Abstract
Background
Glaucoma is a complex, multifactorial disease where apoptosis, microglia activation, and inflammation have been linked to the death of retinal ganglion cells (RGCs) and axon degeneration. We demonstrated previously that FasL-Fas signaling was required for axon degeneration and death of RGCs in chronic and inducible mouse models of glaucoma and that Fas activation triggered RGC apoptosis, glial activation, and inflammation. Here, we investigated whether targeting the Fas receptor with a small peptide antagonist, ONL1204, has anti-inflammatory and neuroprotective effects in a microbead-induced mouse model of glaucoma.
Methods
Intracameral injection of microbeads was used to elevate intraocular pressure (IOP) in Fas-deficient (Faslpr) mice and WT C57BL/6J mice that received an intravitreal injection of the Fas inhibitor, ONL1204 (2 μg/1 μl) (or vehicle only), on day 0 or day 7 after microbead injection. The IOP was monitored by rebound tonometry, and at 28 days post-microbead injection, Brn3a-stained RGCs and paraphenylenediamine (PPD)-stained axons were analyzed. The effects of ONL1204 on retinal microglia activation and the expression of inflammatory genes were analyzed by immunostaining of retinal flatmounts and quantitative PCR (qPCR).
Results
Rebound tonometry showed equivalent elevation of IOP in all groups of microbead-injected mice. At 28 days post-microbead injection, the RGC and axon counts from microbead-injected Faslpr mice were equivalent to saline-injected (no IOP elevation) controls. Treatment with ONL1204 also significantly reduced RGC death and loss of axons in microbead-injected WT mice when compared to vehicle-treated controls, even when administered after IOP elevation. Confocal analysis of Iba1-stained retinal flatmounts and qPCR demonstrated that ONL1204 also abrogated microglia activation and inhibited the induction of multiple genes implicated in glaucoma, including cytokines and chemokines (GFAP, Caspase-8, TNFα, IL-1β, IL-6, IL-18, MIP-1α, MIP-1β, MIP-2, MCPI, and IP10), components of the complement cascade (C3, C1Q), Toll-like receptor pathway (TLR4), and inflammasome pathway (NLRP3).
Conclusions
These results serve as proof-of-principal that the small peptide inhibitor of the Fas receptor, ONL1204, can provide robust neuroprotection in an inducible mouse model of glaucoma, even when administered after IOP elevation. Moreover, Fas signaling contributes to the pathogenesis of glaucoma through activation of both apoptotic and inflammatory pathways.
Similar content being viewed by others
Background
Glaucoma is the leading cause of irreversible blindness worldwide, characterized by the progressive loss of retinal ganglion cells (RGCs). A recent study estimates that approximately 60 million people worldwide currently suffer from glaucoma, and with the rapidly growing aging population, this number is predicted to exceed 100 million by 2040 [1]. Elevated intraocular pressure (IOP) is a major risk factor for the development of glaucoma, and lowering IOP remains the only treatment for this disease [2]. However, the continued progression of the disease in some patients despite successful reduction of IOP [3], combined with the increasing incidence of normal-tension glaucoma [4, 5] and the absence of neurodegeneration in some patients with elevated IOP [6], indicates that IOP-independent mechanisms contribute to the initiation and progression of glaucoma. Therefore, a current priority in the glaucoma field is to further define the molecular mechanisms of RGC death and axon degeneration in order to develop IOP-independent therapeutic treatment strategies to halt disease progression and preserve vision.
There is substantial evidence that apoptosis of RGCs is the final common pathway in both human and experimental models of glaucoma [7,8,9,10]. However, using the DBA/2J mouse model of spontaneous glaucoma, Libby et al. demonstrated that genetic ablation of the proapoptotic molecule BCL2-associated X protein (BAX) prevents apoptosis of RGCs, but does not prevent axon degeneration [11]. Similarly, McKinnon et al. demonstrated that gene therapy with a potent caspase inhibitor, baculoviral IAP repeat-containing protein-4 (BIRC4), only protects about 50% of the RGCs and optic nerve axons in a rodent model of elevated IOP [12]. Therefore, while RGC apoptosis is the common endpoint in glaucoma, therapeutic approaches that only target the apoptotic pathway in RGCs do not completely prevent glaucomatous neurodegeneration.
Glaucoma is a complex multifactorial disease, and while the exact molecular mechanisms of RGC apoptosis are not completely understood, there is growing evidence that suggests microglia activation and neuroinflammation play a central role in both early and late stages of glaucomatous neurodegeneration [13,14,15,16]. In human and experimental models of glaucoma, activated microglia are detected in the optic nerve head (ONH) and retina [14,15,16,17,18,19] and the extent of microglia activation correlates with the extent of neurodegeneration [20, 21]. Moreover, blocking microglia activation with minocycline [14, 20] or anti-TNFα [22, 23] prevents the infiltration of immune cells and significantly reduces axon degeneration and death of RGCs in experimental models of glaucoma. Together, these data suggest that activated microglia are the driving force behind glaucomatous neurodegeneration. However, the molecular mechanism(s) that mediate microglia reactivity in glaucoma are not well understood.
Fas ligand (FasL) is a type II transmembrane protein of the TNF family, which is best known for its ability to induce apoptosis upon binding to the Fas receptor [24,25,26,27]. However, we demonstrated that within the eye, FasL can be expressed as a membrane-bound protein (mFasL), which is pro-apoptotic and pro-inflammatory, or it can be cleaved and released as a soluble isoform (sFasL), which is non-apoptotic and non-inflammatory [28,29,30]. In the normal immune-privileged eye, where inflammation is tightly regulated, FasL is primarily expressed as the non-apoptotic, non-inflammatory sFasL [31]. However, in the DBA/2J mouse model of glaucoma, a shift in the expression of FasL from the soluble form to the proapoptotic and proinflammatory membrane form coincides with the loss of immune privilege and the development of glaucoma [31, 32]. These data suggest mFasL activation of the Fas receptor plays a central role in the pathogenesis of glaucoma. Moreover, treating mice with sFasL, via intravitreal adeno-associated virus-mediated gene delivery, provided significant neuroprotection of RGCs and axons, and this protection correlated with inhibition of retinal glial activation and the induction of the proinflammatory mediators [31]. These data demonstrate that blocking mFasL activation of the Fas receptor inhibits three hallmarks of glaucomatous degeneration: microglia activation, inflammation, and apoptosis. Therefore, we hypothesized that specifically blocking the Fas receptor with a small peptide inhibitor could serve as a novel neuroprotective approach in the treatment of glaucoma.
When developing a small peptide inhibitor of Fas, we first looked into the reports that Met, a growth factor receptor tyrosine kinase, could directly bind to and sequester the Fas receptor in hepatocytes [33]. This sequestration of the Fas receptor prevents Fas activation and subsequent apoptosis, identifying Met as an inhibitor of the Fas pathway. Using this information, we developed Met12, which is a small peptide that inhibits Fas-induced caspase-8 activation in the 661W photoreceptor cell line [34], for ocular use. In vivo, Met12 significantly inhibited photoreceptor apoptosis in a mouse model of retinal detachment [34]. More recently, we demonstrated that Met12 also inhibits Fas activation and subsequent apoptosis of photoreceptors and RPE in a sodium iodate-induced mouse model of retinal degeneration [35]. Together, these studies demonstrate that Met12 can be used in vivo to inhibit Fas-mediated apoptosis in models of retinal injury and degeneration.
Herein, we used a well-defined microbead-induced mouse model of elevated IOP to (i) examine the ability of a new derivative of Met12, ONL1204, to protect RGCs and prevent axon degeneration, and (ii) test the hypothesis that the Fas signaling pathway mediates microglia activation and the induction of neurodestructive inflammation in glaucoma. Our results demonstrate that a single intravitreal administration of the Fas inhibitor, ONL1204, significantly reduced RGC death and axon degeneration, even when administered after elevated IOP. Moreover, the neuroprotection correlated with significant inhibition of retinal microglia activation and inflammatory genes expression, suggesting that Fas signaling contributes to the pathogenesis of glaucoma through both apoptotic and inflammatory pathways. Together, these data underscore the value of targeting Fas in glaucoma and provide proof-of-principal that the small peptide inhibitor of the Fas receptor, ONL1204, can provide robust neuroprotection in an inducible mouse model of glaucoma, even when administered after elevated IOP.
Materials and methods
Animals
All animal experiments were approved by the Institutional Animal Care and Use Committee at Schepens Eye Research Institute and were performed under the guidelines of the Association of Research in Vision and Ophthalmology (Rockville, MD). The 8-week-old C57BL/6J WT mice (Stock No: 000664) and B6.MRL-Faslpr/J Fas receptor-deficient mice (Stock No: 000482) were purchased from Jackson Laboratories (Bar Harbor, ME) and housed and maintained under cyclic light (12 L-30 lux: 12D) conditions in an AAALAC-approved animal facility at the Schepens Eye Research Institute. To avoid sex bias, equal numbers of male and female mice were included in each experimental group.
Microbead-induced model of elevated IOP
Mice were anesthetized by intraperitoneal injection of a mixture of ketamine (100 mg/kg; Ketaset; Fort Dodge Animal Health, Fort Dodge, IA) and xylazine (9 mg/kg; TranquiVed; Vedco, Inc., St. Joseph, MO) supplemented by topical application of proparacaine (0.5%; Bausch & Lomb, Tampa, FL). Elevation of IOP was induced unilaterally by injection of polystyrene microbeads (FluoSpheres; Invitrogen, Carlsbad, CA; 15-μm diameter) into the anterior chamber of the right eye of each animal under a surgical microscope, as previously reported [31]. Briefly, microbeads were prepared at a concentration of 5.0 × 106 beads/ml in sterile physiologic saline. The right cornea was gently punctured near the center using a sharp glass micropipette (World Precision Instruments Inc., Sarasota, FL). A small volume (2 μL) of microbeads was injected through this preformed hole into the anterior chamber followed by injection of an air bubble via the micropipette connected with a Hamilton syringe. Any mice that developed signs of inflammation (clouding of the cornea, edematous cornea, etc.) were excluded from the study.
IOP measurements
IOP was measured with a rebound TonoLab tonometer (Colonial Medical Supply, Espoo, Finland), as previously described [31, 33]. Mice were anesthetized by 3% isoflurane in 100% oxygen (induction) followed by 1.5% isoflurane in 100% oxygen (maintenance) delivered with a precision vaporizer. IOP measurement was initiated within 2 to 3 min after animals lost toe pinch reflex or tail pinch response. Anesthetized mice were placed on a platform, and the tip of the pressure sensor was placed approximately 1/8 in. from the central cornea. Average IOP was displayed automatically after six measurements after elimination of the highest and lowest values. This machine-generated mean was considered as one reading, and six readings were obtained for each eye. All IOPs were taken at the same time of day (between 10:00 and 12:00 h) due to the variation of IOP throughout the day.
Intravitreal injections
The intravitreal injections, just posterior to the limbus and parallel to the conjunctival vessels, were performed as previously described [31, 36]. Mice received a 1-μl intravitreal injection containing ONL1204 (2 mg/ml) or vehicle control on day 0 (just prior to injection of microbeads) or day 7 after microbeads injection.
Quantification of optic nerve axons
For quantification of axons, optic nerves were dissected and fixed in Karnovsky’s reagent (50% in phosphate buffer) overnight. Semi-thin cross-sections of the nerve were taken at 1.0 mm posterior to the globe and stained with 1% p-phenylenediamine (PPD) for evaluation by light microscopy. Ten non-overlapping photomicrographs were taken at × 100 magnification covering the entire area of the optic nerve cross-section. Using ImageJ software, a 50 μM × 50 μM square was placed on each × 100 image and all axons within the square (0.0025 mm2) were counted using the threshold and analyze particles function in image J as previously described [31]. The average axon counts in the 10 images were used to calculate the axon density per square millimeter of the optic nerve (ON). Individuals blinded to the experimental groups performed all axon counts.
Immunohistochemistry-retinal flat mount
Immediately following euthanasia, eyes were enucleated and fixed in 4% paraformaldehyde for 2 h at room temperature. The retina was detached from the eyecup, and four radial incisions reaching approximately 2/3 of the radius of the retina were made to create a butterfly shape. Retinal flatmounts were washed with PBS/T (0.1% Triton X-100) and permeabilized with 0.1% Triton X-100 in 20% superblock blocking buffer (2 ml superblock (Thermo Fisher cat no- 37580) + 8 ml PBS/T + 10μl Triton X) for 30 min at room temperature. Following permeabilization, the retinas were blocked in blocking solution (20% superblock + 10% goat serum) for 1 h at room temperature. Retinas were then incubated at 4 °C overnight with a primary Ab against Brn3a, a RGC-specific marker (Millipore Cat no- 1585, Billerica, MA), or against Iba1, a microglia/macrophage marker (Wako, Chemicals USA, Inc. Cat# 019-19741). An Alexa Fluor 555—conjugated for Brn3a— and Alexa Fluor 488—conjugated for IBA1 (Invitrogen)—was used as secondary Ab. Nuclei were counterstained with DAPI (vector stain).
Quantification of retinal ganglion cells
To quantitate retinal ganglion cells, × 60 oil immersion was used and 16 non-overlapping images were taken (4–5 images per quadrant) using the × 60 oil immersion objective of Leica TCS SP5 confocal microscope system. All Brn3a-stained RGCs were quantitated using an automated counting platform we previously developed using CellProfiler software [37]. ImageJ software was used to calculate the area of each image, and the average number of RGCs in the 16 images was used to calculate the RGC density per square millimeter of retina. Individuals blinded to the experimental groups performed all RGC counts.
Quantification of retinal microglia
To quantitate Iba1+ microglia/macrophages, image stacks of retinal flatmounts were acquired using the × 20 oil immersion objective (zoom 1.7, 35 μm depth (includes GCL and IPL)) of the Leica TCS SP5 confocal microscope system. The retina was divided into four quadrants, and one mid-peripheral region was imaged per quadrant for a total of four images per retina (480 μm by 480 μm per region). Microglial cells were counted manually by an individual blinded to the treatment groups using ImageJ software as previously described [38]. The longest cell process length, which is a marker of cell quiescence, was used as a morphometric descriptor to analyze microglia activation using NeruonJ Fiji Plugin as previously described [39]. Individuals blinded to the experimental groups performed all microglia quantification.
Quantitative RT-PCR
RNA was isolated from the neural retina using a QIAGEN RNeasy Mini Kit (catalog number 74104), according to the manufacturer’s protocol. RNA was treated with DNase (catalog number AM222; Invitrogen) to ensure no contamination of genomic DNA. A total of 500 ng of RNA was reverse-transcribed (Thermo fisher Cat no 11756050 Superscript IV VILO master mix) according to the manufacturer’s instructions. cDNA was diluted 1:4 and then used for each amplification reaction. cDNA was treated with RNase H (18021-014; Invitrogen) to ensure the absence of ssRNA. Quantitative PCR (qPCR) reactions were performed in a 10 μl total volume using the FastStart Universal SYBR Green Master (Rox) (4913914001; Sigma) according to the manufacturer’s protocol. PCR cycles consisted of a denaturation step at 95 °C for 10 min, followed by 50 cycles of 95 °C for 15 s and 60 °C for 60 s. Each sample was subjected to melting curve analysis to confirm amplification specificity. Samples were run in duplicate, and each experiment included nontemplate control wells. Samples were normalized to house-keeping genes and expressed as the relative expression using the δ-delta Ct method. Relative expression to two house-keeping genes β2 microglobulin and PPIA was quantified using the formula: relative expression δ-delta CT = 2^(avg. gene cT−avg. saline-treated cT). Fold changes were calculated with respect to saline-injected control eyes. All of the primers used are listed in Table 1.
Survival assay
The ability of ONL1204 to inhibit FasL-mediated apoptosis of murine A20 B lymphoma cells was evaluated in vitro. Microvesicle preparations were isolated from transfected Neuro2a cells that expressed either murine mFasL (mFasL VP) or the vector control (Neo VP) as described previously [40]. A20 lymphoma cells were incubated for 4 h with titrations of ONL 1204 or the vehicle control together with a 1:100 dilution of either mFasL VP or Neo VP and then cultured overnight in the presence of 3H-thymidine. Survival was assessed by 3H-thymidine incorporation using the formula (cpm of mFasL VP + ONL1204 or vehicle)/cpm Neo VP + ONL1204 or vehicle).
Statistics
Graph Pad Prism 8 (La Jolla, CA, USA) was used to perform statistical analysis of the data. For the A20 in vitro study, one-way ANOVA and Dunnett’s multiple comparisons test were used to compare different treatment groups. One-way ANOVA and Dunnett’s multiple comparisons test were used for RGC, axon, microglia, and qPCR analyses. Two-way ANOVA and Dunnett’s multiple comparisons test were used for all IOP comparisons. A P value of less than 0.05 was considered significant.
Results
ONL1204 blocks FasL-induced apoptosis of Fas+ targets
We previously demonstrated that a small peptide antagonist of the Fas receptor (Met12) inhibits Fas-induced Caspase 8 activation and cell death of photoreceptors and retinal pigment epithelial cells in models of retinal detachment and NaIO3 model of oxidative stress respectively [34, 35]. In this study, we used a new derivative of Met12, ONL1204, with improved pharmaceutical properties. To confirm that ONL1204 blocks Fas death receptor signaling, we treated Fas+ murine A20 B lymphoma cells with membrane-FasL-expressing microvesicles in the presence of increasing concentrations of ONL1204 (Fig. 1). We previously demonstrated that microvesicles isolated from transfected Neuro2a cells expressing murine membrane-bound FasL (mFasL-VP) can serve as a cell-free source of mFasL that is highly efficient in killing Fas+ murine A20 B lymphoma cells [40]. Microvesicles isolated from Neuro2a cells transfected with the vector control (Neo-VP) do not express mFasL and serve as a negative control. Herein, A20 cells were treated with mFasL-VP at a 1:100 dilution for 4 h, and 3H-Thymidine incorporation indicated significant cell death with only 8.0% survival when compared to A20 cells incubated with media alone (Fig. 1). By contrast, no significant cell death was observed in A20 cells treated with Neo-VP, resulting in 100% survival when compared to A20 cells incubated with media alone. To determine whether ONL1204 could block apoptosis triggered by mFasL-VP, A20 cells were treated with mFasL-VP at a 1:100 dilution for 4 h in the presence of increasing concentrations of ONL1204 or vehicle control. Our results showed that FasL-induced apoptosis was inhibited by ONL1204 in a dose-dependent manner, while vehicle only had no effect (Fig. 1). These results demonstrate that ONL1204 can block activation of the Fas death receptor signaling pathway and prevent mFasL-induced apoptosis.
ONL1204 rescues A20 B lymphoma cells from FasL-mediated apoptosis. The ability of ONL1204 to inhibit FasL-mediated apoptosis of murine A20 B lymphoma cells was evaluated in vitro. Microvesicle preparations were isolated from transfected Neuro2a cells that expressed either murine mFasL (mFasL VP) or the vector control (Neo VP) as described previously [40]. A20 lymphoma cells were incubated for 4 h with increasing concentrations of ONL1204 or the vehicle control together with a 1:100 dilution of either mFasL VP or Neo VP and then cultured overnight in the presence of 3H-thymidine. Percent survival was assessed by 3H-thymidine incorporation using the formula (cpm of A20 cells cultured with mFasL VP + ONL1204 or vehicle)/(cpm of A20 cells incubated with media alone). A20 cells cultured with mFasL-VP alone served as the positive control (≈ 8% survival), while A20 cells cultured with neo-VP alone served as the negative control (≈ 100% survival). Data presented as % survival ± SEM. N = 6 per group, ***P < 0.001, ****P < 0.0001
Fas activation is required for death of RGCs and axon degeneration in an inducible mouse model of glaucoma
Using genetically modified mice, we demonstrated previously that the membrane-bound form of FasL (mFasL) is neurotoxic and accelerates RGC death and axon degeneration in inducible and chronic mouse models of glaucoma [31, 36]. By contrast, overexpression of the soluble form of FasL (sFasL) via AAV-mediated gene delivery prevented RGC death and axon degeneration [31]. While these previous studies revealed opposing roles for mFasL and sFasL in the pathogenesis of glaucoma, the requirement of the Fas signaling pathway for the development of glaucoma was never demonstrated. Therefore, to determine whether Fas signaling was required for the development of glaucoma, we utilized a well-defined microbead-induced mouse model of elevated IOP to induce elevated IOP in C57BL/6J WT mice and Fas-deficient LPR mice (Faslpr)) [41]. As previously described [31], a single anterior chamber injection of 15 μm polystyrene microbeads resulted in elevated IOP for up to 21 days in C57BL/6J WT as compared to saline controls (Fig. 2a). The IOP was monitored by rebound tonometry, and there was no significant difference in the time course or magnitude of the microbead-induced elevated IOP between Faslpr mice or C57BL/6J WT mice, indicating Fas signaling was not involved in the elevation of IOP. At 4 weeks post-microbead injection, RGC density was measured in retinal whole mounts stained with a RGC-specific anti-Brn3a antibody [37] (Fig. 2b, c) and axon density was measured in optic nerve sections stained with PPD [31] (Fig. 2d, e). Quantification of RGCs revealed a significant decrease in RGC density in microbead-injected WT mice as compared to saline-injected controls (Fig. 2c). However, in the absence of Fas signaling, the RGC density in microbead-injected Faslpr mice was equal to that of saline-injected controls (Fig. 2c). Similar results were observed in the optic nerve where Fas deficiency afforded complete protection of axons in microbead-injected Faslpr mice as compared to the microbead-injected C57BL/6 WT mice (Fig. 2d, e). Taken together, these results demonstrate that Fas signaling is required for the death of RGCs and loss of axons in the microbead-induced mouse model of glaucoma.
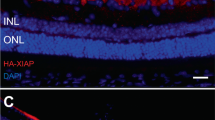
Fas signaling pathway is required for death of RGCs and loss of axons in microbead-induced model of glaucoma. a IOP measurements were taken by rebound tonometry in WT and Fas-deficient Faslpr mice injected with microbeads or saline. Data is presented as mean IOP ± SD, N = 6 mice per group. IOP was significantly elevated on days 3–21 in WT and LPR mice that received microbeads as compared with WT control mice receiving saline (****P < 0.0001). b Representative confocal images of retinal flatmounts isolated at 28 days post-microbead or saline injection and stained with an anti-Brn3a antibody (red, RGC-specific marker) and a DAPI nuclear stain (blue) (scale bar, 50 μm). c Quantification of Brn3a positive RGCs represented as the mean RGC density/mm2 retina ± SD. N = 6 per group, ***P<0.001, **P<0.01. d Representative photomicrographs of PPD-stained optic nerve cross-sections at 28 days post-microbead or saline injections (scale bar, 20 μm). e Quantification of healthy axons represented as the mean axon density (104)/mm2 ON ± SD. N = 6 per group, ****P < 0.0001
Pre-elevated IOP treatment with ONL1204 protects RGCs and prevents axon degeneration in the microbead-induced model of glaucoma
To determine the neuroprotective potential of Fas-receptor inhibition in glaucoma, we pretreated C57BL/6J WT mice with ONL1204, prior to induction of elevated IOP. In this study, C57BL/6J WT mice received an intravitreal injection of ONL1204 (2 μg/μl) or vehicle only, immediately preceding injection of microbeads or saline. IOPs were monitored every 3–4 days by rebound tonometry and revealed no significant difference in the time course or magnitude of the microbead-induced elevated IOP between mice treated with ONL1204 or vehicle only, indicating ONL1204 did not affect IOP (Fig. 3a). Quantification of RGCs at 4 weeks post-microbead injection revealed a significant decrease in RGC density in microbead-injected vehicle-treated mice as compared to the saline-injected controls (Fig. 3b, c). However, pretreatment with ONL1204 was neuroprotective, and the RGC density in microbead-injected ONL1204-treated mice was equal to the RGC density in the saline-injected controls (Fig. 3b, c). Similar results were observed in the optic nerve with a significant decrease in axon density detected in microbead-injected, vehicle-treated mice when compared to saline-injected controls, while pretreatment with ONL1204 afforded complete protection of axons with axon density in microbead-injected ONL1204-treated mice equal to that of the saline-injected controls (Fig. 3d, e). Taken together, these results demonstrate that pretreatment with the Fas inhibitor, ONL1204, prior to elevated IOP provides significant neuroprotection to both RGCs and their axons in the microbead-induced mouse model of glaucoma.
Pre-elevated IOP treatment with ONL1204 protects RGCs and prevents axon degeneration in microbead-induced model of glaucoma. WT C57BL/6J mice received an intravitreal injection of ONL1204 (2 μg/1 μl injection) or vehicle only, immediately followed by an anterior chamber injection of microbeads or saline (day 0). a IOP measurements were taken by rebound tonometry every 3–4 days. Data is presented as mean IOP ± SD, N = 8 mice per group. IOP was significantly elevated on days 3–21 in microbead-injected WT mice treated with ONL1204 or vehicle when compared to saline-injected WT controls treated with ONL1204 or vehicle (****P < 0.0001). b Representative confocal images of retinal flatmounts isolated at 28 days post-microbead or saline injection and stained with an anti-Brn3a antibody (red, an RGC-specific marker) and a DAPI nuclear stain (blue) (scale bar, 50 μm). c Quantification of Brn3a-positive RGCs represented as the mean RGC density/mm2 retina ± SD. N = 8 per group, ***P < 0.001, ****P < 0.0001. d Representative photomicrographs of PPD-stained optic nerve cross-sections at 28 days post-microbead or saline injections (scale bar, 20 μm). e Quantification of healthy axons represented as the mean axon density (104)/mm2 ON ± SD. N = 8 per group, ***P < 0.001, ****P < 0.0001
Post-elevated IOP treatment with ONL1204 protects RGCs and prevents axon degeneration in the microbead-induced model of glaucoma
While pretreatment with ONL1204 provided significant neuroprotection in the microbead-induced mouse model of glaucoma, the more clinically relevant question is whether treatment with ON1204 can provide neuroprotection even when administered after detection of elevated IOP, as this would be the time at which glaucoma patients would most likely receive treatment. To answer this question, C57BL/6J WT mice received an anterior chamber injection of microbeads or saline, and at 7 days post-microbead injection, all mice receive an intravitreal injection of ONL1204 or vehicle alone. IOPs were monitored every 3–4 days by rebound tonometry, verifying that IOP was elevated prior to intravitreal injection of the drug or vehicle. The IOP data revealed no significant difference in the time course or magnitude of the IOP between mice treated with ONL1204 or vehicle at 7 days post-microbead injection (Fig. 4a). At 4 weeks post-microbead injection, quantification of RGCs revealed significant preservation of RGCs in the ONL1204-treated mice when compared to mice treated with vehicle alone (Fig. 4b, c). Significant protection of axons was also observed with axon density in ONL1204-treated mice equivalent to the axon density in saline-treated controls (Fig. 4d, e). In conclusion, these data demonstrate that inhibition of Fas activation provides significant protection to both the RGCs and axons, even when administered after elevated IOP.
Post-elevated IOP treatment with ONL1204 protects RGCs and prevents axon degeneration in microbead-induced model of glaucoma. WT C57BL/6J mice received an intravitreal injection of ONL1204 (2 μg/1 μl injection) or vehicle at 7 days post-anterior chamber injection of microbeads or saline. a IOP measurements were taken by rebound tonometry every 3–4 days. Data is presented as mean IOP ± SD, N = 6 mice per group. IOP was significantly elevated on days 3–21 in microbead-injected WT mice treated with ONL1204 or vehicle when compared to saline-injected WT controls treated with ONL1204 or vehicle (****P < 0.0001). b Representative confocal images of retinal flatmounts isolated at 28 days post-microbead or saline injection and stained with an anti-Brn3a antibody (red, an RGC-specific marker) and a DAPI nuclear stain (blue) (scale bar, 50 μm). c Quantification of Brn3a-positive RGCs represented as the mean RGC density/mm2 retina ± SD. N = 6 per group (***P < 0.001, ****P < 0.0001). d Representative photomicrographs of PPD-stained optic nerve cross-sections at 28 days post-microbead or saline injections (scale bar, 20 μm). e Quantification of healthy axons represented as the mean axon density (104)/mm2 ON ± SD. N = 6 per group, **P < 0.01
ONL1204-mediated neuroprotection correlates with reduced activation of Iba1+ microglia and/or infiltrating macrophages
In human and experimental models of glaucoma, activated microglia are detected in the optic nerve head and retina [14,15,16,17,18,19], and blocking microglia activation with minocycline [14, 20], anti-TNF [22, 23], or irradiation [42] prevents death of RGCs and axon degeneration. While triggering the Fas receptor is best known for inducing apoptosis, we previously demonstrated that accelerated death of RGCs in mice that only express the membrane form of FasL (mFasL) correlated with increased activation of retinal microglia, suggesting that FasL mediates both RGC apoptosis and glial activation [36]. To determine whether ONL1204-mediated neuroprotection correlates with inhibition of microglia activation in the neural retina, C57BL/6J WT mice were pretreated with ONL1204 just prior to the anterior chamber injection of microbeads. At 28 days post-microbead injection, retinal whole mounts were stained with Iba1 (microglia/macrophage marker). Retinal microglia are located in the ganglion cell layer (GCL), inner plexiform layer (IPL), and outer plexiform layer (OPL). However, we did not detect any changes in the microglia in the OPL during the development of glaucoma in our model system, and since glaucoma specifically targets the RGCs and their axons, we focused our analysis on microglia in the GCL and IPL of the retina. Representative confocal images from saline control groups treated with vehicle or ONL1204 reveal Iba1+ cells with a quiescent phenotype and dendritic morphology (Fig. 5a), while confocal images from microbead-injected mice treated with vehicle only reveal Iba1+ cells with an activated phenotype and amoeboid morphology (Fig. 5a). By contrast, the Iba1+ cells in retinal whole mounts prepared from microbead-injected mice pretreated with ONL1204 maintained a quiescent phenotype with dendritic morphology, similar to that observed in the saline-injected control groups (Fig. 5a). Quantification of microglia density in the GCL/IPL revealed no significant difference in absolute number of Iba1+ cells at 28 days post-microbead injection between all groups (Fig. 5b). However, quantification of microglia activation, using the measurement of the longest process length as previously described [39], revealed a significant shortening of the cell process length in Iba1+ cells from microbead-injected mice treated with vehicle as compared to Iba1+ cells from microbead-injected mice treated with ONL1204 (Fig. 5c). These data indicate that Fas activation mediates both RGC apoptosis and microglia activation.
Inhibition of Fas signaling prevents activation of retinal microglia following elevated IOP. WT C57BL/6J mice received an intravitreal injection of ONL1204 (2 μg/1 μl injection) or vehicle just prior to an anterior chamber injection of microbeads or saline (day 0). a Representative confocal images of retinal flatmounts isolated at 28 days post-microbead or saline injection and stained with an anti-Iba1 antibody (red, microglia/macrophage marker). Iba1+ cells in the saline-injected WT mice treated with vehicle or ONL1204 displayed a quiescent phenotype with dendritic morphology (white arrow), while Iba1+ cells in microbead-injected WT mice treated with vehicle display a more activated phenotype, with amoeboid morphology (white arrowhead) that is inhibited in microbead-injected mice treated with ONL1204 (scale bar, 50 μm). b Quantification of Iba1+ cells in the GCL/IPL revealed no significant difference between any groups at 28 days post-microbead injection. c Morphometric analysis was performed on Iba1+ cells in the GCL/IPL (60 cells per retina), and the longest process length measured from the edge of the cell body (in micrometer) was used to quantitate microglia activation as previously described. Data presented as the mean microglia density/mm2 ± SD and the mean longest process length in μM ± SD. N = 3–4 per group, ***P < 0.001, ****P < 0.0001
ONL1204-mediated neuroprotection correlates with a significant reduction in inflammatory cytokines and chemokines
In human and experimental glaucoma, multiple inflammatory pathways have been implicated in the pathogenesis of disease, including the Toll-like receptor signaling pathway [43], the inflammasome pathway [44,45,46,47], the TNFα pathway [22, 23, 48,49,50], and the complement cascade [51,52,53]. While triggering of the Fas receptor is best known for inducing apoptosis through the activation of caspase-8, activated caspase-8 can also induce the production of pro-inflammatory mediators [54,55,56,57]. Moreover, caspase-8 activation has also been linked to microglia activation [58] and inflammation in experimental models of glaucoma and inhibiting caspase-8 blocked inflammation and prevented death of RGCs [45]. To explore the role of Fas activation in triggering inflammation in glaucoma, we pretreated C57BL/6J WT mice with ONL1204 just prior to injection of microbeads, and at 28 days post-microbead injection, the neural retina was isolated, and qPCR was performed to assess the expression of several proinflammatory genes associated with human and/or experimental models of glaucoma. We first examined the gene expression of caspase-8, which plays an essential role in Fas receptor signaling cascades that induces both apoptosis and cytokine production [55], as well as GFAP as a measure of glial activation. The qPCR analysis revealed a significant induction in both GFAP and Caspase-8 in microbead-injected mice treated with vehicle only, as compared to saline-treated controls (Fig. 6a). We then examined the gene expression of several proinflammatory cytokines (TNFα, IL-1β, IL-6, and IL-18) (Fig. 6b) and chemokines (MIP-1α, MIP-1β, MIP-2, MCPI, and IP10) (Fig. 6c) that have been implicated in human and experimental models of glaucoma [43, 48, 59,60,61]. The qPCR analysis revealed significant induction of each of these genes in the retina of microbead-injected mice treated with vehicle only as compared to the saline-treated controls (Fig. 6b, c). By contrast, pretreatment with ONL1204 prevented the induction of each of these genes and gene expression was equivalent to the saline-treated control (Fig. 6b, c). Additionally, key mediators of the Toll-like receptor pathway, inflammasome pathway, and complement cascade that have been identified in human and experimental glaucoma were also examined, specifically TLR4 [43, 44], NLRP3 [44, 45, 48], and complement components C3 and C1Q [53, 62, 63]. Similar to the proinflammatory cytokines and chemokines, gene expressions of C3, C1Q, TLR4, and NLRP3 were all significantly induced at 28 days post-microbead injection in the retina of microbead-injected mice treated with vehicle only as compared to saline-treated controls (Fig. 6d, e). However, the induction of each of these genes was inhibited in microbead-injected mice that were pretreated with ONL1204 (Fig. 6d, e). Together, these results suggest that Fas activation is upstream to multiple inflammatory pathways that have been implicated in glaucoma and blocking Fas activation with ONL1204 prevents RGC apoptosis, as well as microglia activation and the induction of neurodestructive inflammation.
Inhibition of Fas signaling prevents the induction of multiple inflammatory pathways implicated in the pathogenesis of glaucoma. At 28 days post-microbead or saline injection, quantitative PCR was performed on neural retina isolated from saline- and microbead-injected WT mice treated (on day 0) with ONL1204 or vehicle to assess the expression of several proinflammatory genes associated with human and/or experimental models of glaucoma: a Caspase 8 and GFAP, b proinflammatory cytokines (TNFα, IL-1β, IL-18, and IL-6), c proinflammatory chemokines (MIP-1α, MIP-1β, MIP-2, MCPI, and IP10), d complement components C3 and C1Q, and e NLRP3 and TLR4. The threshold cycle values of each gene of interest were normalized to the geometric mean of two housekeeping genes (B2-microglobulin and peptidylpropyl isomerase A) and compared with the saline + vehicle control group using the comparative C method (ΔΔC). Data are presented as fold change of control ± SEM. N = 6 per group, *P < 0.05, **P < 0.01, ***P < 0,001, ****P < 0.0001
Discussion
In this study, we evaluated the neuroprotective effect of ONL1204, a novel small peptide inhibitor of the Fas receptor, in a microbead-induced mouse model of elevated IOP. We previously demonstrated that apoptosis of RGCs in both inducible and chronic mouse models of glaucoma was dependent upon the FasL-Fas signaling pathway [31, 36]. While several studies have implicated the proinflammatory cytokine TNFα as the critical link between elevated IOP and death of RGCs in glaucoma [22, 23, 48, 49], Nakazawa et al. demonstrated in a laser-induced mouse model of ocular hypertension that TNFα does not directly kill RGCs, but rather RGC death is dependent upon TNFR2-mediated activation of microglia [23]. Our laboratory went on to demonstrate that TNFα increased expression of FasL on microglia in the glaucomatous retina and that the membrane-bound form of FasL was the key effector of RGC apoptosis in an inducible mouse model of glaucoma [36]. However, it has become increasingly apparent that in addition to apoptosis, Fas-mediated signaling can also induce the release of proinflammatory cytokines and promote inflammation [40, 64,65,66]. Using our novel Fas inhibitor, ONL1204, in an inducible mouse model of glaucoma, we show that blocking Fas activation prevents axon degeneration and the death of RGCs, as well as the activation of microglia and the induction of multiple inflammatory genes previously implicated in both experimental and human glaucoma. Importantly, many of the cytokines and chemokines we have now quantified in the glaucomatous eyes are the same proinflammatory molecules that we previously found to be produced by FasL-treated macrophages [40]. Moreover, the data presented herein provide proof of principle that treatment with ONL1204 effectively blocks Fas activation and affords significant neuroprotection to RGCs and their axons in an experimental model of glaucoma. Having identified the FasL-Fas signaling pathway as an essential pathway in the pathogenesis of glaucoma, the first aim of the present study was to evaluate the neuroprotective effect of our novel Fas inhibitor, ONL1204, in the microbead-induced mouse model of glaucoma. The ONL1204 inhibitor is a new derivative of Met12, a small peptide that we showed could inhibit Fas activation and subsequent apoptosis of photoreceptors and retinal pigment epithelial cells in models of retinal detachment and retinal degeneration [34, 35]. Through assessment of axon degeneration and RGC survival, our results provide proof-of-principal that ONL1204 can provide robust neuroprotection in an inducible mouse model of glaucoma, even when administered after the detection of elevated IOP. In addition, we found that ONL1204-mediated neuroprotection correlates with significantly reduced activation of retinal microglia and no significant induction of proinflammatory genes implicated in both human and experimental glaucoma. These data support our hypothesis that in glaucoma, Fas activation is a critical mediator of RGC apoptosis, as well as microglial activation and neuroinflammation.
The results of this present study are in agreement with our previous work using an AAV2-mediated gene therapy approach to deliver soluble FasL, considered an antagonist of the proapoptotic and proinflammatory membrane form of FasL [31]. Overexpression of sFasL using the AAV2-mediated gene therapy approach prevented axon degeneration and death of RGCs in both inducible and chronic mouse models of glaucoma, and this neuroprotection correlated with an inhibition of Müller glia activation and induction of inflammatory mediators [31]. Taken together, the previous results of our sFasL-AAV2 study combined with results of the present study with ONL1204 strongly support the value of Fas inhibition as an approach to neuroprotection in glaucoma, both in preserving RGC viability and in preventing neuroinflammation.
Neuroinflammation has long been associated with chronic neurodegenerative diseases such as Alzheimer’s and Parkinson’s [67,68,69]. However, while glial activation and inflammatory cytokines have been detected in the optic nerve head and retina of human [17, 19, 48] and experimental models of glaucoma [20, 21, 60, 70], the specific impact of glial activation and neuroinflammation on the development and/or progression of glaucoma is not well understood. In human and experimental models of glaucoma, activated microglia are detected in the ONH and retina [14, 16, 17, 19, 20]. Microglia are the resident innate immune cells of the retina and optic nerve and are responsible for normal maintenance of neuronal tissue, as well as a local response to injury. However, in retinal degenerative diseases, chronic microglia activation has been linked to retinal damage and neuronal apoptosis [71] and the extent of microglia activation in the ONH coincides with the severity of axon degeneration [14, 20, 21]. Moreover, Barres and colleagues demonstrate in the CNS that neurotoxic astrocytes are induced by activated microglia [72] and blocking microglial activation with minocycline [14, 20] or anti-TNF [22, 23] prevents axon degeneration and death of RGCs suggesting that activated microglia are the driving force behind the axon degeneration and death of RGCs in glaucoma. However, the molecular mechanism(s) that mediate microglia reactivity in glaucoma have not yet been defined.
While the specific trigger(s) of neuroinflammation in glaucoma remains poorly defined, a number of key inflammatory pathways have been implicated in the pathogenesis of glaucoma and are common to both human and animal models of glaucoma. These pathways include the complement cascade [53, 62, 63], Toll-like receptor pathway [43, 44], TNFα pathway [22, 23, 48,49,50], and inflammasome pathway [44,45,46,47]. Using the microbead-induced mouse model of glaucoma, we also show an induction of genes associated with each of these pathways at 4 weeks post-microbead injection, specifically C3 and C1Q (complement cascade), TLR4 (Toll-like receptor pathway), TNFα (TNFα pathway), and NLRP3 (inflammasome pathway). However, treatment with ONL1204 completely abrogated the induction of each of these genes, indicating that Fas activation is upstream to these pathways and plays a central role in mediating neuroinflammation in glaucoma. In addition, the induction of these inflammatory genes correlated with a significant increase in the number of activated, amoeboid-shaped Iba1+ cells in the retina and treatment with ONL1204 completely abrogated the activation of Iba1+ cells in the retina with the Iba1+ cells displaying a homeostatic, dendritic phenotype indistinguishable from the non-glaucoma controls. Together, these data indicate that blocking Fas signaling prevents microglial activation and the development of neuroinflammation.
However, the Fas receptor is expressed on multiple retinal cell types, including astrocytes, RGCs, Mueller cells, microglia, and retinal pigment epithelial cells [7, 31, 36, 73]. Therefore, additional studies in which the Fas receptor is deleted from specific cell types will be necessary to determine which Fas receptor-positive cell(s) actually drive(s) the development of neuroinflammation in glaucoma. Moreover, Fas mediates both apoptotic and inflammatory pathways and it is not possible from the current studies to determine the extent to which Fas-mediated apoptosis and/or Fas-mediated inflammation contributes to axon degeneration and death of RGCs in glaucoma. Yet, previous therapeutic approaches that specifically targeted the apoptotic pathway alone resulted in neuroprotection of the RGC soma but failed to prevent axon degeneration [11, 12], suggesting the robust neuroprotective effect afforded by ONL1204 is dependent upon the ability of ONL1204 to antagonize both Fas-mediated apoptosis of RGCs and Fas-mediated activation of retinal microglia and induction of neuroinflammation. Additional studies in which the Fas receptor is specifically knocked out in RGCs or glial cells (microglia, astrocytes, and Mueller cells) are necessary to determine if the neuroprotective effects of ONL1204 are mainly driven by modulating the inflammatory response of retinal glial cells or preventing FasL-induced apoptosis of RGCs.
While triggering of the Fas receptor is known for inducing apoptosis through the activation of caspase-8, activated caspase-8 can also induce the production of pro-inflammatory mediators [44, 55, 57, 74]. Although activation of IL-1β and IL-18 is most often thought to be inflammasome-dependent, we recently demonstrated that Fas can mediate IL-1β and IL-18 maturation via a caspase-8-dependent inflammasome-independent mechanism [55]. In addition, caspase-8 activation has been linked to inflammation in experimental models of glaucoma and inhibition of caspase-8 blocks inflammation and prevents death of RGCs [44, 45]. Yet, similar to our findings presented herein, the previous caspase-8 studies were unable to determine the extent to which caspase-8-mediated inflammation and/or caspase-8-mediated apoptosis contributed to axon degeneration and RGC apoptosis. However, while caspase-8-mediated inflammation can be triggered by the Fas-receptor [55, 74], TRAIL receptor [75], and Toll-like receptors (TLRs) [76, 77], we demonstrate herein that specifically blocking Fas activation in the microbead-induced mouse model of glaucoma inhibits the induction of caspase-8, retinal microglia activation, and the induction of proinflammatory genes, indicating the TRAIL- and TLR-mediated pathways are downstream of the FasL-Fas pathway. Moreover, determining the extent to which Fas-mediated inflammation and/or apoptosis contributes to axon degeneration and death of RGCs in glaucoma will require the uncoupling the Fas-mediated apoptosis and Fas-mediated inflammatory pathways and this will be the focus of our future studies.
As a complex multifactorial disease, we predict the most successful neuroprotective therapy for glaucoma will have to impact multiple pathways and the data presented herein strongly support pursuing the FasL-Fas signaling pathway as an optimal target for successful neuroprotection in glaucoma. Specifically blocking Fas activation in this present study resulted in significant inhibition of glial activation, neuroinflammation, and RGC death. In the normal eye, the FasL-Fas signaling pathway plays an essential role in the maintenance of ocular immune privilege where inflammation is tightly regulated [28, 78, 79]. However, it has become increasingly clear that immune privilege is not simply established through suppression of all immune responses, but rather through modulation of the immune responses in a way that provides immune protection to the delicate tissues of the eye while limiting the development of destructive inflammation. FasL is constitutively expressed in the immune-privileged eye where the membrane form of FasL is the active form, inducing apoptosis of infiltrating Fas+ immune cells [28, 78, 79]. However, because the Fas receptor is ubiquitously expressed on multiple cell types throughout the eye, the cleavage or shedding of mFasL acts to limit the expression of mFasL and prevent the killing of healthy Fas+ bystander cells [80, 81]. However, in glaucoma, the cleavage or shedding of mFasL is significantly reduced resulting in a significant decrease in release of sFasL and concomitant increase in the expression of mFasL that correlates with the apoptosis of Fas+ RGCs [31]. Therefore, we propose that either treatment with sFasL, as we previously demonstrated [31], or treatment with a Fas inhibitor as shown in this present study will work to (i) block the proapoptotic and proinflammatory activity of mFasL, (ii) promote restoration of the ocular immune-privileged environment, and (iii) support the return of the activated retinal microglia to their original homeostatic phenotype.
Conclusions
In summary, our data provide proof-of-principal that treatment with the small peptide inhibitor of the Fas receptor, ONL1204, provides significant protection of the RGC soma and their axons in an inducible mouse model of glaucoma. In addition, the studies presented herein demonstrate the requirement of Fas activation in both the death of RGCs and axon degeneration, as well as the activation of retinal microglial and induction of neuroinflammation in the development of glaucoma. Future studies will be aimed at identifying the critical source of FasL and uncoupling the Fas-mediated apoptosis and Fas-mediated inflammatory pathways in order to determine the extent to which inflammation versus apoptosis contributes to the development and progression of glaucoma.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- FasL:
-
Fas ligand
- GCL:
-
Ganglion cell layer
- IOP:
-
Intraocular pressure
- mFasL:
-
Membrane-bound Fas ligand
- ON:
-
Optic nerve
- ONH:
-
Optic nerve head
- PPD:
-
Paraphenylenediamine
- RGCs:
-
Retinal ganglion cells
- sFasL:
-
Soluble Fas ligand
References
Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: clinical and experimental concepts. Clin Exp Ophthalmol. 2012;40:341–9.
Heijl A, Leske CM, Bengtsson B, Hyman L, Bengtsson B, Hussein M, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol-chic. 2002;120:1268–79.
Mudumbai RC. Clinical update on normal tension glaucoma. Semin Ophthalmol. 2013;28:173–9.
Song BJ, Caprioli J. New directions in the treatment of normal tension glaucoma. Indian J Ophthalmol. 2014;62:529–37.
Leibowitz H, Krueger D, Maunder L, Milton R, Kini M, Kahn H, et al. The Framingham Eye Study monograph: an ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973-1975. Surv Ophthalmol. 1980;24:335–610.
Kim H, Park C. Retinal ganglion cell death is delayed by activation of retinal intrinsic cell survival program. Brain Res. 2005;1057:17–28.
Quigley H, Nickells R, Kerrigan L, Pease M, Thibault D, Zack D. Retinal ganglion cell death in experimental glaucoma and after axotomy occurs by apoptosis. Invest Ophth Vis Sci. 1995;36:774–86.
Kerrigan LA, Zack DJ, Quigley HA, Smith SD, Pease ME. TUNEL-positive ganglion cells in human primary open-angle glaucoma. Arch Ophthalmol-chic. 1997;115:1031–5.
Garcia-Valenzuela E, Shareef S, Walsh J, Sharma SC. Programmed cell death of retinal ganglion cells during experimental glaucoma. Exp Eye Res. 1995;61:33–44.
Libby RT, Li Y, Savinova OV, Barter J, Smith RS, Nickells RW, et al. Susceptibility to neurodegeneration in a glaucoma is modified by Bax gene dosage. PLoS Genet. 2005;1:e4.
McKinnon SJ, Lehman DM, Tahzib NG, Ransom NL, Reitsamer HA, Liston P, et al. Baculoviral IAP repeat-containing-4 protects optic nerve axons in a rat glaucoma model. Mol Ther. 2002;5:780–7.
Soto I, Howell GR. The complex role of neuroinflammation in glaucoma. Csh Perspect Med. 2014;4:a017269.
Bordone MP, Fleitas MF, Pasquini LA, Bosco A, Sande PH, Rosenstein RE, et al. Involvement of microglia in early axoglial alterations of the optic nerve induced by experimental glaucoma. J Neurochem. 2017;142:323–37.
Bosco A, Steele MR, Vetter ML. Early microglia activation in a mouse model of chronic glaucoma. J Comp Neurol. 2011;519:599–620.
Ebneter A, Casson RJ, Wood JP, Chidlow G. Microglial activation in the visual pathway in experimental glaucoma: spatiotemporal characterization and correlation with axonal injury. Invest Ophth Vis Sci. 2010;51:6448–60.
Yuan L, Neufeld AH. Activated microglia in the human glaucomatous optic nerve head. J Neurosci Res. 2001;64:523–32.
Yuan L, Neufeld AH. Tumor necrosis factor-α: a potentially neurodestructive cytokine produced by glia in the human glaucomatous optic nerve head. Glia. 2000;32:42–50.
Neufeld AH. Microglia in the optic nerve head and the region of parapapillary chorioretinal atrophy in glaucoma. Arch Ophthalmol-chic. 1999;117:1050–6.
Bosco A, Romero CO, Breen KT, Chagovetz AA, Steele MR, Ambati BK, et al. Neurodegeneration severity can be predicted from early microglia alterations monitored in vivo in a mouse model of chronic glaucoma. Dis Model Mech. 2015;8:443–55.
Bosco A, Breen KT, Anderson SR, Steele MR, Calkins DJ, Vetter ML. Glial coverage in the optic nerve expands in proportion to optic axon loss in chronic mouse glaucoma. Exp Eye Res. 2016;150:34–43.
Roh M, Zhang Y, Murakami Y, Thanos A, Lee S, Vavvas DG, et al. Etanercept, a widely used inhibitor of tumor necrosis factor-α (TNF- α), prevents retinal ganglion cell loss in a rat model of glaucoma. Plos One. 2012;7:e40065.
Nakazawa T, Nakazawa C, Matsubara A, Noda K, Hisatomi T, She H, et al. Tumor necrosis factor-α mediates oligodendrocyte death and delayed retinal ganglion cell loss in a mouse model of glaucoma. J Neurosci. 2006;26:12633–41.
Ju S-T, Panka DJ, Cui H, Ettinger R, EI-Khatib M, Sherr DH, et al. Fas(CD95)/FasL interactions required for programmed cell death after T-cell activation. Nature. 1995;373:444–8.
Brunner T, Mogil RJ, LaFace D, Yoo N, Mahboubi A, Echeverri F, et al. Cell-autonomous Fas (CD95)/Fas-ligand interaction mediates activation-induced apoptosis in T-cell hybridomas. Nature. 1995;373:373441a0.
Griffith TS, Yu X, Herndon JM, Green DR, Ferguson TA. CD95-induced apoptosis of lymphocytes in an immune privileged site induces immunological tolerance. Immunity. 1996;5:7–16.
Dhein J, Walczak H, Bäumler C, Debatin K-M, Krammer PH. Autocrine T-cell suicide mediated by APO-1/(Fas/CD95). Nature. 1995;373:373438a0.
Gregory MS, Repp AC, Holhbaum AM, Saff RR, Marshak-Rothstein A, Ksander BR. Membrane Fas ligand activates innate immunity and terminates ocular immune privilege. J Immunol. 2002;169:2727–35.
Matsumoto H, Murakami Y, Kataoka K, Notomi S, Mantopoulos D, Trichonas G, et al. Membrane-bound and soluble Fas ligands have opposite functions in photoreceptor cell death following separation from the retinal pigment epithelium. Cell Death Dis. 2015;6:e1986.
Gregory-Ksander M, Perez VL, Marshak-Rothstein A, Ksander BR. Soluble Fas ligand blocks destructive corneal inflammation in mouse models of corneal epithelial debridement and LPS induced keratitis. Exp Eye Res. 2019;179:47–54.
Krishnan A, Fei F, Jones A, Busto P, Marshak-Rothstein A, Ksander BR, et al. Overexpression of soluble Fas ligand following adeno-associated virus gene therapy prevents retinal ganglion cell death in chronic and acute murine models of glaucoma. J Immunol. 2016;197:4626–38.
Mo J-S, Anderson MG, Gregory M, Smith RS, Savinova OV, Serreze DV, et al. By altering ocular immune privilege, bone marrow–derived cells pathogenically contribute to DBA/2J pigmentary glaucoma. J Exp Med. 2003;197:1335–44. 32.
Wang X, DeFrances MC, Dai Y, Pediaditakis P, Johnson C, Bell A, et al. A mechanism of cell survival sequestration of Fas by the HGF receptor met. Mol Cell. 2002;9:411–21.
Besirli CG, Chinskey ND, Zheng Q-D, Zacks DN. Inhibition of retinal detachment-induced apoptosis in photoreceptors by a small peptide inhibitor of the Fas receptor. Invest Ophth Vis Sci. 2010;51:2177–84.
Xiao J, Yao J, Jia L, Lin C, Zacks DN. Protective effect of Met12, a small peptide inhibitor of Fas, on the retinal pigment epithelium and photoreceptor after sodium iodate injury effect of Met12 on RPE and photoreceptor after NaIO3 injury. Invest Ophth Vis Sci. 2017;58:1801–10.
Gregory MS, Hackett CG, Abernathy EF, Lee KS, Saff RR, Hohlbaum AM, et al. Opposing roles for membrane bound and soluble Fas ligand in glaucoma-associated retinal ganglion cell death. PLoS One. 2011;6:e17659.
Dordea AC, Bray M-A, Allen K, Logan DJ, Fei F, Malhotra R, et al. An open-source computational tool to automatically quantify immunolabeled retinal ganglion cells. Exp Eye Res. 2016;147:50–6.
Gao S, Jakobs TC. Mice homozygous for a deletion in the glaucoma susceptibility locus INK4 show increased vulnerability of retinal ganglion cells to elevated intraocular pressure. Am J Pathology. 2016;186:985–1005.
Paschalis EI, Lei F, Zhou C, Kapoulea V, Thanos A, Dana R, et al. The role of microglia and peripheral monocytes in retinal damage after corneal chemical injury. Am J Pathol. 2018;188:1580–96.
Hohlbaum AM, Gregory MS, Ju S-T, Marshak-Rothstein A. Fas ligand engagement of resident peritoneal macrophages in vivo induces apoptosis and the production of neutrophil chemotactic factors. J Immunol. 2001;167:6217–24.
Nagata S, Suda T. Fas and Fas ligand: lpr and gld mutations. Immunol Today. 1995;16:39–43.
Howell GR, Soto I, Zhu X, Ryan M, Macalinao DG, Sousa GL, et al. Radiation treatment inhibits monocyte entry into the optic nerve head and prevents neuronal damage in a mouse model of glaucoma. J Clin Invest. 2012;122:1246–61.
Luo C, Yang X, Kain AD, Powell DW, Kuehn MH, Tezel G. Glaucomatous tissue stress and the regulation of immune response through glial toll-like receptor signaling. Invest Ophth Vis Sci. 2010;51:5697–707.
Chi W, Li F, Chen H, Wang Y, Zhu Y, Yang X, et al. Caspase-8 promotes NLRP1/NLRP3 inflammasome activation and IL-1β production in acute glaucoma. Proc National Acad Sci. 2014;111:11181–6.
Chi W, Chen H, Li F, Zhu Y, Yin W, Zhuo Y. HMGB1 promotes the activation of NLRP3 and caspase-8 inflammasomes via NF-κB pathway in acute glaucoma. J Neuroinflamm. 2015;12:137.
Yerramothu P, Vijay A, Willcox P. Inflammasomes, the eye and anti-inflammasome therapy. Eye. 2017;32:491.
Albalawi F, Lu W, Beckel JM, Lim JC, McCaughey SA, Mitchell CH. The P2X7 receptor primes IL-1β and the NLRP3 inflammasome in astrocytes exposed to mechanical strain. Front Cell Neurosci. 2017;11:227.
Yang X, Luo C, Cai J, Powell DW, Yu D, Kuehn MH, et al. Neurodegenerative and inflammatory pathway components linked to TNF-α/TNFR1 signaling in the glaucomatous human retina. Invest Ophth Vis Sci. 2011;52:8442–54.
Tezel G, Li L, Patil R, Wax M. TNF-alpha and TNF-alpha receptor-1 in the retina of normal and glaucomatous eyes. Invest Ophth Vis Sci. 2001;42:1787–94.
Tezel G. TNF-α signaling in glaucomatous neurodegeneration. Sect V Neuroprotection New Vistas Pathophysiol. 2008;173:409–21.
Williams PA, Tribble JR, Pepper KW, Cross SD, Morgan PB, Morgan JE, et al. Inhibition of the classical pathway of the complement cascade prevents early dendritic and synaptic degeneration in glaucoma. Mol Neurodegener. 2016;11:26.
Howell GR, Soto I, Ryan M, Graham LC, Smith RS, John SW. Deficiency of complement component 5 ameliorates glaucoma in DBA/2J mice. J Neuroinflamm. 2013;10:851.
Kuehn MH, Kim CY, Ostojic J, Bellin M, Alward W, Stone EM, et al. Retinal synthesis and deposition of complement components induced by ocular hypertension. Exp Eye Res. 2006;83:620–8.
Barca O, Seoane M, Señarís R, Arce VM. Fas/CD95 ligation induces proliferation of primary fetal astrocytes through a mechanism involving caspase 8-mediated ERK activation. Cell Physiol Biochem. 2013;32:111–20.
Bossaller L, Chiang P-I, Schmidt-Lauber C, Ganesan S, Kaiser WJ, Rathinam VA, et al. Cutting edge: FAS (CD95) mediates noncanonical IL-1β and IL-18 maturation via caspase-8 in an RIP3-independent manner. J Immunol. 2012;189:5508–12.
Maelfait J, Beyaert R. Non-apoptotic functions of caspase-8. Biochem Pharmacol. 2008;76:1365–73.
Matsumoto N, Imamura R, Suda T. Caspase-8- and JNK-dependent AP-1 activation is required for Fas ligand-induced IL-8 production. FEBS J. 2007;274:2376–84.
Burguillos MA, Deierborg T, Kavanagh E, Persson A, Hajji N, Garcia-Quintanilla A, et al. Caspase signalling controls microglia activation and neurotoxicity. Nature. 2011;472:319.
Jakobs TC. Differential gene expression in glaucoma. Csh Perspect Med. 2014;4:a020636.
Qu J, Jakobs TC. The time course of gene expression during reactive gliosis in the optic nerve. PLoS One. 2013;8:e67094.
Tezel G. Oxidative stress in glaucomatous neurodegeneration: mechanisms and consequences. Prog Retin Eye Res. 2006;25:490–513.
Harder JM, Braine CE, Williams PA, Zhu X, MacNicoll KH, Sousa GL, et al. Early immune responses are independent of RGC dysfunction in glaucoma with complement component C3 being protective. Proc National Acad Sci. 2017;114:E3839–48.
Jha P, Banda H, Tytarenko R, Bora PS, Bora NS. Complement mediated apoptosis leads to the loss of retinal ganglion cells in animal model of glaucoma. Mol Immunol. 2011;48:2151–8.
Ma Y, Liu H, Tu-Rapp H, Thiesen H-J, Ibrahim SM, Cole SM, et al. Fas ligation on macrophages enhances IL-1R1–Toll-like receptor 4 signaling and promotes chronic inflammation. Nat Immunol. 2004;5:ni1054.
Biancone L, Martino A, Orlandi V, Conaldi P, Toniolo A, Camussi G. Development of inflammatory angiogenesis by local stimulation of Fas in vivo. J Exp Med. 1997;186:147–52.
Saas P, Boucraut J, Quiquerez A, Schnuriger V, Perrin G, Desplat-Jego S, et al. CD95 (Fas/Apo-1) as a receptor governing astrocyte apoptotic or inflammatory responses: a key role in brain inflammation? J Immunol. 1999;162:2326–33.
Ransohoff RM. How neuroinflammation contributes to neurodegeneration. Science. 2016;353:777–83.
Chen W-W, Zhang X, Huang W-J. Role of neuroinflammation in neurodegenerative diseases (review). Mol Med Rep. 2016;13:3391–6.
Frank-Cannon TC, Alto LT, McAlpine FE, Tansey MG. Does neuroinflammation fan the flame in neurodegenerative diseases? Mol Neurodegener. 2009;4:47.
Howell GR, Macalinao DG, Sousa GL, Walden M, Soto I, Kneeland SC, et al. Molecular clustering identifies complement and endothelin induction as early events in a mouse model of glaucoma. J Clin Invest. 2011;121:1429–44.
Ramirez AI, de Hoz R, Salobrar-Garcia E, Salazar JJ, Rojas B, Ajoy D, et al. The role of microglia in retinal neurodegeneration: Alzheimer’s disease, Parkinson, and glaucoma. Front Aging Neurosci. 2017;9:214.
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541:481.
Ju KR, Kim HS, Kim JH, Lee NY, Park CK. Retinal glial cell responses and Fas/FasL activation in rats with chronic ocular hypertension. Brain Res. 2006;1122(1):209–21.
Kang T-B, Oh G-S, Scandella E, Bolinger B, Ludewig B, Kovalenko A, et al. Mutation of a self-processing site in caspase-8 compromises its apoptotic but not its nonapoptotic functions in bacterial artificial chromosome-transgenic mice. J Immunol. 2008;181:2522–32.
Rathore N, Matta H, Chaudhary PM. An evolutionary conserved pathway of nuclear factor-κB activation involving caspase-mediated cleavage and N-end rule pathway-mediated degradation of IκBα. J Biol Chem. 2004;279:39358–65.
Philip NH, DeLaney A, Peterson LW, Santos-Marrero M, Grier JT, Sun Y, et al. Activity of uncleaved caspase-8 controls anti-bacterial immune defense and TLR-induced cytokine production independent of cell death. PLoS Pathog. 2016;12:e1005910.
Lemmers B, Salmena L, Bidère N, Su H, Matysiak-Zablocki E, Murakami K, et al. Essential role for caspase-8 in toll-like receptors and NFκB signaling. J Biol Chem. 2007;282:7416–23.
Sano Y, Sotozono C. Role of Fas ligand in ocular tissue. Cornea. 2002;21:S30–2.
Niederkorn J. Immune privilege and immune regulation in the eye. Adv Immunol. 1990;48:191–226.
Tanaka M, Itai T, Adachi M, Nagata S. Downregulation of Fas ligand by shedding. Nat Med. 1998;4:31.
Dupont PJ, Warrens AN. Fas ligand exerts its pro-inflammatory effects via neutrophil recruitment but not activation. Immunology. 2007;120:133–9.
Acknowledgements
We thank Philip Seifert of the Morphology Core at the Schepens Eye Research Institute of Massachusetts Eye and Ear for his technical support in mouse optic nerve PPD stain.
Funding
This study was supported by a Sponsored Research Grant from ONL Therapeutics (MGK), NIH-NEI EY021543 (MGK), NIH-NEI P30 EY003790 (MGK), and NIH-NIAID AI145097 (AMR).
Author information
Authors and Affiliations
Contributions
AK, AJK, DNZ, AMR, and MGK conceived and planned the experiments. AK, MGK, and AMR carried out the experiments and data analysis. MGK, AK, AJK, DNZ, and AMR contributed to the interpretations of the results. MGK took the lead in writing the manuscript in consultation with all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal experiments were approved by the Institutional Animal Care and Use Committee at Schepens Eye Research Institute and were performed under the guidelines of the Association of Research in Vision and Ophthalmology (Rockville, MD).
Consent for publication
Not applicable
Competing interests
AJK is employed by ONL Therapeutics. DNZ is a co-founder, equity holder, and consultant to ONL Therapeutics. Dr. Zacks is also a co-inventor on ONL’s patent applications, as well as on patents and applications licensed by ONL Therapeutics from the University of Michigan and Massachusetts Eye and Ear that are based on the development and use of novel Fas inhibitors. MGK received a sponsored research grant from ONL Therapeutics. AK, AJK, DNZ, MGK are co-inventors on two patent applications submitted by ONL Therapeutics based in part on the results reported herein. MGK and AMR are co-inventors on a patent application on soluble Fas ligand as a neuroprotective therapeutic that has been licensed by ONL Therapeutics from University of Medical School Worcester and Massachusetts Eye and Ear.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Krishnan, A., Kocab, A.J., Zacks, D.N. et al. A small peptide antagonist of the Fas receptor inhibits neuroinflammation and prevents axon degeneration and retinal ganglion cell death in an inducible mouse model of glaucoma. J Neuroinflammation 16, 184 (2019). https://doi.org/10.1186/s12974-019-1576-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-019-1576-3