Abstract
Background
Gait impairment is a common complication of multiple sclerosis (MS). Gait limitations such as limited hip flexion, foot drop, and knee hyperextension often require external devices like crutches, canes, and orthoses. The effects of mobility-assistive technologies (MATs) prescribed to people with MS are not well understood, and current devices do not cater to the specific needs of these individuals. To address this, a passive unilateral hip flexion-assisting orthosis (HFO) was developed that uses resistance bands spanning the hip joint to redirect energy in the gait cycle. The purpose of this study was to investigate the short-term effects of the HFO on gait mechanics and muscle activation for people with and without MS. We hypothesized that (1) hip flexion would increase in the limb wearing the device, and (2) that muscle activity would increase in hip extensors, and decrease in hip flexors and plantar flexors.
Methods
Five healthy subjects and five subjects with MS walked for minute-long sessions with the device using three different levels of band stiffness. We analyzed peak hip flexion and extension angles, lower limb joint work, and muscle activity in eight muscles on the lower limbs and trunk. Single-subjects analysis was used due to inter-subject variability.
Results
For subjects with MS, the HFO caused an increase in peak hip flexion angle and a decrease in peak hip extension angle, confirming our first hypothesis. Healthy subjects showed less pronounced kinematic changes when using the device. Power generated at the hip was increased in most subjects while using the HFO. The second hypothesis was not confirmed, as muscle activity showed inconsistent results, however several subjects demonstrated increased hip extensor and trunk muscle activity with the HFO.
Conclusions
This exploratory study showed that the HFO was well-tolerated by healthy subjects and subjects with MS, and that it promoted more normative kinematics at the hip for those with MS. Future studies with longer exposure to the HFO and personalized assistance parameters are needed to understand the efficacy of the HFO for mobility assistance and rehabilitation for people with MS.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is chronic neurological disorder in which inflammation leads to the demyelination of nerve fibers and the eventual breakdown of neurons in the central nervous system. This damage causes a long-term accumulation of disability, resulting from sensory and motor impairments [1]. In 2015, over 2 million cases were reported globally [2], and an estimated 75% of people with MS experience mobility impairments over the course of their disease [3]. These deficits, often emerging in early adulthood, constrain activities of daily living and appear to negatively affect quality-of-life [4].
MS-related symptoms such as muscle weakness, spasticity, and sensory changes are highly variable across individuals. Symptoms can vary throughout the day due to fatigue, and as the disease progresses, individuals can experience relapses, remissions, and increasing disability [3, 5, 6]. The effects of MS on gait often include reductions in step length, walking speed, dynamic stability, and range of motion (ROM) in lower limb joints [7,8,9,10].
To address the various mobility limitations caused by MS, a wide range of devices are prescribed to patients. While severe impairments necessitate wheelchairs, ambulatory people with MS often use ankle–foot orthoses (AFOs), crutches, canes, or walkers. While these are helpful interventions for walking impairments, the variability of gait impairment amongst individuals with MS and the lack of evidence-based practice in prescribing mobility devices to people with MS have led to high rates of abandonment and low satisfaction with this equipment [11, 12]. For instance, a common manifestation of MS is difficulty clearing the foot during the swing phase of gait, which is often attributed to dorsiflexion and eversion weakness in the ankle. AFOs are frequently prescribed in this situation [13, 14]. While the literature has shown that AFOs can produce measurable gait improvements in people recovering from stroke [15,16,17,18,19], the data regarding their effects in the context of MS is sparse and inconclusive [13, 20, 21]. This demonstrates the lack of MS-specific research into mobility interventions, and the need for further development of mobility-assistive technologies (MATs) for people living with neurodegenerative disorders.
In recent years, research in MATs has focused on the development of wearable robotic exosuits and exoskeletons. These devices aim to augment human gait through the controlled actuation of motor-driven cables or pneumatic artificial muscles that span various joints in the lower limbs [22,23,24], or motors situated concentrically with joints [25, 26]. Studies have demonstrated that such technology can reduce muscle activation during unloaded [23, 27,28,29,30] and loaded walking [22, 31], and reduce the metabolic cost of walking in both healthy subjects [23, 27, 32,33,34] and subjects with post-stroke hemiparesis [35, 36]. While promising, the costs, power demands, environmental adaptability, noisiness, and size of these devices are hurdles that must be overcome for widespread adoption of this technology [37,38,39].
Despite the practical barriers currently preventing most exosuits from reaching consumers, the research related to these devices has been vital to learning about the biomechanical effects of augmenting forces about the lower-limb joints. Exosuit studies have demonstrated the virtues of carefully-timed assistive forces about the hip during walking [28,29,30,31, 33, 34]. Considering the crucial role that hip flexors play in the swing phase of gait [40, 41], the lack of clinically available hip-centric orthoses for mobility assistance suggests a need for more investigation in this area. In 2008, Sutliff et al. showed that a passive hip flexion-assisting orthosis, consisting of a waist belt with resistive components that span the hip and knee joints, improved clinical gait assessment scores in a group of people with MS over a 12-week period [42]. A similar passive device with elastic components spanning only the hip joint produced significant improvements in timed 6 and 10-min walk tests in a group of persons exhibiting hemiparetic gait post-stroke [43]. More recently, Panizzolo et al. found that a bilateral passive hip flexion device reduced net metabolic power compared to free walking in older healthy adults [44]. While these studies show promising results based on clinical and metabolic assessments, biomechanical investigations of passive hip orthoses that include inverse dynamics and muscle activity have not been published.
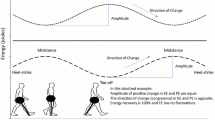
In this paper, we present a custom passive, lightweight, unilateral hip flexion orthosis (HFO), and investigate its biomechanical and neuromuscular effects on individuals with and without MS. The orthosis consists of elastic bands that span the hip joint, store energy during hip extension in stance, and release the stored energy to assist flexion upon swing initiation. This exploratory study examined the effects of passively augmenting hip flexion in impaired gait, and is an important step toward conducting quantitative biomechanical analyses of novel mobility interventions for people with MS.
The aim of this study was twofold: first, to determine whether people with and without MS can tolerate the HFO in steady-state, level walking; and second, to investigate subjects’ biomechanical and neuromotor responses to the HFO under three different stiffness configurations. While we detail the effects of the device for subjects with and without MS, this study does not attempt to match these two groups. The non-MS group was the initial cohort to test the device, and represents a general control response that can be used as a basis of comparison for further studies involving a variety of pathologies. Testing with the MS group followed the successful completion the non-MS trials, and serves as an exploratory study of the effects of a novel device on people with varying levels of mobility impairment due to a neurological disorder.
We hypothesize that that participants’ peak hip flexion angles will increase in the assisted leg while wearing the HFO, and that muscle activity will increase in hip extensors while wearing the HFO, and decrease in hip flexors and plantar flexors.
Materials and methods
Description of the passive unilateral hip flexion orthosis
In this study, our custom hip flexion orthosis is configured for unilateral assistance. The HFO (Fig. 1) consists of: a nylon waist belt for proximal anchoring of resistance bands with a neoprene fabric base layer to interface with the torso; an off-the-shelf neoprene knee brace for distal anchoring of the exercise bands; off-the-shelf elastic suspenders to support the waist belt and distribute tensile forces about the torso; and two resistance exercise bands (TheraBand®) to store and release mechanical energy throughout the gait cycle. The total cost of fabricating the HFO, including custom and off-the-shelf components, was approximately $65.
HFO Overview. a Waist anchors secure resistance bands to waist belt. Anchor locations can be individually adjusted about the belt. b Resistance exercise bands passively store and release energy during gait. c Knee brace for distal anchoring of bands. d Suspenders distribute load of bands about torso and help support waist belt. e Waist belt for proximal anchoring of bands. A soft neoprene base layer provides comfort, while a nylon webbing strap provides rigidity and connects to the waist anchors and suspenders
Each resistance band is tensioned between quick-release attachment points on the waist belt and knee brace, creating a passive flexion moment about the hip joint. The two bands are arranged antagonistically (crossing over at mid-thigh) to aid rotational stability and maintain a low profile. The band that anchors closer to the navel is referred to as the “medial” band, while the band that anchors near the iliac crest is called the “lateral” band. The locations of the waist anchors can be independently adjusted to meet the specific needs of the user.
The HFO is low-profile and it does not extend below the knee, allowing for simultaneous use of an AFO if desired. The HFO is also designed to cater to dexterity limitations experienced by people with MS [3]: when the user assumes a sitting position, tension in the bands is relieved, and the quick-release attachments can be easily connected or disconnected. The waist belt is fastened with a simple buckle, and with the suspenders it can be donned and doffed much like a backpack. The knee brace is fastened with two hook-and-loop straps.
Off-the-shelf resistance exercise bands are used to provide the assistive moment. These bands are commonplace in physical therapy clinics, where the HFO would be configured by the clinician. The wide range of available band stiffnesses provides the ability to adjust the HFO to an appropriate resistive force on a case-by-case basis.
Experimental design
This study was approved by the UT Dallas Institutional Review Board (MOD 1-CL 17-170), and participants provided written informed consent. Five volunteers with no mobility impairments and five volunteers with unilateral hip flexor weakness due to MS were recruited to wear the device configured in four different conditions: no resistive bands; nominal-stiffness bands (B1); intermediate-stiffness bands (B2); and high-stiffness bands (B3). Participant data can be found in Table 1. The MS participants were recruited from the Gait Disorder Clinic at the UT Southwestern School of Health Professions. Inclusion criteria were a confirmed diagnosis of MS, the ability to walk at least 150 feet without physical assistance (with or without an AFO), unilateral hip flexor weakness of 2+/5 or less as determined by Manual Muscle Testing [45], ages 18–75 years, and body mass index less than 35. Volunteers were excluded if they had other neurologic or orthopedic diagnoses that would negatively impact walking. Participants were encouraged not no rely on the handrails of the treadmill for walking, however light use of the treadmill handrails was permitted. One participant opted to wear an AFO during the trials.
Participants had no experience using the HFO prior to data collection. After recording anthropometric data, participants were fitted with the HFO. The leg to which the device was fitted is referred to as the assisted leg, and the other the unassisted leg. Individuals with MS wore the device on their weaker leg, and control subjects wore the device on their non-dominant leg. The distance between the proximal and distal attachment points for both bands was recorded in a neutral standing position, and band segments were sized to a resting length of 75% of this distance. This pre-tension value was chosen subjectively after preliminary tests found it to produce noticeable sensation in B1 without being prohibitively stiff in B3.
Participants with MS were allowed to self-select a comfortable walking pace under HFO assistance on a treadmill, and all controls walked at 1 m/s. We chose a fixed pace for the control group to allow for closer comparison across joint conditions of the joint angles, moment, and muscle activity, which are known to vary significantly with walking speed [46]. For participants with MS, it was not feasible to fix the pace given the varying functional abilities of the individuals in the group. When ready, trials were conducted wherein the subject was recorded for one minute of steady-state, level walking. First, a no-bands trial (N1) was captured for an initial baseline, followed by the nominal (B1), intermediate (B2), and stiff (B3) conditions, in randomized order. Participants completed further no-bands trials (N2, N3, and N4) following each band condition. An example of the full randomized protocol for a subject would be N1-B3-N2-B1-N3-B2-N4. Participants were allowed as much time as they desired to rest between trials.
Joint kinetics and kinematics
Three-dimensional kinematics were recorded by a ten-camera motion capture system (Vicon, Oxford, UK) at 100 Hz, and marker tracking was performed using Vicon Nexus. Three-dimensional ground reaction forces (GRFs) were recorded for each leg with an instrumented split-belt treadmill (Bertec, Columbus, OH, USA) at 2000 Hz. GRF and kinematic data were low-pass filtered (4th order Butterworth, 10 Hz cutoff) and inverse dynamics calculations were conducted in Visual3D (C-Motion, Kingston, ON, CA) to estimate joint moments and powers. Time integrals of positive and negative joint powers were calculated in Matlab (MathWorks, Natick, MA, USA) to estimate positive and negative joint work, respectively. The last ten good strides of each trial were used for statistical analysis. One control subject (C03) and one subject with MS (P05) were excluded from kinematic/kinetic analysis due to insufficient motion capture marker tracking.
Electromyography
Muscle activity was recorded at 2000 Hz with surface electromyography (EMG) sensors (Delsys Inc., Natick, MA, USA). Sensors were placed on the tibialis anterior (TA), gastrocnemius lateralis (GAS), soleus (SOL), rectus femoris (RF), vastus lateralis (VAS), biceps femoris (HAM), abdominal obliques (AB), and latissimus dorsi (LAT). Raw EMG signals were band-pass filtered (4th order Butterworth, 20–450 Hz cutoff), rectified, and then low-pass filtered (4th order Butterworth, 6 Hz cutoff) to obtain a linear envelope. Envelopes were normalized to the average peak amplitude of strides during N1. The mean normalized EMG values of the last ten good strides from each trial were used for statistical analysis. In several cases, EMG sensors made poor contact and were omitted from statistical analysis, and are left blank in the results.
Statistical analysis
Due to the small sample size and high variability of the functional levels of participants, single-subjects analysis was conducted, as group-level analysis would yield results not representative of any particular population [47, 48]. One-way ANOVAs (α = 0.05) were conducted on each observation of interest for each leg. When significant main effects were observed, post-hoc multiple comparisons using the Tukey–Kramer HSD test statistic were performed. These comparisons include all baseline tests for completeness [49], but only the significant pairwise comparisons between the initial baseline (N1) and band (B1, B2, B3) conditions in the assisted leg are reported here for brevity. Full ANOVA results including effect sizes and results on the non-device leg are reported in the Additional file 1. Statistics were computed in Matlab.
Results
We present a summary of all ANOVA results in Figs. 2 and 3. These figures indicate the significant pairwise results between initial baseline (N1) and subsequent conditions for all subjects. Rather than numerical values, we simply indicate the direction of change, if any, that was observed for a given subject and condition, to aid in identifying trends that may be present. Full numerical results can be viewed in Additional file 1.
Band conditions resuts overview. Peak flexion and extension angles, average positive, negative, and net work, and average muscle activity. Orange blocks indicate results significantly greater than N1 condition, blue blocks indicate results significantly less than N1, grey blocks represent no significant difference. Empty blocks are due to unusable EMG signals
Baseline conditions resuts overview. Peak flexion and extension angles, average positive, negative, and net work, and average muscle activity. Orange blocks indicate results significantly greater than N1 condition, blue blocks indicate results significantly less than N1, grey blocks represent no significant difference. Empty blocks are due to unusable EMG signals
Joint kinematics
Hip kinematics results are reported in Figs. 2 and 3, and averaged individual joint trajectories can be viewed in Fig. 4. In support of our hypothesis, all subjects with MS experienced a significant increase in peak hip flexion angle compared to baseline when using the HFO. While these effects were bilateral in several cases, they were more pronounced in the assisted leg, particularly during the B1 condition. Control subjects also showed increases in hip flexion, though not as drastic as those seen in subjects with MS, and with some band trials producing decreases in peak angle for C04 and C05.
Peak hip extension angles were significantly smaller for most MS and control subjects during HFO trials. Again, the greatest changes in peak angles were typically seen during the B1 condition. Significant results of both increases and decreases in hip kinematics were reported during subsequent baseline tests (N2, N3, N4) for both groups.
An increase in peak knee flexion angle was common, occurring for all subjects except for MS2 and C05, who saw decreases. These trends were observed in baseline and HFO trials.
Stance phase peak plantar flexion increased under at least one band condition for all subjects. Swing phase peak plantar flexion increased under at least one band condition for all of the MS group and decreased for C04 and C05. Peak dorsiflexion was largely unaffected, with primarily decreases observed. For most subjects, ankle kinematics experienced significant changes in both HFO and baseline trials.
Joint energetics
Positive work in the assisted hip increased during HFO trials for most subjects (MS3 and MS4 for all HFO conditions), but did not increase for these subjects during baseline trials (Fig. 5). Positive work in the unassisted hip was almost completely unaffected. Negative work in the assisted hip either decreased or remained the same for all subjects with MS and for most controls. The resulting net work produced by the assisted hip increased during HFO trials for all subjects with MS.
Work at the knee and ankle was less affected than at the hip, and there was no apparent trend in those results, with varied effects on both baseline and HFO trials.
Peak hip flexion moment on the assisted side significantly decreased for all participants with MS during the B1 condition compared with initial baseline. The unassisted side tended to increase slightly or remain unchanged (for unassisted side results, see Additional file 1). Hip extensor moments were less consistent across subjects, though MS1 and MS2 saw the greatest reduction in assisted-side hip extensor moments in the B1 trial.
Muscle activity
Significant results in muscle activity are reported in Figs. 2 and 3. We hypothesized that hip extensor (HAM) activity would increase, which was observed in MS2, MS3, MS5, C01, and C04 during HFO trials only. Meanwhile, MS1 and C03 showed decreases in HAM activity. We also hypothesized that hip flexor (RF) activity would be reduced, which was not the case with most of the collected data. A small reduction to RF activity was seen in MS4 B1, and in all band conditions for MS1, though the reductions seen in MS1 were comparable to those seen in their baseline trials. Finally, we hypothesized that plantar flexor (GAS, SOL) muscle activity would be reduced by the HFO. For GAS, only MS4 showed reductions in muscle activity exclusively during HFO trials (B1, B2). For SOL, results were similarly mixed, and no clear trends were observed.
Discussion
HFO efficacy
The primary purpose of this study was to evaluate the efficacy of a novel hip flexion orthosis worn by people with and without MS. All participants were able to complete trials for all conditions. The HFO was adjusted to successfully fit a wide range of body sizes, and was well-tolerated by all participants. The benefits of a low-profile, discrete device should not be overlooked; device abandonment due to non-acceptance by the user is common [50], and a lower profile device might not interfere as much with activities of daily living. Furthermore, the inexpensive materials with which the device was built would make it highly accessible to those in search of a walking aid, and easy to maintain given the availability of off-the shelf exercise bands.
Biomechanical results
Our hypothesis that hip kinematics in the assisted leg would shift towards flexion was largely supported by subjects with MS and several controls, particularly in the B1 condition. This change opposes the shift toward hip extension during swing that has been observed in people with MS [7]. These effects were more pronounced for subjects with MS, indicating that the HFO was able to “target” the pathological gait patterns exhibited in this group. While changes in kinematics do not necessarily reflect changes in energetics [51], the shift to greater hip flexion suggests an increase in foot clearance and lower risk of toe-drag. To highlight this shift toward normative kinematics, an inter-limb comparison of peak hip flexion angle for subjects with MS is given in Fig. 6. The B1 condition resulted in the lowest inter-limb hip angle asymmetry for all but MS3, and was lower than all baseline trials for subjects with MS.
The HFO demonstrated a contribution to positive work at the hip during swing by assisting concentric contraction (Fig. 5). During stance, it contributed to negative work at the hip by opposing extension. It has been shown that human locomotion requires a net positive amount of work, and that in unimpaired level walking, positive work done by the hip is substantially greater than negative work [52]. In this study, all subjects with MS showed the opposite condition, with negative work exceeding positive work at the hip. While wearing the HFO, however, the net work at the hip was more positive than in no-device trials in nearly every case. In the most extreme case (MS4 B2), we observed a shift to net positive work. These findings suggest that the redistribution of mechanical energy by the HFO improved walking for people with MS.
Our hypotheses that hip extensor muscle activity would increase and hip flexor and plantar flexor activity would decrease were not widely supported by the data collected. A major factor in the variability of the muscle activity data was the limited amount of strides analyzed during the relatively short periods of time that data was collected. Furthermore, MS causes the muscles to fatigue quickly, which has a substantial impact on the content of the EMG. Despite limitations, there was a significant increase in HAM activity compared with initial baseline for five of the subjects, including three from the MS group, however MS1 and C03 both saw decreases in HAM activity across conditions.
Device configuration
The variability seen in neuromuscular responses, including several instances of subjects showing opposite responses to the same conditions, emphasizes the need for highly customizable assistive devices for people with MS. The members of the MS group in this study demonstrated a wide range of functional ability, but all wore the device in the same three configurations for experimental control. The HFO can be configured in numerous ways, and a customized approach with a clinician would be more appropriate to tailor the setup to the needs of a given individual.
Even with such variability, a consistent result was that the B1 condition tended to produce more pronounced effects than the B2 or B3 conditions. This is a particularly noteworthy finding, because B1 had the lowest stiffness of the bands tested, thereby introducing the smallest external loading. This trend was not due to the stiffer bands restricting range of motion at the hip, as the range of hip motion was generally consistent across trials. This suggests that there is an upper limit on device effectiveness as band stiffness increases, and presents the need for exploration of lower-stiffness bands in future studies. It has been shown that there are diminishing returns with increased assistance magnitude for a powered hip exoskeleton [53], as well as with assistance onset timing for the same exoskeleton [33]. A similar phenomenon may be observed in the HFO, because both the magnitude and timing of its energy delivery are a function of the device configuration. Quantifying these parameters is not trivial: band stiffness, pre-tension, anchoring locations, user anthropometrics, device deformation, and individual gait characteristics all play a role in determining their values. Further exploration is required to determine the optimal energy storage characteristics for the passive elements in the HFO, and how to best assess individual needs when setting up the device.
The results of the present study demonstrate that an inexpensive and mechanically passive orthosis can produce significant effects on leg joint kinematics and energetics, and specifically in people with MS. The changes observed in participants with MS trended toward more normative gait kinematics, suggesting the device helped restore some functionality for these individuals.
Subsequent baseline trials
The N2, N3, and N4 trials were included to provide a baseline between the tests of the three different band stiffnesses, and to monitor the progression of the baseline condition. Inclusion of these trials showed that the initial baseline is subject to change substantially between device trials. Significant changes in subsequent baseline trials could be the result of acclimation to the task, or to carried-over effects of the device itself. In a longer-term study with fewer variables, inclusion of these baseline trials could help understand whether the device promotes motor learning in users, potentially providing rehabilitative benefits.
Limitations
The outcomes of this experiment are subject to several limitations. Small sample size and single testing session impacts the generalization of these findings. While controlling band stiffness and pre-tension across subjects was part of the design, it meant that individuals were not afforded the opportunity to acclimate to the HFO and make individualized adjustments as needed. Use of the treadmill versus overground walking may have altered the participants’ normal gait characteristics slightly. Treadmill speed was also held constant, so we could not observe the effects on preferred walking speed within subjects. The use of surface EMG sensors meant that muscle activity could not be measured in the iliopsoas, the strongest hip flexor. The highly variable population of subjects prevented meaningful group-level analysis.
Conclusions
This study presented a soft, passive, unilateral hip flexion orthosis that was well-tolerated by healthy adults and adults with MS under three levels of compliance. For subjects with MS, all device trials showed a statistically significant increase in the peak hip flexion angle of the assisted leg. Net work at the hip was more positive in people with MS when wearing the HFO. Muscle activity responses were highly varied, emphasizing the need for case-by-case adjustments to the device configuration. This study demonstrates the efficacy of the HFO as a mobility-assisting device for people with MS, and motivates the need for further investigation into the effects altering various parameters of the device. More generally, it demonstrates that passive devices can significantly affect walking mechanics, and that patient populations could benefit from redistribution, rather than addition, of mechanical energy from a wearable device.
Availability of data and materials
Additional file 1 contains numerical results of the ANOVAs whose significance are reported in Figs. 2 and 3 in table format, as well as the effect size for each test. It is an.xlsx file with four sheets: ankle, knee, hip, and muscle activity.
Additional file 2 contains the data from which ANOVAs were carried out. It in an.xlsx file with two sheets: joint mechanics and muscle activity. Each column, beginning at the top, consists of: the participant ID (as used in this manuscript); device or non-device leg; device condition; type of signal (i.e. angle, moment, power, muscle activity) and units; joint or muscle being measured; and 100 data points representing the full stride represented from heel strike to subsequent heel strike.
Abbreviations
- MS:
-
Multiple sclerosis
- MAT:
-
Mobility assistive technology
- HFO:
-
Hip flexion orthosis
- ROM:
-
Range of motion
- AFO:
-
Ankle–foot orthosis
- GRF:
-
Ground reaction force
- EMG:
-
Electromyography
- TA:
-
Tibialis anterior
- GAS:
-
Gastrocnemius lateralis
- SOL:
-
Soleus
- RF:
-
Rectus femoris
- VAS:
-
Vastis lateralis
- HAM:
-
Hamstring (biceps femoris)
- AB:
-
Abdominal obliques
- LAT:
-
Latissimus dorsi
References
Soldán MMP, Novotna M, Zeid NA, Kale N, Tutuncu M, Crusan DJ, et al. Relapses and disability accumulation in progressive multiple sclerosis. Neurology. 2015;84(1):81–8.
Wallin MT, Culpepper WJ, Nichols E, Bhutta ZA, Gebrehiwot TT, Hay SI, et al. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(3):269–85.
Salter AR, Cutter GR, Bacon TE, Herbert J. Disability in multiple sclerosis. Neurology. 2013;80:1018–24.
Zwibel HL. Contribution of impaired mobility and general symptoms to the burden of multiple sclerosis. Adv Ther. 2009;26(12):1043–57.
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372(9648):1502–17. https://doi.org/10.1016/S0140-6736(08)61620-7.
Hohol MJ, Weiner HL. Disease Steps in multiple sclerosis. Neurology. 1995;22:778.
Filli L, Sutter T, Easthope CS, Killeen T, Meyer C, Reuter K, et al. Profiling walking dysfunction in multiple sclerosis: characterisation, classification and progression over time. Sci Rep. 2018;8(1):1–13.
Pau M, Coghe G, Atzeni C, Corona F, Pilloni G, Marrosu MG, et al. Novel characterization of gait impairments in people with multiple sclerosis by means of the gait profile score. J Neurol Sci. 2014;345(1):159–63. https://doi.org/10.1016/j.jns.2014.07.032.
Thoumie P, Lamotte D, Cantalloube S, Faucher M, Amarenco G. Motor determinants of gait in 100 ambulatory patients with multiple sclerosis. Mult Scler. 2005;11(4):485–91. https://doi.org/10.1191/1352458505ms1176oa.
Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, et al. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult Scler. 2006;12(5):620–8.
Souza A, Kelleher A, Cooper RAR, Cooper RAR, Iezzoni LI, Collins DM. Multiple sclerosis and mobility-related assistive technology: systematic review of literature. J Rehabil Res Dev. 2010;47(3):213. http://www.rehab.research.va.gov/jour/10/473/pdf/souza.pdf
Fay BT, Boninger ML. The science behind mobility devices for individuals with multiple sclerosis. Med Eng Phys. 2002;24(6):375–83.
Sheffler LR, Hennessey MT, Knutson JS, Naples GG, Chae J. Functional effect of an ankle foot orthosis on gait in multiple sclerosis. Am J Phys Med Rehabil. 2008;87(1):26–32. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002060-200801000-00005
Davies BL, Hoffman RM, Healey K, Zabad R, Kurz MJ. Errors in the ankle plantarflexor force production are related to the gait deficits of individuals with multiple sclerosis. Hum Mov Sci. 2017;51:91–8. https://doi.org/10.1016/j.humov.2016.11.008.
Franceschini M, Massucci M, Ferrari L, Agosti M, Paroli C. Effects of an ankle-foot orthosis on spatiotemporal parameters and energy cost of hemiparetic gait. Clin Rehabil. 2003;17(4):368–72.
Gök H, Küçükdeveci A, Altinkaynak H, Yavuzer G, Ergin S. Effects of ankle-foot orthoses on hemiparetic gait. Clin Rehabil. 2003;17(2):137–9.
Pohl M, Mehrholz J. Immediate effects of an individually designed functional ankle-foot orthosis on stance and gait in hemiparetic patients. Clin Rehabil. 2006;20(4):324–30. https://doi.org/10.1191/0269215506cr951oa.
Danielsson A, Sunnerhagen KS. Energy expenditure in stroke subjects walking with a carbon composite ankle foot orthosis. J Rehabil Med. 2004;36(4):165–8.
Leung J, Moseley AM. Impact of ankle-foot orthoses on gait and leg muscle activity in adults with hemiplegia. Physiotherapy. 2003;89(1):39–60.
Ramdharry GM, Marsden JF, Day BL, Thompson AJ. De-stabilizing and training effects of foot orthoses in multiple sclerosis. Mult Scler J. 2006;12(2):219–26. https://www.researchgate.net/profile/Gita_Ramdharry/publication/7152055_De-stabilizing_and_training_effects_of_foot_orthoses_in_multiple_sclerosis/links/0c960528ba149124e9000000.pdf
Cattaneo D, Marazzini F, Crippa A, Cardini R. Do static or dynamic AFOs improve balance? Clin Rehabil. 2002;16(8):894–9.
Panizzolo FA, Galiana I, Asbeck AT, Siviy C, Schmidt K, Holt KG, et al. A biologically-inspired multi-joint soft exosuit that can reduce the energy cost of loaded walking. J Neuroeng Rehabil. 2016;13(1):43. https://doi.org/10.1186/s12984-016-0150-9.
Mooney LM, Rouse EJ, Herr HM. Autonomous exoskeleton reduces metabolic cost of human walking. J Neuroeng Rehabil. 2014;11(1):151. https://doi.org/10.1186/1743-0003-11-151.
Do Nascimento BG, Vimieiro CBS, Nagem DAP, Pinotti M. Hip orthosis powered by pneumatic artificial muscle: Voluntary activation in absence of myoelectrical signal. Artif Organs. 2008;32(4):317–22.
Giovacchini F, Vannetti F, Fantozzi M, Cempini M, Cortese M, Parri A, et al. A light-weight active orthosis for hip movement assistance. Rob Auton Syst. 2015;73:123–34. https://doi.org/10.1016/j.robot.2014.08.015.
Jung S, Kim C, Park J, Yu D, Park J, Choi J. A wearable robotic orthosis with a spring-assist actuator. In: Proceedings of Annual international conference of the IEEE engineering in medicine and biology society EMBS. 2016, p 5051–4.
Young AJ, Gannon H, Ferris DP. A biomechanical comparison of proportional electromyography control to biological torque control using a powered hip exoskeleton. Front Bioeng Biotechnol. 2017;5:87. https://doi.org/10.3389/fbioe.2017.00037/full.
Lee J, Seo K, Lim B, Jang J, Kim K, Choi H. Effects of assistance timing on metabolic cost, assistance power, and gait parameters for a hip-type exoskeleton. IEEE Int Conf Rehabil Robot. 2017;45:498–504.
Lenzi T, Carrozza MC, Agrawal SK. Powered hip exoskeletons can reduce the user’s hip and ankle muscle activations during walking. IEEE Trans Neural Syst Rehabil Eng. 2013;21(6):938–48.
Grazi L, Crea S, Parri A, Lova RM, Micera S, Vitiello N. Gastrocnemius myoelectric control of a robotic hip exoskeleton can reduce the user’s lower-limb muscle activities at push off. Front Neurosci. 2018;12:1–11.
Ding Y, Panizzolo FA, Siviy C, Malcolm P, Galiana I, Holt KG, et al. Effect of timing of hip extension assistance during loaded walking with a soft exosuit. J Neuroeng Rehabil. 2016;13(1):1–10. https://doi.org/10.1186/s12984-016-0196-8.
Quinlivan BT, Lee S, Malcolm P, Rossi DM, Grimmer M, Siviy C, et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Sci Robot. 2017;2(2):4416. https://doi.org/10.1126/scirobotics.aah4416.
Young AJ, Foss J, Gannon H, Ferris DP. Influence of power delivery timing on the energetics and biomechanics of humans wearing a hip exoskeleton. Front Bioeng Biotechnol. 2017;5:1–11. https://doi.org/10.3389/fbioe.2017.00004/full.
Ding Y, Kim M, Kuindersma S, Walsh CJ. Human-in-the-loop optimization of hip assistance with a soft exosuit during walking. Sci Robot. 2018;3(15):5438. https://doi.org/10.1126/scirobotics.aar5438.
Awad LN, Bae J, O’Donnell K, De Rossi SMM, Hendron K, Sloot LH, et al. A soft robotic exosuit improves walking in patients after stroke. Sci Transl Med. 2017;9(400):9084. https://doi.org/10.1126/scitranslmed.aai9084.
Takahashi KZ, Lewek MD, Sawicki GS. A neuromechanics-based powered ankle exoskeleton to assist walking post-stroke: a feasibility study. J Neuroeng Rehabil. 2015;12(1):1–13.
Zhang Y, Arakelian V, Baron JLE. Design concepts and functional particularities of wearable walking assist devices and power-assist suits—a review. In: Proceedings of 58th international conference of machine design departments. 2017(September):436–41.
Schiele A. Ergonomics of exoskeletons: objective performance metrics. In: Proceedings of 3rd Jt EuroHaptics Conf Symp Haptic Interfaces Virtual Environ Teleoperator Syst World Haptics 2009. 2009;103–8.
Burton A. Expecting exoskeletons for more than spinal cord injury. Lancet Neurol. 2018;17(4):302–3. https://doi.org/10.1016/S1474-4422(18)30074-7.
Campanini I, Merlo A, Damiano B. A method to differentiate the causes of stiff-knee gait in stroke patients. Gait Posture. 2013;38(2):165–9. https://doi.org/10.1016/j.gaitpost.2013.05.003.
Goldberg SR, Anderson FC, Pandy MG, Delp SL. Muscles that influence knee flexion velocity in double support: implications for stiff-knee gait. J Biomech. 2004;37(8):1189–96.
Sutliff MH, Naft JM, Stough DK, Lee JC, Arrigain SS, Bethoux FA. Efficacy and safety of a hip flexion assist orthosis in ambulatory multiple sclerosis patients. Arch Phys Med Rehabil. 2008;89(8):1611–7.
Carda S, Invernizzi M, Cognolato G, Piccoli E, Baricich A, Cisari C. Efficacy of a hip flexion assist orthosis in adults with hemiparesis after stroke. Phys Ther. 2012;92(5):734–9. https://doi.org/10.2522/ptj.20110112.
Panizzolo FA, Freisinger GM, Karavas N, Eckert-Erdheim AM, Siviy C, Long A, et al. Metabolic cost adaptations during training with a soft exosuit assisting the hip joint. Sci Rep. 2019;9(1):1–10.
Hislop H, Avers D, Brown M. Daniels and Worthingham’s muscle testing: techniques of manual examination. 9th ed. Elsevier; 2013. 528 p.
Neptune RR, Sasaki K, Kautz SA. The effect of walking speed on muscle function and mechanical energetics. Gait Posture. 2008;28:135–43.
Bates BT. Single-subject methodology: an alternative methodology. Med Sci Sport Exerc. 1996;28:631.
Bates BT, Dufek JS, James CR, Harry JR, Eggleston JD. Measurement in physical education and exercise science the influence of experimental design on the detection of performance differences the influence of experimental design on the detection of performance differences. Meas Phys Educ Exerc Sci. 2016;20(4):200–7. http://shapeamerica.tandfonline.com/action/journalInformation?journalCode=hmpe20
Stergiou N, Scott MM. Baseline measures are altered in biomechanical studies. J Biomech. 2005;38(1):175–8.
Verza R, Lopes Carvalho ML, Battaglia MA, Messmer UM. An interdisciplinary approach to evaluating the need for assistive technology reduces equipment abandonment. Mult Scler. 2006;12(1):88–93.
Lewis CL, Ferris DP. Invariant hip moment pattern while walking with a robotic hip exoskeleton. J Biomech. 2011;44(5):789–93. https://doi.org/10.1016/j.jbiomech.2011.01.030.
DeVita P, Helseth J, Hortobagyi T. Muscles do more positive than negative work in human locomotion. J Exp Biol. 2007;210(19):3361–73.
Kang I, Hsu H, Young A. The effect of hip assistance levels on human energetic cost using robotic hip exoskeletons. IEEE Robot Autom Lett. 2019;4(2):430–7.
Acknowledgements
The authors would like to thank UTDesign and the efforts of design team members Adrian Alegre, Olufunto Faweya, Minh Nguyen, Matthew Pelto, and Michael Theisen in designing and fabricating the HFO.
Funding
This study was funded by The University of Texas at Dallas and UT Southwestern Medical Center.
Author information
Authors and Affiliations
Contributions
KM and SS proposed the HFO be designed, provided feedback during design, recruited and assessed functional level of participants with MS, contributed to carrying out experiments, and contributed to writing and editing the manuscript. NF oversaw design of the HFO, helped design experimental protocol, contributed to carrying out experiments, interpreting data, and editing the manuscript. RN and design team (see acknowledgements) designed and fabricated the HFO. RN contributed to designing experimental protocol and carrying out experiments, processed and analyzed biomechanical data, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the UT Dallas Institutional Review Board (MOD 1-CL 17-170).
Consent for publication
All individuals in the present study provided written informed to consent to use and publish their data.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. ANOVA numerical results including effect sizes and results from non-device-wearing leg.
Additional file 2
. Data from which ANOVAs were carried out in .xlsx format. Includes joint mechanics and muscle activity for both legs of all participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neuman, R.M., Shearin, S.M., McCain, K.J. et al. Biomechanical analysis of an unpowered hip flexion orthosis on individuals with and without multiple sclerosis. J NeuroEngineering Rehabil 18, 104 (2021). https://doi.org/10.1186/s12984-021-00891-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12984-021-00891-7