Abstract
Background
In the last decade, incomplete Kawasaki disease (KD), intravenous immunoglobulin (IVIG) non-response and coronary artery abnormalities (CAA) have experienced the increasing trends in China. In addition, the enhancement of pediatricians’ awareness may also raise the diagnostic rate of incomplete KD and stimulate more aggressive initial therapy in the acute episode of KD. Given this background, we hypothesize that the time option of IVIG treatment should be in parallel with peak time of systemic inflammation; either earlier or later IVIG treatment may affect the clinical classification, therapeutic responsiveness and CAA occurrence in KD patients. Therefore, the major objective of the present study is to identify whether the time option of IVIG treatment could be associated with the clinical classification, therapeutic responsiveness and CAA occurrence in the acute episode of KD.
Materials and methods
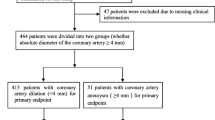
A total of 153 children with KD were recruited between July 2015 and May 2018. All patients received the standard therapy of KD, including a single infusion of IVIG (2 g/kg) and aspirin (30–50 mg/kg/d). Blood samples were collected from all subjects within 24 h pre-IVIG treatment, respectively. Echocardiography was performed during the period from 2 days to 14 days after IVIG treatment.
Results
(1) The clinical classification presented no significant heterogenicity among different treatment time (x2 = 1.59, p > 0.05) (2) Eleven KD patients resisted to IVIG treatment and 7 of them (63.60%) received the initial IVIG dose on day 5 and 6. (3) The distribution of CAA onset was subjected to a significant difference according to timing option of IVIG treatment (x2 = 11.94, p < 0.05).
Conclusions
The time option of IVIG treatment is associated with therapeutic responsiveness and CAA but not with clinical classification in the acute episode of KD.
Similar content being viewed by others
Background
Kawasaki disease (KD) is an acute self-limited vasculitis of childhood that leads to coronary artery abnormalities (CAA) in approximate 5% of treated cases [1]. It is the leading cause of acquired heart disease in children younger than 5 years of age in Asian countries. According to a latest epidemiological study in Shanghai, China, the average annual incidence rate of KD was 50.5 per 100,000 children during the period of 2008–2012 [2]. In light of the 2017 American Heart Association (AHA) guidelines, the diagnosis criteria of KD include fever ≥5 days and four or more of the five major clinical features. Besides, incomplete KD should be considered in any case with persistent unexplained fever, fewer than 4 of the major clinical features, and compatible laboratory or echocardiographic findings [3]. Elevation of acute-phase reactants such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) is nearly universal and very helpful to reflect disease severity. Song et al. [4] evaluated the diagnostic efficiency of ESR and CRP in 67 children with persistent fever and found that the estimated sensitivity of ESR for predicting KD was 93.9%, and specificity was 83.3%; the estimated sensitivity of CRP for predicting KD was 69.0%, and specificity was 72.7%. Echocardiography is the primary imaging modality for cardiac assessment because it is noninvasive and has a very high sensitivity (100%) and specificity (95–100%) for the detection of abnormalities of the proximal coronary artery segments [5].
Intravenous immunoglobulin (IVIG) combined with high-dose aspirin is the first choice for suppressing systemic inflammation and preventing CAA. In our latest study, white blood cells counts (WBC), absolute neutrophil counts (ANC), CRP and procalcitonin (PCT) levels markedly increased in the acute episode of KD, whereas declined to 30%~ 90% after IVIG treatment [1]. On the other hand, a multi-center, randomized trial from USA documented that timely initiation of IVIG treatment could reduce the incidence of CAA from 20 to 6.8% at the two-week visit [6]. Nevertheless, patients with a delayed diagnosis may still be candidates for IVIG treatment. Qiu et al. [7] analyzed inflammatory mediators and risk factors for CAA in 59 KD children who received IVIG treatment > 10 days and found that a delayed IVIG treatment may contribute to the higher levels of CRP and ESR, and serve as an independent risk factor for the development of CAA (adjusted OR = 2.90, 95%CI = 1.42, 5.91). Despite IVIG plus high-dose aspirin is considered as the first-line treatment, some KD patients develop recrudescent or persistent fever more than 36 h after the end of IVIG infusion and are termed IVIG non-response [3]. In this condition, another 2 g/kg dose of IVIG plus a corticosteroid is usually advocated [8].
Several previous epidemiologic surveys have suggested the onset of incomplete KD experiences an increasing trend in China. A long-term retrospective study from Inner Mongolia revealed that the incidence of incomplete KD increased from 10.38% in 2003 to 40.12% in 2012 [9]. In the last decade, the incidence of IVIG non-response ranged from 4.9 to 17.8% [2, 10, 11]. Based on several epidemiological surveys from mainland China, the overall trend in CAA occurrence also appeared to be on the rise from 15.9 to 63.3%, far higher than the other Asian countries [2, 12, 13]. Several published scoring systems have revealed that age in months, CRP and ESR were associated with incomplete KD; day of illness at initial treatment, age in months, percentage of neutrophils, platelet count (PLT), serum aspartate aminotransferase, sodium and CRP served as independent predictors of IVIG non-response; male, fever duration, albumin, percentage of eosionphils and monocytes predicted CAA risks [11, 14,15,16]. In addition, the enhancement of pediatricians’ awareness may raise the diagnostic rate of incomplete KD and stimulate more aggressive initial therapy in the acute episode of KD. Given this background, we hypothesize that the time option of IVIG treatment should be in parallel with peak time of systemic inflammation; either earlier or later IVIG treatment may affect the clinical classification, therapeutic responsiveness and CAA occurrence in KD patients. Therefore, the major objective of the present study is to identify whether the time option of IVIG treatment could be associated with the clinical classification, therapeutic responsiveness and CAA occurrence in the acute episode of KD.
Materials and methods
Patient selection
The observational period of our study covered the time from July 2015 to May 2018. Therefore, the sample size was completely dependent on the total number of KD patients admitted to our center in this period. After retrospectively reviewing all the medical records, 153 KD patients were involved eventually. Approval for this study was acquired from the Medical Ethic Committee of Anhui Medical University and informed consent was obtained from all parents before study entry. According to AHA guidelines [17], the diagnosis of complete KD is based on the presence of ≥5 days of fever and ≥ 4 of the following five signs: (1) bilateral conjunctival injection without exudates; (2) changes in the oral mucosa, such as erythema and cracking lips, erythema of the pharynx, strawberry tongue; (3) changes in extremities, such as redness and swelling in the acute phase, periungual desquamation in the subacute phase; (4) polymorphous exanthema; (5) cervical lymphadenopathy, (≥1.5 cm in diameter), usually unilateral. Patients with fever for ≥5 days and at least 2 of the principal features were diagnosed as incomplete KD, if no other disease processes could explain the illness. All patients received the standard therapy of KD, including a single infusion of IVIG (2 g/kg) and aspirin (30–50 mg/kg/d). IVIG-nonresponsive KD was defined as persistent or recrudescent fever ≥36 h after completion of the initial IVIG infusion [17].
Laboratory analysis
Blood samples were collected from all subjects within 24 h pre-IVIG treatment, respectively. Venous blood (2 ml) was collected in a gel coagulation-promoting vacuum tube and centrifuged immediately at 2800 g for 15 min at room temperature, and plasma samples were stored at − 80 °C. WBC, ANC and PLT were performed using a flow cytometer (Sysmex XE-2100). ESR and CRP were determined by the Westergren method and immunoturbidimetry respectively.
Echocardiography
Echocardiography was performed during the period from 2 days to 14 days after IVIG treatment. Children unable to cooperate were sedated according to local practice. CAA is defined as a coronary artery having an internal diameter of at least 3 mm in Children < 5 years or at least 4 mm in children ≥5 years; or a segment with an internal diameter at least 1.5 times larger than that of an adjacent segment by echocardiogram [17]. Echocardiographic results were interpreted independently by 2 echocardiographers who were blinded to treatment assignment. A third reading was performed if necessary to resolve discordant interpretations.
Statistical analysis
The collected data were stratified with respect to the time of IVIG treatment. Normally distributed continuous data were expressed as mean ± standard deviation. Comparisons of the frequencies between groups were analyzed using Pearsons’ chi-square tests. Comparison of mean values between groups was carried out using the independent sample t-test. Comparison of mean values among groups was carried out using one-way ANOVA and post hoc analysis was calculated using the Student-Newman-Keuls test. Statistical significance was identified with a p value < 0.05. Statistical analysis was performed using the statistical package for social studies SPSS version 16.0.
Results
Demographic features
In the present study, 85 males and 68 females were diagnosed as having KD, with a mean age of 35.22 ± 30.22 months and a range from 3 months to 13 years
Clinical classification
All 5 classic diagnostic criteria for KD were met in 48 cases (31.37%), 4 criteria in 60 (39.22%), 3 criteria in 25 (16.34%), and 2 criteria in 20 (13.07%). Therefore, 108 children (70.59%) had complete KD, including 64 males and 44 females with the mean age of 36.43 ± 30.52 months; 45 children (29.41%) had incomplete KD, including 21 males and 24 females with the mean age of 32.33 ± 29.64 months. The mean age and male/female ratio were almost identical between different clinical phenotypes (p > 0.05).
IVIG treatment
Among 153 KD patients, 11 of them (7.19%) were identified as IVIG-nonresponsive KD and had persistent fever about 71.00 ± 12.27 h after IVIG treatment, including 4 males and 7 females with the mean age of 33.73 ± 27.46 months. In contrast, 142 patients were diagnosed with IVIG-responsive KD and exhibited a dramatic decrease in fever duration after IVIG treatment (8.13 ± 7.04 h, t = 8.470, p < 0.05), including 81 males and 61 females with the mean age of 35.34 ± 30.51 months.
Coronary artery involvement
According to the enlarged internal diameter of coronary artery, 10 KD patients (6.54%) were defined as having coronary arteritis during the whole observational period (left coronary artery: 3.34 ± 0.42 mm; right coronary artery: 2.93 ± 0.97 mm), including 7 males and 3 females with the mean age of 28.50 ± 23.96 months. In contrast, 143 patients (93.46%) had normal coronary artery after IVIG treatment (left coronary artery: 2.09 ± 0.37 mm, right coronary artery: 2.01 ± 0.33 mm), including 78 males and 65 females with the mean age of 35.69 ± 30.02 months.
Inflammatory mediators
Inflammatory mediators in patients with different types of KD are presented in Table 1. Plasma WBC was significantly increased in patients with IVIG-nonresponsive KD when compared with their IVIG-responsive counterparts (t = 2.000, p < 0.05); however, no significant differences in ANC, PLT, CRP and ESR were observed between the 2 groups (p > 0.05). Regardless incomplete KD and coronary arteritis existed or not, no significant differences were observed in WBC, ANC, PLT, CRP and ESR (p > 0.05).
Inflammatory mediators among different treatment time are illustrated in Fig. 1. As disease progression, the plasma levels of WBC, ANC, PLT, CRP and ESR markedly increased in the acute phase of KD. In the total patients, WBC, ANC, CRP and ESR reached the largest values on day 10, and significant differences were observed in WBC and CRP among different treatment time (F = 3.418, p < 0.05; F = 2.545, p < 0.05); more specifically, WBC increased time-dependently and reached statistical significance on day 8 (p < 0.05) and day 10 (p < 0.05) when comparing with day 5, and CRP also increased and reached statistical difference on day 6 (p < 0.05) and day 10 (p < 0.05) when comparing with day 5. To probe the influences of clinical classifications to inflammatory mediators, the total patients were divided into the complete KD group and the incomplete KD group at each treatment time. Compared with the complete KD group, WBC significantly increased in the incomplete group on day 7 (p < 0.05), ANC significantly increased in the incomplete group on day 5 and day 7 (p < 0.05), and CRP significantly increased in the incomplete group on day 5 (p < 0.05).
The distribution of inflammatory mediators among different treatment time. *p < 0.05, inflammatory mediators increased time-dependently and reached statistical significance. ※p < 0.05, inflammatory mediators significantly increased in the incomplete group. a WBC increased time-dependently and reached statistical significance on day 8 and day 10 when comparing with day 5 (*p < 0.05). WBC significantly increased in the incomplete group on day 7 (※p < 0.05). b ANC significantly increased in the incomplete group on day 5 and day 7 (※p < 0.05). d CRP increased time-dependently and reached statistical significance on day 6, day 10 and after 10 days when comparing with day 5 (*p < 0.05). CRP significantly increased in the incomplete group on day 5 (※p < 0.05). There were no significant differences were found in PLT (c) and ESR (e) among different treatment time
Timing option of IVIG treatment & clinical classification
Pearsons’ chi-square test was conducted to observe the association of IVIG treatment with clinical classification Table 2. According to the timing option of IVIG treatment, 140 KD patients (91.50%) received the initial IVIG treatment within 10 days of illness, including 50 cases (32.68%) on day five, 46 cases (30.06%) on day six, 22 cases (14.38%) on day seven, 14 cases (9.15%) on day eight, 6 cases (3.92%) on day nine, and 2 cases (1.31%) on day ten; in addition, there were still 13 cases (8.50%) receiving the initial IVIG treatment after 10 days of illness. However, the clinical classification presented no significant heterogenicity among different treatment time (x2 = 1.59, p > 0.05), thus the earlier IVIG treatment appeared not to relate to the onset of incomplete KD.
Timing option of IVIG treatment & CAA
In the present study, 10 KD patients were defined as having CAA in the acute stage. According to the timing option of IVIG treatment, 7 of them received the initial IVIG treatment within 10 days of illness, including 2 cases on day five, 2 cases on day six, 1 case on day eight and 2 cases on day nine; in addition, there were still 3 cases receiving the initial IVIG treatment after 10 days of illness. The distribution of CAA onset was subjected to a significant difference according to timing option of IVIG treatment (x2 = 11.94, p < 0.05).
Discussion
IVIG is a well-established standard therapy for KD and effectively reduces systemic inflammation [3]. Furthermore, IVIG treatment is effective in shortening the length of hospital stay and preventing undesirable cardiac events in KD patients. Klassen et al. [18] compared the length of hospital stay and cost effectiveness in 100 KD patients with different treatment strategies, and discovered that the hospitalization time (3 days) was significantly shorter and the total medical expense ($118,200) was significantly lower in the IVIG high-dose group than those in the aspirin alone group (10 days and $323,400). In another retrospective study, Bal et al. [19] identified the risks for development and delay in resolution of CAA in association with IVIG administration within or after 10 days of KD onset. The risk for CAA was significantly lower among these patients admitted within 10 days (OR = 3.1) in comparison with their counterparts received IVIG after 10 days (OR = 5.3); and the resolution time of CAA was significantly shorter among these patients admitted within 10 days than their counterparts (6 months vs.12 months). In the present study, we observed that the duration of fever decreased dramatically after the initial IVIG treatment in 142 KD patients, which was mainly attributed to the depressed systemic inflammation. Besides, the potential mechanisms of IVIG treatment may include several immunoregulative processes. Lau et al. [20] established a murine model of KD to examine the effect of IVIG, and showed that IVIG inhibited T cell proliferation, tumor necrosis factor-α production and nuclear factor (NF) -κB activation in a dose-dependent manner, all of which are critical steps preventing coronary artery damage.
Although IVIG is highly effective in KD, approximately 10 to 20% of KD patients develop recrudescent or persistent fever at least 36 h after the end of their IVIG infusion [21]. To date, the immunologic basis of IVIG non-response remains unknown. Several studies have documented that the single-nucleotide polymorphisms in STX1B and carcinoembryonic antigen-related cell adhesion molecule 1 play a vital role in IVIG non-response [22, 23]. In the present study, 11 KD patients resisted to IVIG treatment and 7 of them (63.60%) received the initial IVIG dose on day 5 and 6. Similarly, a multi-institutional, retrospective cohort study from Japan indicated that the early treatment group (on day 4) had a significantly higher rate of IVIG non-response than the conventional treatment group [24]. Therefore, earlier intervention before peak time of systemic inflammation may contribute to IVIG non-reponse.
As outlined in the 2017 AHA guidelines [3], KD is accompanied by the gradual elevations of WBC, ANC, CRP and ESR time-dependently in the acute stage. Consistently, the present study also showed that WBC, ANC, CRP and ESR reached the largest values on day 10. In California, Tremoulet et al. [25] performed a retrospective chart review of 380 KD patients and found that ANC and CRP peaked within the first 10 days of illness, whereas PLT peaked between day 11 and day 20. Lee et al. [26] evaluated the inflammatory mediators according to the fever duration in 152 Korean children with KD and discovered that WBC, ANC and CRP reached their summits on day 6, earlier than our findings. Therefore, understanding the dynamic changes in laboratory parameters may assist pediatricians in evaluating the inflammatory status of KD patients.
The presence of fever for ≥5 days with 4 of the 5 other principal features fulfills the diagnosis of complete KD, whereas the above criteria unfortunately do not identify all children with the illness. According to the current available data, approximately 20 to 40% of patients are diagnosed with incomplete KD [27, 28]. In this study, 45 patients developed incomplete KD (29.40%) and 27 of them (60.00%) received the initial IVIG dose on day 5 and 6. However, the clinical classification presented no significant heterogenicity among different treatment time, thus early recognition to incomplete KD seemed to be relatively challenging. Identically, Sittiwangkul et al. [29] analyzed the medical records of 170 KD patients in Thailand from 2000 to 2008 and found that timing option of IVIG treatment was not associated with the onset of incomplete KD. In contrast, another clinical survey from Wenzhou [7], China revealed that the proportion of incomplete KD in the delayed therapy group (received IVIG treatment > 10 days) was significantly higher than in the conventional therapy group (received IVIG treatment ≤10 days).
CAA serves as a predictor to the long-term prognosis of KD. Currently, several inflammatory mediators, such as NF-κB, interleukin (IL)-1β, IL-6, fibroblast growth factor-23 and transforming growth factor-β, have been reported to participate in CAA onset [30,31,32]. Besides, a growing body of evidence have shown that SLC8A1, male, infants < 6 months old, low serum albumin, high ESR, CRP, mycoplasma infection, IVIG started after the 10th day of illness and IVIG non-responders may increase the risk of CAA [33,34,35]. In the present study, the distribution of CAA onset was subjected to a significant difference according to timing option of IVIG treatment; a subsequent usage of IVIG may result in a higher occurrence of CAA and a more severe vasculitis requires more aggressive therapy. More persuasively, according to the 20th nationwide survey of KD in Japan [36], CAA incidence during the convalescent phase was significantly higher in the late IVIG treatment group (≥10 days) than those who received IVIG treatment within day 10. Therefore, the early treatment of IVIG is considered to be effective for suppressing systemic inflammation and preventing CAA.
Conclusions
The time option of IVIG treatment is associated with therapeutic responsiveness and CAA but not with clinical classification in the acute episode of KD.
Availability of data and materials
The datasets generated and/or analysed during current study are available from the corresponding author on reasonable request.
Abbreviations
- AHA:
-
American Heart Association
- ANC:
-
absolute neutrophil counts
- CAA:
-
coronary artery abnormalities
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- IVIG:
-
Intravenous immunoglobulin
- KD:
-
Kawasaki disease
- PCT:
-
Procalcitonin
- WBC:
-
White blood cells counts
References
Hu P, Jiang GM, Wu Y, Huang BY, Liu SY, Zhang DD, et al. TNF-α is superior to conventional inflammatory mediators in forecasting IVIG nonresponse and coronary arteritis in Chinese children with Kawasaki disease. Clin Chim Acta. 2017;471:76–80.
Chen JJ, Ma XJ, Liu F, Yan WL, Huang MR, Huang M, et al. Shanghai Kawasaki disease research group. Epidemiologic features of Kawasaki disease in Shanghai from 2008 through 2012. Pediatr Infect Dis J. 2016;35:7–12.
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term Management of Kawasaki Disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–99.
Xiu-Yu S, Jia-Yu H, Qiang H, Shu-Hui D. Platelet count and erythrocyte sedimentation rate are good predictors of Kawasaki disease: ROC analysis. J Clin Lab Anal. 2010;24:385–8.
Capannari TE, Daniels SR, Meyer RA, Schwartz DC, Kaplan S. Sensitivity, specificity and predictive value of two-dimensional echocardiography in detecting coronary artery aneurysms in patients with Kawasaki disease. J Am Coll Cardiol. 1986;7:355–60.
Newburger JW, Takahashi M, Burns JC, Beiser AS, Chung KJ, Duffy CE, et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986;315:341–7.
Qiu H, He Y, Rong X, Ren Y, Pan L, Chu M, et al. Delayed intravenous immunoglobulin treatment increased the risk of coronary artery lesions in children with Kawasaki disease at different status. Postgrad Med. 2018;130:442–7.
Eleftheriou D, Levin M, Shingadia D, Tulloh R, Klein NJ, Brogan PA. Management of Kawasaki disease. Arch Dis Child. 2014;99:74–83.
Zhu H, Yu SF, Bai YX, Liang YY, Su XW, Pan JY. Kawasaki disease in children: epidemiology, clinical symptoms and diagnostics of 231 cases in 10 years. Exp Ther Med. 2015;10:357–61.
Tan XH, Zhang XW, Wang XY, He XQ, Fan C, Lyu TW, Tian J. A new model for predicting intravenous immunoglobin-resistant Kawasaki disease in Chongqing: a retrospective study on 5277 patients. Sci Rep. 2019;9:1722.
Hua W, Ma F, Wang Y, Fu S, Wang W, Xie C, Zhang Y, Gong F. A new scoring system to predict Kawasaki disease with coronary artery lesions. Clin Rheumatol. 2019;38:1099–107.
Zhang X, Liang Y, Feng W, Su X, Zhu H. Epidemiologic survey of Kawasaki disease in Inner Mongolia, China, between 2001 and 2013. Exp Ther Med. 2016;12:1220–4.
Zhang X, Zhang Z, Liu S, Sun J. Epidemiologic survey of Kawasaki disease in Jilin from 1999 through 2008. Pediatr Cardiol. 2012;33:272–9.
Liu HC, Lo CW, Hwang B, Lee PC. Clinical manifestations vary with different age spectrums in infants with Kawasaki disease. ScientificWorldJournal. 2012;2012:210382.
Bai L, Feng T, Yang L, Zhang Y, Jiang X, Liao J, et al. Retrospective analysis of risk factors associated with Kawasaki disease in China. Oncotarget. 2017;8:54357–63.
Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, Kobayashi T, Morikawa A. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006;113:2606–12.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004;114:1708–33.
Klassen TP, Rowe PC, Gafni A. Economic evaluation of intravenous immune globulin therapy for Kawasaki syndrome. J Pediatr. 1993;122:538–42.
Bal AK, Prasad D, Umali Pamintuan MA, Mammen-Prasad E, Petrova A. Timing of intravenous immunoglobulin treatment and risk of coronary artery abnormalities in children with Kawasaki disease. Pediatr Neonatol. 2014;55:387–92.
Lau AC, Duong TT, Ito S, Yeung RS. Intravenous immunoglobulin and salicylate differentially modulate pathogenic processes leading to vascular damage in a model of Kawasaki disease. Arthritis Rheum. 2009;60:2131–41.
Newburger JW, Sleeper LA, McCrindle BW, Minich LL, Gersony W, Vetter VL, et al. Randomized trial of pulsed corticosteroid therapy for primary treatment of Kawasaki disease. N Engl J Med. 2007;356:663–75.
Shendre A, Wiener HW, Zhi D, Vazquez AI, Portman MA, Shrestha S. High-density genotyping of immune loci in Kawasaki disease and IVIG treatment response in European-American case-parent trio study. Genes Immun. 2014;15:534–42.
Popper SJ, Shimizu C, Shike H, Kanegaye JT, Newburger JW, Sundel RP, et al. Gene-expression patterns reveal underlying biological processes in Kawasaki disease. Genome Biol. 2007;8:R261.
Shiozawa Y, Inuzuka R, Shindo T, Mafune R, Hayashi T, Hirata Y, et al. Effect of i.v. immunoglobulin in the first 4 days of illness in Kawasaki disease. Pediatr Int. 2018;60:334–41.
Tremoulet AH, Jain S, Chandrasekar D, Sun X, Sato Y, Burns JC. Evolution of laboratory values in patients with Kawasaki disease. Pediatr Infect Dis J. 2011;30:1022–6.
Lee KY, Han JW, Hong JH, Lee HS, Lee JS, Whang KT. Inflammatory processes in Kawasaki disease reach their peak at the sixth day of fever onset: laboratory profiles according to duration of fever. J Korean Med Sci. 2004;19:501–4.
Yellen ES, Gauvreau K, Takahashi M, Burns JC, Shulman S, Baker AL, et al. Performance of 2004 American Heart Association recommendations for treatment of Kawasaki disease. Pediatrics. 2010;125:e234–41.
Liu YC, Lin MT, Wang JK, Wu MH. State-of-the-art acute phase management of Kawasaki disease after 2017 scientific statement from the American Heart Association. Pediatr Neonato. 2018;30592-2:S1875–9572.
Sittiwangkul R, Pongprot Y, Silvilairat S, Phornphutkul C. Delayed diagnosis of Kawasaki disease: risk factors and outcome of treatment. Ann Trop Paediatr. 2011;31:109–14.
Matsuda A, Morita H, Unno H, Saito H, Matsumoto K, Hirao Y, et al. Anti-inflammatory effects of high-dose IgG on TNF-α-activated human coronary artery endothelial cells. Eur J Immunol. 2012;42:2121–31.
Masi L, Franceschelli F, Leoncini G, Gozzini A, Rigante D, La Torre F, et al. Can fibroblast growth factor (FGF)-23 circulating levels suggest coronary artery abnormalities in children with Kawasaki disease? Clin Exp Rheumatol. 2013;31:149–53.
Shimizu C, Jain S, Davila S, Hibberd ML, Lin KO, Molkara D, et al. Transforming growth factor-beta signaling pathway in patients with Kawasaki disease. Circ Cardiovasc Genet. 2011;4:16–25.
Shimizu C, Eleftherohorinou H, Wright VJ, Kim J, Alphonse MP, Perry JC, et al. Genetic variation in the SLC8A1 calcium signaling pathway is associated with susceptibility to Kawasaki disease and coronary artery abnormalities. Circ Cardiovasc Genet. 2016;9:559–68.
Salgado AP, Ashouri N, Berry EK, Sun X, Jain S, Burns JC, et al. High risk of coronary artery aneurysms in infants younger than 6 months of age with Kawasaki disease. J Pediatr. 2017;185:112–6.
Tang Y, Gao X, Shen J, Sun L, Yan W. Epidemiological and clinical characteristics of Kawasaki disease and factors associated with coronary artery abnormalities in East China: nine years experience. J Trop Pediatr. 2016;62:86–93.
Muta H, Ishii M, Yashiro M, Uehara R, Nakamura Y. Late intravenous immunoglobulin treatment in patients with Kawasaki disease. Pediatrics. 2012;129:e291–7.
Acknowledgments
At the point of finishing this paper, I’d like to express my sincere thanks to all those who have lent me hands in the course of my writing this paper. We greatly appreciate PhD. Xun Xia, Dr. Bo Hu and Dr. Wei Wei for their helpful comments, Department of Pediatrics, the First Affiliated Hospital of Anhui Medical University, Hefei, China.
Funding
No.
Author information
Authors and Affiliations
Contributions
PH conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. SS, FFL, GM and JJW drafted the manuscript. HHLi, Yang Fang Wu, HHLu and YW carried out the initial analyses. WXC, DDZ and WW collected literatures. All authors have seen and approved the final version of the manuscript being submitted. The article is the authors’ original work, hasn’t received prior publication and isn’t under consideration for publication elsewhere.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Research Ethics Commission of the First Affiliated Hospital of Anhui Medical University. Permission to carry out the study and access patient records was sought from the respective hospital administrators.
Consent for publication
No applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Samadli, S., Liu, F.F., Mammadov, G. et al. The time option of IVIG treatment is associated with therapeutic responsiveness and coronary artery abnormalities but not with clinical classification in the acute episode of Kawasaki disease. Pediatr Rheumatol 17, 53 (2019). https://doi.org/10.1186/s12969-019-0352-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-019-0352-3