Abstract
Background
Long acting and permanent contraceptive methods by far are the most effective, very safe and convenient methods than short acting contraceptive methods. But in less developed countries, use of long acting reversible contraceptive or permanent methods (LARCs/PMs) is very low. Therefore the aim of this study was to identify determinants of long acting contraceptive method utilization among HIV positive reproductive age women.
Methods
An institutional based case control study was conducted among random sample of 354 HIV positive reproductive age women (total of 97.8% response rate) at Anti-Retroviral Therapy clinics from February 20 to March 20, 2019. Case to control ratio was 1:2. A structured questionnaire and information recorded from ART card review were used to collect the data. Each variable was entered in Bivariate analysis with dependent variables and those variables with P-value of ≤ 0.25 were included in the Multivariate analysis. Significance was determined at the level of P-value < 0.05 with 95% CI of AOR.
Results
A total of 354 (33.3% cases and 66.7% controls) HIV positive reproductive age women were interviewed with response rate of 97.8%. The study revealed being in age group of 39 and above [AOR = 0.17, 95% CI (0.06, 0.48)], being divorced/separated and widowed [AOR = 0.05, 95% CI (0.003, 0.61)], having supportive opinion and strongly supportive opinion regarding family planning service availability in ART clinic [AOR = 5.01, 95% CI (1.79, 14.07)], [AOR = 7.81, 95% CI (2.54, 24.01)] and having no future fertility intention [AOR = 7.03, 95% CI (2.73, 18.06)] were statistically significant determinants for long acting contraceptive method utilization.
Conclusion
Woman in age group of 39 and above, having no future fertility intention and being divorced/separated and widowed was found to be determinants of long acting contraceptive method utilization among HIV positive reproductive age women. In addition our study support the WHO Strategic Considerations for Strengthening the Linkages between Family Planning and HIV/AIDS Policies, Programs, and Services.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
All individuals and couples have a basic human right to decide freely and responsibly the number, spacing and timing of their children [1, 2]. Fulfilling this right is an important intervention for improving maternal and child health, preventing HIV infections, and improving the overall well-being of entire families [3]. Long acting and permanent contraceptive methods (LAPMs) by far is the most effective (99% or greater), very safe and convenient methods than short acting methods. LAPMs provide 3 to 12 years and life time uninterrupted protection against unintended pregnancy [4, 5]. HIV/AIDS is the most important public health challenge globally, especially the largest burden in Sub-Saharan Africa (SSA) [6]. Dual protective which includes use of a reliable hormonal contraceptive method like LAPMs and a barrier method like using the male or female condom is encouraged to prevent further transmission of HIV [4]. According to the United Nations report, Ethiopia is stated as one of 22 priority countries for eliminating mother-to-child transmission of HIV [7].
Fertility is not affected by HIV infection, however behavioural change, existing subfertility, low body mass index, AIDS, and inter current illness may lower conception rates [8]. Women with HIV infection, like other women, may wish to plan pregnancy, limit their family, or avoid pregnancy [9]. In the least developed countries, use of long acting reversible contraceptive or permanent methods (LARCs/PMs) accounts for less than one-fifth (19%) of the contraceptive method mix [10]. According to different studies done in Ethiopia, LARCs/PMs utilization has been seen very low among HIV positive reproductive age women [11,12,13,14]. Hence the aim of this study was to identify the determinants of long acting contraceptive methods utilization among HIV positive reproductive age women attending care in ART clinics in all public health facilities of Arba Minch Town.
Method and materials
Study design and setting
An institutional based case control study was conducted in three public health facilities of Arba Minch town, Gamo zone, Southern Ethiopia from February 20 to March 20, 2019. Arba Minch town is the capital city of Gamo zone with 3 public health care facilities (one general hospital and two health centers) and 33 private clinics (18 level one clinics and 15 medium clinics). All 3 public health care facilities are giving ART clinic services for seropositive peoples in the town and surrounding areas.
Population
All HIV positive reproductive age group women (15–49 years) who had ART follow up in all public health facilities of Arba Minch town were source population and those women who fulfilled the inclusion criteria during the data collection period were study population.
All HIV positive reproductive age women who were using long acting contraceptive methods were considered as cases while all HIV positive reproductive age women who were not using contraceptive methods (non-user) were considered as controls.
All HIV positive reproductive age women who use short acting contraceptive methods and women who were severely ill during data collection period were excluded from the study.
Sample size determination and Sampling technique
The sample size was determined by using the double population proportion approach using Epi Info version 7.02 statistical software package with the assumption of 95% confidence level (Zα/2 = 1.96), 80% power. Case to control ratio of 1:2 and the sample size was calculated by taking different factors from two different studies done in Bahir Dar North West Ethiopia [11, 13].
The larger sample size which was 344 taken from previous study done in Bahir Dar City, Ethiopia was taken for this study [11]. After adding 5% for non-response rate, the total sample size was 362 (121 cases and 241 controls).
Cases and controls were selected from each health facilities that are giving ART clinic services for Arba Minch town and surrounding areas. The sample was proportionally allocated depending on their 3 month performance before data collection using the patient registry log book at ART clinics. Using systematic random sampling techniques the required sample size were drawn as follows. From Arba Minch General hospital 272 (91 cases and 181 Controls), from Sikela health center 86 samples (29 cases and 57 controls) and from Secha health center 3 samples (1 case and 2 controls) were included in the study.
Operational definitions and definition of terms
-
Long acting contraceptive methods: Modern contraceptive methods that prevent unintended pregnancy for more than 1 year which include Long Acting Reversible contraceptive Methods (LARMs) such as Intra Uterine Devices (IUDs) and sub dermal Implants and permanent contraceptive methods (Tubal ligation) [11].
-
Myths heard: When women had ever heard any rumor or misconceptions about LAPMs [13].
-
Past experience for LAPMs: It is when a women had ever used LAPMs before current used method [13].
-
Current use of contraceptive method: Referred to respondents who responded positively for use of at least one type of contraceptive methods at time of the survey to delay or avoid pregnancy [14].
Data collection tool, method and procedure
Data was collected using structured questionnaire to interview all eligible women and data extraction tool which was adapted from previous study and some adjustment were made for this study [15]. The questionnaire mainly addressed socio demographic variables of mothers (age, women’s educational status, husband educational status, marital status, wealth index and place of residence), Reproductive health variables (parity, gravidity, number of live children, discussion with husband, discussion with health care providers, family planning counseling, pregnancy intention, experience of contraceptive) and Risky sexual behaviour variables (sexual intercourse in the past 6 months, using condom, having multiple sexual partner). Data extraction tool was used for Medical history variables (clinical WHO staging, disclosure of HIV status, CD4 count, time of HIV diagnosed and HAART user). Five nurses and one public health officer participated as data collectors and supervisor, after training and orientation had given for 2 days. The principal investigator checked the completeness of the data each day.
Data quality control
Data collectors and the supervisor were trained for 2 days on data collection tool and the procedure by the principal investigator. Pre-test was done in Chencha hospital 1 week before the actual data collection, and few amendment were made after the pre-test. The required data were collected after obtaining ethical clearance from Arba Minch University Institutional Review Board (AMU/IRB). In addition permission from the three health institutions and consent from the patient was taken. The entire questionnaire was checked and reviewed for completeness and consistency every day by principal investigator before data entry.
Data analysis
After the data collection, data was coded and then entered, cleaned and edited by Epi Info version 7 and exported to Statistical package for Social Sciences (SPSS) software version 23. Wealth index of the participants was analyzed by principal component analysis method. On binary logistic regression analysis, a variable with P-value of ≤ 0.25 was used as a candidate for multiple logistic regression analysis. Multicollinearity was checked by using standard error greater than two. Multi variable logistic regression with backward method was done to find determinant factors. Odds ratio, 95% confidence interval and P-value < 0.05 were used to determine the significance and strength of association with dependant variable.
Ethical considerations
Ethical approval and clearance were obtained from an ethical review committee of Arba Minch University, College of Medicine and Health sciences. Further permission was obtained from all public health facilities. Confidentiality was maintained by making the data collectors aware not to record any identification information found.
Results
Socio demographic and economic characteristics of the participants
The total number of women visited the ART clinic during the study period was more than 800. Of which, 362 HIV positive reproductive age women were participated in the study. 354 HIV positive reproductive age women were included in the final analysis with a response rate of 97.8% in the study and 8 women excluded due to non-response or incomplete data. Among those 118 (33.3%) cases and 236 (66.7%) controls were responded to the interview respectively. 83 (70.3%) cases and 139 (58.9%) controls were in the age category of 29-38 years. Orthodox was the predominant religion for cases 67 (56.8%) and controls 136 (57.6%). Of the total 91 (77.1%) cases and 104 (44.1%) controls were married. Concerning their educational status 16 (13.6%) cases and 28 (11.9%) controls were attended above secondary level and regarding their husbands educational status 19 (17.6%) cases and 23 (18.7%) controls attend above secondary level. Regarding the Economic status of the respondents, around one fifth of cases and controls were in the lowest wealth quantile (Table 1).
Reproductive health related characteristics among HIV positive reproductive age women
Among the total cases, the majority of the respondents were using implanon 98 (83.1%) followed by intrauterine device 14 (11.9%) and Tuba-ligation 6 (5.1%). Of the total cases 71 (61.2%) women were utilizing dual contraceptive methods. Two third of the cases (67.5%) were using the current long acting contraceptive for 1 to 3 years. Among the respondents, 74 (62.7%) of cases and 115 (48.7%) of controls get pregnant after becoming HIV positive and for both groups more than 90% women become pregnant only 1–2 times (Table 2).
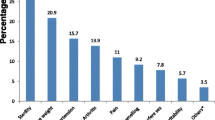
Of the total participants 84 (71.2%) cases and 143 (60.6%) controls report that they do not have future fertility intention (Fig. 1).
Medical history related and risky sexual behaviour characteristics among HIV positive reproductive age women
This study indicate that nearly two third of the cases (68.6%) and 134 (56.8%) controls diagnosed HIV with in the last 5 years. Regarding the ART initiation, 76 (64.4%) cases and 128 (54.2%) controls start ART drug with in the last 5 years. Nearly 72 (65%) cases and 141 (66.5%) controls have CD4 count greater than 500 mm/cells and 97.5% of cases and 96.2% of controls were in WHO stage one.
Out of the total respondents 107 (90.7%) cases and 198 (83.9%) controls had information about mother to child transmission of HIV. More than half of the respondents (60.7% cases and 60.1% controls) report health care providers in ART clinic were the main source of information followed by mass media (13.1% cases and 9.1% controls). Only 30 (28.0%) of cases and 54 (27.3%) of controls have information that HIV can transmit during pregnancy, delivery and breast feeding (Table 3).
Determinant factors of long acting contraceptive utilization among HIV positive reproductive age women
In the final model of this study, the determinant factors which were statistically significant with long acting contraceptive utilization among HIV positive reproductive age women attending care at ART clinics in all public health facilities of Arba Minch town were age, Marital status, future fertility intention and opinion about family planning service availability in ART clinic.
Being in 39 and above age group were found to be associated with long acting contraceptive method utilization with the odds of 90% less likely to use long acting contraceptive than those who were in age group of 19–28 years old women [AOR = 0.10, 95% CI (0.02, 0.54)].
Marital status of being divorced/separated and widowed as compared to married women were associated with long acting contraceptive utilization with the odds of 95% [AOR = 0.05, 95% CI (0.003, 0.61)] (Table 4).
Discussion
This study finding revealed that women aged 39 years old and above, divorced/separated and widowed women, women who support and strongly support availability of family planning method in ART clinic and women who have no future fertility intention were associated with long acting contraceptive utilization.
Women aged 39 years old and above were 90% less likely to use long acting contraceptive methods. This finding is consistent with a study conducted at University of Gonder hospital and Mizan Tepi teaching and referral hospital which indicated that reproductive age women who were 35 years old and above were 83% and 70% less likely to use modern contraceptive methods [14, 16]. This could be explained as majority of women (60.4%) who were 39 and above years of age in this study were divorced/separated and widowed. In addition women 39 and above years of age did not use long acting contraceptive methods due to expectation of the natural cessation of menses and due to fear of side effects and misconceptions. Commonly reported Misconceptions and fear of side effects mentioned in another study done in Southern Ethiopia included headache, disturbance of menstruations, weight gain, nausea, loss of appetite, infertility and other medical problems like hypertension, anemia, cancer, kidney stone and other disease after long use [17].
According to this study women who were divorced/separated and widowed were associated with long acting contraceptive utilization compared to single women with the odds of 95%. This result is supported by a study conducted in Mizan Tepi, Southern Ethiopia indicate women who were divorced, separated or widowed were 79% less likely to use modern contraceptive than women who were married [14]. The result is also consistent with studies conducted at university of Gonder hospital and Addis Ababa, [16, 18]. This may be due to above half of them were in age group of 39 and above years of age and they may not need long acting contraceptive methods to prevent unwanted pregnancy. In addition majority of women in this group had neutral opinion on the availability of family planning service in ART clinic.
As this study indicated women who had no future fertility intention were seven times more likely to use long acting contraceptive than those women who had fertility intention. This finding is supported by study conducted in Bahir Dar, Ethiopia, on demand of long acting contraceptive among married HIV positive women, it showed women who had no fertility intention were 7.7 times more likely to had intension to use long acting contraceptive [11] similarly studies conducted in Arba Minch Zuriya District, in Bahir Dar town and indicate the same [19, 20]. This may be due to women who had no fertility intention prefer long acting contraceptive methods which is the more effective contraceptive methods.
This study also found women who have supportive and strongly supportive opinion on the availability of family planning service in ART clinic were five times and eight times more likely to use long acting contraceptive than those who have neutral opinion. A longitudinal cohort study done in Malawi [21] on integrating family planning service into HIV care also demonstrate the rapid increase in contraceptive use during implementation of enhanced Family Planning-Electronic Medical Record (FP EMR) module, possibly due to increased counselling and FP-related communications with the women [2].
The above result strongly support the WHO’s Strategic Considerations for Strengthening the Linkages between Family Planning and HIV/AIDS Policies, Programs, and Services. The strategy indicate integration of family planning at HIV service delivery points providing a valuable opportunity to comprehensively address the risk of HIV infection, prevent unintended pregnancy and promote healthy birth spacing and birth outcomes [2].
Limitation of study
The limitation of the study was that the study relied on participants’ self-reported data, which was prone to social desirability bias. However, close monitoring by supervisor and PI was made to minimize such biases and clarification of potential ambiguities and misunderstandings, maintaining privacy of participants during interview carried out by interviewers. In addition, data lack adequate published litratures on same study design to compare detrminant variables more.
Conclusion
Family planning (FP) is one aspect of RH where linkages with HIV programs are especially important. Integrating FP services into HIV prevention, treatment, and care services provides an opportunity to increase access to contraception among clients of HIV services who do not want to become pregnant, or to ensure a safe and healthy pregnancy and birth for those who wish to have a child [2].
This study identified having supportive and strongly supportive opinion on availability of family planning service in ART clinic and had no future fertility intention were positively associated with long acting contraceptive utilization while being in age group of 39 and above years old and being divorced/separated and widowed were negatively associated with long acting contraceptive utilization among HIV positive reproductive age women.
Availability of data and materials
The data used in this study was collected by trained data collectors and the lead author are willing to share the data upon request from peer researchers.
Abbreviations
- AOR:
-
Adjusted odds ratio
- AIDS:
-
Acquired immunodeficiency syndrome
- ART:
-
Ant retro viral therapy
- FP:
-
Family planning
- HAART:
-
Highly active antiretroviral therapy
- HIV:
-
Human immune deficiency virus
- IUDs:
-
Intra uterine devices
- LAPMs:
-
Long acting and permanent contraceptive methods
- LARMs:
-
Long acting reversible contraceptive methods
- PM:
-
Permanent methods
- PMTCT:
-
Prevention of mother to child transmission
- RH:
-
Reproductive health
- SSA:
-
Sub-Saharan Africa
References
Republic FD. National guideline for family planning Federal Democratic Republic of Ethiopia. Nepal: Republic FD; 2011. p. 1–69.
World Health Organization, USAID, Family Health International. Strategic considerations for strengthening the linkages between family planning and HIV/AIDS policies, programs, and services. World Health Organization; 2009.
Kulczycki A. Overcoming family planning challenges in Africa: toward meeting unmet need and scaling up service delivery. Afr J Reprod Health. 2018;22(1):9. https://doi.org/10.29063/ajrh2018/v22i1.1.
Siraha P. The reasons for low utilization of long acting contraceptives amongest HIV positive women at harare post test support services clinic. Zimbabue: Stellenbosch Univ; 2013.
USAID. Addressing unmet need for family planning in Africa. Washington: USAID; 2007.
UNAIDS fact sheet. Report on the global AIDS epidemic, global statistics. 2014.
Progress report on the global plan towards the elimination of new HIV infections among children and keeping their mothers alive. Progress report on the global plan. UNAIDS; 2015.
Mitchell HS, Stephens E. Contraception choice for HIV positive women. Sex Transm Infect. 2004;80:167–73.
Mitchell HS, Stephens E. Contraception choice for HIV positive women. Sex Transm Infect. 2004;80(167–173):167–73.
Hubacher D, Kimani J, Solomon MJ, Ndugga MB. Contraceptive implants in Kenya: current status and future prospects. Contraception. 2007;75(6):468–73.
Gelagay AA, Koye DN, Yeshita HY. Demand for long acting contraceptive methods among married HIV positive women attending care at public health facilities at Bahir Dar City, Northwest Ethiopia. J List Heal. 2015;12:76.
Alene KA, Atalell KA. Contraceptive use and method preference among HIV-positive women in Amhara region, Ethiopia. BMC Womens Health. 2018;18:97.
Gelagay AA, Negese D, Yeshita HY. Factors affecting long acting and permanent contraceptive methods utilization among HIV positive married women attending care at ART clinics in Northwest Ethiopia. Public Health. 2018;76:47.
Mitiku K, Mulugeta S, Lemessa B. Modern contraceptive utilization and associated factors among HIV positive women on antiretroviral therapy in Mizan-Tepi Teaching and Referral Hospital, South-West Ethiopia. J Reprod Health Contracept. 2017;2(2):1–9.
Kebede H, Nahusenay H, Birhane Y, Tesfaye D. Assessment of contraceptive use and associated factors among HIV positive women in Bahir-Dar Town, Northwest Ethiopia. Open Access Libr J. 2015;2:1–19. https://doi.org/10.4236/oalib.1101942.
Worke MD, Bezabih LM, Woldetasdik MA. Utilization of contraception among sexually active HIV positive women attending art clinic in University of Gondar Hospital: a hospital based cross-sectional study. BMC Womens Health. 2016;16(67):1–9.
Endriyas M, Eshete A, Mekonnen E, Misganaw T, Shiferaw M. Where we should focus ? Myths and misconceptions of long acting contraceptives in Southern Nations, Nationalities and People’ s Region, Ethiopia : qualitative study. BMC Pregnancy Childbirth. 2018;18:98.
Adilo TM. Prevalence and determinants of contraceptive utilization among reproductive age women living with HIV/AIDS in Addis Ababa, Ethiopia; a cross sectional study design. EC Gynaecol. 2017;4(3):97–112.
Gultie T, Hailu D, Workineh Y. Predictors of long acting contraceptives utilization among reproductive age women in Arba Minch Zuria district, Ethiopia. Qual Prim Care. 2016;24(1):17–22.
Yemaneh Y, Birie B. Assessment of knowledge, attitude and utilization of long acting family planning method among women of reproductive age Groupe in Mizan-Aman Twon, Bench- Majizone, South West Ethiopia, 2016. iMedPub J. 2017;1(2):11.
Hannock T, Caryl F, Lisa BH, Chimango M, Mwantha B, Colin S. Integrating family planning service into HIV care: use of a point-of-care electronic medical record system in Lilongwe, Malawi. Glob Health Action. 2017;10(1):1383724.
Acknowledgements
We would like to thank Arba Minch University College of Medicine and Health Science for funding this research. Our gratitude goes to supervisors, data collectors and study respondents. Finally, we would like to thank all those, who in one way or another have contribute in this work.
Funding
This work was funded by Arba Minch University (Grant For Masters Program).
Author information
Authors and Affiliations
Contributions
Authors will take public responsibility for the contents, have contributed substantially to the drafting, and have approved the final version. BY (MPH/RH): This author made substantial intellectual contributions to conception, design, and acquisition of data, analysis, and interpretation of data as well as on preparing the manuscript to this study. FG (MPH/RH, Assistant professor): have made substantial contributions to conception, design, analysis and interpretation of data and participated in the critical review and editing of the manuscript drafts for scientific merit and depth. GG (MPH/Biostatic & epidemiology, Assistant professor): have made substantial contributions on the analysis and interpretation of data and participated in the critical review and editing of the manuscript drafts for scientific merit and depth. TS (MPH, M.Sc.): has been involved in analysis, interpretation of data and drafting the manuscript and revising it critically for important intellectual contents. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The required data were collected after obtaining ethical clearance from Arba Minch University Institutional Review Board (AMU/IRB). In addition permission from the three health institutions and verbal consent from each patient was taken.
Consent for publication
The Author declares that any person named as co-author of the contribution is aware of the fact and has agreed to being so named. The Authors guarantees that the Work has not been previously published elsewhere. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yirsaw, B., Gebremeskel, F., Gebremichael, G. et al. Determinants of long acting contraceptive utilization among HIV positive reproductive age women attending care at ART clinics of public health facilities in Arba Minch town, Southern Ethiopia, 2019: a case control study. AIDS Res Ther 17, 34 (2020). https://doi.org/10.1186/s12981-020-00288-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-020-00288-x