Abstract
Introduction
Women with postpartum haemorrhage (PPH) in developing countries often present in critical condition when treatment might be insufficient to save lives. Few studies have shown that application of non-pneumatic anti-shock garment (NASG) could improve maternal survival.
Methods
A systematic review of the literature explored the effect of NASG use compared with standard care for treating PPH. Medline, EMBASE and PubMed were searched. Methodological quality was assessed following the criteria suggested by the Cochrane Effective Practice and Organization of Care Group. Guidelines on Meta-analysis of Observational Studies in Epidemiology were used for reporting the results. Mantel-Haenszel methods for meta-analysis of risk ratios were used.
Results
Six out 31 studies met the inclusion criteria; only one cluster randomized controlled trial (c-RCT). Among observational studies, NASG fared better than standard care regarding maternal mortality reduction (Relative Risk (RR) 0.52 (95% Confidence interval (CI) 0.36 to 0.77)). A non-significant reduction of maternal mortality risk was observed in the c-RCT (RR: 0.43 (95% CI: 0.14 to 1.33)). No difference was observed between NASG use and standard care on use of blood products. Severe maternal outcomes were used as proxy for maternal death with similar pattern corroborating the trend towards beneficial effects associated with NASG.
Conclusion
NASG is a temporizing alternative measure in PPH management that shows a trend to reduce PPH-related deaths and severe morbidities. In settings where delays in PPH management are common, particularly where constraints to offer blood products and definitive treatment exist, use of NASG is an intervention that should be considered as a policy option while the standard conditions for care are being optimized.
Similar content being viewed by others
Introduction
Maternal mortality is a public health indicator related to social development and health equity around the world and one of the main indicators for monitoring the progress toward the Millennium Development Goal 5 (MDG-5). According to global estimates, haemorrhage accounted for 661,000 maternal deaths around the world between 2003 and 2009 which represents about 27% of all maternal deaths [1]. Most of these deaths are avoidable and take place in low-income countries [2]. Severe postpartum haemorrhage (PPH) is a leading cause of these deaths and is defined as a condition of maternal active genital bleeding after delivery, with at least one of the following: perceived abnormal bleeding (1000 mL of more) or any bleeding with hypotension or blood transfusion [3]. The use of uterotonics following cord clamping can reduce the occurrence of postpartum haemorrhage [2,3]. In addition to prophylactic uterotonics, growing evidence suggest that appropriate management of PPH could prevent maternal deaths related to severe PPH. Appropriate PPH management includes a rapid recognition of persistent blood loss after initial interventions such as uterotonics and fluid resuscitation [2,4]. Continuous monitoring and assessment of the woman just after delivery would allow implementation of appropriate interventions to reduce blood loss should PPH occur. However, in many settings around the world, delays during PPH prevention, diagnosis and treatment occur and contribute to avoidable maternal death and morbidity [5].
The Non-pneumatic Anti-Shock Garment (NASG) is a device developed as a temporizing measure to regain hemodynamic stability and allow patient transfer or definitive PPH treatment. The NASG is a compression suit made of five neoprene segments that close tightly with Velcro around the legs, pelvis and abdomen [6]. The lower body circumferential pressure made by the device shunts blood from the lower extremities and abdominal area to the essential core organs: heart, lungs, and brain. Within minutes of application, women suffering from shock have been seen to regain consciousness, normalize their vital signs and reduce the blood loss [7,8]. An observational study suggested that NASG use adds some time for postpartum haemorrhage women until definitive treatment can be reached, especially in other aetiologies rather than ruptured uterus [9]. In five quasi-experimental, non-randomized studies, NASG intervention at tertiary facilities was associated with reduced odds of death for women with hypovolemic shock secondary to obstetric hemorrhage [10]. Lastly a qualitative study in rural areas in Mexico suggested positive responses on acceptability of health personel to NASG [11]. Fostered by the observational trends of effect on NASG use for improving maternal health conditions. We conducted a systematic review to assess the effectiveness and safety of using NASG in improving maternal outcomes following severe PPH in settings where recourses are scare or definitive treatment to PPH may be delayed.
Methods
We conducted a systematic review of the literature following the Meta-Analysis Of Observational Studies in Epidemiology guidelines and the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement with a pre-specified protocol for data collection [12,13]. The standard care for treating PPH is defined by WHO guideline consisting on using uterotonics, uterine massage and fluid resuscitation with crystalloids [2]. All studies presenting comparison between standard care for treating hypovolemic shock secondary to PPH and standard care plus NASG application were eligible to this systematic review. Data collection process followed a standard collection form. The outcomes of interest were maternal mortality, severe maternal outcomes defined by the severe maternal morbidity plus maternal deaths, maternal side effects requiring treatment and the use of blood products.
An electronic search was conducted in March 2014 using the following online databases: Medline, EMBASE and PubMed. The search strategy used was NASG [All Fields] OR (non-pneumatic [All Fields] AND anti-shock [All Fields] AND (“clothing”[MeSH Terms] OR “clothing” [All Fields] OR “garment”[All Fields])). All studies identified through the electronic search had their titles and abstracts examined. Publications with incomplete reporting results and non-intention to treat analysis were excluded. Full texts of eligible studies were retrieved and assessed without language restrictions. The reference list of eligible studies was also screened to identify other potentially relevant paper to this review. Leading researchers in the field were contacted in the search for additional studies, particularly unpublished ones. Two reviewers assessed all eligible studies and a third reviewer was consulted in the cases of disagreement (CPC). Quality assessment of the studies was conducted based on Cochrane Effective Practice and Organisation of Care Group guidelines [14], Strengthening the Reporting of Observational studies in Epidemiology [13] and Consolidated Standards of Reporting Trials (CONSORT: extension to cluster randomized trials) [15]. Single data extraction was conducted (VNP) and checked by a second reviewer (JPS). Authors of included studies were contacted for providing data on outcomes of interest not included in the published reports.
Review Manager 5 Software (RevMan, computer program. Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012) was used for quantitative analysis [16]. Random effect Mantel-Haenszel methods for meta-analysis of risk ratios were used to produce pooled estimates of effect on NASG use for controlling PPH. Heterogeneity was measured with I2 test. Grading of the quality of evidence and the strength of recommendations tables were produced in order to inform decision making process for developing recommendations once it combines transparency in judgments of the best available evidence, with regards on the measure of effect, quality and assessment of important outcomes for end users of the intervention (GRADE software, Version 3.6, 2011 update) [17]. Outcomes selected by the 2012 WHO Postpartum haemorrhage guidelines were used for assessing the quality of evidence generated by included studies [2].
Results
The electronic search strategy produced a total of 27 citations and additional four records were identified through other sources, such as personal communication with experts and reference lists review. Among the 31 records that had the titles and abstracts screened, 11 were excluded because were considered as clearly not relevant. Twenty full text articles were retrieved and assessed for eligibility. Fourteen studies were excluded because they reported on different analysis of the same data or because there was no comparison with standard treatment. Only six studies met the inclusion criteria of this systematic review, five observational studies (four before-after, one non-randomized clinical trial) and one cluster randomized trial (cRCT) [18-23]. There was no report on side effects of the intervention requiring treatment. Figure 1 shows the PRISMA flow diagram for the selection of eligible studies [12]. Table 1 presents the characteristics of included studies with risk of bias assessment of each study and Table 2 shows excluded studies (link to Tables 1 and 2). Pooled analysis proceeded for observational studies.
The five observational studies were considered as providing low quality evidence due to the study design and the cRCT was considered as providing moderate quality evidence (this study was downgraded due to imprecision of findings, few number of events occurred. The overall quality assessment is presented in the GRADE table (Table 3). All data pooled were from observational studies and a comparison was made with the result of the cRCT on reporting the effect of NASG use for treating postpartum haemorrhage.
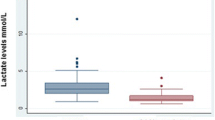
In Figure 2 the pooled analysis for measuring effect of NASG use to prevent maternal mortality is presented. A significant reduction of maternal deaths was seen with NASG use compared to standard treatment, with a pooled risk ratio (RR) and 95% confidence interval of 0.52 (95% CI: 0.36-0.77), five observational studies with NASG group: 1274 women and 46 maternal deaths; and standard care group: 1056 women and 72 maternal deaths. The cRCT showed a non-significant reduction in maternal death in favour of NASG use, RR 0.43 (95% CI: 0.14-1.33); NASG group: 405 women and 4 maternal deaths; and standard care group: 475 women and 11 maternal deaths.
In Figure 3 the outcome of interest was severe maternal complication. The pooled analyses of two observational studies showed a significant reduction on severe maternal outcomes occurrence showing benefit of NASG use, RR 0.31 (95% CI: 0.17 - 0.59), NASG group: 764 women and 13 cases of severe maternal outcomes; standard group: 590 women and 32 cases of severe maternal outcomes. A non-significant trend towards a beneficial effect of NASG use for severe maternal outcomes was also observed in the analysis of c-RCT, RR 0.38 (95% CI: 0.13-1.18); NASG group: 403 women and 4 cases of severe maternal outcomes; standard group: 465 women and 12 cases of severe maternal outcomes.
When NASG use was compared with standard care to prevent blood products transfusion no effect was shown, forest plot for 4 observational studies and for the c-RCT is presented in Figure 4. The pooled analysis of observational studies shows a RR of 0.99 (95% CI: 0.97-1.02); NASG group: 1069 women and 803 women receiving blood transfusion; standard group: 898 women and 623 women receiving blood transfusion. The RR from the c-RCT was 1.09 (95% CI: 0.92-1.28); NASG group: 398 women and 167 women receiving blood transfusion; standard group: 435 women and 168 women receiving blood transfusion.
Discussion
This systematic review reports on the effects of NASG use as part of PPH management. By systematically reviewing the available scientific evidence, we found that NASG may be able to temporarily mitigate the effects of blood loss after delivery. Among observational studies, NASG was associated with reductions in maternal mortality, compared to standard treatment. There were fewer maternal deaths in NASG group in the randomized controlled trial, but the results were not statistically significant. Despite maternal mortality globally is counted in great figures, at local level; in a health facility, it may represent a rare event. Severe maternal outcomes, such postpartum haemorrhage, blood products use, hypotension were used as proxies for maternal deaths. With maternal death proxies or the presence of any severe maternal complication used as outcome of interest in this systematic review, a similar pattern was observed supporting the trend towards beneficial effects associated with NASG use. However the use of this device did not show an association with reduction of blood transfusion, which suggests that NASG was able to prolong survival until definitive treatment and more resources, such as blood products, become available.
Our findings corroborate the theoretical basis for NASG use: once the systemic blood pressure is maintained in normal ranges for longer periods, progression in the organ dysfunction pathway (i.e. the sequence of blood loss, hypotension, hypovolemic shock, multiple organ failure and death) may be interrupted or delayed. An experimental study suggests a significant increase in internal iliac artery resistive index with NASG application in a small group of postpartum volunteers, which may provide a physiological explanation of how the NASG might reduce postpartum haemorrhage [24]. It should be noted that studies reporting on potential effects of an intervention on maternal mortality are very rare, which underlines the importance of this device and body of knowledge. NASG seems a promising device to be used in developing countries for preventing maternal deaths as it allows additional time of hemodynamic stability for referral and transfer to higher complexity level of facility. An important characteristic of the NASG is the easy use without need of major requirements or training personnel to be included in standard care for PPH. The device is a non-inflatable garment that produces circumferential pressure on the lower extremities and abdomen with no need of tubes, pumps, valves or gauges. The pressure is performed through the elasticity of the neoprene material maintained by the Velcro. The relatively low cost of this device, together with the possibility of reuse makes this device an attractive option for mitigating PPH effects (around USD 50 to 65 per unit) [8]. A cost-effectiveness assessment of NASG use in tertiary hospitals in Egypt and Nigeria found an important improvement in health outcomes at very low costs for treating severe haemorrhagic shock [25]. But it should also be noted that there are some complexities associated with NASG use. These include difficulties to ensure safe re-use (i.e. appropriate cleaning after use and the number of re-uses is possible without loss of compressibility); secure storage after use and availability at site of use of adequate size to fit to anthropometric variation of populations. Another limitation is that this intervention is not definitive: the need for substantive PPH treatment (such as uterotonics) remains.
This systematic review has some strengths and weaknesses that should be acknowledged. It used a comprehensive literature search strategy without limitation of language and databases and research authors were contacted for including unpublished data. Nevertheless, the retrieved evidence is dominated by observational studies, which rendered mostly evidence of low quality due to inherent research design limitations. Additional high quality studies are welcome to assess NASG use, particularly those performed by other research groups in different settings. All studies included in this systematic review were developed by the same research group, five in African countries and one in India. Diversification of scientific experience with NASG would contribute to explore efficacy, safety and applicability in different settings. Knowledge gaps that need to be addressed include the scalability and sustainability of this intervention and the impact that generalized use of NASG may have in strengthening the capacity of health systems to provide definitive PPH treatment. It could be a potential problem if countries prioritize investments in temporizing measures at the expense of more definitive PPH treatments. Other aspects that need to be addressed are related to the expansion of manufacture capacity for NASG and harmonization of clinical pathways to include NASG and with other temporizing measures.
Conclusion
NASG is a temporizing measure in PPH management potentially able to reduce PPH related deaths and severe morbidities. In settings where delays in PPH management are common, particularly where constraints to offer blood products and definitive treatment exist, use of NASG is an intervention that should be considered as policy option while the conditions for optimal PPH care are created. It is highly recommended that health programs adopting NASG implement a careful monitoring and evaluation strategy to assess the impact of NASG use in PPH management.
References
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–33.
WHO. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva Switzerland: World Health Organization Library; 2012. p. 48.
WHO. Evaluating the quality of care for severe pregnancy complications: The WHO near-miss approach for maternal health. Geneva, Switzerland: World Health Organization Library, 2011. p29.
Abdul-Kadir R, McLintock C, Ducloy AS, El-Refaey H, England A, Federici AB, et al. Evaluation and management of postpartum hemorrhage: consensus from an international expert panel. Transfusion. 2014;54(7):1756–68. doi:10.1111/trf.12550. Epub 2014 Mar 12.
Devine PC. Obstetric hemorrhage. Semin Perinatol. 2009;33(2):76–81.
LaBarre P. Non-pneumatic anti-shock garment. 2011. Acessed in: May 2014. Available at: http://www.who.int/medical_devices/innovation/new_emerging_tech_30.pdf
Hensleigh PA. Anti-shock garment provides resuscitation and haemostasis for obstetric haemorrhage. BJOG Int J Obstetrics Gynaecol. 2002;109(12):1377–84.
Brees C, Hensleigh PA, Miller S, Pelligra R. A non-inflatable anti-shock garment for obstetric hemorrhage. Int J Gynaecol Obstetrics. 2004;87(2):119–24.
El Ayadi A, Raifman S, Jega F, Butrick E, Ojo Y, Geller S, et al. Comorbidities and lack of blood transfusion may negatively affect maternal outcomes of women with obstetric hemorrhage treated with NASG. PLoS One. 2013;8(8):e70446.
El Ayadi AM, Butrick E, Geissler J, Miller S. Combined analysis of the non-pneumatic anti-shock garment on mortality from hypovolemic shock secondary to obstetric hemorrhage. BMC Pregnancy Childbirth. 2013;13:208. doi:10.1186/1471-2393-13-208.
Berdichevsky KTC, Martinez A, Miller S. Acceptance of a new technology for management of obstetric hemorrhage: a qualitative study from rural Mexico. Health Care Women Int. 2010;31(5):444–57. doi:10.1080/07399330903518491.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Stroup DFB JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, et al. Meta-analysis of Observational Studies in Epidemiology. A Proposal for Reporting. JAMA. 2000;283(15):2008–12. doi:10.1001/jama.283.15.2008.
Cochrane Collaboration. Suggested risk of bias criteria for EPOC reviews. 2013. Acessed in: May 2014. Available at: http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/Suggested%20risk%20of%20bias%20criteria%20for%20EPOC%20reviews.pdf
Campbell MK, Piaggio G, Elbourne DR, Altman DG, Group C. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Schünemann H BJ, Guyatt G, Oxman A (editors). GRADE handbook for grading quality of evidence and strength of recommendation. Version 3.6 [updated October 2011]. The GRADE Working Group, 2011. Available from http://www.gradepro.org/gradepro/. 2011.
Miller S, Hamza S, Bray EH, Lester F, Nada K, Gibson R, et al. First aid for obstetric haemorrhage: the pilot study of the non-pneumatic anti-shock garment in Egypt. BJOG Int J Obstetrics Gynaecol. 2006;113(4):424–9.
Miller S, Fathalla MM, Youssif MM, Turan J, Camlin C, Al-Hussaini TK, et al. A comparative study of the non-pneumatic anti-shock garment for the treatment of obstetric hemorrhage in Egypt. Int J Gynaecol Obstetrics Off Organ Int Federation Gynaecol Obstet. 2010;109(1):20–4.
Ojengbede OA, Morhason-Bello IO, Galadanci H, Meyer C, Nsima D, Camlin C, et al. Assessing the role of the non-pneumatic anti-shock garment in reducing mortality from postpartum hemorrhage in Nigeria. Gynecol Obstet Investig. 2011;71(1):66–72.
Magwali T, Butrick E, Mambo V, El Ayadi A, Lippman S, Bergel E, et al. Non-pneumatic anti-shock garment (NASG) for obstetric hemorrhage: Haraze, Zimbabwe. Int J Gynecol Obstet. 2010;119:S410.
Maknikar S, Nanda R, Miller S. NASG reduces mortality in indian women with PPH. Int J Gynecol Obstet. 2012;119(Supplement 3):S413.
Miller S, Bergel EF, El Ayadi AM, Gibbons L, Butrick EA, Magwali T, et al. Non-pneumatic anti-shock garment (NASG), a first-aid device to decrease maternal mortality from obstetric hemorrhage: a cluster randomized trial. PLoS One. 2013;8(10):e76477.
Lester F, Stenson A, Meyer C, Morris J, Vargas J, Miller S, et al. Impact of the Non-pneumatic Antishock Garment on pelvic blood flow in healthy postpartum women. Am J Obstet Gynecol. 2011;204:409.e1–5.
Sutherland T, Downing J, Miller S, Bishai DM, Butrick E, Fathalla MM, et al. Use of the non-pneumatic anti-shock garment (NASG) for life-threatening obstetric hemorrhage: a cost-effectiveness analysis in Egypt and Nigeria. PLoS One. 2013;8(4):e62282.
Acknowledgements
We thank Professor Suellen Miller for providing additional information on various studies and unpublished data.
Sources of funding
This systematic review was funded by UNDP-UNFPA-UNICEF-WHO World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Department of Reproductive Health and Research, WHO, Geneva, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
VNP carried out the literature search and conducted the first data extraction. JPS checked the extracted data. CPC decided on disagreements and checked quality assessment of the studies. VNP and CPC participated in the sequence alignment and drafted the manuscript. All authors contributed substantially to the final version of this review, read and approved the submission version of this manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Pileggi-Castro, C., Nogueira-Pileggi, V., Tunçalp, Ö. et al. Non-pneumatic anti-shock garment for improving maternal survival following severe postpartum haemorrhage: a systematic review. Reprod Health 12, 28 (2015). https://doi.org/10.1186/s12978-015-0012-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-015-0012-0