Abstract
Background
Globally Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome (HIV/AIDS) is an ongoing public health issue associated with high morbidity and mortality. Efforts have been made to reduce HIV/AIDS-related morbidity and mortality by delivering antiretroviral therapy. However, the incidence and predictors of mortality in border areas like Metema were not investigated. This study aimed to assess predictors of mortality rate among adult HIV-positive patients on antiretroviral therapy at Metema Hospital.
Methods
Retrospective follow-up study was employed among ART patients from January 1, 2013, to December 30, 2018. Data were entered in Epi-data 3.1 and exported to STATA 14 for analysis. Kaplan–Meier and Log-Rank test was used to compare survival differences among categories of different variables. In bi-variable analysis p-values < 0.20 were entered into a multivariable analysis. Multivariate Weibull model was used to measure the risk of death and identify the significant predictors of death. Variables that were statistically significant at p-value < 0.05 were concluded as predictors of mortality.
Result
A total of 542 study participants were included. The overall incidence rate was 6.7 (95% CI: 5.4–8.4) deaths per 100 person-years of observation. Being male (HR = 2.4; 95% CI: 1.24–4.62), STAGE IV (HR = 5.64; 95% CI: 2.53–12.56), stage III (HR = 3.31; 95% CI: 1.35–8.10), TB-coinfection (HR = 3.71; 95% CI: 1.59–8.64), low hemoglobin (HR = 4.14; 95% CI: 2.18–7.86), BMI ≤ 15.4 kg/m2 (HR = 2.45; 95% CI: 1.17–5.10) and viral load > 1000 copy/ml (HR = 6.70; 95% CI: 3.4–13.22) were found to be a significant predictor for mortality among HIV patients on ART treatment.
Conclusion
The incidence of death was high. Being male, viral load, those with advanced STAGE (III & IV), TB co-infected, low BMI, and low hemoglobin were at a higher risk of mortality. Special attention should be given to male patients and high public interventions needed among HIV patients on ART to reduce the mortality rate.
Similar content being viewed by others
Background
Globally Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome (HIV/AIDS) is an ongoing public health issue associated with high morbidity and mortality [1, 2]. An estimated 37 million people were living with HIV across the globe; among those, 70% reside in Sub-Saharan Africa [2,3,4].
Accessing antiretroviral therapy (ART) has been increased since 2005, globally an estimated 21.7 million people were accessing antiretroviral therapy (ART) and 940,000 people died from AIDS-related illnesses at the end of 2017 [3, 5, 6]. Even though the introduction of Highly active antiretroviral therapy (HAART) brought a significant reduction of mortality and morbidity among patients living with HIV (PLHIV), several patients die after starting ART [7,8,9]. Since the success of ART depends on regular patient follow up, treatment adherence and awareness of patients regarding the relevance of ART in his life [10, 11]. AIDS-related mortality among ART experienced patients’ ranges from 4.5 to 17% [12,13,14]. Ethiopia is one HIV high burden Sub-Saharan country where an estimated 610,000 HIV infected people and 15,000 AIDS-related mortality occurred at the end of 2017 [15, 16]. The prevalence of HIV in Ethiopia ranges from 1.13 to 1.4% in the Amhara region [17], Metema Hospital accounts for 6.3% of HIV prevalence [10]. The survival and epidemiology of HIV in Ethiopia vary along the study periods, geographic regions, and the study population [15, 18]. Many studies in Ethiopia indicated that the incidence of mortality among HIV-infected patients who are on ART ranges from 1.75 deaths per 100 person-years of observation to 7 death per 100-person year of observation which was lowest in Jinka and highest in Asela [19,20,21,22,23,24,25,26,27]. Despite the risk factors of mortality among people who are on ART were researched, some settings which provide HIV/AIDS care and treatment services for a high number of seasonal daily migrant workers (Mobile workers) and movable populations like Metema Hospital were not fully addressed. There was a high magnitude of HIV in Metema Hospital compared to regional and national reports. Even though governmental and many non-governmental organizations exerted great efforts on HIV care and treatment in Metema Hospitals in all settings. However, HIV/AIDS-related mortality continues a major public health concern in the area. As a result, there is a need for local data to provide evidence for organizations working on HIV/AIDS and ART at national, regional, and district levels on risk factors of mortality among HIV/AIDS patients who are on ART. Hence, this study aimed to determine the incidence and predictors of mortality among adult HIV/AIDS patients who were on ART at Metema Hospital, Ethiopia.
Methods
Study setting, design, and period
Institutional based retrospective follow-up study was conducted from January 1, 2013, to December 30, 2018, in Metema Hospital, which is located in west Gondar province of the Amhara National Regional State. It is 158 km away from Gondar town, 338 km from Bahir Dar (the capital of Amhara), and 908 km from the country’s capital Addis Ababa.
The town has a total population of 119,054 (63,433 males and 55,617 females) [45]. There are over 120,000 seasonal migrant workers (a majority of males) traveling to Metema for temporary labor and return to their original residence after 3–6 months of stay every year. The town is also noted for its border with Sudan Ethio-Sudan highway. Metema Hospital provides services for over 420,000 catchment population in West Gondar, Northwest Ethiopia, per year. Metema Hospital HIV/AIDS care and treatment clinic was established in 2005. It provides care, treatment, and monitoring for HIV-positive patients as per the national guideline.
Study population, sample size, and sampling procedure
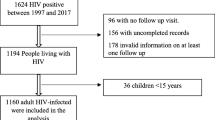
All adult HIV-positive individuals who were on ART at Metema Hospital and who enrolled from January 1, 2013, to December 30, 2018, were included. However, transferred in-patients with incomplete baseline data and unknown initiation date of treatment and status of patients were excluded. The sample size was estimated using Log-Rank and Cox proportional hazard model in STATA version 14. The calculation was done based on the assumption that type I error of 5%, power of 80% and the exposure is body mass index (BMI) the most significant variable [21]. Survival probability for patients with body mass index greater than 18.5 kg/m2 = 0.93. Based on this, the calculated sample size by using STATA 14 software is 542. Regarding the sampling technique, a record of study participants have been filtered first from the ART database according to their entry time to follow up, next patients have been filtered using age and eligibility criteria, then we give a unique number for the remaining records and select each record for our study using systematic random sampling.
Data collection technique and quality control issues
The outcome variable was the time event (death) of patients on ART. The independent variables considered in the study were socio-demographic characteristics such as age, sex, level of education, occupation, marital status, clinical factors like WHO clinical stage, CD4 count, functional status, TB/HIV co-infection, opportunistic infection other than TB, drug adherence, viral load, hemoglobin level, body mass index (BMI) and substance use which is a behavioral factor.
Drug adherence
In this study was based on records as Good (equal to or greater than 95% or ≤ 3 doses missed per month), Fair (85–94% or 4–8 doses missed per month) or Poor (less than 85% or ≥ 9 doses missed per month), health workers used reports by the patient or by directly counting the pills to classify adherence. Those patients who adhere greater than or equal to 95% was considered as good adherence; 85–94% fair adherence and Less than 85% was considered as poor adherence [28]. Patient more than three months late for a scheduled visit and who did not return later during follow-up was considered as lost to follow up [29].
The hemoglobin level > 10 gm/dl was categorized as normal hemoglobin and hemoglobin ≤ 10 gm/dl was categorized as low hemoglobin level [30]. In this study, viral load > 1000 copies/ml was recorded as high viral load and viral load ≤ 1000 copies/ml was recorded as low viral load [31]. Substance use was recorded as among those three factors such as alcohol, cigarette smoking, and khat chewing, with a minimum of one record documented in patients' charts or register present.
To assure the data quality, high emphasis was given in designing a data collection instrument. The training was given for data collectors and supervisors to have a common understanding of the purpose of research and the techniques of data collection. A standard checklist was used to record information extracted from electronic and patient cards. Before the actual data collection pretest was done on 25 patient charts, those charts were not included in the study. A standard checklist was used for recording information from the database and patient cards. This form was developed using the standardized ART entry and follow-up form employed by the ART clinic. Three experienced ART Nurses who were trained on comprehensive HIV care were involved in data collection. Throughout the data collection process, completeness, consistency, and accuracy were checked by supervisors and the principal investigator daily.
Data management and analysis
The data was entered in Epi-data 3.1 and exported to STATA 14 for analysis. Descriptive statistics including proportions, median, tables, and charts was done to describe the characteristics of study participants. Nonparametric estimations of Kaplan–Meier was done graphically and Log-rank test was used to compare the survival probabilities of categorical variables. After fitting the survival model, the proportional hazard assumption was checked using a graphical and global test (goodness test). The model goodness of fit was checked by using the Cox-Snell residual. Cox proportional and parametric models were compared using Akaike Information Criteria (AIC) or Bayesian Information Criteria (BIC). Weibull model was selected since they have low value of AIC and had a good fitness of the Cox Snell residual. Those covariates with a p-value < 0.2 in the bi-variable analysis were again fitted to the multivariable Weibull regression analysis. Both crud and adjusted hazard ratio with the corresponding 95% Confidence Interval (CI) was calculated to show the strength of association. In multivariable analysis, covariates with a p-value of < 0.05 were considered statistically significant.
Results
Baseline Scio-demographic, Clinical, and treatment-related characteristics
A total of 542 HIV infected patients on ART were included in this study. Among those, more than half of the 285 (52.6%) study participants were females. The median age of study participants was 32 (IQR = 26–39) years. Nearly two-thirds of the study participants were not educated. Almost half of the 278 (51.3%) study participants disclosed their HIV status and nearly half of the 274 (50.5%) study subjects are co-infected with tuberculosis (TB) (Table 1). Among the study subjects, 179 (33.0%) had a baseline CD4 count < 200 cells/mm3, and the baseline WHO staging 2470 (45.6%) of patients were at stage I followed by stage III and stage IV 115 (21.2%). Most of the 413 (76.2%) of the study participants had working functional status and three-fourths of the study subjects had good treatment adherence (Table 1).
Incidence of mortality
The study subjects followed a total of 72 months after initiation of treatment with a total observation time of 1245 person years. During those total follow up period, the overall incidence rate of mortality was 6.7 (95% CI (5.4–8.4)) per 100-person year of observation. Over the 72 months follow-up period; 4.9 per 100 adult-months (95% CI 3.7–6.3) died during the first 12 months and 0.7 per 100 adult-months (95% CI 0.4–1.1) died during the second year of follow-up. The cumulative survival probability of patients on ART was 77.44% at the end of the study period (Fig. 1).
Comparison of survival experience by different factors
Using the Kaplan–Meier survival curve, the survival experience of the patients was assessed with different categories of predictor variables. Patients with normal hemoglobin had a longer survival experience than those adults with low hemoglobin (Fig. 2) and the difference were statistically significant (Log-Rank, p < 0.001) (Table 2). The observed difference of longer survival of patients with a viral load below threshold compared with those adults above the threshold was found to be statistically significant (Log-Rank, p < 0.001) (Table 2). Patients with TB-co-infection at the era of ART were shorter survival experience than those adults with no TB co-infection (Fig. 2) and the difference were statistically significant (Log-Rank p < 0.001) (Table 2).
Assessing proportional hazard assumption and model selection criteria
Graphical assessment of the proportional hazard assumption was done by comparing the estimated ln(–ln) survivor curves versus ln (survival time) over different categories of variables. The graph of the two categories of tuberculosis and hemoglobin level hazards does not cross each other, which means that the proportional hazard assumption was satisfied (Fig. 3). An additional global test of proportional-hazard assumption based on the Schoenfeld residuals was done and all independent variables satisfy the proportional hazard assumption (Chi square = 11.76, p-value = 0.6971) (Table 3). The model with the smallest value of AIC and BIC was selected. Due to these criteria, the Weibull model was selected and found to be appropriate for this study (Additional file 1).
The Cox-Snell residuals (together with their Nelson-Aalen cumulative hazard function) were done to check the goodness of fit for all models. The figure shows that the plot of the Nelson Aalen cumulative hazard function with Cox-Snell follows the 45° line closely. Hence, the output shows Cox–Snell residuals of the Weibull model were satisfied the overall model fitness compared with other models. Among all models, the Weibull model was appropriately fitted data compared with others (Fig. 4).
Predictors of mortality among adult patients on ART
After fitting a bi-variable hazard regression model, most predictor variables, i.e., age, sex educational level, occupation, hemoglobin level, viral load, TB co-infection, WHO stage, functional status, adherence, disclosure status OI other than TB and BMI were found to have p-value < 0.2 and entered into multivariable analysis and variables such as sex, hemoglobin level, viral load, WHO clinical stage, and TB co-infection were found to be significant predictors of mortality at 5% level of significance.
In our study, the effect of other variables was constant, the hazard of death among males was 2.4 (HR = 2.4; 95% CI (1.24, 4.62)) times higher than females. Patients with low hemoglobin patients were 4.14 (HR = 4.14; 95% CI (2.18–7.86)) times higher risk of death than those with normal hemoglobin. The hazard of death among patients who had a high viral load was 6.7 ((HR = 6.70; 95% CI (3.40–13.22)) times higher than that of low viral load. Patients at baseline on ART advanced CLINICAL stage IV had 5.64 (HR = 5.64, 95% CI (2.53–12.56)) times increased risk of mortality compared to those presenting with WHO clinical Stage I at the initiation of ART (Table 4).
Discussion
This study aimed to assess the incidence and predictors of mortality among adult HIV patients on ART at Metema Hospital, Northwest Ethiopia. Many other studies presented different predictors for mortality, and our study also assessed the magnitude of mortality and corresponding socio-demographic, clinical, and treatment-related factors. In this study, the overall incidence rate of mortality among adult HIV/ADIS patients who are on ART was 6.7 (95% CI (5.4–8.4)) per 100-person year of observation, consistent with other studies conducted in different areas of Ethiopia [20, 27]. This might be due to the implementation of ART services based on the ART guideline. However, the current finding of this study is higher than in other studies of Ethiopia [18, 19, 22, 23, 25, 26]. This difference might be due to our study was conducted in large number of migrant workers and daily laborers since daily laborers pass their time in the whole day in the work place and they do not have enough time to come health facility for medication and follow up. Because of the nature work, they are also more mobile and have no constant workplace that may end up with loss to follow up and poor treatment adherence which promotes death. Also, this group of population had low income (unable to feed themselves) and they believe that taking ART medication on an empty stomach is difficult and dangerous that leads them to seek an alternative options like holy water by stopping ART which facilitates death. However, the current finding is lower than the findings in Cameroon [32] and Uganda [33]. This might be due to a variation in the ART enrollment period with different treatment eligibility criteria and there was a variation in the implementation of new WHO treatment initiation recommendations in Sub-Saharan countries [34].
In this study, the hazards of death among male patients were 2.4 times higher than females in line with other studies [13, 35, 36], systematic review and meta-analysis conducted in low and middle-income country [14] and south Africa [37]. Since females have a better opportunity to practice the early diagnosis of HIV/AIDS, such as at a time of pregnancy, females were screened for HIV tests as a part of the PMTCT program. Besides this, a higher risk of mortality in males might be due to behavioral factors of males like substance use, potentially leading to late HIV diagnosis and poor adherence to ART. Also, another study assessing mortality rate among HIV positive patients in Uganda indicated that male patients 37% more risk of mortality compared to female patients at the starting of ART [13].
In this study, those ART clients with higher viral load had an increased hazard of death in agreement with the study conducted in seven teaching Hospitals of Ethiopia [27]. This could be a lower rate of viral suppression and poor immunological recovery at baseline.
Similarly, patients who had advanced WHO clinical stages (stage III and IV) were a higher hazard of death than those in the WHO clinical stage I consistency with studies conducted in Sub-Saharan Africa [12, 38,39,40,41]. This reflects the advanced immunodeficiency increases the risk of mortality.
Patients who had low hemoglobin levels have an increased hazard of death than those who had normal hemoglobin levels. This finding is comparable with the studies conducted in Sub-Saharan Africa [8, 33, 42,43,44]. This might be the HIV is directly affecting the bone marrow and the high incidence of anemia might increase with the progression of HIV infection, which probably has contributed to the increasing the risk of mortality. Moreover, anemia among HIV patients can lead to impaired physical functioning, psychological distress, poor quality of life, accelerated disease progression, and shorter life expectancy [30].
Patients with TB-co infected with increased the hazard of death compared to clients not developing TB. This finding is consistent with studies conducted in rural Uganda [33] and in Ethiopia [21, 22]. This might be due to host responses to M. tuberculosis enhance HIV replication, accelerating the natural progression of HIV, and further depressing cellular immunity [45]. Decreased gut absorption of anti-tuberculosis drugs leads to impaired treatment outcomes including mortality. Furthermore, TB and HIV is double burden infection which leads to cause of mortality worldwide [46].
In this study, the hazard of death among patients with BMI ≤ 15.4 kg/m2 was 2.4 times higher than those with a BMI ≥ 18.5 kg/m2. This study is similar to studies conducted in Tanzania [8], Ethiopia [22], Cameroon [32], Uganda [33], and Malawi [38]. Patients with lower BMI are malnourished and unable to cope with the disease and had a high exposure to opportunistic infections that leads to death [47].
Limitation of study
The potential limitation of this study was because of the retrospective nature of the study which lacks completeness of patient records like substance use, provision of opportunistic infection, prophylaxis status, and hospitalization of patients. We could not ascertain that all recorders of mortality were AIDS-related, so all mortality was considered as HIV/ AIDS-related because of the lack of records on the cause of mortality.
Conclusion
In this study, the incidence of mortality was high. Patients on ART who have Advanced WHO patients (stage III and IV), viral load > 1000 copy /ml, hemoglobin ≤ 10 mg/dl, TB co-infection, BMI ≤ 15.4 kg/m2, and being male sex had a higher risk of mortality. Special attention should be given to male patients and high public interventions needed among HIV patients on ART to reduce the mortality rate. Nutritional support and close monitoring of patients in the early period of ART treatment initiation is very vital to improve patient survival.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIC:
-
Akaike Information Criteria
- AIDS:
-
Acquired Immune Deficiency Syndrome
- ART:
-
Antiretroviral Therapy
- BIC:
-
Bayesian Information Criteria
- MI:
-
Body mass index
- HAART:
-
Highly active antiretroviral therapy
- Hgb:
-
Hemoglobin
- OI:
-
Opportunistic infection
- PMTCT:
-
Prevention of Mother to Child Transmission
- PYO:
-
Person Year Observation
- UNAIDS:
-
United Nations Joint Program on HIV/AIDS
- WHO:
-
World Health Organization
References
Piot P, et al. Defeating AIDS—advancing global health. Lancet. 2015;386(9989):171–218.
Marrazzo JM, et al. HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society–USA Panel. JAMA. 2014;312(4):390–409.
HIV/AIDS, U.N.J.P., United Nations Joint Programme on HIV/AIDS (UNAIDS). . Unaids Data 2018, 2018. 20(18): p. 1–369.
Boutayeb A. The impact of HIV/AIDS on human development in African countries. BMC Public Health. 2009;9(S1):S3.
Granich R, et al. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden; 1990–2013. PLoS ONE. 2015;10(7):e0131353.
Verma S. Health, well-being and development of adolescents through awareness about HIV/AIDS. J Psychosoc Res. 2016;11(1):183.
Ojikutu BO, et al. Predictors of mortality in patients initiating antiretroviral therapy in Durban, South Africa. S Afr Med J. 2008;98(3):204–8.
Johannessen A, et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008;8(1):52.
Wajanga BM, et al. Inpatient mortality of HIV-infected adults in sub-Saharan Africa and possible interventions: a mixed methods review. BMC Health Serv Res. 2014;14(1):1–8.
Ababa, A., Report on the 2014 round antenatal care based Sentinel HIV Surveillance in Ethiopia. Ethiop Public Heal Instititute, 2015.
Ayele W, et al. Treatment outcomes and their determinants in HIV patients on anti-retroviral treatment program in selected health facilities of Kembata and Hadiya zones, Southern Nations, Nationalities and Peoples Region, Ethiopia. BMC Public Health. 2015;15(1):826.
Jerene D, et al. Predictors of early death in a cohort of Ethiopian patients treated with HAART. BMC Infect Dis. 2006;6(1):136.
Rubaihayo J, et al. Trends and predictors of mortality among HIV positive patients in the era of highly active antiretroviral therapy in Uganda. Infect Dis Rep. 2015;7(3):66–73.
Gupta A, et al. Early mortality in adults initiating antiretroviral therapy (ART) in low-and middle-income countries (LMIC): a systematic review and meta-analysis. PLoS ONE. 2011;6(12):e28691.
Biset Ayalew M. Mortality and its predictors among HIV infected patients taking antiretroviral treatment in Ethiopia: a systematic review. AIDS Res Treat. 2017;2017:5415298.
Susuman AS. HIV/AIDS in Ethiopia: health view. J Asian Afr Stud. 2017;52(3):302–13.
EHNRI F. HIV related estimates and projections for Ethiopia. Addis Ababa: FMoH; 2012. p. 6–14.
Tarekegne D, et al. Prevalence of human immunodeficiency virus infection in a cohort of tuberculosis patients at Metema Hospital, Northwest Ethiopia: a 3 years retrospective study. BMC Res Notes. 2016;9(1):1–6.
Hambisa MT, Ali A, Dessie Y. Determinants of mortality among HIV positives after initiating antiretroviral therapy in Western Ethiopia: a hospital-based retrospective cohort study. Int Sch Res Notices. 2013;20(13):491601.
Alemu AW, Sebastián MS. Determinants of survival in adult HIV patients on antiretroviral therapy in Oromiyaa, Ethiopia. Glob Health Action. 2010;3(1):5398.
Tachbele E, Ameni G. Survival and predictors of mortality among human immunodeficiency virus patients on anti-retroviral treatment at Jinka Hospital, South Omo, Ethiopia: a six years retrospective cohort study. Epidemiol Health. 2016;38:e2016049.
Damtew B, Mengistie B, Alemayehu T. Survival and determinants of mortality in adult HIV/Aids patients initiating antiretroviral therapy in Somali Region, Eastern Ethiopia. Pan Afr Med J. 2015;22(1):138.
Biadgilign S, Reda AA, Digaffe T. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: a retrospective cohort study. AIDS Res Ther. 2012;9(1):15.
Tadele A, Shumey A, Hiruy N. Survival and predictors of mortality among adult patients on highly active antiretroviral therapy at Debre-markos referral hospital, North West Ethiopia; a retrospective cohort study. J AIDS Clin Res. 2014;5:2.
Mengesha S, Belayihun B, Kumie A. Predictors of survival in HIV-infected patient after Initiation of HAART in Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Int Sch Res Notices. 2014;2014:250913.
Tadesse K, Haile F, Hiruy N. Predictors of mortality among patients enrolled on antiretroviral therapy in Aksum hospital, northern Ethiopia: a retrospective cohort study. PLoS ONE. 2014;9(1):e87392.
Fekade D, et al. Predictors of survival among adult Ethiopian patients in the national ART program at Seven University Teaching Hospitals: a prospective cohort study. Ethiop J Health Sci. 2017;27(1):63–71.
Gurmu, D.E., Predictors of mortality among human immunodeficiency virus infected patients' records in Gondar University hospital, Ethiopia. 2011, Citeseer.
Organization WH. Patient monitoring guidelines for HIV care and antiretroviral therapy (ART). 2006.
Melese H, et al. Anemia among adult HIV patients in Ethiopia: a hospital-based cross-sectional study. Hiv/aids. 2017;9:25.
Ministry of Health, E., National Comprehensive HIV Prevention, Care and Treatment Training for Health care Providers. 2017.
Sieleunou I, et al. Determinants of survival in AIDS patients on antiretroviral therapy in a rural centre in the Far-North Province, Cameroon. Trop Med Int Health. 2009;14(1):36–43.
Moore DM, et al. Determinants of early and late mortality among HIV-infected individuals receiving home-based antiretroviral therapy in rural Uganda. J Acquir Immune Defic Synd. 2011;58(3):289.
Organization, W.H., Progress report 2016: prevent HIV, test and treat all: WHO support for country impact. 2016, World Health Organization.
Setegn T, et al. Predictors of mortality among adult antiretroviral therapy users in southeastern Ethiopia: retrospective cohort study. AIDS Res Treat. 2015;2015:148769.
Gunda DW, et al. Prevalence and risk factors of mortality among adult HIV patients initiating ART in rural setting of HIV care and treatment services in north western Tanzania: a retrospective cohort study. J Sex Transm Dis. 2017;2017:7075601.
Naidoo K, et al. High mortality rates in men initiated on anti-retroviral treatment in KwaZulu-Natal, South Africa. PLoS ONE. 2017;12(9):e0184124.
Ferradini L, et al. Scaling up of highly active antiretroviral therapy in a rural district of Malawi: an effectiveness assessment. The lancet. 2006;367(9519):1335–42.
Lawn SD, et al. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22(15):1897.
Djomand G, et al. Virologic and immunologic outcomes and programmatic challenges of an antiretroviral treatment pilot project in Abidjan. Cote d’Ivoire Aids. 2003;17:S5–15.
Zachariah R, et al. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. AIDS. 2006;20(18):2355–60.
Etard J-F, et al. Mortality and causes of death in adults receiving highly active antiretroviral therapy in Senegal: a 7-year cohort study. AIDS. 2006;20(8):1181–9.
Stringer JS, et al. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: feasibility and early outcomes. JAMA. 2006;296(7):782–93.
Toure S, et al. Rapid scaling-up of antiretroviral therapy in 10,000 adults in Cote d’Ivoire: two-year outcomes and determinants. AIDS. 2008;22(7):873.
Falvo JV, et al. Arc of a vicious circle: pathways activated by Mycobacterium tuberculosis that target the HIV-1 long terminal repeat. Am J Respir Cell Mol Biol. 2011;45(6):1116–24.
Swaminathan S, Padmapriyadarsini C, Narendran G. HIV-associated tuberculosis: clinical update. Clin Infect Dis. 2010;50(10):1377–86.
Van der Sande MA, et al. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. JAIDS J Acquir Immune Defic Syndr. 2004;37(2):1288–94.
Acknowledgements
The researcher would like to thank the University of Gondar for ethical approval. We also like to extend our appreciation to data collectors and Metema hospital staff for their devoted cooperation.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
KL and DA and TY conceived of the study and were involved in the design of the study, coordination and reviewed the article, analysis, report writing, and preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate data
Ethical clearance was obtained from the Institutional Review Committee of the University of Gondar. A permission letter was also obtained from Metema Hospital. All information collected from patient cards were kept strictly confidential and the names of patients on ART were not included in the data collection tool.
Consent for publication
Not applicable.
Competing interests
No potential conflict of interests concerning the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
AIC and BIC value for model comparison of Cox and parametric model
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Workie, K.L., Birhan, T.Y. & Angaw, D.A. Predictors of mortality rate among adult HIV-positive patients on antiretroviral therapy in Metema Hospital, Northwest Ethiopia: a retrospective follow-up study. AIDS Res Ther 18, 27 (2021). https://doi.org/10.1186/s12981-021-00353-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-021-00353-z