Abstract
Background
The risk of death from complications relating to pregnancy and childbirth over the course of a woman’s lifetime is higher in the developing countries. Improving the health of mothers and children through well-organized institutional delivery service is central to achieve reduced maternal and child morbidity and mortality. So, factors that underlie the level of institutional delivery service utilization need to be investigated, especially in areas where little is known about the problem. Therefore, the objective of this study was to assess factors influencing institutional delivery service utilization in Dembecha district, Northwest Ethiopia.
Methods
Community based quantitative cross-sectional study was conducted from March 1 to 30, 2015 among 674 mothers who gave birth within the last two years preceding the study using interviewer administered questionnaire. Multi-stage sampling with stratification sampling technique was used. Descriptive statistics were done to characterize the study population using different variables. Bivariate and multivariable logistic regression models were fitted to determine association. Odds ratios with 95% confidence intervals were computed. Statistical significance was declared at p-value <0.05.
Results
Of all 674 respondents, 229(34%, 95% CI: 29.8%–37.9%) of them utilized health institutions for their last delivery. History of still birth (AOR (adjusted odds ratio) =0.25, 95% CI (confidence interval) =0.07–0.77), number of ANC visit (AOR = 38.51, 95% CI = 22.35–66.33), functional media (AOR = 2.61, 95% CI = 1.59–4.28) and distance to nearby health facility (AOR = 0.52, 95% CI = 0.32–0.83) were found to be significantly associated with institutional delivery service utilization.
Conclusion
In this research the level of institutional delivery service utilization is still low compared to government initiatives. History of still birth, low number of ANC visit, unavailability of functional media and existence of distant health facilities were found to be significantly associated with low utilization of the service. So, concerned bodies should contribute their share to improve institutional delivery service utilization in the study area by tackling modifiable risk factors.
Similar content being viewed by others
Plain English summary
Institutional delivery service utilization is one of the most important interventions to reduce maternal death. In this study the factors that underlie institutional delivery service utilization was investigated.
To achieve the objective, community based quantitative cross-sectional study was conducted among systematically selected mothers using interviewer administered questionnaire. Descriptive and analytical statistics were applied for the analysis.
One third of study participates were utilized health institutions for their last delivery which is still low compared to government initiatives. Institutional delivery service utilization was determined by history of still birth, number of ANC visit, functional media and distance to nearby health facility. So, concerned bodies should contribute their share to improve institutional delivery service utilization in the study area and tackle modifiable risk factors that affect utilization of the service.
Background
More than 20 million women worldwide become pregnant annually, 15% of whom are likely to develop complications [1]. The risk of death from complications relating to pregnancy and childbirth over the course of a woman’s lifetime is higher in the developing compared to the developed world which is one in 76, and one in 8000 respectively [2, 3]. Almost all annual deaths from pregnancy related complications are occurring in Asia and Africa, leading the world in pregnancy related complications [3,4,5]. Most Sub- Saharan African (SSA) countries are not also on track for meeting the targets pertaining to maternal mortality, as recent estimates suggest that the average annual rate of reduction in maternal mortality rate (MMR) in SSA countries is less than 1% [5, 6].
Institutional delivery service utilization is one of the most important interventions to reduce maternal death and the proportion of women who delivered with the assistance of a skilled birth attendant is one of the indicators in every country health plans [7,8,9,10]. Maternal death is highest among countries which have less skilled professionals such as trained midwife, Nurse, doctor or other trained health professionals [2]. In almost all countries where health professionals attend more than 80% of deliveries, MMR is below 200 per 100,000 live births [5]. A woman who is going to give birth at a health facility can get sufficient medical care during child birth which in turn can highly prevent maternal and neonatal deaths [10]. However, rate of delivery attended by skilled birth attendants at health facilities is still very low in many developing countries and is lowest in sub-Saharan Africa (average facility delivery in 2008 was only 47%) [11,12,13].
Being one of the developing countries, pregnancy related complications are among the many health challenges of Ethiopia. The MMR in the country was 676 per 100,000 live births in 2011 which was not significantly different from the 2005 EDHS report (673 per 100,000 live births) [14, 15]. Major causes of maternal deaths in Ethiopia are preventable that include hemorrhage (APH and PPH), prolonged/obstructed labor and ruptured uterus, severe pre-eclampsia and eclampsia, sepsis, and complications of abortion which account for 69% of the deaths [16]. This high maternal death are due mainly to the fact that over 90% of births take place at home, and women with complications may not be arriving at a health facility in time (Federal ministry of health (FMOH): National Baseline Assessment for Emergency Obstetric and Newborn Care in Ethiopia, unpublished). Even though the country is aggressively constructing and equipping health facilities with staff and equipment’s, and strategies like user-fee exemption for delivery and associated cares have been in place to enhance access, still the use of health facilities for maternal health services is very low. According to 2011 EDHS, skilled delivery attendance in Ethiopia was only 10% of the total deliveries [14]. For the observed low coverage different barriers are incriminated that are varying in different contexts [17,18,19,20,21,22,23,24,25]. Literatures from different corners of the country are also show discrepancies in findings indicates the importance of site specific studies on it especially in areas where access to health information is limited. Though there are literatures in Ethiopia on level and factors associated with institutional delivery, little is known about the issue in the study area. Investigating the issue provides an opportunity for different stakeholders and health workers to tackle factors that could possibly influence institutional delivery service utilization. Therefore, the objective of this study was to assess factors influencing institutional delivery service utilization among mothers who gave birth within the last two years in Dembecha district, Northwest Ethiopia from March 1 to 30, 2015.
Methods
Study design and period
A community based cross-sectional study was carried out from March 1 to March 30, 2015 among 700 randomly selected pregnant women who lived in the selected Kebeles of the district for more than six months.
Study area
The study was conducted in Dembecha district, West Gojam zone, Amhara region located at the north western part of Ethiopia, about 350 km from Addis Ababa and 220 km from Bahir Dar. The district has four urban 25 rural Kebeles (lowest administration unit in Ethiopia). Within the district there are six health centers and 25 health posts. According to Dembecha district health office report, 2015 population projection estimate, Dembecha district has total population of 129,977 of which 66,475 are female and 31,720 of the total female population are in a reproductive age group (15–49 years). The total number of women deliver per year was expected to be 7376 with general fertility rate of 232.5/1000 [26].
Sample size and sampling procedure
The sample size was calculated using a single population proportion formula with the following assumptions: P = Expected proportion of the population (proportion of institutional delivery service utilization is 15.7%) [22], d = Desired precision/the margin of error (4%), a design effect of two (as stratified multistage sampling was used) and 10 % non-response rate. Accordingly the required, sample size was 700. Since this research considers institutional delivery as deliveries attended either at hospitals, health centers or health posts, there is heterogeneity in service delivery across urban and rural Kebeles. Therefore, this study utilized multi stage sampling with stratification sampling technique to select the study participants. The district was classified into urban and rural strata. Kebeles (one urban and six rural) and study participants (700 women) from each stratum were selected using lottery and systematic sampling methods respectively. Sampling frame (list of all women that gives birth within last two years from each selected Kebeles) was obtained from Health extension workers (HEWs) in the selected Kebeles since they record all mothers in their location regularly to prepare them for maternal health care services.
Data collection tool and procedure
Data collection questionnaire was adapted from tools used to assess institutional delivery service utilization used by different studies that could satisfy the objectives of the study and variables under study [6, 14, 17, 19, 20, 22,23,24,25]. Semi-structured questionnaire was used and it was translated in to Amharic language (local language) then back to English language to check consistency. The data was collected by eight clinical nurses who were not working in a health facility where the selected kebele is under its catchment)and supervised by two BSc nurses. The data collectors and supervisors were trained for one day on how to interview and how to fill the questionnaire based on a prepared instruction. The tool was pretested seven days before the actual data collection on 5% of the total sample at non-selected Kebele of the study district among women who gave birth within the last two years.
Data quality assurance
To increase the quality of data; translated and pretested questionnaire was used, data collectors were trained and close supervision was made during the data collection. The collected data were also cross checked on each day of activity for consistency and completeness. Double entry of data and cleaning of data using frequency, sorting and listing to identify any missed value and outlier was made and identified errors was cross checked with the original questionnaire.
Data processing and analysis
The collected data were double entered using EPI Data software version 3.0. Then it was exported to SPSS version 16.0 for data processing and analysis. The outcome variable, delivery service utilization was dictated as “YES = 1” if a mother gave birth only in hospital, health center or health post for her recent delivery and NO = 0 (women who delivered at home). Descriptive statistics like proportions mean and standard deviations and analytic tests like bivariate and multivariable logistic regression analysis were computed. Odds ratio along with the 95% CI was estimated to ascertain the association between covariates and institutional delivery service utilization. Covariates that have P-value of <0.2 at the bivariate analysis were included in the multivariable logistic regression to control all possible confounding factors. For all statistical tests P-value <0.05 was used as a cut-off point for statistical significance.
Ethical consideration
Ethical clearance was obtained from research committee of Debre Markos University, College of medicine and health sciences. The heads of the district health office were informed about the purpose of the study and permission was obtained. Informed consent was also obtained from study participants. All information obtained from the study participants was kept confidential and at the end of the interview mothers with deliveries other than health institutions were advised to use health facilities for obstetric care services for the next planned pregnancy.
Results
Socio-demographic characteristics of respondents
A total of 674 out of 700 women who gave birth within the last two years were interviewed with a response rate of 96.3%. The 26 non-responders were due to migration (one), absent after three time’s visit (nine) and refusal to participate (sixteen). The mean age of the study participants was 31.93 ± 6.2. Of the total respondents, majority of them were rural residents, 577(85.6%), Orthodox in their religion 659(97.8%), married, 641 (95.1%) and house wives, 525(77.9%). Most of respondent’ husbands’ were farmers 497 (77.5%). Regarding to educational status, majority of women and their husband were able to read and write but without formal education, 280 (41.5%) and 272 (42.4%) respectively (Table 1).
Obstetric characteristics of respondents
Majority of study participant’s age at first marriage 334 (49.6%) and age at first pregnancy 381 (56.5%) was 15–19 years. Most 421 (62.5%) and 445 (66%) had two to four history of gravidity and parity respectively but 87 (12.4%) and 53 (7.6%) had a history of abortion and still birth in their life time. 511 (75.8%) of the deliveries were planned pregnancies. Out of the total pregnancies, 311 (46.1%) of them had ANC visits. Among pregnancies which had ANC visits, 179 (56.8%) had two to three ANC visits (Table 2).
Accessibility characteristics of respondents
Most of respondents has health facility within one to two hour distance, 374 (55.5%) and have available functional media, 433 (64.2%) (Table 3).
Level of institutional delivery utilization
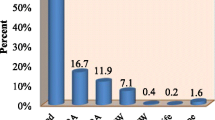
Out of 674 interviewed mothers who gave birth within the last two years, 229 (34%; 95% CI: 29.8%–37.9%) of them utilized health institutions for their last delivery and the rest, 445 (66%) were delivered at home. Among mothers who utilized health institutions for their last delivery, their most visited place of delivery was health center 171 (74.7%) (Fig. 1).
Factors associated with institutional delivery service utilization
The results of bivariate and multivariable analysis between institutional delivery service utilization and selected independent factors are presented in Table 4. Accordingly, in the bivariate analysis; educational status of women, marital status, family size, gravidity, abortion history, still birth history, planned pregnancy, ANC visit, presence of functional media and distance from nearby health facility were the main significant factors associated with institutional delivery service utilization (Table 4).
In the final model (multivariable analysis); variables with P-value of >0.2, and parity and family size that show multicollinarity with gravidity were not included. Whereas other variables like: place of residence, age, educational status of a mother, marital status, family size, gravidity, abortion history, still birth history, planned pregnancy, ANC visit, presence of functional media and distance from nearby health facility were found to have P-value <0.2 in which this variables were taken to multivariable analysis. Accordingly; the results of the final multiple variable logistic regression model revealed history of still birth, number of ANC visit, functional media and distance to nearby health facility were found to be significantly associated with institutional delivery service utilization in multivariable analysis with P-value <0.05 (Table 4).
Discussion
In this study the level of institutional service utilization was 34%. This finding is lower than the findings from India 95.2% and 84.9% [27, 28]; Tanzania 74.5% [29]; Ghana 37.5% [30] and Bahir Dar, Ethiopia 78.8% [17] and Woldeia, Ethiopia 48.3% [23]. But higher than findings from Munisa Woreda, South East Ethiopia 12.3% [18]; Sekela District, North West of Ethiopia, 12.1% [19]; Dodota district, Oromia region, Ethiopia 18.2% [20]; Rural Jimma Horro District, Southwest Ethiopia 8% [21]; Banja District, Awi Zone, Amhara Region, Ethiopia 15.7% [22] and mini-EDHS 2014 report, 12% in Amhara Region and 16% in Ethiopia [15]. The possible explanations for the observed differences might be related with differences in study place, year of study, sample size and study design. Another possible explanation could be introduction of the new “mother waiting center approach” in the study area that create opportunity for mothers to deliver at health institution.
In this study; the association of respondent’s and their partner’s socio-demographic variables, obstetric variables and accessibility variables with institutional delivery service utilization was assessed. Those mothers having history of ANC visit were 38 times more likely (AOR = 38.51, 95% CI = 22.35–66.33) to utilize health institutions for delivery compared to those who had no history of ANC visit. This finding was supported by findings from Tanzania [29], Ghana [30], Nigeria [31] and Ethiopia [17,18,19]. This might be due to the fact that among ANC services, birth preparedness plan is a major task at ANC4 and majority of mothers might get convinced to deliver at health institutions.
On the other hand, those mothers having a history of still birth in life time were 75% less likely (AOR =0.25, 95% CI = 0.07–0.77) to utilize health institutions for delivery compared to those who had no a history of still birth. The possible explanations for this finding could be some of the mothers with a history of still birth may be a habit of delivering at home, and may develop attitude of ignorance hence be ambivalence in delivering at health institutions.
Those mothers who were living in a place where 1–2 h distance away from nearby Health institution were 48% more likely (AOR = 0.52, 95% CI = 0.32–0.83) to utilize health institutions for delivery compared to those who were living in a place where less than 1 h distance away from nearby Health institution. This finding was also supported by other findings from Ethiopia [19, 21, 24]. This is because mothers who were living near health institutions may have access to health education, ANC service and transport.
Mothers who had functional media were two and half more likely (AOR = 2.61, 95% CI = 1.59–4.28) to utilize health institutions for delivery compared to those who had no functional media. The possible explanation for this finding is mothers who had access to media may have a chance to get informed about institutional delivery service and consequences of home delivery.
Limitations of the study
Data was collected from mothers about their experience since 2 years that might lead to a recall bias and cross sectional nature of the study could not allow cause effect relationship.
Conclusions
In this research the level of institutional delivery service utilization is one in every three women which is still low compared to government initiatives which is increasing to 60% the proportion of births attended by skilled health personnel either at home or in a facility. Still birth history, ANC visit, availability of functional media and distance from health facility were found to be significantly associated with institutional delivery service utilization. Based on the findings the following recommendations are forwarded:
-
Focused ANC and mother waiting centers for delivery service need to be strengthened.
-
Transportation and Ambulance services need to be available and accessible so that mothers can access the health facilities in a short period of time.
-
Awareness creation needs to be done about birth preparedness plan for pregnant mothers during their ANC visit.
-
Health professionals working in the district should follow “mother friendly approach” in providing maternal health services and need to create opportunities mothers to share experiences about using health institutions for delivery service
References
International online resource centre. [Available from: http://www.asksource.info/resources/search/subjects-resources/mother-child-health]. Accessed 29 Apr 2015.
United Nations Children’s Fund (UNICEF). Progress for Children: A Report Card on Maternal Mortality. New York; 2008. Report No.: 7.
WHO, UNICEF, UNFPA and The World Bank. Trends in maternal mortality: 1990 to 2010. Geneva: World Health Organization; 2010. p. 3. [Available on: http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/].
The World Bank. Over 99 percent of maternal deaths occur in developing countries. 2012 [Available from: http://blogs.worldbank.org/opendata/over-99-percent-maternal-deaths-occur-developing-countries]. Accessed 23 Apr 2015.
World Health Organization (WHO). Maternal mortality. [Available from: http://www.who.int/mediacentre/factsheets/fs348/en/].
Envuladu EA, Agbo HA, Lassa S, Kigbu JH, Zoakah AI. Factors determining the choice of a place of delivery among pregnant women in Russia village of Jos North, Nigeria: achieving the MDGs 4 and 5. Int J Med Biomed Res. 2013;2(1):23–7.
Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. The Lancet. 2006;367(9516):1066–74.
Group SMI-A. The safe motherhood action agenda: priorities for the next decade, Report on the safe motherhood technical consultation 18–23 October 1997. Colombo: Sri Lanka; 1997.
Khan M, Pillay T, Moodley JM, Connolly CA. Maternal mortality associated with tuberculosis-HIV-1 co-infection in Durban. South Afr AIDS. 2001;1863:15.
World Health Organization (WHO). Making pregnancy safer (MPS): a strategy for action. Safe Motherhood Newsletter. 2002.
Wagstaff A, Claeson M. The millennium development goals for health rising to the challenges. Washington DC: The World Bank; 2004.
Lozano R, Wang H, Foreman KJ, Rajaratnam JK, Naghavi M, Marcus JR, Dwyer-Lindgren L, Lofgren KT, Phillips D, Atkinson C, Lopez AD. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. The Lancet. 2011;378(9797):1139–65.
MEASURE DHS. Measure DHS Statcompiler. ORC Macro: Calverton; 2008.
Central Statistical Agency (CSA). Ethiopia Demographic and Health Survey 2011. Addis Ababa and Calverton: 2012.
Central Statistical Agency (CSA). Ethiopian Mini Demographic and Health Survey 2014. Addis Ababa and Calverton: 2014.
Ahmed A. Maternal Mortality Trend in Ethiopia. Ethiop J Health Dev. 2010;24:1.
Abeje G, Azage M, Setegn T. Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reproductive Health. 2014;11(1):22.
Amano A, Gebeyehu A, Birhanu Z. Institutional delivery service utilization in Munisa Woreda, South East Ethiopia. BMC Pregnancy Childbirth. 2012;12:105.
Shimeka AT, Mazengia FA, Meseret SW. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia. BMC Pregnancy Childbirth. 2012;12:74.
Alem A, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health. 2012;9:33.
Zegeye K, Gebeyehu A, Melese T. The Role of Geographical Access in the Utilization of Institutional Delivery Service in Rural Jimma Horro District, Southwest Ethiopia. Prim Health Care. 2014:4, 1.
Wolelie A, Aychiluhm M, Awoke W. Institutional delivery service utilization and associated factors in Banja District, Awie Zone, Amhara Regional Sate, Ethiopia. Open J Epidemiol. 2014;4(01):30.
Awoke W, Muhammed J, Abeje G. Institutional Delivery Service Utilization in Woldia, Ethiopia. Sci J Public Health. 2013;1:1.
Feyissa TR, Genemo GA. Determinants of Institutional Delivery among Childbearing Age Women in Western Ethiopia, 2013: Unmatched Case Control Study. PLoS One. 2014;9(5):1–7.
Odo D, Shifti D. Institutional delivery service utilization and associated factors among child bearing age women in Goba Woreda, Ethiopia. J Gynecol Obstet. 2014;2(4):63–70.
Dembecha district health office. 2014/15 Annual health plan, Dembecha, Ethiopia.
Ravi RP, Kulasekaran RA. Does Socio-demographic Factors Influence Women’s Choice of Place of Delivery in Rural Areas of Tamilnadu State in India. Am J Public Health Res. 2014;2(3):75–80.
Roy MP, Mohan U, Singh SK, Singh VK, Srivastava AK. Factors associated with the preference for delivery at the government hospitals in rural areas of Lucknow district in Uttar Pradesh. Indian J Public Health. 2013;57(4):268.
Exavery A. Access to institutional delivery care and reasons for home delivery in three districts of Tanzania. Int J Equity Health. 2014;13(48):11.
Esena RK, Sappor MM. Factors associated with the utilization of skilled delivery services in the Ga East Municipality of Ghana Part 2: barriers to skilled delivery. Int J Sci Tech Res. 2013;2(8):195–207.
Idris SH, Gwarzo UMD, Shehu AU. Determinants of Place of Delivery among Women in a Semi-Urban Settlement in Zaria, Northern Nigeria. Ann Afr Med. 2006;5:68–72.
Acknowledgments
Authors would like to thank Debre Markos University, Dembecha district health office, data collectors and study participants for their contribution for the finalization of this research.
Funding
The funding for this study was self.
Availability of data and materials
“The data that support the findings of this study has a sort of identifier of individual participants and researcher reserved to send it”.
Author information
Authors and Affiliations
Contributions
SK: Conception and design of the study, acquisition of data, analysis and interpretation of data. GD and TY: advising during proposal development, data analysis and interpretation and preparing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study proposal got ethical approval from Debre Markos University, health science college ethical review committee. Administrative bodies of Dembecha district were asked for their permission of the research to be conducted in the area. Informed oral and written consent was obtained from participants.
Consent for publication
“Not applicable”
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kidanu, S., Degu, G. & Tiruye, T.Y. Factors influencing institutional delivery service utilization in Dembecha district, Northwest Ethiopia: A community based cross sectional study. Reprod Health 14, 98 (2017). https://doi.org/10.1186/s12978-017-0359-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-017-0359-5