Abstract
Background
The association of lipoprotein(a) [Lp(a)] and stroke functional outcomes was conflicting. The aim of the study was to clarify whether high Lp(a) is associated with unfavorable functional outcomes in patients with ischemic stroke.
Methods
A total of 9709 individuals from the third China National Stroke Registry cohort were recruited. Plasma level of Lp(a) at admission was measured with enzyme-linked immunosorbent assay. The cut-off was set at the median for Lp(a). Functional outcome was assessed using the modified Rankin scale (mRS) at 3 months and 1 year after ischemic stroke. The association between Lp(a) and functional outcomes was evaluated using a logistic regression model.
Results
The median age was 63.0 years, and 31.1% participants were women. Patients in higher Lp(a) group had higher incidences of unfavorable functional outcomes at 3 months. In logistic regression model, elevated Lp(a) levels were associated with unfavorable functional outcomes at 3 months (Q4 vs. Q1: odds ratio 1.33, 95% confidence interval 1.11–1.61). Subgroup analysis showed that in the lower Lp-PLA2 group, Lp(a) level was not associated with functional outcomes, but in the higher Lp-PLA2 group, Lp(a) level was significantly associated with functional outcomes. After grouped by different levels of Lp(a) and Lp-PLA2, the Lp(a) high/ Lp-PLA2 high group showed the highest incidence of unfavorable functional outcomes at 3 months and 1 year.
Conclusions
Elevated Lp(a) level is associated with unfavorable functional outcomes in patients with ischemic stroke. The increment in both Lp(a) and Lp-PLA2 are associated with unfavorable functional outcomes at 3 months and 1 year after ischemic stroke.
Similar content being viewed by others
Background
Lipoprotein(a) [Lp(a)] is composed of low-density lipoprotein (LDL)-like particle and apolipoprotein B-100 (apoB), which is linked to apolipoprotein(a) [apo(a)] by disulfide bond. The pathogenic characteristics of Lp(a) include proinflammatory, proatherogenic, and prothrombotic. The pro-inflammatory of Lp(a) is partially mediated by oxidized phospholipids attached to apo(a) [1]. Lp(a) has attracted considerable attention because of its several large clinical genetic observation studies, which confirmed that plasma Lp(a) level is positively associated with increased risks of stroke, [2] myocardial infarction [3, 4], and aortic valve stenosis [1, 5, 6].
Inflammation is involved in the occurrence and development of unfavorable functional outcomes in patients with ischemic stroke [7]. Lipoprotein-associated phospholipase A2 [Lp-PLA2], an inflammatory marker, is an independent predictor of ischemic stroke and coronary heart disease [8, 9]. More importantly, Lp-PLA2 is intimately associated with Lp(a) in atherosclerosis and cardiovascular disease [10]. Although previous studies examined the association of Lp(a) with risk of unfavorable functional outcomes in patients with ischemic stroke [11,12,13], rare studies have conducted the association of Lp(a) and Lp-PLA2 levels to stroke functional outcomes.
In this study, we aimed to evaluate the hypothesis that a high level of Lp(a) is associated with unfavorable functional outcomes and Lp(a) high/Lp-PLA2 high have a significant association with unfavorable functional outcomes in patients with ischemic stroke from the third China National Stroke Registry (CNSR-III) database.
Methods
Study population
We used the CNSR-III, a nationwide, prospective, multicenter, observational registration study based on etiology, imaging, and biology markers from patients with ischemic stroke and transient ischemic attack (TIA) between August 2015 and March 2018 in China [14]. Specific information about the database has been described in detail in our previous studies. [14]. All patients were enrolled within 7 days after symptom onset. We included 9709 individuals with complete information on plasma Lp(a) measurements. According to the principles mentioned in the Declaration of Helsinki, the ethics committees of Beijing Tiantan Hospital and all other recruited participating centers approved the study protocol [15]. Written informed consent was obtained from all participants (or guardians of participants) in this study.
Baseline data collection
An electronic data capture system by face-to-face interviews was used to collect CNSR-III clinical baseline data. The subsequent data were gathered from the registry database, including age, sex, body mass index (BMI), and smoking status; medical history of hypertension, diabetes mellitus, hyperlipidemia and transient ischemic attack (TIA); systolic blood pressure (SBP), fasting plasma glucose (FPG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), high-sensitivity C-reactive protein (hsCRP), and lipoprotein-associated phospholipase A2 [Lp-PLA2]; stroke subtypes, classified as large artery atherosclerosis (LAA), cardioembolism (CE), small artery occlusion (SAO), other determined cause, or undetermined cause according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) criteria [16], and other determined cause and undetermined cause are defined as Others [17], discharge medication rate of Lipid-lowering drugs and antiplatelet drugs, and the National Institutes of Health Stroke Scale (NIHSS) score at admission.
Functional outcomes of stroke evaluation
The severity of ischemic stroke was evaluated using the NIHSS score at admission. Functional outcome was assessed with the modified Rankin scale (mRS) at 3 months and 1 year after stroke separately. The mRS scale ranges from 0 to 6. An mRS score of 0 was defined as no residual stroke symptoms; 5, severe disability; and 6, death. The mRS score of 0 to 2 points was defined as a favorable functional outcome, and mRS score of 3 to 6 points was defined as a unfavorable functional outcome [11, 12].
Laboratory analyses
Fasting blood specimens from 10,491 patients were collected using EDTA anticoagulation tubes within 1 day after admission and were centrifuged on-site within 2 h of collection to separate plasma for subsequent testing. Standard hospital assays were used on fresh plasma samples to measure plasma FPG, LDL-C, HDL-C, TG, hsCRP, and Lp-PLA2.
Lp(a) measurement
Lp(a) ELISA (Mercodia, Uppsala, Sweden) detects human Lp(a) and in terms of isoforms, is size-independent in terms of the kringle IV type 2 domain. The Mercodia ELISA is a solid phase two-site enzyme immunoassay and include a 5-point calibrator. The coefficient of variation (CV) was 7%.
Statistical analyses
For displaying the information of the Lp(a) and functional outcomes more detailed, the Lp(a) quartiles were used for baseline characteristics classification and comparison. Furthermore, the cut-off was set at the median for Lp(a). Data on basic characteristics were presented as medians (interquartile ranges) for continuous variables. Categorical variables were presented as percentages. Nonparametric Wilcoxon test was used for comparisons of continuous variables, and chi-square test was used for comparisons of categorical variables among multiple groups. The associations of Lp(a) with mRS at 3 months and 1 year were examined using a logistic regression model. We adjusted the potential confounders measured at baseline in the analysis. The model was adjusted for age, sex, BMI, diabetes mellitus, LDL-C, HDL-C, TG, Lp-PLA2, TOAST subtype, and NIHSS score at admission. The strength of the associations was demonstrated using odds ratios (ORs) with 95% confidence intervals (CIs). The sensitivity analysis was used to rule out the effects of recurrence on the association between the levels of Lp(a) and outcomes at 3 months. Two-sided p < 0.05 was considered to be statistically significant. The above statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina).
Results
In brief, a total of 15,166 consecutive patients from 201 sites were recruited, among which 93.3% with ischemic stroke (n = 14,146) and 6.7% with TIA (n = 1020), According to the inclusion criteria, 1020 TIA patients were excluded from 15,166 patients. A total of 10,491 ischemic stroke patients’ blood samples were collected and examined at the laboratory, of which 664 patients lack of Lp(a) data and 118 patients lack of functional outcomes were excluded, and a total of 9709 patients were included in the study (Additional file 1: Figure S1). In Additional file 1: Table S1, the comparison of the included and excluded patients is shown. Compared with the excluded patients, the included patients tended to be older and had higher Lp-PLA2, and higher discharge medication rates of Lipid-lowering drugs and antiplatelet drugs.
Baseline characteristics
Table 1 shows the baseline characteristics of the 9709 individuals stratified by Quartiles of baseline plasma Lp(a) levels. With the increment in plasma Lp(a) levels, patients tended to be older and had lower levels of BMI, FPG and TG, a higher proportion of LAA, and higher LDL-C, HDL-C, hsCRP, and Lp-PLA2.
Association between the levels of Lp(a) and functional outcomes at 3 months and 1 year
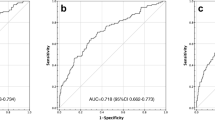
Additional file 1: Figure S2 demonstrates a positive association between the levels of Lp(a) and functional outcomes of stroke at 3 months. In the unadjusted model, elevated levels of Lp(a) were positively associated with the unfavorable functional outcomes of stroke as evaluated using mRS score ≥ 3 at 3 months [Quartile 4 vs. Quartile 1, OR 1.58, 95% CI 1.34–1.86, p < 0.0001] (Table 2). Furthermore, elevated Lp(a) levels were significantly associated with the unfavorable functional outcomes of stroke as evaluated by mRS score ≥ 3 at 1 year [Quartile 4 vs. Quartile 1, OR 1.46, 95% CI 1.23–1.72, p < 0.0001]. After adjustment for age, sex, BMI, diabetes mellitus, LDL-C, HDL-C, TG, Lp-PLA2, TOAST subtype, and NIHSS score at admission, similar results were observed. Elevated levels of Lp(a) were positively associated with the unfavorable functional outcomes of stroke as evaluated by mRS score ≥ 3 at 3 months [Quartile 4 vs. Quartile 1, OR 1.33, 95% CI 1.11–1.61, p < 0.0001] and at 1 year [Quartile 4 vs. Quartile 1, OR 1.25, 95% CI 1.04–1.51, p < 0.0001]. Distribution of mRS scores at 3 months according to Lp(a) levels showed similar trends (Fig. 1).
Subgroup analysis for the association between Lp(a) levels and mRS ≥ 3 at 3 months and 1 year
Figure 2 shows that in the lower Lp-PLA2 group, Lp(a) level was not associated with functional outcomes, but in the higher Lp-PLA2 group, Lp(a) level was significantly associated with functional outcomes. We then used Lp-PLA2 for subgroup analysis to further evaluate the association between Lp(a) levels and functional outcomes of stroke assessed using mRS ≥ 3 at 3 months and 1 year.
Forest plot of subgroup analysis for the association between Lp(a) levels and mRS ≥ 3 at 3 months. The cut-off of continuous variable was the median value except for hsCRP. NIHSS: National Institutes of Health Stroke Scale; LAA: large-artery atherosclerosis; CE: cardioembolism; SAO: small artery occlusion; TPA: tissue plasminogen activator; hsCRP: high-sensitivity C-reactive protein; Lp-PLA2: lipoprotein-associated phospholipase A2
Association of functional outcomes grouped by different levels of Lp(a) and Lp-PLA2
Table 3 shows the association of functional outcomes grouped by different levels of Lp(a) and Lp-PLA2 (< median value vs. ≥ median value). Compared with Lp(a) low/ Lp-PLA2 low group, patients with Lp(a) high/ Lp-PLA2 high group showed a significant association with unfavorable functional outcomes at 3 months (OR 1.21, 95% CI 1.01–1.46) and 1 year (OR 1.25, 95% CI 1.03–1.51) after ischemic stroke.
Sensitivity analysis
Association between the levels of Lp(a) and functional outcomes at 3 months after removing patients with recurrent stroke
To rule out the effect of recurrence on the association between the levels of Lp(a) and functional outcomes at 3 months, we excluded the 3 months recurrent stroke population for further analysis. As shown in Additional file 1: Table S2, in the unadjusted model, elevated levels of Lp(a) were positively associated with the unfavorable functional outcomes of stroke as evaluated by mRS score ≥ 3 at 3 months. After adjustment for age, sex, BMI, diabetes mellitus, LDL-C, HDL-C, TG, Lp-PLA2, TOAST subtype, and NIHSS score at admission, similar results were observed. Elevated levels of Lp(a) were positively associated with the unfavorable functional outcomes of stroke as evaluated by mRS score ≥ 3 at 3 months.
Discussion
In the CNSR-III cohort study, we investigated the association between plasma Lp(a) levels and the functional outcomes of ischemic stroke. The results demonstrated a positive association between the levels of Lp(a) and functional outcomes evaluated by mRS at 3 months and 1 year after stroke. The association remained after excluding patients with recurrence of stroke at 3 months. More importantly, compared with Lp(a) low/ Lp-PLA2 low group, patients with Lp(a) high/ Lp-PLA2 high group showed a significant association with unfavorable functional outcomes at 3 months and 1 year after ischemic stroke.
In recent years, several small clinical studies have demonstrated that elevated Lp(a) levels are positively associated with unfavorable functional outcomes in patients with ischemic stroke. In a clinical study by Wang et al. who included 232 consecutive patients with an acute ischemic stroke diagnosis complicated with type 2 diabetes, higher Lp(a) levels at admission are associated with increased risk of unfavorable functional outcomes at 3 months according to mRS scores [11]. Similarly, in a study conducted by Wang et al., who investigated 153 patients with acute ischemic stroke and 120 controls, an increased risk of unfavorable functional outcomes was associated with Lp(a) levels [12]. In another study that recruited 100 consecutive patients with acute ischemic stroke and 120 controls, a positive association is suggested between Lp(a) levels and poorer long-term prognosis of stroke [18]. By contrast, Kooten et al. failed to find any association of stroke prognosis with Lp(a) levels [13]. The association of stroke prognosis with Lp(a) level remains unclear. Therefore, a large sample cohort study is warranted to further clarify the association of ischemic stroke prognosis with Lp(a) levels. The current results demonstrated a positive association between the levels of Lp(a) and functional outcomes evaluated by mRS at 3 months and 1 year after stroke. To remove the effect of stroke recurrence on the conclusion, we further analyzed the association between Lp(a) levels and functional outcomes after excluding patients with stroke recurrence at 3 months, the association still existed. Our study confirmed a positive association between plasma Lp(a) levels and functional outcomes at 3 months and 1 year after ischemic stroke.
The mechanism through which Lp(a) levels are associated with functional outcomes of ischemic stroke remains unclear until now. Inflammation runs through the onset, process, and progression of acute ischemic stroke. In acute ischemic stroke, inflammatory cascade affects functional outcomes [7]. Our study revealed that the increment in both Lp(a) and Lp-PLA2 are associated with unfavorable functional outcomes at 3 months and 1 year after ischemic stroke. The pathogenic effect of Lp(a) is partly due to its pro-inflammatory effect, which is harmful to the progression of ischemic stroke. The pro-inflammatory effect including endothelial inflammation is mediated partially by its oxidized phospholipid (OxPL) content [19]. As a pro-inflammatory indicator, Lp-PLA2 is mainly expressed on the surface of inflammatory cells enriched in plaques, and it promotes the secretion of inflammatory mediators by degrading OxPL to cause endothelial dysfunction [20]. Endothelial dysfunction is associated with unfavorable functional outcomes of ischemic stroke [21, 22]. In addition, observational studies have shown plausible mechanisms through which Lp(a)–Lp-PLA2–OxPL may mediate atherosclerosis and cardiovascular disease [10, 23]. In summary, we speculate that Lp(a) may aggravates the inflammation mediated by Lp-PLA2, leading to endothelial dysfunction and unfavorable functional outcomes of ischemic stroke.
The present study is the largest by far to evaluate the clear association between plasma Lp(a) levels and functional outcomes after ischemic stroke. However, it has several limitations. First, we only measured Lp(a) at admission, and no serial measurement of Lp(a) levels was performed. For this reason, we could not conclude any causal relationship of functional outcomes with high Lp(a) levels. We only demonstrated a positive association of unfavorable functional outcomes after ischemic stroke with high Lp(a) levels. Second, the study samples comprised Chinese individuals, limiting the application of its conclusions to other races and populations. Third, genetic data were lacking because of the observational nature of the study. Future studies are warranted to further investigate the effect of these factors on Lp(a) and functional outcomes in patients with ischemic stroke.
Conclusions
Elevated Lp(a) level is associated with unfavorable functional outcomes evaluated by mRS at 3 months and 1 year after ischemic stroke. The increment in both Lp(a) and Lp-PLA2 are associated with unfavorable functional outcomes at 3 months and 1 year after ischemic stroke. Further studies should be carried out regarding the inflammation mechanism between increased Lp(a) levels and unfavorable functional outcomes in patients with ischemic stroke.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- Lp(a):
-
Lipoprotein(a)
- CNSR-III:
-
The third China National Stroke Registry
- mRS:
-
The modified Rankin scale
- NIHSS:
-
The National Institutes of Health Stroke Scale
- TIA:
-
Transient ischemic attack
- BMI:
-
Body mass index
- TOAST:
-
Trial of ORG 10172 in Acute Stroke Treatment
- LAA:
-
Large artery atherosclerosis
- SAO:
-
Small artery occlusion
- CE:
-
Cardioembolism
- SBP:
-
Systolic blood pressure
- FPG:
-
Fasting plasma glucose
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglyceride
- hsCRP:
-
High-sensitivity C-reactive protein
- Lp-PLA2 :
-
Lipoprotein-associated phospholipase A2
References
Nordestgaard BG, Langsted A. Lipoprotein (a) as a cause of cardiovascular disease: insights from epidemiology, genetics, and biology. J Lipid Res. 2016;57:1953–75.
Langsted A, Nordestgaard BG, Kamstrup PR. Elevated Lipoprotein(a) and Risk of Ischemic Stroke. J Am Coll Cardiol. 2019;74:54–66.
Clarke R, Peden JF, Hopewell JC, Kyriakou T, Goel A, Heath SC, Parish S, Barlera S, Franzosi MG, Rust S, Bennett D, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009;361:2518–28.
Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301:2331–9.
Kamstrup PR, Tybjaerg-Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol. 2014;63:470–7.
Bouchareb R, Mahmut A, Nsaibia MJ, Boulanger MC, Dahou A, Lepine JL, Laflamme MH, Hadji F, Couture C, Trahan S, et al. Autotaxin derived from lipoprotein(a) and valve interstitial cells promotes inflammation and mineralization of the aortic valve. Circulation. 2015;132:677–90.
Fu Y, Liu Q, Anrather J, Shi FD. Immune interventions in stroke. Nat Rev Neurol. 2015;11:524–35.
Oei HH, van der Meer IM, Hofman A, Koudstaal PJ, Stijnen T, Breteler MM, Witteman JC. Lipoprotein-associated phospholipase A2 activity is associated with risk of coronary heart disease and ischemic stroke: the Rotterdam Study. Circulation. 2005;111:570–5.
Lp PL, Thompson A, Gao P, Orfei L, Watson S, Di Angelantonio E, Kaptoge S, Ballantyne C, Cannon CP, Criqui M, et al. Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet. 2010;375:1536–44.
Tsimikas S, Tsironis LD, Tselepis AD. New insights into the role of lipoprotein(a)-associated lipoprotein-associated phospholipase A2 in atherosclerosis and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2007;27:2094–9.
Wang H, Zhao J, Gui Y, Yan H, Yan Z, Zhang P, Liu L, Chang L, Zhang J. Elevated lipoprotein (a) and risk of poor functional outcome in Chinese patients with ischemic stroke and type 2 diabetes. Neurotox Res. 2018;33:868–75.
Zhang W, Zhang XA. Prognostic value of serum lipoprotein(a) levels in patients with acute ischemic stroke. NeuroReport. 2014;25:262–6.
van Kooten F, van Krimpen J, Dippel DW, Hoogerbrugge N, Koudstaal PJ. Lipoprotein(a) in patients with acute cerebral ischemia. Stroke. 1996;27:1231–5.
Wang Y, Jing J, Meng X, Pan Y, Wang Y, Zhao X, Lin J, Li W, Jiang Y, Li Z, et al. The Third China National Stroke Registry (CNSR-III) for patients with acute ischaemic stroke or transient ischaemic attack: design, rationale and baseline patient characteristics. Stroke Vasc Neurol. 2019;4:158–64.
Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, Wang C, Li H, Meng X, Cui L, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11–9.
Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41.
Xu J, Cheng A, Song B, Zhao M, Xue J, Wang A, Dai L, Jing J, Meng X, Li H, Zheng L, Wang Y. Trimethylamine N-oxide and stroke recurrence depends on ischemic stroke subtypes. Stroke. 2021. https://doi.org/10.1161/STROKEAHA.120.031443.
Chakraborty B, Vishnoi G, Goswami B, Gowda SH, Chowdhury D, Agarwal S. Lipoprotein(a), ferritin, and albumin in acute phase reaction predicts severity and mortality of acute ischemic stroke in North Indian Patients. J Stroke Cerebrovasc Dis. 2013;22:e159-167.
Schnitzler JG, Hoogeveen RM, Ali L, Prange KHM, Waissi F, van Weeghel M, Bachmann JC, Versloot M, Borrelli MJ, Yeang C, et al. Atherogenic lipoprotein(a) increases vascular glycolysis, thereby facilitating inflammation and leukocyte extravasation. Circ Res. 2020;126:1346–59.
Thompson A, Gao P, Orfei L, Watson S, Di Angelantonio E, Kaptoge S, Ballantyne C, Cannon C, Criqui M, Cushman M, et al. Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet (London, England). 2010;375:1536–44.
Hoffmann CJ, Harms U, Rex A, Szulzewsky F, Wolf SA, Grittner U, Lattig-Tunnemann G, Sendtner M, Kettenmann H, Dirnagl U, et al. Vascular signal transducer and activator of transcription-3 promotes angiogenesis and neuroplasticity long-term after stroke. Circulation. 2015;131:1772–82.
Fan Y, Shen F, Frenzel T, Zhu W, Ye J, Liu J, Chen Y, Su H, Young WL, Yang GY. Endothelial progenitor cell transplantation improves long-term stroke outcome in mice. Ann Neurol. 2010;67:488–97.
Hung MY, Witztum JL, Tsimikas S. New therapeutic targets for calcific aortic valve stenosis: the lipoprotein(a)-lipoprotein-associated phospholipase A2-oxidized phospholipid axis. J Am Coll Cardiol. 2014;63:478–80.
Acknowledgements
Not applicable.
Funding
This work was supported by Grants from the capital health research and development of special (2020-2Z-20411), National Key R&D Program of China (2016YFC0901002, 2017YFC1310901, 2018YFC1312903), Beijing Municipal Science & Technology Commission (D171100003017002), National Science and Technology Major Project (2017ZX09304018), National Natural Science Foundation of China (81970425, 81770272), China National Key R&D Program (2020YFA0803700), China Postdoctoral Science Foundation (2021M692248), Beijing Postdoctoral Research Foundation (2021-ZZ-020).
Author information
Authors and Affiliations
Contributions
YJW, and LMZ contributed to the conception and design of the study. All authors (YJW, LMZ, XJ, JX, XWH, JX, KL, AMJ, JXL, and XM) contributed to the acquisition and analysis of data. XJ, YJW, and LMZ contributed to drafting the text, preparing the tables and figures. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
According to the principles mentioned in the Declaration of Helsinki, the ethics committees of Beijing Tiantan Hospital and all other recruited participating centers approved the study protocol. Written informed consent was obtained from all participants (or guardians of participants) in this study.
Consent for publication
All authors have approved this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table S1. Comparisons of Baseline characteristics between included patients and excluded patients. Table S2. Association between the levels of Lp(a) and functional outcomes at 3 months after excluding stroke recurrence. Table S3. Association between the Lp-PLA2 and functional outcomes at 3 months and 1 year. Table S4. Association between the levels of Lp(a) and functional outcomes at 3 months and 1 year. Table S5. Comparisons of Baseline characteristics between included patients and excluded patients. Table S6. Association between the levels of Lp(a) and functional outcomes at 3 months and 1 year. Table S7. Association of functional outcomes grouped by different levels of Lp(a) and Lp-PLA2. Figure S1. Flowchart of patients’ inclusion analysis strategy. Figure S2. The association between the levels of Lp(a) and outcomes at 3 months. Figure S3. The association of Lp(a) and functional outcomes in patients with ischemic stroke at 3 months and 1 year.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, X., Xu, J., Hao, X. et al. Elevated lipoprotein(a) and lipoprotein-associated phospholipase A2 are associated with unfavorable functional outcomes in patients with ischemic stroke. J Neuroinflammation 18, 307 (2021). https://doi.org/10.1186/s12974-021-02359-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-021-02359-w