Abstract
The treatment of cancer is becoming more precise, targeting specific oncogenic drivers with targeted molecular therapies. The epidermal growth factor receptor has been found to be over-expressed in a multitude of solid tumours. Immunohistochemistry is widely used in the fields of diagnostic and personalised medicine to localise and visualise disease specific proteins. To date the clinical utility of epidermal growth factor receptor immunohistochemistry in determining monoclonal antibody efficacy has remained somewhat inconclusive. The lack of an agreed reproducible scoring criteria for epidermal growth factor receptor immunohistochemistry has, in various clinical trials yielded conflicting results as to the use of epidermal growth factor receptor immunohistochemistry assay as a companion diagnostic. This has resulted in this test being removed from the licence for the drug panitumumab and not performed in clinical practice for cetuximab. In this review we explore the reasons behind this with a particular emphasis on colorectal cancer, and to suggest a way of resolving the situation through improving the precision of epidermal growth factor receptor immunohistochemistry with quantitative image analysis of digitised images complemented with companion molecular morphological techniques such as in situ hybridisation and section based gene mutation analysis.
Similar content being viewed by others
Background
Personalised cancer medicine, depends upon and requires a detailed analysis of both immunohistochemical and molecular therapeutic targets. Over the last decade, emphasis has shifted from empirical treatment of patients to a biomarker-led, precision approach. Scientific discoveries in carcinogenesis, particularly within the field of molecular pathology, have shaped the personalised medicine paradigm [1–4]. The epidermal growth factor receptor (EGFR) is expressed on the surface of cells of epithelial, mesenchymal and neuronal origin, with an expression range of up to 100,000 receptors per cell. This overexpression sequentially leads to tumour promoting properties such as increased proliferation, evasion of apoptosis and survival [5–9]. Aberrant over-expression of this biomarker has been a widely investigated therapeutic target in a range of solid tumours including colorectal cancer (CRC) with different anti-EGFR therapies being considered.
Following the application of immunohistochemistry (IHC) within the field of diagnostic histopathology in late 1970’s, this method has remained popular for detecting and visualising cellular proteins in tissue samples where it can be used for both clinical diagnosis and classification of tumours [10, 11], including the assessment of EGFR over-expression. The conventional, visual assessment of protein expression within a tissue microarray or whole tissue section involves subjective scoring of the tumour cells and normal cells according to the intensity and the distribution of the stain. However, this subjective classification system does not sufficiently define the cellular and sub-cellular categories, and where the immunohistochemical heterogeneity of cells is not adequately taken into account [12]. For example, classifying the tumour based only on the highest intensity—the so-called ‘hot spot’ method, allocates little significance to regions that have stained with a lower intensity. The heterogeneity of staining observed within tumours and its interpretative complications have been highlighted in a number of recent seminal papers [13–19].
Modern biomarker focused clinical trials must aim to identify reliable prognostic and/or predictive biomarkers for patient stratification [20, 21]. However, variation in IHC methodology, lack of a standardised scoring criteria for EGFR and tissue heterogeneity introduce a range of variables which impact the reliable application of EGFR IHC as a method to determine treatment efficacy [22].
Immunohistochemical variability in EGFR detection
In both the clinical and translational research setting, protein quantification and visualisation are important [10, 23]. The most common method of assessing protein expression in cancerous cells is immunohistochemistry, with other methodologies such as next generation sequencing (NGS) also being used to detect appropriate targets in specific cancer types [24]. The advantage of using IHC is that this method is fast, cost effective; available within all routine diagnostic laboratories and retains tissue context. However, it has the major disadvantage of being qualitative or at best semi-quantitative visual scoring with inherent inter- and intra-observer variability [25–27]. The limited predictive utility of EGFR expression for the benefit of EGFR monoclonal antibody therapy may be due to a myriad of pre-analytical variables [28–30]. Chromogenic intensity of immunohistochemical assays have been shown to be affected by the type of fixative and the duration of tissue fixation, duration of storage and the conditions of the immunohistochemistry methodology [28, 30–32]. Although EGFR IHC is not used in current clinical practice for selecting patients for cetuximab treatment, there are no universally standardised methodological guidelines [20, 21] unlike HER2 interpretation and other IHC markers [33–37]. This in turn has made both the reproducibility and interpretation of EGFR results somewhat difficult. Studies have found that some EGFR IHC results in various cancer types are dependent on the type of antibody used [11, 38]. Currently, the DakoCytomation® EGFR PharmDx® kit [K1492, Clone 218-C9, Dako, Glostrup, Denmark] remains the only FDA approved method for EGFR detection. Despite the pitfalls in EGFR IHC, EGFR remains one of the most commonly investigated cancer biomarkers due to its oncogenic role in various tumour types [11, 39, 40]. The clinical utility of EGFR expression detection by IHC in colorectal cancer is still somewhat inconclusive, with numerous studies failing to demonstrate a predictive and/or prognostic role for EGFR IHC as a companion diagnostic test for cetuximab [20, 41–43].
EGFR expression does not correlate with response to anti-EGFR therapies?
The EGFR and downstream components of the pathway have an integral role in tumorigenesis by means of regulating proliferation, angiogenesis and metastasis [7, 8, 39] (Figure 1). EGFR inhibition can be achieved by using two classes of drugs, tyrosine kinase inhibitors or monoclonal antibodies [44]. Cetuximab and panitumumab are monoclonal antibodies that bind specifically to both EGFR homodimers and its heterodimers [39, 40, 44]. Cetuximab is an IgG1 chimerised, monoclonal antibody containing 34% mouse protein, which binds specifically to EGFR and its heterodimers [45] (Figure 2). Panitumumab is a fully humanised IgG2 antibody and has been found to have less hypersensitivity reactions compared to cetuximab [46]. KRAS and NRAS mutations have been identified as negative predictive markers for cetuximab and panitumumab efficacy in colorectal cancer [47–50] (Figure 2). This mutation is now used in current clinical practice to stratify patients eligible for cetuximab administration. However, recent studies identified that tumours with a KRAS wild type (KRAS WT) and positive EGFR expression as measured by IHC was not predictive of anti-EGFR efficacy [20, 42, 50, 51].
The use of cetuximab and panitumumab as both a single agent and in combination with chemotherapy has shown efficacy in several studies [20, 45, 52–54]. Results published from the COIN and CRYSTAL clinical trials, and more recent scientific literature seems to suggest irinotecan ±5-fluorouracil as preferred chemotherapy partners to be used with cetuximab [20, 42, 55–58]. A recent meta-analysis by Vale et al. [59] suggest that the differences in the effect may be partially explained by the use of oxaliplatin-based or irinotecan-based chemotherapy. Chung et al. reported that 25% of patients who were found to be EGFR negative demonstrated a complete response to anti-EGFR therapy, the National Cancer Institute of Canada Clinical Trials Group CO.17 Trial enrolled patients on the basis of EGFR IHC positivity; however, there was no correlation between expression and response [20, 41, 42, 56, 60, 61]. Also the conventional IHC antibodies used do not reliably detect EGFR mutations [62, 63], or differentiate between high affinity and low affinity binding receptors [64], which may in turn account for the lack of correlation between EGFR expression and response to EGFR targeting therapies. From the reports of EGFR negative patients benefiting from cetuximab therapy, it may be hypothesised that these patients may indeed have a high ratio of low affinity to high affinity binding receptors and/or EGFR variants within the tumour [60, 61]. Another possible reason for an EGFR IHC negative tumour responding to the treatment response may be heterogeneous overexpression of EGFR in such cases similar to apparently HER2 negative breast cancer cases showing response to Herceptin treatment [65, 66]. The opinion within the clinical setting is that the current recommendations for EGFR detection and determining cetuximab efficacy in colorectal cancer from these are not ‘fit for purpose’.
Potential for molecular methods as companion confirmatory diagnostic tests for EGFR IHC
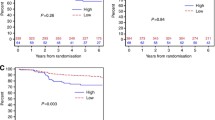
Determining EGFR gene amplification status and gene copy number (GCN) using fluorescence in situ hybridisation (FISH) and silver enhanced in situ hybridisation (SISH) has been shown to be extremely useful in determining efficacy of some classes of anti-EGFR therapies [67–69]. Major advantages of using SISH rather than FISH is that SISH can be assessed using a bright-field microscope and probe signal remains stable in storage unlike fluorescent probes [69–72]. Attempts to standardise a method for EGFR FISH yielded inconclusive results, with inter-laboratory variability of scoring cut-offs [73, 74]. Similar to that of KRAS mutational status, patients who have been found to have a low EGFR GCN are unlikely to respond to treatment with either cetuximab or panitumumab [69, 70, 74, 75]. A study carried out by Personeni et al. found that EGFR GCN could be used to predict the outcome after treatment with cetuximab in colorectal cancer patients and was able to predict response and overall survival independent of KRAS status [76]. However, like many other EGFR studies in colorectal cancer the cut-offs used in the complete patient cohort did not perform as well as in the training set from which they were derived and the authors recommended that their cut-offs should not be used as part of any decision making process [76]. Algars et al. [70] demonstrated a clinical benefit from anti-EGFR therapy using EGFR gene copy number, from regions of high EGFR expression in KRAS WT patients to determine response to targeted therapies. This was different from the method used by Personeni et al. [76] in a molecularly unselected population. The aspect of non-molecularly defined cohort may account for the inability of Personeni et al. [70, 76] to standardise reproducible SISH cut-offs for the clinical setting. In relation to determining the regions of high EGFR expression, it is important to note that the antibodies used were not from the FDA approved PharmDx™ assay.
The role of sub-cellular localisation of epidermal growth factor receptor
EGFR protein expression in colorectal cancer has been widely reported as membranous; however, numerous studies have noted the expression of EGFR within the cytoplasm of tumoural cells [77–79]. Unlike HER2, positive expression of EGFR is not predictive of response to anti-EGFR therapies, however, overexpression has however been linked to a poorer prognosis in colorectal cancer [20, 42, 80–82]. Upon interaction with a ligand the EGFR is internalised which initiates a complex signalling cascade and is degraded in the lysosomal compartment within the cytoplasm [7, 8, 83–85]. In previous studies in pancreatic and thyroid cancer, cytoplasmic expression of EGFR has been linked to a poor prognosis [77–79, 86, 87]. These studies suggest that the cellular localisation of EGFR depend on tumour stage and cancer context and may have significant clinicopathological value particularly in those patients treated with cetuximab with predictive or prognostic utility. Although Chung and colleagues [60] demonstrated that patients benefited from the cetuximab in the absence of membranous EGFR staining, what was not reported was whether any patients exhibited cytoplasmic EGFR staining.
Furthermore, the cytoplasmic localisation of EGFR in both RAS wild type and mutant metastatic colorectal cancer may confer an aggressive phenotype with these tumour cells having an altered intracellular metabolism and may be indicative of tumour cell population having undergone epithelial to mesenchymal transition [88, 89]. Additionally KRAS mutations are known to have different phenotypes with mutations in codon 13 shown to benefit from the addition of cetuximab. KRAS mutations can signal through the RAF-MEK-ERK MAPK pathway or the PI3K-AKT-mTOR pathway, suggesting that cytoplasmic localisation depending on KRAS mutant isoform may have predictive and prognostic utility in RAS mutant colorectal cancers [90–92].
Extracellular and intracellular mechanisms as predictive markers for anti-EGFR therapies in colorectal cancer
KRAS and NRAS mutations are established negative predictive markers for cetuximab [20, 50, 53, 56–58, 93], and account for approximately 50% of all mutations in colorectal cancer, coupled with other mutations approximately 40% of patients are eligible for anti-EGFR therapies, however, not all eligible patients respond to these therapies. Even with the extensive molecular characterisation of colorectal cancer [94–96], there are few molecular markers implemented in the clinical setting to determine clinical efficacy of anti-EGFR therapies. There are a variety of molecular markers that are still under extensive investigation such as BRAF and PI3KCA mutations to determine their roles in predicting efficacy [1, 4, 57, 58] (Figure 2). The histopathological evaluation of tissue has demonstrated an integral role of the micro-environment in tumoural development and progression. Studies have identified and highlighted the complexity of the crosstalk between tumour cells and host cells such as immune cells, cytokines and blood vessels which modulates tumour progression [97–101]. This observation has been expanded upon by Galon, Pagés and colleagues which led to the publication of seminal papers which defined the Immunoscore and has demonstrated the prognostic and predictive significance of immune involvement in colorectal tumours amongst others [100–108]. Automated interpretation of tissue biomarkers to predict response to therapy and future clinical behaviour of a tumour will provide an objective, standardised and reproducible method for tissue biomarker discovery and validation [22, 109].
Metastatic colorectal cancer has one of the poorest 5-year survival rates which emphasises the need for additional predictive and prognostic markers to facilitate efficient and informative patient stratification [110]. There have been eleven ligands identified that are part of the HER family with various receptor specificity, six of these ligands have been found to associate with the epidermal growth factor receptor which induces dimerization and initiation of complex intracellular signalling cascades [7, 8, 111] (Figure 1). Activation of oncogenic signaling through autocrine, paracrine or juxtacrine mechanisms have been shown to have both a predictive effect for response to targeted therapies [112, 113] and as a resistance mechanism through the activation of alternative survival pathways [114, 115] (Figure 2). Gene expression profiling of these ligands have associated epiregulin (EREG) and amphiregulin (AREG) having a role in cetuximab efficacy [112]. An increased mRNA level of either ligand has been shown to be associated with sensitivity to cetuximab monotherapy which has reflected by the longer progression free survival [112, 113, 116]. Tumours with increased levels of both AREG and EREG ligands and a KRAS WT benefited the most from anti-EGFR therapies these findings shows strong predictive value as KRAS and NRAS have strong negative predictive value [47, 48, 56, 112, 113], with a recent publication reporting that patients with KRAS mutant adenocarcinoma of the lung with induced epiregulin expression was associated with an aggressive phenotype [117].
Beyond total EGFR: determining pathway activation for predicting anti-EGFR response
The presence or absence of total EGFR has been shown to have no predictive utility for anti-EGFR therapies in mCRC [42, 45, 60], thus emphasising the complexity of not just the epidermal growth factor receptor but of the entire EGFR signalling pathway [118]. Ascertaining the activation status of the EGFR pathway may indeed unveil additional EGFR-mediated insights, which has to date eluded clinical practice. However, the challenge facing this paradigm is how to best measure and interpret activation status, what is well known is the plethora of phosphorylation of proteins within the intracellular compartment of cells. Indeed subtle changes in cellular biochemistry can alter the expression pattern of these proteins as well as gene expression profiles therefore providing misleading information as to the activation status of the cellular pathways [30].
The activation status of most signalling pathways can be determined through the measurement of post-translational modifications, such as the phosphorylation status of key amino acids, involved in signal transduction. Phospho-specific antibodies using immunohistochemistry or western blot analysis can be used to measure these. These dynamic post-translational changes can be used demonstrate inhibition of signalling pathways by investigational drugs. The utility of these pathway activation markers and technologies in clinical trials has, however, been limited by the evanescent nature of amino acid phosphorylation which is rapidly reversed by endogenous phosphatases. Extensive studies have shown that the rate of tissue penetration by fixatives, such as formalin, in most solid tumours is too slow to inactivate phosphatases resulting in preservation of phosphorylation only in the outer few millimetres (<5mm) of the tissue sample [119]. The lack of reliable means to collect, store and ship such samples and to reliably preserve and measure these labile events has often failed to generate reproducible clinically translatable results. However, recent translational studies carried out by Chafin et al. [120, 121] identified a method termed “2+2” as a robust method to preserve these phosphorylated proteins.
What has become apparent in precision medicine that no single field can answer the complexity of cancer. A holistic understanding of the tumour genome, phenome, immunome and a myriad of other “ome” related classifications is needed to realize the potential of precision medicine. Genomic stratification of colorectal cancers has identified at least five molecular subtypes of colorectal cancer all of which have various phenotypes and clinical outcomes [122, 123]. Irrespective of EGFR IHC status, a significant proportion of RAS wild type colorectal cancers are resistant to cetuximab, which suggests other EGFR-mediated or related mechanisms, contribute to this paradox. Thus looking beyond total EGFR is warranted, EGFR can be activated through the auto-phosphorylation of its tyrosine residues that in-turn stimulates a myriad of downstream signaling cascades. Integrating this knowledge into the EGFR paradigm, it is plausible that, if accurately detected, phosphorylated EGFR (pEGFR) may indeed reflect receptor utilization by the specific tumour.
Elegant studies carried out by Prahallad et al. [1] and Corcoran et al. [4] identified that BRAF mutant colorectal cancer cell lines were sensitive to dual inhibition with cetuximab and vemurafenib compared to melanoma cell lines. Indeed as shown by Corcoran and Prahallad inhibition of a single oncogenic mutation in colorectal cancer cells with vemurafenib, the same drug which has shown up to 50% response rates in melanoma, efficacy is not the same [1, 4]. This is indeed an example of how the microenvironment of the specific tissue type can regulate resistance mechanisms to both targeted therapies and chemotherapy treatment. However, by addressing this ‘kinome remodeling’ [124] through the use of combination therapies, efficacy was demonstrated. BRAF mutations are found in up to 60% of all melanomas [125] and up to 10% of colorectal cancers, with BRAF mutant CRCs having a poorer prognosis to both wild type and RAS mutant tumours. Corcoran et al. [4] found that phosphorylated EGFR was overexpressed in over 60% of BRAF mutant colorectal cancers compared to pEGFR in melanoma. Taking these findings in subtype specific context suggests that baseline pEGFR levels may make these tumours more prone to EGFR-mediated resistance suggesting the use of pEGFR as a predictive marker to identify patient populations who may respond to different combination therapy approaches. Thus patients with high tumoural pEGFR levels may indeed respond better to cetuximab and/or erlotinib in combination with vemurafenib, for which there are several on-going clinical trials an example of which is the EViCT trial being conducted in Melbourne (ACTRN12614000486628). Patients with low pEGFR may be better candidates for MEK inhibitors such as trametinib, in combination with vemurafenib which has shown improved clinical efficacy in melanomas compared to those treated with vemurafenib alone [126, 127]. It is plausible that mCRC patients whose tumours are negative for EGFR IHC indeed have elevated pEGFR which may explain why a subgroup of these total EGFR negative patients respond to anti-EGFR therapies.
Digital image analysis for improving the precision and predictive potential of EGFR IHC
Visual interpretation of immunohistochemistry is a subjective measurement coupled with an arbitrary threshold to differentiate and classify patients into expression categories [128]. In addition to the subjectivity, there are well recognised issues of poor reproducibility in evaluation of tissue structures such as determining viable tumour percentage and tumour cellularity for molecular testing and grading systems such as Gleason grading in prostate cancer [129–131]. The increased use of digital slides and whole slide imaging in the last decade has ushered in an exciting era of computer-aided histopathology, with image analysis approaches providing a powerful companion tool for the extraction of quantitative data from digital images in a robust and reproducible manner [132]. Not only does this quantitative, multi-parametric data enable clinical correlations but also offers the ability to visualise quantitative tumoural phenotypes and provide deeper insights into the biological characteristics of tissue specimens. As stated in the preceding sections, immunohistochemistry is an extremely important tool for the identification of single disease-related protein biomarkers [10]. Although the advantages of immunohistochemistry in biomarker discovery and validation are clear, the accompanying issues of inherent subjectivity and poor reproducibility of chromogenic interpretation of routine biomarkers and tissue architecture even by experienced pathologists are well described [109, 128–130]. Image analysis can significantly improve EGFR IHC evaluation through the quantification of expression within an automatically detected tumoural regions, providing an objective histological score. In recent guidelines published for the interpretation of biomarkers in breast cancer, the American Society of Clinical Oncology and the College of American Pathologist’s recommended quantification of ER, PR and HER2 by image analysis and in recent years some commercial image analysis algorithms have been approved for the evaluation of these markers [34, 35]. Riley et al. [133] used a novel quantitative approach to investigate the co-localisation of biomarkers within the cytoplasm and nucleus in NSCLC within both tumoural and stromal tissue, highlighting prognostic clinical insights as to the expression of these biomarkers in various histological subtypes, which may benefit from targeted therapies. Of recent promise and excitement is the development of an automated approach by Galon and colleagues to quantify the type, density and localisation of immune cells in cancer, which has been shown to have prognostic utility across multiple cancer types [101, 102, 106]. A comprehensive review on the role of digital pathology and image analysis in tissue biomarker research has recently been published by our group [109]. Quantitative studies of EGFR IHC are underway by a number of groups which may throw new light the role of EGFR in predicting response to therapy. These studies and the integration of ‘big data’ obtained from quantitative image analysis are likely to be important in defining a specific cancer phenome on a patient by patient basis, establishing new patient signatures and helping deliver the personalised medicine promise of ‘the right drug, for the right patient’ [134–139].
Conclusion
EGFR over-expression in colorectal cancer as determined by immunohistochemistry has led to initial clinical trials investigating patient selection for cetuximab and panitumumab therapies and shown promising results [41, 45]. However, what is now apparent is that patients can benefit from the addition of cetuximab in the absence of positive EGFR immunohistochemistry [20, 42, 46, 51, 60]. The impact of both intra- and inter-tumoural heterogeneity on therapeutic response, and an effective screening methodology has yet to be clinically implemented [140–142]. Additionally it is important to acknowledge that pre-analytical variables alone do not solely contribute to our inability to predict responsiveness to anti-EGFR therapy using tissue-based EGFR analysis. Indeed the complexity of the EGFR pathway as highlighted by a multitude of publications in recent years merits more in-depth studies in relation to this pathway.
The tumour tissue investigated for EGFR expression is usually the primary tumour sample, however, this may not reflect the molecular landscape and immunohistochemical profile of the metastatic site [13, 57, 58, 143, 144]. Studies by Chung and other authors have proposed that the expression of EGFR may vary within cancer types due to the ratio of low to high affinity binding receptors, which are not differentiated between by the commonly used EGFR assays [60, 62, 145–147]. Rather than relying upon an IHC method alone for determining patients who will benefit from cetuximab a more reliable approach based on a two-pronged strategy utilising a combination of EGFR IHC and EGFR SISH could be utilised to determine the EGFR status. Using such a combined approach it has been possible to identify clinically beneficial therapeutic cohorts of patients based on highest EGFR protein expression and assessing the gene copy number specifically within this region [70]. There is therefore a case to develop an assay for EGFR similar to that of the Dual ISH approach in HER2 [148]. In addition to the benefits of the dual method there is also the technically feasible scope for assessing the two independent molecular markers of the EGFR status on a single tissue section making the overall analysis more precise and reproducible.
Digital pathology and image analysis may indeed serve as companion prognostic and or predictive tools in personalised medicine [109], with some companies receiving FDA clearance for algorithms evaluating tissue biomarkers such as HER2, ER, PR and Ki67. For EGFR, quantitative analysis of cell membrane expression may not be sufficient for patient stratification and selection for anti-EGFR therapy, and more precise localisation of the biomarker may be key. Whilst difficult to achieve this using visual scoring, this becomes entirely feasible using computer-aided image analysis. In the current immunohistochemical interpretation guidelines for EGFR and HER2, cytoplasmic localisation is not included. Expression of immunohistochemical markers must be evaluated depending on cellular context and in a cancer specific manner; the prognostic utility of sub-cellular localisation of biomarkers is exemplified by beta-catenin expression and localisation in solid tumours [149]. Molecular interactions are both intracellular and extracellular, and so it is a reasonable assumption that the internalisation and cytoplasmic accumulation of EGFR may indeed alter tumour cell morphology, metabolism and confer an invasive cellular phenotype [88, 89]. Adopting a novel digital pathology based approach for the evaluation of EGFR IHC expression in both the cytoplasm and membrane may elucidate clinically beneficial subgroups that could benefit from the addition of targeted therapies. The objective and reproducible approach of image analysis in tissue biomarker evaluation could initiate a paradigm shift in the way in which we evaluate tissue biomarkers for patient stratification and personalised therapy regimens and indeed the way in which cellular immunohistochemistry is reported [22].
The TCGA consortium reported the frequencies of up-regulation of other HER family members in colorectal cancer which provides scientific and clinical rationale for combination therapies to block different members [1, 4, 96, 150, 151]. Furthermore, as demonstrated by multiple authors through the action of EGFR ligands, tumours do not have to express the EGFR to elicit a response to EGFR-targeted therapies, implying that cetuximab resistance and indeed response in specific cohorts may be governed by ligand-dependent and/or ligand-independent mechanisms [112, 113]. Spano et al. reported that immunohistochemical expression of EGFR was stage-dependent which may suggest that membranous expression of EGFR may not have a predictive utility for monoclonal antibody therapy in the metastatic setting as demonstrated in previous clinical trials however, may indeed have clinical utility in the adjuvant or neo-adjuvant setting [20, 42, 45, 80]. Furthermore, using either total EGFR IHC and/or pEGFR IHC in a subtype specific context may enable more effective patient stratification approaches in CRC as demonstrated by Prahallad et al. [1] and Corcoran et al. [4].
Before we abandon EGFR IHC as an unreliable companion diagnostic for patient selection, a detailed investigation is necessary to include quantitative image analysis of aberrant EGFR expression within the membrane and cytoplasmic compartments, combined with ligand expression, molecular analysis of genetic abnormalities such as gene copy number variation and mutational status. This will provide definitive insight into EGFR as a tissue-based biomarker in patients with colorectal cancer and other malignancies.
Abbreviations
- EGFR:
-
epidermal growth factor receptor
- IHC:
-
immunohistochemistry
- CRC:
-
colorectal cancer
- GCN:
-
gene copy number
- AREG:
-
amphiregulin
- EREG:
-
epiregulin
- TCGA:
-
the cancer genome atlas
- ER:
-
oestrogen receptor
- PR:
-
progesterone receptor
- pEGFR:
-
phosphorylated EGFR
- HER2:
-
human epidermal growth factor receptor 2
- ISH:
-
in situ hybridisation
- SISH:
-
silver in situ hybridisation
- FDA:
-
food and drug administration
References
Prahallad A, Sun C, Huang S, Di Nicolantonio F, Salazar R, Zecchin D et al (2012) Unresponsiveness of colon cancer to BRAF[V600E] inhibition through feedback activation of EGFR. Nature 483(7387):100–103
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW et al (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350(21):2129–2139
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S et al (2007) Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 448(7153):561–566
Corcoran RB, Ebi H, Turke AB, Coffee EM, Nishino M, Cogdill AP et al (2012) EGFR-mediated re-activation of MAPK signaling contributes to insensitivity of BRAF mutant colorectal cancers to RAF inhibition with vemurafenib. Cancer Discov 2(3):227–235
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100(1):57–70
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2(2):127–137
Yarden Y (2001) The EGFR family and its ligands in human cancer. Signalling mechanisms and therapeutic opportunities. Eur J Cancer 37(Suppl 4):S3–S8
Henriksen L, Grandal MV, Knudsen SL, van Deurs B, Grovdal LM (2013) Internalization mechanisms of the epidermal growth factor receptor after activation with different ligands. PLoS One 8(3):e58148
McCourt CM, Boyle D, James J, Salto-Tellez M (2013) Immunohistochemistry in the era of personalised medicine. J Clin Pathol 66(1):58–61
Anagnostou VK, Welsh AW, Giltnane JM, Siddiqui S, Liceaga C, Gustavson M et al (2010) Analytic variability in immunohistochemistry biomarker studies. Cancer Epidemiol Biomarkers Prev 19(4):982–991
Rivenbark AG, O’Connor SM, Coleman WB (2013) Molecular and cellular heterogeneity in breast cancer: challenges for personalized medicine. Am J Pathol 183(4):1113–1124
Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA Jr, Kinzler KW (2013) Cancer genome landscapes. Science 339(6127):1546–1558
Burrell RA, McGranahan N, Bartek J, Swanton C (2013) The causes and consequences of genetic heterogeneity in cancer evolution. Nature 501(7467):338–345
Aparicio S, Caldas C (2013) The implications of clonal genome evolution for cancer medicine. N Engl J Med 368(9):842–851
Almendro V, Marusyk A, Polyak K (2013) Cellular heterogeneity and molecular evolution in cancer. Annu Rev Pathol 24(8):277–302
de Bruin EC, Taylor TB, Swanton C (2013) Intra-tumor heterogeneity: lessons from microbial evolution and clinical implications. Genome Med 5(11):101
Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E et al (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366(10):883–892
Fisher R, Pusztai L, Swanton C (2013) Cancer heterogeneity: implications for targeted therapeutics. Br J Cancer 108(3):479–485
Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT, Wilson RH et al (2011) Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet 377(9783):2103–2114
Seymour MT, Maughan TS, Ledermann JA, Topham C, James R, Gwyther SJ et al (2007) Different strategies of sequential and combination chemotherapy for patients with poor prognosis advanced colorectal cancer [MRC FOCUS]: a randomised controlled trial. Lancet 370(9582):143–152
Fitzgibbons PL, Lazar AJ, Spencer S (2014) Introducing new College of American Pathologists reporting templates for cancer biomarkers. Arch Pathol Lab Med 138(2):157–158
Idikio HA (2009) Immunohistochemistry in diagnostic surgical pathology: contributions of protein life-cycle, use of evidence-based methods and data normalization on interpretation of immunohistochemical stains. Int J Clin Exp Pathol 3(2):169–176
Russnes HG, Navin N, Hicks J, Borresen-Dale AL (2011) Insight into the heterogeneity of breast cancer through next-generation sequencing. J Clin Invest 121(10):3810–3818
Thomson TA, Hayes MM, Spinelli JJ, Hilland E, Sawrenko C, Phillips D et al (2001) HER-2/neu in breast cancer: interobserver variability and performance of immunohistochemistry with 4 antibodies compared with fluorescent in situ hybridization. Mod Pathol 14(11):1079–1086
Turashvili G, Leung S, Turbin D, Montgomery K, Gilks B, West R et al (2009) Inter-observer reproducibility of HER2 immunohistochemical assessment and concordance with fluorescent in situ hybridization [FISH]: pathologist assessment compared to quantitative image analysis. BMC Cancer 9:165
Gavrielides MA, Gallas BD, Lenz P, Badano A, Hewitt SM (2011) Observer variability in the interpretation of HER2/neu immunohistochemical expression with unaided and computer-aided digital microscopy. Arch Pathol Lab Med 135(2):233–242
Atkins D, Reiffen KA, Tegtmeier CL, Winther H, Bonato MS, Storkel S (2004) Immunohistochemical detection of EGFR in paraffin-embedded tumor tissues: variation in staining intensity due to choice of fixative and storage time of tissue sections. J Histochem Cytochem 52(7):893–901
Hewitt SM, Badve SS, True LD (2012) Impact of preanalytic factors on the design and application of integral biomarkers for directing patient therapy. Clin Cancer Res 18(6):1524–1530
Neumeister VM, Parisi F, England AM, Siddiqui S, Anagnostou V, Zarrella E et al (2014) A tissue quality index: an intrinsic control for measurement of effects of preanalytical variables on FFPE tissue. Lab Invest 94(4):467–474
Press MF, Hung G, Godolphin W, Slamon DJ (1994) Sensitivity of HER-2/neu antibodies in archival tissue samples: potential source of error in immunohistochemical studies of oncogene expression. Cancer Res 54(10):2771–2777
Tong LC, Nelson N, Tsourigiannis J, Mulligan AM (2011) The effect of prolonged fixation on the immunohistochemical evaluation of estrogen receptor, progesterone receptor, and HER2 expression in invasive breast cancer: a prospective study. Am J Surg Pathol 35(4):545–552
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ et al (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 25(1):118–145
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013
Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S (2010) American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 6(4):195–197
Allred DC, Harvey JM, Berardo M, Clark GM (1998) Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol 11(2):155–168
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J et al (2011) Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst 103(22):1656–1664
Won JR, Gao D, Grant D, Cupples J, Rahemtulla A, Wolber R et al (2012) Variable performance of commercial epidermal growth factor receptor antibodies in detection of basal-like breast cancer. Histopathology 61(3):518–519
Ciardiello F, Tortora G (2003) Epidermal growth factor receptor [EGFR] as a target in cancer therapy: understanding the role of receptor expression and other molecular determinants that could influence the response to anti-EGFR drugs. Eur J Cancer 39(10):1348–1354
Ciardiello F, Tortora G (2008) EGFR antagonists in cancer treatment. N Engl J Med 358(11):1160–1174
Saltz LB, Meropol NJ, Loehrer PJS, Needle MN, Kopit J, Mayer RJ (2004) Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol 22(7):1201–1208
Van Cutsem E, Peeters M, Siena S, Humblet Y, Hendlisz A, Neyns B et al (2007) Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol 25(13):1658–1664
Pirker R, Pereira JR, von Pawel J, Krzakowski M, Ramlau R, Park K et al (2012) EGFR expression as a predictor of survival for first-line chemotherapy plus cetuximab in patients with advanced non-small-cell lung cancer: analysis of data from the phase 3 FLEX study. Lancet Oncol 13(1):33–42
You B, Chen EX (2011) Anti-EGFR monoclonal antibodies for treatment of colorectal cancers: development of cetuximab and panitumumab. J Clin Pharmacol
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A et al (2004) Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351(4):337–345
Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ et al (2008) Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol 26(10):1626–1634
Lievre A, Bachet JB, Le Corre D, Boige V, Landi B, Emile JF et al (2006) KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res 66(8):3992–3995
Lievre A, Bachet JB, Boige V, Cayre A, Le Corre D, Buc E et al (2008) KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol 26(3):374–379
Di Fiore F, Blanchard F, Charbonnier F, Le Pessot F, Lamy A, Galais MP et al (2007) Clinical relevance of KRAS mutation detection in metastatic colorectal cancer treated by cetuximab plus chemotherapy. Br J Cancer 96(8):1166–1169
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M et al (2013) Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 369(11):1023–1034
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M et al (2010) Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin [FOLFOX4] versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol 28(31):4697–4705
Bokemeyer C, Bondarenko I, Hartmann JT, de Braud F, Schuch G, Zubel A et al (2011) Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol 22(7):1535–1546
Stintzing S, Fischer von Weikersthal L, Decker T, Vehling-Kaiser U, Jager E, Heintges T et al (2012) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer-subgroup analysis of patients with KRAS: mutated tumours in the randomised German AIO study KRK-0306. Ann Oncol 23(7):1693–1699
Bokemeyer C, Bondarenko I, Makhson A, Hartmann JT, Aparicio J, de Braud F et al (2009) Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol 27(5):663–671
Jonker DJ, O’Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ et al (2007) Cetuximab for the treatment of colorectal cancer. N Engl J Med 357(20):2040–2048
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC et al (2008) K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med 359(17):1757–1765
De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G et al (2010) Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol 11(8):753–762
De Roock W, De Vriendt V, Normanno N, Ciardiello F, Tejpar S (2011) KRAS, BRAF, PIK3CA, and PTEN mutations: implications for targeted therapies in metastatic colorectal cancer. Lancet Oncol 12(6):594–603
Vale CL, Tierney JF, Fisher D, Adams RA, Kaplan R, Maughan TS et al (2012) Does anti-EGFR therapy improve outcome in advanced colorectal cancer? A systematic review and meta-analysis. Cancer Treat Rev 38(6):618–625
Chung KY, Shia J, Kemeny NE, Shah M, Schwartz GK, Tse A et al (2005) Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J Clin Oncol 23(9):1803–1810
Wierzbicki R, Jonker DJ, Moore MJ, Berry SR, Loehrer PJ, Youssoufian H et al (2011) A phase II, multicenter study of cetuximab monotherapy in patients with refractory, metastatic colorectal carcinoma with absent epidermal growth factor receptor immunostaining. Invest New Drugs 29(1):167–174
Cunningham MP, Essapen S, Thomas H, Green M, Lovell DP, Topham C et al (2005) Coexpression, prognostic significance and predictive value of EGFR, EGFRvIII and phosphorylated EGFR in colorectal cancer. Int J Oncol 27(2):317–325
Allo G, Bandarchi B, Yanagawa N, Wang A, Shih W, Xu J et al (2014) EGFR mutation-specific immunohistochemical antibodies in lung adenocarcinoma. Histopathology 64(6):826–839
Brabyn CJ, Kleine LP (1995) EGF causes hyperproliferation and apoptosis in T51B cells: involvement of high and low affinity EGFR binding sites. Cell Signal 7(2):139–150
Braun S, Schlimok G, Heumos I, Schaller G, Riethdorf L, Riethmuller G et al (2001) ErbB2 overexpression on occult metastatic cells in bone marrow predicts poor clinical outcome of stage I-III breast cancer patients. Cancer Res 61(5):1890–1895
Ithimakin S, Day KC, Malik F, Zen Q, Dawsey SJ, Bersano-Begey TF et al (2013) HER2 drives luminal breast cancer stem cells in the absence of HER2 amplification: implications for efficacy of adjuvant trastuzumab. Cancer Res 73(5):1635–1646
Hirsch FR, Varella-Garcia M, Bunn PA Jr, Di Maria MV, Veve R, Bremmes RM et al (2003) Epidermal growth factor receptor in non-small-cell lung carcinomas: correlation between gene copy number and protein expression and impact on prognosis. J Clin Oncol 21(20):3798–3807
Hirsch FR, Herbst RS, Olsen C, Chansky K, Crowley J, Kelly K et al (2008) Increased EGFR gene copy number detected by fluorescent in situ hybridization predicts outcome in non-small-cell lung cancer patients treated with cetuximab and chemotherapy. J Clin Oncol 26(20):3351–3357
Wulf MA, Bode B, Zimmermann D, Rufibach K, Weder W, Moch H et al (2012) Silver-enhanced in situ hybridization for determination of EGFR copy number alterations in non-small cell lung cancer. Am J Surg Pathol 36(12):1801–1808
Algars A, Lintunen M, Carpen O, Ristamaki R, Sundstrom J (2011) EGFR gene copy number assessment from areas with highest EGFR expression predicts response to anti-EGFR therapy in colorectal cancer. Br J Cancer 105(2):255–262
Werner M, Chott A, Fabiano A, Battifora H (2000) Effect of formalin tissue fixation and processing on immunohistochemistry. Am J Surg Pathol 24(7):1016–1019
Liotta LA, Espina V, Mehta AI, Calvert V, Rosenblatt K, Geho D et al (2003) Protein microarrays: meeting analytical challenges for clinical applications. Cancer Cell 3(4):317–325
Sartore-Bianchi A, Fieuws S, Veronese S, Moroni M, Personeni N, Frattini M et al (2012) Standardisation of EGFR FISH in colorectal cancer: results of an international interlaboratory reproducibility ring study. J Clin Pathol 65(3):218–223
Sartore-Bianchi A, Moroni M, Veronese S, Carnaghi C, Bajetta E, Luppi G et al (2007) Epidermal growth factor receptor gene copy number and clinical outcome of metastatic colorectal cancer treated with panitumumab. J Clin Oncol 25(22):3238–3245
Luber B, Deplazes J, Keller G, Walch A, Rauser S, Eichmann M et al (2011) Biomarker analysis of cetuximab plus oxaliplatin/leucovorin/5-fluorouracil in first-line metastatic gastric and oesophago-gastric junction cancer: results from a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie [AIO]. BMC Cancer 11:509
Personeni N, Fieuws S, Piessevaux H, De Hertogh G, De Schutter J, Biesmans B et al (2008) Clinical usefulness of EGFR gene copy number as a predictive marker in colorectal cancer patients treated with cetuximab: a fluorescent in situ hybridization study. Clin Cancer Res 14(18):5869–5876
Mahipal A, Mcdonald MJ, Witkiewicz A, Carr BI (2012) Cell membrane and cytoplasmic epidermal growth factor receptor expression in pancreatic ductal adenocarcinoma. Med Oncol 29(1):134–139
Pu YS, Huang CY, Kuo YZ, Kang WY, Liu GY, Huang AM et al (2009) Characterization of membranous and cytoplasmic EGFR expression in human normal renal cortex and renal cell carcinoma. J Biomed Sci 16:82
Ueda S, Ogata S, Tsuda H, Kawarabayashi N, Kimura M, Sugiura Y et al (2004) The correlation between cytoplasmic overexpression of epidermal growth factor receptor and tumor aggressiveness: poor prognosis in patients with pancreatic ductal adenocarcinoma. Pancreas 29(1):e1–e8
Spano JP, Fagard R, Soria JC, Rixe O, Khayat D, Milano G (2005) Epidermal growth factor receptor signaling in colorectal cancer: preclinical data and therapeutic perspectives. Ann Oncol 16(2):189–194
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M et al (2011) Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med 365(14):1273–1283
Mosesson Y, Mills GB, Yarden Y (2008) Derailed endocytosis: an emerging feature of cancer. Nat Rev Cancer 8(11):835–850
Liao HJ, Carpenter G (2009) Cetuximab/C225-induced intracellular trafficking of epidermal growth factor receptor. Cancer Res 69(15):6179–6183
Tomas A, Futter CE, Eden ER (2014) EGF receptor trafficking: consequences for signaling and cancer. Trends Cell Biol 24(1):26–34
Piyathilake CJ, Frost AR, Manne U, Weiss H, Bell WC, Heimburger DC et al (2002) Differential expression of growth factors in squamous cell carcinoma and precancerous lesions of the lung. Clin Cancer Res 8(3):734–744
Einama T, Ueda S, Tsuda H, Ogasawara K, Hatsuse K, Matsubara O et al (2012) Membranous and cytoplasmic expression of epidermal growth factor receptor in metastatic pancreatic ductal adenocarcinoma. Exp Ther Med 3(6):931–936
De Craene B, Berx G (2013) Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer 13(2):97–110
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol 15(3):178–196
Mendoza MC, Er EE, Blenis J (2011) The Ras-ERK and PI3K-mTOR pathways: cross-talk and compensation. Trends Biochem Sci 36(6):320–328
Vartanian S, Bentley C, Brauer MJ, Li L, Shirasawa S, Sasazuki T et al (2013) Identification of mutant K-Ras-dependent phenotypes using a panel of isogenic cell lines. J Biol Chem 288(4):2403–2413
Parsons BL, Myers MB (2013) Personalized cancer treatment and the myth of KRAS wild-type colon tumors. Discov Med 15(83):259–267
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE et al (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer [FIRE-3]: a randomised, open-label, phase 3 trial. Lancet Oncol 15(10):1065–1075
Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M et al (1988) Genetic alterations during colorectal-tumor development. N Engl J Med 319(9):525–532
Fearon ER, Vogelstein B (1990) A genetic model for colorectal tumorigenesis. Cell 61(5):759–767
Cancer Genome Atlas Network (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487(7407):330–337
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331(6024):1565–1570
Liotta LA, Kohn EC (2001) The microenvironment of the tumour-host interface. Nature 411(6835):375–379
Emens LA, Silverstein SC, Khleif S, Marincola FM, Galon J (2012) Toward integrative cancer immunotherapy: targeting the tumor microenvironment. J Transl Med 10:70
Galon J, Fridman WH, Pages F (2007) The adaptive immunologic microenvironment in colorectal cancer: a novel perspective. Cancer Res 67(5):1883–1886
Mlecnik B, Tosolini M, Kirilovsky A, Berger A, Bindea G, Meatchi T et al (2011) Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 29(6):610–618
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C et al (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313(5795):1960–1964
Galon J, Pages F, Marincola FM, Thurin M, Trinchieri G, Fox BA et al (2012) The immune score as a new possible approach for the classification of cancer. J Transl Med 10:1
Galon J, Pages F, Marincola FM, Angell HK, Thurin M, Lugli A et al (2012) Cancer classification using the Immunoscore: a worldwide task force. J Transl Med 10:205
Galon J, Angell HK, Bedognetti D, Marincola FM (2013) The continuum of cancer immunosurveillance: prognostic, predictive, and mechanistic signatures. Immunity 39(1):11–26
Angell H, Galon J (2013) From the immune contexture to the Immunoscore: the role of prognostic and predictive immune markers in cancer. Curr Opin Immunol 25(2):261–267
Galon J, Mlecnik B, Bindea G, Angell HK, Berger A, Lagorce C et al (2014) Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J Pathol 232(2):199–209
Bindea G, Mlecnik B, Angell HK, Galon J (2014) The immune landscape of human tumors: implications for cancer immunotherapy. Oncoimmunology 3(1):e27456
Hamilton PW, Bankhead P, Wang Y, Hutchinson R, Kieran D, McArt DG et al (2014) Digital pathology and image analysis in tissue biomarker research. Methods 70(1):59–73
Van Schaeybroeck S, Allen WL, Turkington RC, Johnston PG (2011) Implementing prognostic and predictive biomarkers in CRC clinical trials. Nat Rev Clin Oncol 8(4):222–232
Schneider MR, Wolf E (2009) The epidermal growth factor receptor ligands at a glance. J Cell Physiol 218(3):460–466
Khambata-Ford S, Garrett CR, Meropol NJ, Basik M, Harbison CT, Wu S et al (2007) Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J Clin Oncol 25(22):3230–3237
Jacobs B, De Roock W, Piessevaux H, Van Oirbeek R, Biesmans B, De Schutter J et al (2009) Amphiregulin and epiregulin mRNA expression in primary tumors predicts outcome in metastatic colorectal cancer treated with cetuximab. J Clin Oncol 27(30):5068–5074
Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J et al (2012) Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature 487(7408):500–504. doi:10.1038/nature11183 (1476-4687 (Electronic); 0028-0836)
Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E et al (2012) Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature 487(7408):505–509. doi:10.1038/nature11249 (1476-4687 (Electronic); 0028-0836)
Kuramochi H, Nakajima G, Kaneko Y, Nakamura A, Inoue Y, Yamamoto M et al (2012) Amphiregulin and epiregulin mRNA expression in primary colorectal cancer and corresponding liver metastases. BMC Cancer 12:88
Sunaga N, Kaira K, Imai H, Shimizu K, Nakano T, Shames DS et al (2013) Oncogenic KRAS-induced epiregulin overexpression contributes to aggressive phenotype and is a promising therapeutic target in non-small-cell lung cancer. Oncogene 32(34):4034–4042
Oda K, Matsuoka Y, Funahashi A, Kitano H (2005) A comprehensive pathway map of epidermal growth factor receptor signaling. Mol Syst Biol 1:2005.0010 (Epub 2005 May 25. (1744-4292 (Electronic); 1744-4292))
Mandell JW (2003) Phosphorylation state-specific antibodies: applications in investigative and diagnostic pathology. Am J Pathol 163(5):1687–1698 (0002-9440 (Print); 0002-9440)
Chafin D, Theiss A, Roberts E, Borlee G, Otter M, Baird GS (2013) Rapid two-temperature formalin fixation. PLoS One 8(1):e54138. doi:10.1371/journal.pone.0054138
Theiss AP, Chafin D, Bauer DR, Grogan TM, Baird GS (2014) Immunohistochemistry of colorectal cancer biomarker phosphorylation requires controlled tissue fixation. PLoS One 9(11):e113608. doi:10.1371/journal.pone.0113608
Phipps AI, Limburg PJ, Baron JA, Burnett-Hartman AN, Weisenberger DJ, Laird PW et al (2015) Association between molecular subtypes of colorectal cancer and patient survival. Gastroenterology 148(1):77–87.e2. doi:10.1053/j.gastro.2014.09.038 (Epub 2014 Sep 30. (1528-0012 (Electronic); 0016-5085))
Sadanandam A, Lyssiotis CA, Homicsko K, Collisson EA, Gibb WJ, Wullschleger S et al (2013) A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Nat Med. 19(5):619–625. doi:10.1038/nm.3175 (Epub 2013 Apr 14. (1546-170X (Electronic); 1078-8956))
Duncan JS, Whittle MC, Nakamura K, Abell AN, Midland AA, Zawistowski JS et al (2012) Dynamic reprogramming of the kinome in response to targeted MEK inhibition in triple-negative breast cancer. Cell 149(2):307–321. doi:10.1016/j.cell.2012.02.053 (1097-4172 (Electronic); 0092-8674)
Ascierto PA, Kirkwood JM, Grob J-J, Simeone E, Grimaldi AM, Maio M et al (2012) The role of BRAF V600 mutation in melanoma. J Transl Med 10:85. doi:10.1186/1479-5876-10-85
Flaherty KT, Infante JR, Daud A, Gonzalez R, Kefford RF, Sosman J et al (2012) Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N Engl J Med 367(18):1694–1703. doi:10.1056/NEJMoa1210093 (Epub 2012 Sep 29. (1533-4406 (Electronic); 0028-4793))
Larkin J, Ascierto PA, Dréno B, Atkinson V, Liszkay G, Maio M et al (2014) Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med 371(20):1867–1876. doi:10.1056/NEJMoa1408868 (Epub 2014 Sep 29. (1533-4406 (Electronic); 0028-4793))
Polley MY, Leung SC, McShane LM, Gao D, Hugh JC, Mastropasqua MG et al (2013) An international Ki67 reproducibility study. J Natl Cancer Inst 105(24):1897–1906
Smits AJ, Kummer JA, de Bruin PC, Bol M, van den Tweel JG, Seldenrijk KA et al (2014) The estimation of tumor cell percentage for molecular testing by pathologists is not accurate. Mod Pathol 27(2):168–174
Viray H, Li K, Long TA, Vasalos P, Bridge JA, Jennings LJ et al (2013) A prospective, multi-institutional diagnostic trial to determine pathologist accuracy in estimation of percentage of malignant cells. Arch Pathol Lab Med 137(11):1545–1549
Shaw GL, Thomas BC, Dawson SN, Srivastava G, Vowler SL, Gnanapragasam VJ et al (2014) Identification of pathologically insignificant prostate cancer is not accurate in unscreened men. Br J Cancer 110(10):2405–2411
Foran DJ, Chen W, Yang L (2011) Automated image interpretation computer-assisted diagnostics. Anal Cell Pathol [Amst] 34(6):279–300
Riley JS, Hutchinson R, McArt DG, Crawford N, Holohan C, Paul I et al (2013) Prognostic and therapeutic relevance of FLIP and procaspase-8 overexpression in non-small cell lung cancer. Cell Death Dis 5(4):e951
Petrovski S, Goldstein DB (2014) Phenomics and the interpretation of personal genomes. Sci Transl Med 6(254):254fs35
Zemojtel T, Kohler S, Mackenroth L, Jager M, Hecht J, Krawitz P et al (2014) Effective diagnosis of genetic disease by computational phenotype analysis of the disease-associated genome. Sci Transl Med 6(252):252ra123
Lu JT, Campeau PM, Lee BH (2014) Genotype-phenotype correlation—promiscuity in the era of next-generation sequencing. N Engl J Med 371(7):593–596
Zbuk KM, Eng C (2007) Cancer phenomics: RET and PTEN as illustrative models. Nat Rev Cancer 7(1):35–45
Houle D, Govindaraju DR, Omholt S (2010) Phenomics: the next challenge. Nat Rev Genet 11(12):855–866
Kelloff GJ, Sigman CC (2012) Cancer biomarkers: selecting the right drug for the right patient. Nat Rev Drug Discov 11(3):201–214. doi:10.1038/nrd3651 (1474-1784 (Electronic); 1474-1776)
Kent DM, Rothwell PM, Ioannidis JP, Altman DG, Hayward RA (2010) Assessing and reporting heterogeneity in treatment effects in clinical trials: a proposal. Trials 11:85
Kleppe M, Levine RL (2014) Tumor heterogeneity confounds and illuminates: assessing the implications. Nat Med 20(4):342–344
Cadioli A, Rossi G, Costantini M, Cavazza A, Migaldi M, Colby TV (2014) Lung cancer histologic and immunohistochemical heterogeneity in the era of molecular therapies: analysis of 172 consecutive surgically resected, entirely sampled pulmonary carcinomas. Am J Surg Pathol 38(4):502–509
Baldus SE, Schaefer KL, Engers R, Hartleb D, Stoecklein NH, Gabbert HE (2010) Prevalence and heterogeneity of KRAS, BRAF, and PIK3CA mutations in primary colorectal adenocarcinomas and their corresponding metastases. Clin Cancer Res 16(3):790–799
Xie T, Cho YB, Wang K, Huang D, Hong HK, Choi YL et al (2014) Patterns of somatic alterations between matched primary and metastatic colorectal tumors characterized by whole-genome sequencing. Genomics 104(4):234–241
Modjtahedi H, Essapen S (2009) Epidermal growth factor receptor inhibitors in cancer treatment: advances, challenges and opportunities. Anticancer Drugs 20(10):851–855
Modjtahedi H, Khelwatty SA, Kirk RS, Seddon AM, Essapen S, Del Vecchio CA et al (2012) Immunohistochemical discrimination of wild-type EGFR from EGFRvIII in fixed tumour specimens using anti-EGFR mAbs ICR9 and ICR10. Br J Cancer 106(5):883–888
Fan QW, Cheng CK, Gustafson WC, Charron E, Zipper P, Wong RA et al (2013) EGFR phosphorylates tumor-derived EGFRvIII driving STAT3/5 and progression in glioblastoma. Cancer Cell 24(4):438–449
Bartlett JM, Campbell FM, Ibrahim M, O’Grady A, Kay E, Faulkes C et al (2011) A UK NEQAS ISH multicenter ring study using the Ventana HER2 dual-color ISH assay. Am J Clin Pathol 135(1):157–162
van de Wetering M, Sancho E, Verweij C, de Lau W, Oving I, Hurlstone A et al (2002) The beta-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell 111(2):241–250
Chakrabarty A, Sanchez V, Kuba MG, Rinehart C, Arteaga CL (2012) Feedback upregulation of HER3 [ErbB3] expression and activity attenuates antitumor effect of PI3K inhibitors. Proc Natl Acad Sci USA 109(8):2718–2723
Laurent-Puig P, Manceau G, Zucman-Rossi J, Blons H (2012) Dual blockade of epidermal growth factor receptor-induced pathways: a new avenue to treat metastatic colorectal cancer. J Clin Oncol 30(13):1550–1552
Authors’ contributions
RAH conceived the concept of the review, compiled the literature, drafted the manuscript and revised the content. RAA, DGM, MST, BJ and PWH contributed to the core manuscript ideas, manuscript layout, content and revised the updated text. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Professor Paul M. Waring for reading through the final version of the manuscript. This work was partially funded from the People Programme (Marie Curie Actions) of the European Union’s Seventh Framework Programme FP7/2007-2013/ under REA grant agreement no [285910].
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hutchinson, R.A., Adams, R.A., McArt, D.G. et al. Epidermal growth factor receptor immunohistochemistry: new opportunities in metastatic colorectal cancer. J Transl Med 13, 217 (2015). https://doi.org/10.1186/s12967-015-0531-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-015-0531-z