(1):77–84.
Boender TS, Hoenderboom BM, Sigaloff KC, et al. Pretreatment HIV drug resistance increases regimen switches in Sub-Saharan Africa. Clin Infect Dis. 2015;61(11):1749–58.
Kantor R, Smeaton L, Vardhanabhuti S, et al. Pre-treatment HIV drug resistance and HIV-1 subtype C are independently associated with virologic failure: results from the multi-national PEARLS (ACTG A5175) clinical trial. Clin Infect Dis. 2015;60(10):1541–9.
Phanuphak P, Sirivichayakul S, Jiamsakul A, et al. Transmitted drug resistance and antiretroviral treatment outcomes in non-subtype B HIV-1-infected patients in South East Asia. J Acquir Immune Defic Syndr (1999). 2014;66(1):74–9.
European AIDS Clinical Society. Guidelines version 8.0, October 2015. http://www.eacsociety.org/files/guidelines_8_0-english_web.pdf. Accessed 26 Oct 2015.
Asboe D, Aitken C, Boffito M, et al. British HIV Association guidelines for the routine investigation and monitoring of adult HIV-1-infected individuals 2011. HIV Med. 2012;1:1–44.
Gianella S, Richman DD. Minority variants of drug-resistant HIV. J Infect Dis. 2010;202:657–66.
Chabria S, Gupta S, Kozal MJ. Deep sequencing of HIV: clinical and research applications. Annu Rev Genomics Hum Genet. 2014;15:295–325.
Jakobsen MR, Tolstrup M, Søgaard OS, et al. Transmission of HIV-1 drug-resistant variants: prevalence and effect on treatment outcome. Clin Infect Dis. 2010;50(4):566–73.
Peuchant O, Thiébaut R, Capdepont S, et al. Transmission of HIV-1 minority-resistant variants and response to first-line antiretroviral therapy. AIDS. 2008;22(12):1417–23.
Geretti AM, Paredes R, Kozal MJ. Transmission of HIV drug resistance: lessons from sensitive screening assays. Curr Opin Infect Dis. 2015;28(1):23–30.
Li JZ, Paredes R, Ribaudo HJ, et al. Low-frequency HIV-1 drug resistance mutations and risk of NNRTI-based antiretroviral treatment failure: a systematic review and pooled analysis. JAMA. 2011;305(13):1327–35.
Lataillade M, Chiarella J, Yang R, et al. Prevalence and clinical significance of HIV drug resistance mutations by ultra-deep sequencing in antiretroviral-naive subjects in the CASTLE study. PLoS One. 2010;5, e10952.
Paredes R, Lalama CM, Ribaudo HJ, et al. Pre-existing minority drug-resistant HIV-1 variants, adherence, and risk of antiretroviral treatment failure. J Infect Dis. 2010;201:662–71.
National consolidated guidelines for the prevention of mother to child transmission of HIV (PMTCT) and management of HIV in children, adolescents and adults. National Department of Health, South Africa. 2015. http://www.health.gov.za/index.php/2014-03-17-09-09-38/policies-andguidelines/category/230-2015p##. Accessed 26 Oct 2015.
Manasa J, Katzenstein D, Cassol S, Newell ML, de Oliveira T. Southern Africa Treatment And Resistance Network (SATuRN). Primary drug resistance in South Africa: data from 10 years of surveys. AIDS Res Hum Retroviruses. 2012;28(6):558–65.
Manasa J, Danaviah S, Pillay S, et al. An affordable HIV-1 drug resistance monitoring method for resource limited settings. J Vis Exp. 2014;85, e51242.
Barth RE, van der Loeff MFS, Schuurman R, Hoepelman AL, Wensing AM. Virological follow-up of adult patients in antiretroviral treatment programmes in sub-saharan Africa: a systematic review. Lancet Infect Dis. 2010;10:155–66.
Pingen M, Nijhuis M, Mudrikova T, van Laarhoven A, Langebeek N, Richter C, Boucher CA. Infection with the frequently transmitted HIV-1 M41L variant has no influence on selection of tenofovir resistance. J Antimicrob Chemother. 2015;70(2):573–80.
Johnson JA, Li JF, Wei X, et al. Minority HIV-1 drug resistance mutations are present in antiretroviral treatment–naïve populations and associate with reduced treatment efficacy. PLoS Med. 2008;5(7), e158.
Antiretroviral Therapy Cohort Collaboration (ART-CC), Vandenhende MA, Ingle S, et al. Impact of low-levelviremia on clinical and virological outcomes in treated HIV-1-infected patients. AIDS. 2015;29(3):373–83.
Calcagno A, Motta I, Ghisetti V, et al. HIV-1 very low level viremia is associated with virological failure in highly active antiretroviral treatment-treated patients. AIDS Res Hum Retroviruses. 2015;31(10):999–1008.
Chun TW, Murray D, Justement JS, Hallahan CW, Moir S, Kovacs C, Fauci AS. Relationship between residual plasma viremia and the size of HIV proviral DNA reservoirs in infected individuals receiving effective antiretroviral therapy. J Infect Dis. 2011;204(1):135–8.
Wirden M, Todesco E, Valantin MA, et al. Low-level HIV-1 viraemia in patients on HAART: risk factors and management in clinical practice. J Antimicrob Chemother. 2015;70(8):2347–53.
Rawizza HE, Chaplin B, Meloni ST, et al. Immunologic criteria are poor predictors of virologic outcome: Implications of HIV treatment monitoring in resource-limited settings. Clin Infect Dis. 2011;53(12):1283–90.
Anude CJ, Eze E, Onyegbutulem HC, et al. Immuno-virologic outcomes and immuno-virologic discordance among adults alive and on anti-retroviral therapy at 12 months in Nigeria. BMC Infect Dis. 2013;13:113.
Datay MI, Boulle A, Mant D, Yudkin P. Associations with virologic treatment failure in adults on antiretroviral therapy in South Africa. J Acquir Immune Defic Syndr. 2010;54(5):489–95.
El-Khatib Z, Katzenstein D, Marrone G, et al. Adherence to drug re-fill is a useful early warning indicator of virologic and immunologic failure among HIV patients on first-line ART in South Africa. PLoS One. 2011;6(3), e17518.
Messou E, Chaix ML, Gabillard D, et al. Association between medication possession ratio, virologic failure and drug resistance in HIV-1-infected adults on antiretroviral therapy in Cote d’Ivoire. J Acquir Immune Defic Syndr. 2011;56:356–64.
Ekstrand ML, Shet A, Chandy S, et al. Suboptimal adherence associated with virological failure and resistance mutations to first-line highly active antiretroviral therapy (HAART) in Bangalore, India. Int Health. 2011;3:27–34.
Bennett DE, Camacho RJ, Otelea D, et al. Drug resistance mutations for surveillance of transmitted HIV-1 drug-resistance: 2009 update. PLoS One. 2009;4(3), e4724.
Funding
This work is based on the research supported by grants awards from South African Research Chairs Initiative of the Department of Science and Technology and National Research Foundation of South Africa (C.T. Tiemessen), the HIV Research Trust (M.L. Mzingwane), the National Health Laboratory Service Research Trust and the Poliomyelitis Research Foundation.
Authors’ contribution
MLM participated in the design of the study, recruited participants, collected data from patient’s records, carried out the sequencing assays, performed statistical analysis and drafted the manuscript. CTT participated in the design of the study and helped to draft the manuscript. KR coordinated and facilitated the ultra deep sequencing assays. SHM participated in the design of the study and helped in participants’ recruitment and collection of data from patient’s records. GH participated in analysis of ultra deep sequencing results. SMB conceived of the study and participated in its design. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was granted ethics approval by the University of Pretoria Faculty of Health Sciences Ethics committee (Protocol number 167/2013) and the Gauteng Province Tshwane Health Research committee (Project number 25/2013). Participants were recruited after written informed consent.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Figure S1.
Deep sequencing coverage. C – E shows sequencing coverage for samples with virologicalfailure (L031, L054 and L064 respectively), F shows coverage for a sample with detectable viremia (L009)and G and H show coverage for virally suppressed samples (L074 and L075 respectively). Mutations wereexcluded from analysis for any of the following: noisy mutations filtering, coverage filtering, forward/reverse unbalanced frequency and forward/reverse unbalanced coverage. (DOCX 1189 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mzingwane, M.L., Tiemessen, C.T., Richter, K.L. et al. Pre-treatment minority HIV-1 drug resistance mutations and long term virological outcomes: is prediction possible?. Virol J 13, 170 (2016). https://doi.org/10.1186/s12985-016-0628-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-016-0628-x