Abstract
Background
Having a health worker with midwifery skills present at delivery is one of the key interventions to reduce maternal and newborn mortality. We sought to estimate the frequencies of (a) skilled birth attendant coverage, (b) institutional delivery, and (c) the combination of place of delivery and type of attendant, in LMICs.
Methods
National surveys (DHS and MICS) performed in 80 LMICs since 2005 were analyzed to estimate these four categories of delivery care. Results were stratified by wealth quintile based on asset indices, and by urban/rural residence. The combination of place of delivery and type of attendant were also calculated for seven world regions.
Results
The proportion of institutional SBA deliveries was above 90 % in 25 of the 80 countries, and below 40 % in 11 countries. A strong positive correlation between SBA and institutional delivery coverage (rho: 0.97, p <0,001) was observed. Eight countries had over 10 % of home SBA deliveries, and two countries had over 10 % of institutional non-SBA deliveries. Except for South Asia, all regions had over 80 % of urban deliveries in the institutional SBA category, but in rural areas, only two regions (CEE & CIS, Middle East & North Africa) presented average coverage above 80 %. In all regions, institutional SBA deliveries were over 80 % in the richest quintile. Home SBA deliveries were more common in rural than in urban areas, and in the poorest quintiles in all regions. Facility non-SBA deliveries also tended to be more common in rural areas and among the poorest.
Conclusion
Four different categories of delivery assistance were identified worldwide. Pro-urban and pro-rich inequalities were observed for coverage of institutional SBA deliveries.
Similar content being viewed by others
Background
Globally, it is estimated between 1990 and 2015, 10.7 million women died from complications related to pregnancy and childbirth [1]. Besides, 2.8 million newborns died annually within 28 days of birth, with 2 million occurring within the first week of life [2, 3], and there are 2.6 million stillbirths of which 45 % occur during childbirth or labor [4]. Most of these deaths (99 %) and complications occur in LMICs, due to causes that are usually preventable [5]. However, laudable progress have been observed and the global maternal mortality rate (MMR) fell from 385 deaths per 100 000 livebirths in 1990 to 216 in 2015, corresponding to a relative decline of 43.9 % [1]. The neonatal mortality rate fell from 33 deaths per 1000 live births in 1990 to 20 in 2013, and stillbirths rate from 24.7 per 1000 live births in 2000 to 18.4 in 2015 [6]. Progress also have been observed in the countdown countries with reduction of maternal mortality ratio of 45 % over the past two decades [7].
To reduce these maternal, fetal and newborn deaths, several initiatives have been launched [8]; these include ensuring that deliveries are assisted by SBAs, and the extension of institutional deliveries coverage [9].
In 2000, maternal health was included as one of the Millennium Development Goal (MDG5), with the target of reducing the maternal mortality rate by three quarters by 2015 [8]. The proportion of births attended by a SBA was considered as a key indicator for monitoring progress on maternal and newborn health [10]. However, the MDGs have been criticized due to lack of emphasis on inequalities and recent efforts are underway to measure progress towards universal health care from an equity perspective [11, 12].
At a special session held by the United Nations General Assembly, it was agreed that all countries should increase their efforts to reach 80 % (by 2005) and 90 % (by 2015) coverage of skilled birth attendance [13]. Since then, countries have employed several strategies to achieve these goals [14]. However, there is variation among countries about the proper definition of SBA and the most appropriate place for delivery assistance. Some countries invested in training health care professionals to increase the coverage of institutional deliveries or home deliveries by a SBA. Other countries invested in providing some formal training to traditional birth attendants (TBAs) such as matrones [15].
The first attempt at defining SBA was made by the WHO/UNFPA/UNICEF/World Bank in 1999. However, it has been criticized for failing to refer to the place of delivery and therefore being biased towards facility births [16]. In 2004, a joint statement by WHO, the International Confederation of Midwives (ICM) and the International Federation of Gynecology and obstetrics (FIGO), proposed a more refined definition of a SBA relative to what had been first proposed in 1999 [17]. SBAs were defined as accredited health professionals such as midwifes, doctors or nurses who have been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns [17]. It was also recommended that deliveries should take place in a range of appropriate settings, from home to tertiary referral centre, depending on availability and need [18].
The term TBA (also known as traditional midwife, community midwife, matrones or rural auxiliary midwife, among others) refers to a health care provider who usually has not received any formal training, and who does not have professional certification or licensure [19, 20]. TBAs often work in rural and remote areas. Because of their access to such underserved communities, some countries, training institutions and non-governmental organizations have initiated efforts to TBAs in basic and emergency obstetric and other maternal health topics in order to strengthen the links between health services and communities, and thus improve health outcomes among women and newborns [15, 21]. Several countries regard TBAs who received some amount of formal training as SBAs, and include them in the primary health system [22]. The variability in the definition of SBAs has to be kept in mind when carrying out international comparisons [22, 23].
The recommendation on place of delivery, however, is controversial [24, 25]. Whereas some suggest that home delivery should be encouraged for women with low-risk, under the supervision of a SBA, others argue that pregnancy is always associated with risk and recommend institutional delivery for all. Yet, a third group argues that the place of delivery should be decided upon as a joint judgment between patients and professionals.
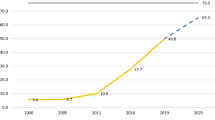
Monitoring of global SBA coverage showed an increase from 61.5 % in 2000 to 73 % in 2013 [26]. However, important inequalities remain between and within-country, with SBA coverage being the least equitable indicator related to maternal and newborn health [27, 28]. Developed countries had over 99 % coverage on SBA, while South Asia and the Sub-Saharan Africa had only 53 and 51 % coverage respectively [26]. While some countries have reached coverage over 90 % since 1990, many others are still struggling, even at the national aggregate level [29]. Place of residence (urban/rural) and household wealth are two keys dimension of inequalities in SBA coverage [30]. According to Channon et al., countries that have achieved high coverage of maternal health care by SBA from a relatively low baseline over the last decades have progressed through a common pathway. Further, the coverage has increased first among the urban rich, followed by the rural rich, the urban poor and the rural poor the last to be reached [30].
A review of the literature and preliminary analyses from various countries led to the identification of four categories of delivery assistance: 1) institutional delivery by a SBA; 2) home births by a SBA; 3) institutional delivery by an unskilled health provider [31, 32]; and 4) home births by an unskilled health provider [33, 34]. The present analyses were aimed at describing between and within-country inequalities in (a) skilled birth attendant coverage, (b) institutional delivery, and (c) the combination of place of delivery and type of attendant in LMICs.
Methods
Design and data sources
This study was based on publicly available data sets from large cross-sectional surveys nationally representative including Demographic Health Surveys (DHS) and the Multiple Indicator Cluster Surveys (MICS). Both types of surveys use standardized questionnaires, to collect information from women on birth attendance, place of delivery, childbirth, as well as on individual, household and community characteristics that allow for comparison of the result across countries. The surveys are typically conducted and implemented by the national central statistic agencies. Each survey contains information provided by women of reproductive age from 15 to 49 years old. Ethical approval was the responsibility of the institution that commissioned, funded, or carried out the surveys, which ensured the complete confidentiality of respondents. Details on DHS and MICS are available elsewhere [35, 36].
We used the latest available surveys from 80 LMICs belonging to the seven world regions as defined by the United Nations Children’s Fund (UNICEF) [36], and for which information were available for birth attendant and place of delivery as of 2005. Of these countries, 55 had DHS and 25 had MICS. For MICS, data were obtained from the child file and participants were women aged from 15 to 49 years with at least one live birth in the last two years. For DHS, data were obtained from the woman’s file and participants were women aged from 15 to 49 years with at least one live birth in the last 3 years; such limits of time periods were intended to avoid recall bias, and it is practically the only difference in terms of data collection on this topic. For both surveys, these files were matched with the household files that include the asset indices.
Outcomes
Two outcomes relative to childbirth were analyzed: delivery by a SBA and the place of delivery.
SBAs include doctors, nurses, midwifes and other cadres that individual countries recognize as such (auxiliary midwife, auxiliary nurse, community health officer) [13, 22]. Information on birth attendance in the survey questionnaires were collected through unprompted answers to the question “Who assisted with the delivery of (NAME OF THE CHILD)?”. Examples of the actual questions used in DHS and MICS are included in Additional file 1: Appendix A.
Regarding place of the delivery in both DHS and MICS questionnaires, the discrete nominal response variable was as followed: home (respondent’s home or another non-institutional setting); Public sector (government hospital, government health centre, government health post or other public sector); or private medical sector (private hospital or clinic, other private medical facility). Both public and private sector deliveries were considered as “institutional”. These information were obtained from a face-to-face application questionnaire with open response option (i.e. allowed multiple provider to be indicated per delivery) [35, 36].
These two outcome variables were then combined and categorized into four categories of delivery assistance: 1) institutional, SBA; 2) institutional, non-SBA; 3) home, SBA; 4) and home, non-SBA. These news variables are referred to as “combination of place of delivery and type of attendant.”
Another important category of delivery that has recently become a focus of interest in some countries is the women who deliver absolutely alone with “no one present (NOP)” [37]. In our analyses, we opted not to include this category because data on NOP were not available for most countries.
Stratification variables
Two main stratifiers were considered in this study: place of residence of the women and the wealth index scores. Place of residence was coded as either urban or rural. As direct measures of living standards such as income, expenditure and consumption are rarely collected in the DHS and MICS surveys. These surveys collect information on household assets and characteristics of the dwelling, that can be used as a proxy measure for living standards, known as asset or wealth index [38, 39]. We used the wealth index scores based on Principal Component Analyses, calculated by the original DHS and MICS survey team for each household and presented in quintiles [39]. Quintile 1 (Q1) represents the poorest 20 % of households in the survey sample and quintile 5 (Q5) represents the richest 20 %.
Statistical analysis
Descriptive analyses were carried out for each country to estimate the frequencies of (a) SBA coverage, (b) institutional delivery, and (c) the combination of place of delivery and type of attendant. Analyses were stratified according to the seven UNICEF world regions. Pearson’s correlation was used to calculate the association between SBA and institutional deliveries at country level. Significance testing of the association between the outcomes and place of residence and wealth quintiles, at individual level, was done using chi-squared tests for heterogeneity and for linear trends for a subset of countries with unusual pattern of delivery assistance (see below). When a proportion was equal to zero or 100 %, exact binomial confidence intervals were calculated.
All analyses were carried out with STATA (version 13.1) and EXCEL 2013, taking into account the sampling design characteristics of each survey and the sample weights. When calculating regional mean values, we opted not to use country weights because information was missing for several countries in some regions.
Results
In the 80 countries studied, 73.8 % (±23.2 SD) of births were assisted by SBAs, and 70.5 % (±24.6 SD) were inside a health institution.
Figure 1 shows the description of the four categories of delivery assistance in the most recent surveys by country. For 25 out of the 80 countries, the proportion of deliveries by a SBA in a health facility was above 90.0 %. However, 11 countries have fewer than 40.0 % of births in this category. All of the latter are low-income countries according to the World Bank classification.
Six countries - Azerbaijan (10.3 %), Cambodia (14.4 %), Indonesia (18.5 %), Iraq (14.5 %), Philippines (10.0 %) and Tajikistan (10.8 %) - had more than 10 % of all births assisted by a SBA outside a health facility. Two countries - Senegal (19.4 %) and Togo (13.8 %) - had over 10.0 % of all births carried out in a health facility by a non-SBA.
Figure 2 shows a strong positive correlation between SBA and institutional delivery coverage, by country (Pearson’s correlation: 0.97, p <0,001). In the 80 countries studied, 98.3 % of institutional deliveries are performed by a SBA, and 95.8 % of SBA deliveries are in an institution. Eight countries (Azerbaijan, Cambodia, Indonesia, Iraq, Philippines, Tajikistan, Senegal and Togo) are outliers, and will be discussed below.
Association between SBA and institutional delivery coverage in low and middle-income countries (see Additional file 5 for country codes) (Pearson correlation coefficient = 0.97, P <0.001)
Descriptions of the four categories of delivery assistance according to place of residence and wealth quintiles with the corresponding significance levels are presented in appendix (Additional file 2: web appendix tables A1 and A2).
Figure 3 shows the unweighted average value of the four categories of delivery assistance by world region, according to place of residence (urban or rural). Except for South Asia, all regions have over 80.0 % of urban deliveries by a SBA in a health facility. In rural areas, only two regions (CEE & CIS, Middle East & North Africa) present average coverage above 80.0 %. Home SBA deliveries are more common in rural than in urban areas in all regions. However, regional averages may hide important differences among countries (see Additional file 2: web appendix figures A1–A7). For example, home SBA deliveries are common in the rural areas of countries such as Peru (5.6 %), Suriname (6.1 %) and Bolivia (7.4 %) (Additional file 2: Figure A1); Philippines (10.0 %), Cambodia (15.6 %) and Indonesia (26.5 %) (Additional file 2: FigureA2); and in Azerbaijan (15.6 %) and Tajikistan (12.2 %) (Additional file 2: Figure A3). In contrast, home SBA deliveries are common in the urban areas of Afghanistan (9.4 %), Guinea (13.6 %), Chad (15.8 %) and Madagascar (21.2 %) (Additional file 2: Figure A4–A6). In Egypt and Iraq, home SBA deliveries were common in both urban and rural areas (Additional file 2: Figure A7).
Results stratified by wealth quintiles are shown in Fig. 4. In all regions, births in a health facility by a SBA were more common in the richest quintiles, while home deliveries (with or without a SBA) were more common in the poorest quintiles. Despite a relative lower prevalence, facility deliveries by unskilled health workers also tended to be more common among the poor. In East Asia Pacific, 8.3 % of deliveries in the poorest quintile are home SBA, but in other regions these represent only 3.0 %. Important differences were also observed among countries: Indonesia and Tajikistan have more than 15.0 % of home SBA deliveries in the poorest quintiles, while in Madagascar the situation is reversed, with 23.6 % in the richest quintile (Additional file 2: web appendix figures B1-B7).
Countries with more than 10.0 % of either home SBA delivery (Tajikistan, Philippines, Iraq, Indonesia, Cambodia and Azerbaijan), or facility non-SBA deliveries (Togo and Senegal) were analyzed separately (Figs. 5 and 6). Home SBA deliveries were more pronounced in rural areas. In Senegal, facility non-SBA deliveries were common in both urban and rural areas (15.2 and 22.6 % respectively); while in Togo, these were more frequent in rural areas (20.1 %) (Fig. 5). All differences were significant except for Iraq (p = 0,93) and Philippines (p = 0,23) (Additional file 3: Web appendix C).
Figure 6 shows a similar analysis by wealth quintiles. In the poorest quintiles, home SBA deliveries vary from 12.6 % in Cambodia to 28.1 % in Indonesia, and in the richest quintiles, this proportion goes from 0.9 % in Azerbaijan to 12.6 % in Iraq. In both Senegal and Togo, facility births by a non-SBA were more common in the three poorest quintiles.
Pro-poor patterns were observed for home SBA and institutional deliveries by an unskilled worker, except for Iraq (p: 0.071) (Additional file 4: Web appendix D).
Discussion
Place of delivery and type of attendant are both important determinants of maternal and newborn health [7, 26]. The purpose of this study was to estimate the frequencies of (a) SBA coverage, (b) institutional delivery, and (c) the combination of place of delivery and type of attendant in LMICs. Similar analyses were recently published for 57 countries using DHS data, with a focus on the private and public sectors in four world regions [40]. We present analyses for 80 countries with data from both MICS and DHS, stratified by place of residence and wealth asset index. Our results are analyzed according to seven world regions using the UNICEF classification. Place of delivery and type of attendant were combined into four categories of delivery assistance, to allow for the possibilities that deliveries in health facilities are not necessarily performed by SBAs, and that deliveries outside a health facility do not necessarily represent unskilled birth attendance. We did not find any systematic studies on these four categories of delivery assistance in the literature.
We show that coverage of SBA at delivery varies widely across LMICs. In 25 out of the 80 countries studied, the national coverage was over 90.0 %; these countries have reached the 2015 target proposed by the United Nations General assembly in 1999 [22, 41]. On the other extreme, 11 low-income countries [42] have national coverage below 40 %. These results are consistent with recent findings in the literature [29, 40, 42, 43]. In addition, pro-urban and pro-rich inequalities were documented, both at the national and regional level. These results are also consistent with other recent publications [29, 44, 45].
When we analyzed the correlations between SBA coverage and institutional deliveries at country level, two groups of countries were outliers. Azerbaijan, Cambodia, Indonesia, Philippines, Iraq and Tajikistan the prevalence of home SBA deliveries was over 10.0 %, being higher in rural areas and in the poorest quintiles. In Senegal and Togo, the proportion of births in a health facility by unskilled birth attendants was above 10.0 %, being higher in the poorest quintiles and – in Togo – in rural areas. We sought to understand why these categories are so prevalent in these two groups of countries.
Since the launch of the Safe Motherhood Initiative in 1987 and of the Millennium Development Goals in 2000, countries have adopted different strategies to improve maternal and newborn health outcomes [10, 46, 47]. In several countries, delivery by SBAs outside health facilities have been promoted. In the Philippines, “birthing homes” supervised by public or private health facilities provide birthing services including antenatal, normal spontaneous delivery, and postnatal care, particularly in rural and poor population [44, 45]. This service is provided by accredited health personnel, generally midwives, with a minimum of 2 years training [48–50]. In Indonesia, the situation is very similar except that the duration of the training program is one year [51, 52]. In Cambodia, no formal program about home SBA is reported in the literature. According to Por et al., home SBA deliveries are driven by economic interest from government health personnel, who can charge women for the delivery at home, but not in a public facility [53, 54]. In Tajikistan, health care has deteriorated dramatically since 1991 [55, 56], and most rural maternities are operating without the basic conditions such as heat or running water. Thus, women consider giving birth at home safer, more comfortable and affordable than in a facility [55–57]. In contrast, in Azerbaijan, a system known as “feldsher-accoucher points” staffed by mid-level health care providers who focus on primary health care in rural areas is in charge of assisting deliveries at home [57, 58]. In Iraq, due to decades of war and economic sanctions, many health facilities have faced serious difficulties in keeping functioning and providing adequate health care [59]. Besides, the fear of terrorist attacks has reportedly led patients to avoid public spaces such as health facilities, and some women feel more secure by requesting a health care provider to assist their births at home [59]. These are likely the reasons why home SBA deliveries are so prevalent in these countries, especially in rural areas and in the poorest quintiles.
A different pattern was observed in West-African countries such as Senegal and Togo, where more than 10 % of institutional deliveries were carried out by unskilled birth attendants. According to Kodio et al., in some villages in Senegal, no qualified midwife or nurse are presented in the health facility and deliveries are generally assisted by a traditional birth attendant (known as “matrone” in French or a community health worker (CHW)) [32]. In Togo, the situation is not different and health post at village level provide maternity services that are often run by matrones or other voluntary community health workers [60]. Institutional deliveries by unskilled attendants were also common – although not as much as in Togo and Senegal – in other African countries such as Benin (4 %), Central African Republic (5 %), and The Gambia (6 %).
In 1997, the World Health Organization document stated that “birth can take place in a range of appropriate settings, from home to tertiary referral centres, depending on availability and need [61]. It also recognized that home delivery could be appropriate for normal deliveries, provided the person attending the delivery is well trained and equipped [61]. Over time, the focus on SBA moved from coverage to quality of care in facilities, as many countries adopted strategies for promoting institutional deliveries. The World Health Report 2005 promoted care close to home – e.g. with midwives deployed in health centers and referral backup hospitals staffed by doctors, nurses and midwives [62]. Over time, the focus is also changing from measuring coverage to assessing and improving quality of care for facility births [63]. The shift from coverage to quality is at least in part motivated by studies showing that increased coverage of SBA and/or institutional deliveries does not necessarily improve maternal or newborn outcomes [64–68]. The growing focus on institutional birth should take into account the fact that in a few countries, many such deliveries are carried out by unskilled birth attendants, and therefore do not contribute to achieving the recommendations for increasing SBA coverage [18].
There is little evidence about the effectiveness of home SBA deliveries in the literature. Most research regarding home birth strategies has focused on the training of TBAs [15, 21], while home SBA deliveries have received little attention. In our study, pro-poor and pro-rural inequalities on home SBA deliveries at the national level were observed, consistently with previous publications [55, 69]. In spite of the existing inequalities among home SBA utilization, information on the quality of care provided at home remain scant. Constraints encountered by SBAs during home delivery are numerous and include inappropriate environment for delivery, insufficient supplies and equipment, lack of security, inadequate training for home delivery, lack of transportation for referrals, and the social pressure in life-and-death situations, all of which affect the quality of care [25, 70]. Some authors have stressed the limitations of home SBA deliveries for reducing maternal and newborn outcomes [51, 64]. On the other hand, several advantages have been reported for home SBAs deliveries, such as lower rate of medical interventions (episiotomy, forceps, vacuum extraction among others), social support, privacy and higher proportions of birth receiving skin-to-skin practices in immediate breastfeeding within one hour after birth [24, 71, 72]. Assessing the quality of home deliveries by SBAs is beyond the scope of the present analyses, but our contribution lies in highlighting that such births are common in several countries, and deserve further evaluation.
Our analyses have some limitations. The first is related to the definition of SBA. As initially proposed by WHO, SBAs included doctors, nurses and midwives [18]. In many countries, others cadres such as auxiliary nurses, auxiliary midwifes, community health workers, and even TBAs or matrones who received some degree of formal training may be considered as skilled, making it difficult to compare among countries [22]. We believe that analyses such as ours may help identify countries with unusual patterns, which may be associated with non-standard definitions of SBA. Second, SBA coverage in national surveys was based on maternal reports, and some women may be unable to provide accurate information. For example, Hussein et al. described the difficulties of women in discriminating accurately among different types of birth attendants in Ghana [73]. We believe that this situation could be similar in others countries, especially where SBA coverage is low. On the other hand, studies on the validity of self-report SBA question during delivery conducted in Kenya and Mexico have shown that, while this indicator is not recommended for use at the individual level, it could be used to generate acceptable estimate of SBA coverage at population level [74, 75]. Third, our analysis uses available data for countries for the period 2005–2014, but only three surveys were carried out prior to 2007, and with a few exceptions SBA coverage is increasing slowly in most countries [76]. Because not every country was included, there may be additional examples of the outlier patterns we described above. Fourth, wealth asset indices were used to analyze economic status; such indices may vary according to the choice of assets and are affected by issues of comparability between urban and rural household [77, 78]. In addition, wealth quintiles are relative measures, that is, the poorest quintile in a middle-income country might be the wealthier than the third or fourth quintile in an extremely poor country [27].
Nevertheless, use of asset indices allows systematic comparisons of inequalities in health that would not be possible with other more complex measures of socioeconomic position [27]. Finally, we defined inequality based on wealth asset indices and place of residence, a common tool for evaluating inequalities within populations [78]. Other determinants such as education, distance to health facility, ethnicity, occupation and religion, among others may be equally or even more important in affecting access to delivery care.
The above limitations, however, are unlikely to affect our main conclusions. To our knowledge, this is the first study that analyzes inequalities in these four categories of delivery assistance in a large number of LMICs countries using both DHS and MICS survey databases.
Conclusions
We report a high correlation between coverage with SBA and institutional delivery coverage. As noted, approximately 98.0 % of institutional deliveries are performed by a SBA, and 96.0 % of SBA deliveries are in an institution. There are, however, some exceptions and 4,2 % of SBA deliveries are performed outside a health facility and 1,7 % of institutional deliveries are by unskilled birth attendants. Except for institutional deliveries carried out by SBAs, all other types of assistance were more common among the poor and rural populations. Analyses that take into account both place of delivery and type of attendant are important to help scale up safe delivery attendance for all women, and specially in remote areas where SBAs are scarce.
Abbreviations
CAR, Central African Republic; CEE, Central and Eastern Europe; CHW, Community Health Worker; CIS, Commonwealth of Independent States; DHS, Demographic Health Surveys; FIGO, International Federation of Gynecology and obstetrics; ICM, International Confederation of Midwives; LAC, Latin American and Caribbean; LMIC, Low and Middle-Income Country; MDG, Millennium Development Goal; MICS, multiple indicator cluster surveys; SBA, skilled birth attendant; SD, standard deviation; TBA, traditional birth attendant; UNICEF, United Nations Children’s Fund; WHO, World Health Organization
References
Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2015;387:462-74.
Levels & Trends in Child Mortality. Report 2014. Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. 2014.
You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet. 2015;386(10010):2275–86.
Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2016;4(2):e98–e108.
UNICEF (United Nations Children’s Fund). Trends in maternal mortality: 1990 to 2013. New York: UNICEF; 2014.
Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387(10018):587–603.
Requejo J, et al. A Decade of Tracking Progress for Maternal, Newborn and Child Survival, the 2015 Report. Geneva: UNICEF and World Health Organization; 2015.
Starrs A. Safe motherhood initiative: 20 years and counting. Lancet. 2006;368(9542):1130–2.
WHO (World Health Organization), UNICEF (United Nations Children’s Fund), UNFPA (United Nations Fund for Population Activities). Trends in Maternal Mortality: 1990 to 2010: WHO, UNICEF, UNFPA, and The World Bank estimates. Geneva: WHO; 2012.
Graham WJ, Bell JS, Bullough CHW. Can skilled attendance at delivery reduce maternal mortality in developing countries. In: De Brouwere V, Van Lerberghe W, editors. Safe motherhood strategies: a review of the evidence. New York: ITGPress; 2001. p. 97–130.
Waage J, Banerji R, Campbell O, Chirwa E, Collender G, Dieltiens V, et al. The Millennium Development Goals: a cross-sectoral analysis and principles for goal setting after 2015. Lancet. 2010;376(9745):991–1023.
WHO (World Health Organization), The World Bank. Monitoring progress towards universal health coverage at country and global levels: framework, measures and targets. Geneva: WHO; 2014.
WHO (World Health Organization). Skilled attendant at birth: 2006 updates. Geneva: WHO; 2006.
Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999;77(5):399.
Gloyd S, Floriano F, Midwife MS, Chadreque MA, Nyangezi JM, Platas A. Impact of traditional birth attendant training in Mozambique: a controlled study. J Midwifery Womens Health. 2001;46(4):210–6.
WHO (World Health Organization), UNFPA (United Nations Fund for Population Activities), UNICEF (United Nations Children’s Fund), World Bank. Reducing maternal mortality. A joint statement by WHO/UNFPA/UNICEF/World Bank. Geneva: WHO; 1999.
WHO (World Health Organization). Making pregnancy safer: the critical role of the skilled attendant: joint statement by WHO, ICM and FIGO. Geneva: WHO; 2004.
WHO (World Health Organization). Maternal and newborn health: safe motherhood. Geneva: WHO; 1997.
Leedam E. Traditional birth attendants. Int J Gynaecol Obstet. 1985;23(4):249–74.
Warren N, Norr KF, Keeney GB. Matroniya: the lived experiences of rural auxiliary midwives in Koutiala, Mali. Health Care Women Int. 2013;34(6):482–98.
Bergström S, Goodburn E. The role of traditional birth attendants in the reduction of maternal mortality: Studies in Health Service Organization and Policy. 2000.
WHO (World Health Organization). Proportion of births attended by a skilled attendant: 2008 updates. Geneva: WHO; 2008.
Adegoke A, Utz B, Msuya SE, Van Den Broek N. Skilled Birth Attendants: who is who? A descriptive study of definitions and roles from nine Sub Saharan African countries. PLoS One. 2012;7(7):e40220.
Mahdi SS, Habib OS. A study on preference and practices of women regarding place of delivery. East Mediterr Health J. 2010;16(8):874–78.
Blum LS, Sharmin T, Ronsmans C. Attending home vs. clinic-based deliveries: perspectives of skilled birth attendants in Matlab, Bangladesh. Reprod Health Matters. 2006;14(27):51–60.
WHO (World Health Organization). Tracking universal health coverage: first global monitoring report. Geneva: WHO; 2015.
Barros AJ, Ronsmans C, Axelson H, Loaiza E, Bertoldi AD, França GV, et al. Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. 2012;379(9822):1225–33.
WHO (World Health Organization). State of inequality: Reproductive, maternal, newborn and child health. Geneva: WHO; 2015.
Neal S, Channon AA, Carter S, Falkingham J. Universal health care and equity: evidence of maternal health based on an analysis of demographic and household survey data. Int J Equity Health. 2015;14(1):56.
Channon AA, Neal S, Matthews Z, Falkingham J. Maternal health inequalities over time: is there a common pathway? Background paper for “addressing inequalities the heart of the post-2015 development agenda and the future we want for all global thematic consultation”. 2013.
Kodio B, De Bernis L, Ba M, Ronsmans C, Pison G, Etard JF. Levels and causes of maternal mortality in Senegal. Trop Med Int Health. 2002;7(6):499–505.
Ministere de la Sante. Normes du district sanitaire au Togo. Lomé: MS; 2001.
Fikre AA, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health. 2012;9:33.
Fapohunda BM, Orobaton NG. When women deliver with no one present in Nigeria: who, what, where and so what? PLoS One. 2013;8(7):e69569.
Macro International. Demographic and Health Surveys (DHS). https://dhsprogram.com/What-We-Do/Methodology.cfm (accessed 17 May 2016).
UNICEF (United Nations Children’s Fund). Information by country and programme. New York: UNICEF; 2015. http://www.unicef.org/statistics/index_24302.html (accessed May 17, 2016).
Orobaton N, Austin A, Fapohunda B, Abegunde D, Omo K. Mapping the prevalence and sociodemographic characteristics of women who deliver alone: evidence from demographic and health surveys from 80 Countries. Glob Health Sci Pract. 2016;4(1):99–113.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure Data—Or tears: an application to educational enrollments in states of india. Demography. 2001;38(1):115–32.
Rutstein SO, Johnson K. The DHS wealth index. DHS comparative reports no. 6. Calverton: ORC Macro; 2004.
Benova L, Macleod D, Footman K, Cavallaro F, Lynch CA, Campbell OM. Role of the private sector in childbirth care: cross‐sectional survey evidence from 57 low‐and middle‐income countries using Demographic and Health Surveys. Trop Med Int Health. 2015;20(12):1657–73.
UN (United Nations). Report of the Ad Hoc Committee of the Whole of the Twenty-first Special Session of the General Assembly (General Assembly document, No. A/S-21/5/Add.1). New York: UN; 1999.
The World Bank. Country and Lending Groups. New York: WB; 2015.
Amoako Johnson F, Padmadas SS, Matthews Z. Are women deciding against home births in low and middle income countries? PLoS One. 2013;8(6):e65527.
Limwattananon S, Tangcharoensathien V, Sirilak S. Trends and inequities in where women delivered their babies in 25 low-income countries: evidence from Demographic and Health Surveys. Reprod Health Matters. 2011;19(37):75–85.
Victora CG, Barros AJ, Axelson H, Bhutta ZA, Chopra M, França GV, et al. How changes in coverage affect equity in maternal and child health interventions in 35 Countdown to 2015 countries: an analysis of national surveys. Lancet. 2012;380(9848):1149–56.
Van Lerberghe W, De Brouwere V. Of blind alleys and things that have worked: history’s lessons on reducing maternal mortality: epidemiological report. 2000.
McClure EM, Saleem S, Goudar SS, Moore JL, Garces A, Esamai F, et al. Stillbirth rates in low-middle income countries 2010–2013: a population-based, multi-country study from the Global Network. Reprod Health. 2015;12 Suppl 2:S7.
Republic of the Philippines, Department of Health. Implementing health reforms for rapid reduction of maternal and neonatal mortality. Manila: Department of Health; 2008.
Republic of the Philippines, Office of the President, Commission on Higher Education. Updated policies and standards for midwifery education. Manila: Commission on Higher Education; 2007.
Sobel HL, Oliveros YE, Nyunt US. Secondary analysis of a national health survey on factors influencing women in the Philippines to deliver at home and unattended by a healthcare professional. Int J Gynaecol Obstet. 2010;111(2):157–60.
Hatt L, Stanton C, Ronsmans C, Makowiecka K, Adisasmita A. Did professional attendance at home births improve early neonatal survival in Indonesia? Health Policy Plan. 2009;24(4):270–8.
Ronsmans C, Endang A, Gunawan S, Zazri A, McDermott J, Koblinsky M, et al. Evaluation of a comprehensive home‐based midwifery programme in South Kalimantan, Indonesia. Trop Med Int Health. 2001;6(10):799–810.
Ir P, Korachais C, Chheng K, Horemans D, Van Damme W, Meessen B. Boosting facility deliveries with results-based financing: a mixed-methods evaluation of the government midwifery incentive scheme in Cambodia. BMC Pregnancy Childbirth. 2015;15:170.
Por I, Horeman D, Narin S, Van Damme W. Improving access to safe delivery for poor pregnant women: a case study of vouchers plus health equity funds in three health districts in Cambodia. Studies in HSO&P. 2008;24:225-53.
Falkingham J. Inequality and changes in women’s use of maternal health-care services in Tajikistan. Stud Fam Plann. 2003;34(1):32–43.
Falkingham J, Evandrou M, Lyons-Amos M. Inequalities in child and maternal health outcomes in CEE and the CIS. Southampton: Centre for Population Change; 2012.
European Observatory on Health Care Systems. Health Care Systems in Transition: Kazakhstan. Geneva: WHO; 1999.
Sule H, Kazimov S, Shahmaliyev O, Sirois A. State of emergency medicine in Azerbaijan. Int J Emerg Med. 2008;1(1):3–9.
Kupyers B. The impact of war on the practice of midwifery and the wellbeing of women and children in Iraq. In: Reid L, editor. Midwifery, Freedom to Practise? An International Exploration and Examination of Midwifery Practice. Edinburgh: Churchill Livingstone; 2007. p. 164.
Republique Togolaise, Ministere de la Sante. Normes du district sanitaire au Togo. Lomé: MS; 2001.
WHO (World Health Organization). Care in normal birth: a practical guide. Geneva: WHO; 1997.
WHO (World Health Organization). Make every mother and child count: overview. Geneva: WHO; 2005.
Tunçalp Ӧ, Were WM, MacLennan C, Oladapo OT, Gülmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns: the WHO vision. BJOG. 2015;122(8):1045–9.
Ronsmans C, Scott S, Qomariyah SN, Achadi E, Braunholtz D, Marshall T, et al. Professional assistance during birth and maternal mortality in two Indonesian districts. Bull World Health Organ. 2009;87(6):416–23.
Singh K, Brodish P, Suchindran C. A regional multilevel analysis: can skilled birth attendants uniformly decrease neonatal mortality? Matern Child Health J. 2014;18(1):242–9.
Pfeiffer C, Mwaipopo R. Delivering at home or in a health facility? Health-seeking behaviour of women and the role of traditional birth attendants in Tanzania. BMC Pregnancy Childbirth. 2013;13(1):55.
Montgomery AL, Fadel S, Kumar R, Bondy S, Moineddin R, Jha P. The effect of health-facility admission and skilled birth attendant coverage on maternal survival in India: a case–control analysis. PLoS One. 2014;9(6):e95696.
Fink G, Ross R, Hill K. Institutional deliveries weakly associated with improved neonatal survival in developing countries: evidence from 192 Demographic and Health Surveys. Int J Epidemiol. 2015;44(6):1879–88.
Anwar I, Sami M, Akhtar N, Chowdhury M, Salma U, Rahman M, et al. Inequity in maternal health-care services: evidence from home-based skilled-birth-attendant programmes in Bangladesh. Bull World Health Organ. 2008;86(4):252–9.
Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370(9595):1358–69.
Johnson KC, Daviss B-A. Outcomes of planned home births with certified professional midwives: large prospective study in North America. BMJ. 2005;330(7505):1416.
Pagel C, Prost A, Hossen M, Azad K, Kuddus A, Roy SS, et al. Is essential newborn care provided by institutions and after home births? Analysis of prospective data from community trials in rural South Asia. BMC Pregnancy Childbirth. 2014;14(1):99.
Hussein J, Hundley V, Bell J, Abbey M, Asare GQ, Graham W. How do women identify health professionals at birth in Ghana? Midwifery. 2005;21(1):36–43.
Berdichevsky K, Diaz-Olavarrieta C, McCarthy K, Blanc A. Validating indicators of the quality of maternal health care: final report, Mexico. Mexico City: Population Council; 2014.
Warren C, Kimani J, Kivunaga J, Mdawida B, Ndwiga C, McCarthy K, et al. Validating indicators of the quality of maternal health care: final report, Kenya. Nairobi: Population Council; 2014.
Walker N, Yenokyan G, Friberg IK, Bryce J. Patterns in coverage of maternal, newborn, and child health interventions: projections of neonatal and under-5 mortality to 2035. Lancet. 2013;382(9897):1029–38.
Houweling TA, Kunst AE, Mackenbach JP. Measuring health inequality among children in developing countries: does the choice of the indicator of economic status matter? Int J Equity Health. 2003;2(1):8.
Rutstein SO, The DHS. Wealth index: approaches for rural and urban areas. Calverton: Macro International; 2008.
Acknowledgments
This paper was made possible thanks to the contribution of The Wellcome Trust Foundation (Grant Number: 101815/Z/13/Z); Bill & Melinda Gates Foundation; and Associação Brasileira de Saúde Coletiva (ABRASCO). We thank Cíntia Borges for her contribution in the formatting process of the tables and Figures, and Fatima Maia for her contribution with the formatting process of the references. We also thank the contribution of Matthews Mathai for providing useful information about maternal health service in some Asian countries.
Funding
Wellcome Trust Foundation, Bill & Melinda Gates Foundation; Associação Brasileira de Saúde Coletiva (ABRASCO).
Data availability
Data supporting our finding are made available through a spreadsheet document “Datasets availability.xlsx”.
Authors’ contributions
GJ participated in the conception of the study, performed the statistical analysis, interpreted the results and drafted the manuscript. FCW and AJDB participated in the acquisition, the statistical analysis and in the interpretation of the findings. CGV and ICS participated in the design of the study, the interpretation of the findings and the writing of the manuscript. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Ethical approval was the responsibility of the institution that commissioned, funded, or carried out the surveys, which ensured the complete confidentiality of respondents.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Web appendix A: DHS and MICS QUESTIONNAIRE. (PDF 178 kb)
Additional file 2:
(PDF 1141 kb)
Additional file 3:
Web appendix C: Distribution of place of delivery and type of professional in countries with at least 10 % of home SBA deliveries (Azerbaijan, Cambodia, Indonesia, Iraq, Philippines and Tajikistan) or at least 10 % of institutional deliveries by an unskilled worker (Senegal and Togo), by urban-rural residence. (PDF 217 kb)
Additional file 4:
Web appendix D: Distribution of place of delivery and type of professional in countries with at least 10 % of home SBA deliveries (Azerbaijan, Cambodia, Indonesia, Iraq, Philippines and Tajikistan) or at least 10 % of institutional deliveries by an unskilled worker (Senegal and Togo), by wealth quintile. (PDF 155 kb)
Additional file 5:
Web appendix B: ISO codes. (PDF 196 kb)
Additional file 6:
(XLSX 47 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Joseph, G., da Silva, I.C.M., Wehrmeister, F.C. et al. Inequalities in the coverage of place of delivery and skilled birth attendance: analyses of cross-sectional surveys in 80 low and middle-income countries. Reprod Health 13, 77 (2016). https://doi.org/10.1186/s12978-016-0192-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-016-0192-2