Abstract
Background
The prognostic impact of surgical paraaortic staging remains unclear in patients with locally advanced cervical cancer (LACC). The objective of our study was to evaluate the survival impact of surgical staging in patients with LACC and no evidence of paraaortic lymph node (PALN) metastasis on pre-operative imaging work-up.
Methods
Data of 1447 patients with cervical cancer treated between 1996 and 2016 were extracted from maintained databases of 10 French University hospitals. Patients with locally advanced disease (IB2 or more) treated by concurrent chemoradiation therapy (CRT) and no evidence of paraaortic metastasis on pre-operative imaging work-up were selected for further analysis. The Kaplan–Meier method was used to estimate the survival distribution. A Cox proportional hazards model was used to account for the influence of multiple variables.
Results
Six hundred and forty-seven patients were included, 377 (58.3%) with surgical staging and 270 (41.7%) without, with a mean follow up of 38.1 months (QI 13.0–56.0). Pathologic analysis revealed positive lymph nodes in 47 patients (12.5%). In multivariate model analysis, surgical staging remained an independent prognostic factor for DFS (OR 0.64, CI 95% 0.46–0.89, p = 0.008) and OS (OR 0.43, CI 95% 0.27–0.68, p < 0.001). The other significant parameter in multivariate analysis for both DFS and OS was treatment by intracavitary brachytherapy (OR respectively of 0.7 (0.5–1.0) and 0.6 (0.4–0.9), p < 0.05).
Conclusion
Nodal surgical staging had an independent positive impact on survival in patients with LACC treated with CRT with no evidence of metastatic PALN on imaging.
Similar content being viewed by others
Background
Cervical cancer is the third most common cancer in women worldwide and around half of the patients are diagnosed with locally advanced cervical cancer (LACC) [1]. After multiple phase III studies demonstrated that concurrent chemoradiotherapy improved overall survival (OS) in patients with LACC, current guidelines recommend chemoradiation therapy (CRT) as the standard treatment for these patients [1, 2].
The latest FIGO classification for cervical cancer do not include lymph node status [3] despite considerable evidence reporting a major impact on prognosis [4, 5]. This may be because developing countries—where the incidence of cervical cancer is the highest—cannot afford imaging techniques such as positron emission tomography–computed tomography (PET-CT). However, determining paraaortic lymph node (PALN) status would appear to be of paramount importance to tailor adjuvant concurrent chemoradiation therapy (CRT) and personalize the fields of radiation [6, 7]. Personalized radiation fields are mandatory to prevent unnecessary radiation and the associated morbidity.
The debate about the most effective way to assess PALN status is ongoing. On one hand, imaging exams are non-invasive but lacks sensitivity for detecting PALN metastasis especially in cases of micrometastases [8]. On the other hand, surgical staging is invasive but is associated with a low rate of complications in well-trained teams [9] and provides robust results for PALN evaluation. The prognostic impact of surgical paraaortic staging remains unclear in patients with LACC and there are some discrepancies in the scientific literature regarding this issue [10,11,12]. The benefit of correctly identifying a higher proportion of patients with PALN by surgical staging could be tempered by a delay in initiating CRT and surgical morbidity [11]. It is thus important to determine whether surgical staging has any impact on survival and disease recurrence.
The objective of our study was to evaluate the survival impact of paraaortic nodal surgical staging in patients with LACC and no evidence of PALN metastasis on pre-operative imaging work-up.
Methods
We conducted a retrospective study using maintained databases from 10 French institutions (Creteil University Hospital, Tenon University Hospital, Poissy University Hospital, Reims University Hospital, Lille University Hospital, Tours University Hospital, Bondy University Hospital, Rennes University Hospital, and Marseille Public Hospital North). These databases registered all patients diagnosed with cervical cancer at any stage between January 1996 and December 2016. The research protocol was approved by the Institutional Review Board (IRB) of the French College of Obstetrics and Gynaecology (CEROG 2016-GYN-0502).
Patients with locally advanced cervical cancer (LACC) treated with CRT and no distant or para-aortic invaded nodes on pre-treatment computed tomography scanner (CT-scan) or PET-CT were selected for further analysis. LACC was defined as patients with at least stage IB2 according to the latest 2009 International Federation of Gynecology and Obstetrics (FIGO) classification. Exclusion criteria were: patients with stage IVB; patients treated by radiotherapy only; and patients with missing data for surgical staging.
The decision to perform surgical paraaortic staging or other complementary therapies (extended field radiotherapy, intracavitary brachytherapy, completion surgery) was center–driven. As for all aspects of patient management, the decision was made within a multidisciplinary committee and was based on both patient and tumor characteristics. During surgical para-aortic staging, all of the lymphatic tissue from the aorta was removed from the iliac bifurcation to the left renal vein. Pelvic lymphadenectomy was not routinely performed since the area is covered by traditional pelvic radiation fields. All patients were subsequently treated by CRT and received pelvic conformational radiotherapy at the total dose of 45 Grays (25 fractions) in 5 weeks with a concomitant 40 mg/m2 weekly base of cisplatinium ± 5FU in some centers. Some patients received intracavitary brachytherapy (15 grays) to complete pelvic conformational radiotherapy.
Patients with positive nodes after surgical staging were supposed to receive an extension of the radiation fields in the paraaortic region. However, some patients without surgical para-aortic staging also received paraaortic radiation therapy in the case of pelvic lymph node involvement on PET-CT. Some centers commonly performed completion surgery (hysterectomy) following RCT in patients with residual disease.
Follow-up protocol included a gynecologic examination every 3 months for 2 years and then every 6 months for 2 years. Magnetic resonance imaging (MRI) or a PET-CT scan were performed when clinically indicated. Recurrences were diagnosed either on biopsy or with an imaging exam.
According to previous reports, we applied the following definitions to stratify the sites of recurrence: (i) local recurrence was defined as a vaginal or central pelvic location without lymph node involvement; (ii) regional recurrence was defined as a non-central pelvic location or a peritoneal carcinomatosis and no lymph node involvement; (iii) nodal recurrence included pelvic and/or paraaortic nodal locations; (iv) distant recurrence included distant metastasis (bone, liver, lung and brain); (v) multiple site recurrence included any combination of the locations mentioned above.
The date of the end of primary treatment was used to calculate disease free survival (DFS) and OS.
Databases were managed using Excel (Microsoft Corporation, Redmond, WA, USA) and statistical analyses were performed using R software (3.3.1 version, available online). Statistical analysis was based on the Student’s t test for continuous variable and the χ2 test or Fisher’s exact test for categorical variables. The Kaplan–Meier method was used to estimate the survival distribution. Comparisons of survival were made using the log rank test. A Cox proportional hazards model including all the parameters statistically significant in univariate analysis, was used to account for the influence of multiple variables. Values of p < 0.05 were considered to denote significant differences.
Results
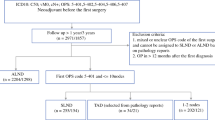
Between 1996 and 2016, 1447 patients were treated for cervical cancer within our institutions. Among them, 647 fulfilled the inclusion criteria and were included for analysis: of these, 377 had undergone surgical staging and 270 had not (Fig. 1).
The main characteristics of the patients included are presented in Table 1. Two hundred and seventy-six patients (42.7%) had a pre operative CT-scan to assess lymph nodes status and 371 (57.3%) a PET-CT. Most patients had a tumor > 4 cm and 53% received intracavitary brachytherapy. Surgical staging was laparoscopic in all but five patients (2 laparotomy, 1 robot assisted, 2 laparoscopy converted during procedure to open laparotomy). Eighteen patients (4.8%) experienced per-operative complications (mostly vascular) and 50 (13.3%) postoperative complications of any severity. Among the patients with surgical staging, 47 (12.5%) had positive paraaortic lymph nodes on final pathologic analysis.
Survival analysis
Mean follow up was 38.1 months (QI 13.0–56.0). During follow up, 140 patients died: 53 patients (14.1%) with surgical staging and 87 (32.2%) without. Two hundred and two patients experienced recurrance during follow up: 102 with surgical staging and 100 without. Surgical staging was significantly associated with better DFS and OS than clinical staging (p < 0.001) (Figs. 2 and 3). Para-aortic radiotherapy boost was not associated with a difference in survival. Patterns of recurrence are presented in Table 2. There were no differences in the site of recurrence between patients with and without surgical staging. Most patients had either local, distant or multiple site metastases. Within patients that had surgical paraaortic lymph nodes staging, patients with histologically confirmed lymph nodes metastases had significantly worse overall survival than those with no evidence of metastases on final pathological analysis (p < 0.01) (Additional file 1: Figure S1).
Multivariate model analysis
Results of the multivariate model analysis for factors influencing DFS and OS are presented in Table 3. Surgical staging remained an independent prognostic factor for DFS (OR 0.64, CI 95% 0.46–0.89, p = 0.008) and OS (OR 0.43, CI 95% 0.27–0.68, p < 0.001) in multivariate analysis. The other parameter that remained significant for both DFS and OS was treatment by intracavitary brachytherapy associated with CRT (respectively OR 0.7 (0.5–1.0) p = 0.04 and 0.6 (0.4–0.9) p = 0.02). This parameter was not different in the two study groups (p = 0.24).
Discussion
Our study shows that surgical paraaortic staging is associated with increased OS and DFS in patients with LACC treated with CRT and with no evidence of PALN metastasis on pre operative imaging.
We believe that two parameters are responsible for fueling the debate around this controversy that has lasted for many years. The first is the confusing role of the pre-operative imaging in the initial assessment of patients with LACC, and the second is the role of extended radiation fields in these patients.
As mentioned in the introduction, current FIGO classification is based on clinical staging. However, in developed countries, most patients have a CT-scan or a PET-CT pre-operatively to assess initial disease spread with high true positive value for identification of positive lymph nodes, especially for PET-CT [13]. When PET-CT shows an uptake in the paraaortic area, extended radiation fields should be applied and surgical staging would seem to be at best unnecessary and at worst harmful. False negative rates for PET-CT in the paraaortic area have been reported to be as high as 13% in patients with LACC [12, 14,15,16,17] with a low sensitivity of detection of small node disease: 22% if histologically confirmed PA nodal metastasis < 5 mm in size [15] as well as failure to identify most patients with peritoneal disease. This underlines the lack of sensitivity of PET-CT for small volume metastases in PALN. Our inclusion criteria resulted in selecting patients either without metastases or with small volume metastases only. In this population, surgical staging would increase occult metastasis detection. Increased DFS and OS in patients with surgical staging clearly demonstrate the therapeutic effect of PALN dissection. In our cohort, 47 patients (12.5%) had positive PALN on final pathologic analysis and these patients, with small volume metastases, probably benefited the most from the surgical staging.
In our cohort, only a small proportion of patients had an extended radiation field in the paraaortic area (23.6%) and this proportion was similar in patients with and without surgical staging. The decision of whether to apply extended radiation fields was thus not based on the results of the surgical staging. As mentioned by Pomel et al. [18], no study has shown a clear benefit of extended field radiotherapy on survival following the introduction of cisplatin systemic therapy in the initial management of patients with LACC [19]. The benefit of surgical staging in patients with negative preoperative workup seems to be independent of the extent of the radiation fields. Moreover, patterns of recurrence in patients with or without surgical staging are similar, with most recurrences occurring locally or at distant sites. Such patterns emphasize the need to improve local tumor-control in patients with LACC.
We recognize that the retrospective nature of our study limits the generalization of our findings. However, this cohort is the largest ever reported and large multicenter cohorts are of utmost importance to accumulate evidence to resolve this long-standing controversy. Patients in our cohort had either a CT-scan or a PET-CT pre operatively despite the fact PET-CT is known a higher sensitivity for detecting lymph nodes metastases. Our choice to also include patients with CT-scan was driven by the fact that most centers do not have routinely access to PET-CT pre-operatively. Because of the retrospective nature of our study, data regarding recurrences’ management was not available. As we report the therapeutic benefit of surgical paraaortic dissection prior to initiation of concomitant radio-chemotherapy, salvage paraaortic lymph nodes removal in patients experiencing lymph nodal recurrence using minimally invasive surgery could be a valid therapeutic approach as recently suggested by Gallotta et al. [20].
A commonly used argument against surgical staging is the subsequent delay in starting concomitant chemo-radiotherapy. We were not able to evaluate this parameter but in light of our results, with increased survival rates in patients with surgical staging, it is safe to think that this hypothesis can be ruled out. This is all the more true when taking into consideration that others have reported no significant delays in starting chemoradiation therapy in these patients [21]. Finally, while surgical morbidity in our cohort was acceptable, most of the participating centers have a considerable expertise in laparoscopic staging in gynecologic malignancies. Generalization of surgical staging to centers with less experience might result in greater morbidity with a negative impact on survival. Recently, some authors developed nomograms to predict paraaortic lymph nodes invasion in patients with locally advanced cervical cancer. As this approach might be of interest, these nomograms usually lack of sensitivity and are not validated in prospective cohort yet [22].
The complex interactions between the different variables determining prognosis, have delayed initiation of a randomized controlled trial to answer the issue. The LILACS study by Frumovitz et al. [23] should bring interesting results and provide us with some answers. To date, the only randomized trial, conducted by Lai et al. [11], concluded that clinical staging led to better DFS and OS than surgical staging. However, this study has been highly criticized with major differences in patient characteristics between the groups and more patients receiving concurrent chemotherapy in the radiologically staged group compared with the surgically staged group. The trial was ended prematurely without reaching its primary endpoint. On the other hand, some retrospective studies have suggested a positive survival impact of surgical staging [10, 24]. Our study is in line with these and, by virtue of including more patients than the previous studies, could serve as a basis to design further prospective trials.
Conclusion
We found surgical staging had a therapeutic value in women with node metastases not detected on pre-operative imaging, with significant improvement in DFS and OS achieved by tailoring radiation therapy plans or modifying planned therapy, and identifying patients with peritoneal spread. This benefit could vary from one patient to another due to the numerous therapeutic factors involved in improving survival, as well as from one center to another as experience in laparoscopic staging is a determining factor to limit associated morbidity. Further studies should help select patients that will benefit the most from surgical staging.
References
Colombo N, Carinelli S, Colombo A, Marini C, Rollo D, Sessa C, et al. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii27–32.
Koh W-J, Greer BE, Abu-Rustum NR, Apte SM, Campos SM, Cho KR, et al. Cervical Cancer, Version 2.2015. J Natl Compr Cancer Netw. 2015;13(4):395–404.
Hwang L, Bailey A, Lea J, Albuquerque K. Para-aortic nodal metastases in cervical cancer: a blind spot in the International Federation of Gynecology and Obstetrics staging system: current diagnosis and management. Future Oncol. 2015;11(2):309–22.
Kim HS, Song YS. International Federation of Gynecology and Obstetrics (FIGO) staging system revised: what should be considered critically for gynecologic cancer? J Gynecol Oncol. 2009;20(3):135–6.
Stehman FB, Bundy BN, DiSaia PJ, Keys HM, Larson JE, Fowler WC. Carcinoma of the cervix treated with radiation therapy. I. A multi-variate analysis of prognostic variables in the Gynecologic Oncology Group. Cancer. 1991;67(11):2776–85.
Marnitz S, Köhler C, Roth C, Füller J, Hinkelbein W, Schneider A. Is there a benefit of pretreatment laparoscopic transperitoneal surgical staging in patients with advanced cervical cancer? Gynecol Oncol. 2005;99(3):536–44.
Hasenburg A, Salama JK, Van TJ, Amosson C, Chiu JK, Kieback DG. Evaluation of patients after extraperitoneal lymph node dissection and subsequent radiotherapy for cervical cancer. Gynecol Oncol. 2002;84(2):321–6.
Choi HJ, Roh JW, Seo S-S, Lee S, Kim J-Y, Kim S-K, et al. Comparison of the accuracy of magnetic resonance imaging and positron emission tomography/computed tomography in the presurgical detection of lymph node metastases in patients with uterine cervical carcinoma: a prospective study. Cancer. 2006;106(4):914–22.
Smits RM, Zusterzeel PLM, Bekkers RLM. Pretreatment retroperitoneal para-aortic lymph node staging in advanced cervical cancer: a review. Int J Gynecol Cancer. 2014;24(6):973–83.
Leblanc E, Katdare N, Narducci F, Bresson L, Gouy S, Morice P, et al. Should systematic infrarenal para-aortic dissection be the rule in the pretherapeutic staging of primary or recurrent locally advanced cervix cancer patients with a negative preoperative para-aortic PET imaging? Int J Gynecol Cancer. 2016;26(1):169–75.
Lai C-H, Huang K-G, Hong J-H, Lee C-L, Chou H-H, Chang T-C, et al. Randomized trial of surgical staging (extraperitoneal or laparoscopic) versus clinical staging in locally advanced cervical cancer. Gynecol Oncol. 2003;89(1):160–7.
Gouy S, Morice P, Narducci F, Uzan C, Martinez A, Rey A, et al. Prospective multicenter study evaluating the survival of patients with locally advanced cervical cancer undergoing laparoscopic para-aortic lymphadenectomy before chemoradiotherapy in the era of positron emission tomography imaging. J Clin Oncol. 2013;31(24):3026–33.
Grigsby PW. The prognostic value of PET and PET/CT in cervical cancer. Cancer Imaging. 2008;8:146–55.
Haie-Meder C, Pötter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74(3):235–45.
Leblanc E, Gauthier H, Querleu D, Ferron G, Zerdoud S, Morice P, et al. Accuracy of 18-fluoro-2-deoxy-d-glucose positron emission tomography in the pretherapeutic detection of occult para-aortic node involvement in patients with a locally advanced cervical carcinoma. Ann Surg Oncol. 2011;18(8):2302–9.
Roh J-W, Seo SS, Lee S, Kang KW, Kim S-K, Sim JS, et al. Role of positron emission tomography in pretreatment lymph node staging of uterine cervical cancer: a prospective surgicopathologic correlation study. Eur J Cancer. 2005;41(14):2086–92.
Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012;13(5):e212–20.
Pomel C, Martinez A, Bourgin C, Beguinot M, Benoit C, Naik R, et al. Survival effect of laparoscopic para-aortic staging in locally advanced cervical cancer: a retrospective cohort analysis. BJOG Int J Obstet Gynaecol. 2017. https://doi.org/10.1111/1471-0528.14492.
Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90-01. J Clin Oncol. 2004;22(5):872–80.
Gallotta V, Giudice MT, Conte C, Sarandeses AV, D’Indinosante M, Federico A, et al. Minimally invasive salvage lymphadenectomy in gynecological cancer patients: a single institution series. Eur J Surg Oncol. 2018;44(10):1568–72.
Köhler C, Mustea A, Marnitz S, Schneider A, Chiantera V, Ulrich U, et al. Perioperative morbidity and rate of upstaging after laparoscopic staging for patients with locally advanced cervical cancer: results of a prospective randomized trial. Am J Obstet Gynecol. 2015;213(4):503.e1–7.
Shim S-H, Kim D-Y, Lee SJ, Kim S-N, Kang S-B, Lee S-W, et al. Prediction model for para-aortic lymph node metastasis in patients with locally advanced cervical cancer. Gynecol Oncol. 2017;144(1):40–5.
Frumovitz M, Querleu D, Gil-Moreno A, Morice P, Jhingran A, Munsell MF, et al. Lymphadenectomy in locally advanced cervical cancer study (LiLACS): phase III clinical trial comparing surgical with radiologic staging in patients with stages IB2-IVA cervical cancer. J Minim Invasive Gynecol. 2014;21(1):3–8.
Gold MA, Tian C, Whitney CW, Rose PG, Lanciano R. Surgical versus radiographic determination of para-aortic lymph node metastases before chemoradiation for locally advanced cervical carcinoma: a Gynecologic Oncology Group Study. Cancer. 2008;112(9):1954–63.
Authors’ contributions
Conceptualization: CT, BH, ED. Validation: SB. Formal analysis: YD, MB, VL, ER, CH. Investigation: MB, XC, SB, LO, GC, ER, CC, OG, PC, AB. Data curation: XC, CC, VS. Original draft: YD, VS, CT. Review: All authors. Visualization: PC, AB. Supervision: CT, BH, MB. All authors revised the manuscript for important intellectual content. All authors reviewed and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
CT has occasionally served as a consultant for TWA-ADELPHI. The other authors declare that they have no conflict of interest.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research protocol was approved by the Institutional Review Board (IRB) of the French College of Obstetrics and Gynaecology (CEROG 2016-GYN-0502). As our study was non interventional and retrospective, formal written consent from patients included was not necessary.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional file

Additional file 1: Figure S1.
Kaplan–Meier curve for overall survival in patients with surgical staging stratified by final pathological analysis of paraaortic lymph nodes. In black: patients without lymph nodes metastases. In red: patients with paraaortic lymph nodes metastases.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dabi, Y., Simon, V., Carcopino, X. et al. Therapeutic value of surgical paraaortic staging in locally advanced cervical cancer: a multicenter cohort analysis from the FRANCOGYN study group. J Transl Med 16, 326 (2018). https://doi.org/10.1186/s12967-018-1703-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-018-1703-4