Abstract
Background
Physical Activity 4 Everyone (PA4E1) is an evidence-based program effective at increasing adolescent physical activity (PA) and improving weight status. This study aimed to determine a) the effectiveness of an adapted implementation intervention to scale-up PA4E1 at 24-month follow-up, b) fidelity and reach, and c) the cost and cost-effectiveness of the implementation support intervention.
Methods
A cluster randomised controlled trial using a type III hybrid implementation-effectiveness design in 49 lower socio-economic secondary schools, randomised to a program (n = 24) or control group (n = 25). An adapted implementation intervention consisting of seven strategies was developed to support schools to implement PA4E1 over 24-months. The primary outcome was the proportion of schools implementing at least four of the 7 PA practices, assessed via computer assisted telephone interviews (CATI) with Head Physical Education Teachers. Secondary outcomes included the mean number of PA practices implemented, fidelity and reach, cost and cost-effectiveness. Logistic regression models assessed program effects.
Results
At baseline, no schools implemented four of the 7 PA practices. At 24-months, significantly more schools in the program group (16/23, 69.6%) implemented at least four of the 7 PA practices than the control group (0/25, 0%) (p < 0.001). At 24-months, program schools were implementing an average of 3.6 more practices than control schools (4.1 (1.7) vs. 0.5 (0.8), respectively) (P < 0.001). Fidelity and reach of the implementation intervention were high (> 75%). The total cost of the program was $415,112 AUD (2018) ($17,296 per school; $117.30 per student).
Conclusions
The adapted implementation intervention provides policy makers and researchers with an effective and potentially cost-effective model for scaling-up the delivery of PA4E1 in secondary schools. Further assessment of sustainability is warranted.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12617000681358 prospectively registered 12th May 2017.
Similar content being viewed by others
Introduction
Physical inactivity has been well documented as a risk factor for chronic disease and a significant contributor to the burden of disease in Australia and internationally [1, 2]. Despite the undisputed benefits of physical activity (PA), 81% of adolescents aged 11–17 years globally do not meet the current World Health Organization (WHO) recommendations of 60 min of moderate-to-vigorous PA (MVPA) per day [2]. As a result, widespread implementation of school-based PA programs at a population level have been recommended [3].
Adolescence is a key life stage, where investments could yield triple benefits – e.g. benefits today, into adulthood and into the next generation [4]. Despite the acknowledged benefits of a universal prevention approach, few school-based PA programs have been implemented at scale [5], particularly targeting adolescents. For example, recent reviews of PA programs implemented at scale found no programs targeting adolescents in the secondary school setting [6]. This is perhaps unsurprising given very few school-based PA programs targeting adolescents have demonstrated effective outcomes [7, 8]. Of the limited number of programs effective at increasing adolescent PA [7, 8], those tested under ideal research conditions may not be amenable for implementation at scale in real-world contexts, as they require expertise and resources not readily available within schools [7, 8]. Consequently, policy makers and practitioners select programs that require substantial adaptations for implementation at scale [9, 10], diluting their effectiveness [6]. Carefully planned adaptations to the implementation approach to support scale-up may overcome such challenges [9].
Physical Activity 4 Everyone (PA4E1) is an evidence-based PA program targeting secondary schools located in economically disadvantaged areas [11]. PA4E1 consists of a multi-strategy implementation support intervention (herein referred to as the ‘implementation intervention’) that aims to support schools to implement seven evidence-based PA practices, which have been shown to increase adolescent PA and improve weight status in a previous efficacy trial conducted from 2012 to 2014 [12,13,14,15]. The efficacy trial of PA4E1 cost AUD $329,952 over 24-months ($394 per student; $65,990 per school), equating to $56 ($35–$147) per additional minute of moderate to vigorous intensity PA [13]. For decision makers, outcomes relating to cost and economic analyses are an important consideration for scale-up [16]. To support the scale-up of PA4E1, the implementation intervention was adapted [11] to explicitly incorporate theoretically derived implementation support strategies. A 24-month randomised controlled trial of this adapted PA4E1 program was initiated in 2017. Results at 12-months (mid-program) demonstrated a significant increase in school PA practice implementation in the program schools compared to control schools, with 67% (16/24) of schools in the program arm implementing at least four of the seven school PA promoting practices compared to 4% (1/25) of schools in the control arm (OR = 33 [4–1556], p < 0.001) [17].
To address the need to scale-up and evaluate PA programs targeting adolescents, this paper extends on the previously reported 12-month outcomes [17] by evaluating the longer-term impacts at the completion of the 24-month implementation intervention. This paper reports the effectiveness, fidelity and reach, cost and cost-effectiveness of the implementation intervention on the implementation of school PA practices.
Methods
Study design and setting
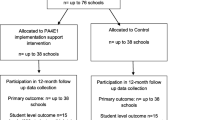
Details of the trial methods have been previously reported [11, 18]. Briefly, this trial employed a type III hybrid implementation-effectiveness design with 49 secondary schools located in New South Wales (NSW), Australia (Fig. 1). Secondary schools in NSW cater for 11–18 year olds (Grade 7–12). There are 509 secondary schools in NSW [19]. The three types of schools, Government, Catholic and Independent, represent 71, 18 and 11% of all schools, respectively [19, 20]. This paper reports the school-level implementation of PA practices (primary outcome), fidelity and reach of the implementation support strategies, and program costs and cost-effectiveness at completion of the 24-month implementation intervention (secondary outcomes). In line with the published protocols [11, 18], separate papers will report the secondary trial outcomes, such as PA outcomes and a comprehensive process evaluation [11, 18].
Consort Flow Diagram describing progress to 24 months (final follow-up). *Grade 7 enrolments [19]. # of Head PE Teacher
The trial adheres to Consolidated Standards of Reporting Trials (CONSORT) Statement (Supplementary File 1), the Standards for Reporting Implementation Studies (StaRI) Statement and checklist (Supplementary File 2) and the Template for Intervention Description and Replication (TIDieR) checklist (Supplementary File 3).
Sample, participants and recruitment
Schools were recruited from four NSW Local Health Districts (LHD); Mid-North Coast, South-Western Sydney, Central Coast and Hunter New England. Schools were eligible if they were: a) not involved in the original PA4E1 trial; b) Government or Catholic schools; c) enrolled students from grades 7–9; d) not a specialist academic/ sporting/ performing arts/ agriculture/ boarding school; e) located in areas classified as being disadvantaged by the SEIFA Index of Relative Socio-economic Disadvantage (suburb in lower 50% of NSW) [20]; and f) not participating in other major whole school PA trials or initiatives.
Eligible schools were stratified by LHD and school sector (Government or Catholic). A letter outlining the study was emailed to the school principal requesting the information be shared with Head Physical Education (PE) teachers. Secondary schools in NSW have a Head PE teacher who leads the Health and PE teachers. A PE trained project officer employed by the research team then contacted the principal or Head PE teacher to invite school participation. Face-to-face meetings and additional telephone meetings were offered to further outline the study requirements, confirm eligibility and gain written consent. In consenting schools, all PE teachers were emailed a study information sheet. At baseline, 12-month and 24-months, Head PE teachers were emailed an invitation to participate in a computer assisted telephone interview (CATI). Consent was implied by completing the CATI.
Randomisation and blinding
Stratified block randomisation was used to allocate consenting schools to one of two groups in a 1:1 ratio. Separate random block sequences of sizes two and four were used within each of eight strata. The blocks were created through SAS version 9.3. Population of the blocks involved using a random number generator in Microsoft Excel to randomise the order of the schools, prior to pasting into their respective stratum block. This was conducted by a statistician not involved in recruitment and blinded during the randomisation phase. Principals were notified by research staff of their school’s allocation to either the program (intervention) or usual care control following baseline collection of school practice measures (Head PE teacher CATI). Schools were not blinded to group allocation, however interviewers conducting the CATI were not informed of group allocation nor was the statistician undertaking the randomisation and analysis.
Evidence-based PA program (PA4E1) – program group
The program involved two components:
-
1)
Physical activity practices
The program protocol paper [11], process evaluation protocol paper [18] and 12-month midpoint outcomes paper [17] provide a detailed description of 7 PA4E1 school PA practices. A detailed description of adaptations to the original efficacy trial made for scale-up is reported separately [18]. The 7 PA practices were (i) quality PE Lessons; (ii) student PA plans; (iii) enhanced school sport program; (iv) recess/ lunchtime PA; (v) school PA policy or procedure; (vi) links with community PA providers; (vii) communicating PA messages to parents. The PA practices are further outlined in Supplementary File 4.
-
2)
Implementation intervention
Table 1 outlines the implementation intervention, consisting of seven overarching implementation strategies, within which there were 23 sub-strategies. The Behaviour Change Wheel and the Theoretical Domains Framework were used to develop the implementation intervention [11]. Implementation support was delivered over eight school terms (two school years) as described in Table 1.
Control group
Schools randomly allocated to the control group received no contact from the research team other than to participate in the study data collection at baseline, 12 and 24-months. These schools continued with their usual practices for delivering PE lessons, school sport and other PA programs and practices.
Data collection procedures and measures
Baseline data were collected August–October 2017, at 12-months from September–December 2018 and at 24-months from September–December 2019 following completion of the 24-month program. Schools were offered half a day of teacher relief ($175AUD) at each data collection point to reimburse for time.
Primary trial outcome
The primary outcome was the proportion of schools in each group implementing any four of the 7 PA practices at 24-months. Our prior efficacy trial demonstrated a significant effect on objectively measured student MVPA [12] when the implementation of four of the 7 PA practices was achieved by program schools. Measures of school practices were undertaken via CATI with Head PE teachers, administered by trained interviewers. The CATI items were pilot tested and forwarded to all participants via email before data collection. The questions relating to the implementation of the school practices within the current school year (2017 at baseline, 2018 at 12-months, 2019 at 24-months) are available in Supplementary File 5. For program schools, if Head PE teachers were not in the role of in-School Champion, they were asked to discuss (prior to the CATI) their schools involvement and uptake of the PA4E1 program with their PA4E1 in-School Champion. Telephone interviews (including CATI) regarding PA practice implementation have successfully been used in large studies with validity and reliability and achieve high response rates [21, 22].
Secondary outcomes
Mean number of school practices
Mean number of school PA practices implemented and whether or not schools implemented each of the seven practices were assessed via CATI as described for the primary outcome.
Fidelity and reach of implementation support strategies
To determine the proportion of schools that were provided (fidelity) and took up (reach) each of the seven implementation strategies (Table 1), we used: project records kept by External Support Officers, website usage data, termly implementation audit and feedback surveys completed by PA4E1 in-School Champions and Head PE teacher CATI. See Supplementary File 6 for an outline of the criteria for fidelity and reach.
Economic outcomes
Economic outcomes included the mean incremental cost per school and mean incremental cost per student to implement the program, mean cost per implementation support strategy and the incremental cost-effectiveness ratio (ICER). Incremental cost is the difference in the mean cost per student between study groups and the incremental effect is the difference in the primary trial outcome. The incremental cost–effectiveness ratio (ICER) represents the additional cost to achieve a percent change in the proportion of schools implementing at least four of the seven school PA practices (reflective of the primary trial outcome) [11]. Resource use was captured through a bespoke cost-capture tool. Economic outcomes are described in detail in Supplementary File 7.
School characteristics/ head PE teacher characteristics
Information regarding school sector, postcode, size (total enrolments), Indigenous enrolments, and students who speak a language other than English (LOTE) was assessed via publicly available data [23]. Additional information including number of PE teachers and full time equivalent PE positions at the school; language groups most commonly represented (when the school has more than 10% of students from LOTE households), sex of Head PE teacher, PE training, years of teaching experience, how long they’ve taught PE at their current school, and grades they teach in the current year were obtained through the Head PE teacher CATI.
Sample size
Using consent rates obtained from previous trials conducted in schools by the research team (65–70% consent) [14], a sample of 76 schools (38 per arm) was estimated to provide 80% power to detect an absolute increase of ~ 35% between groups in the proportion of schools implementing at least four of the seven practices at 24-months. Without prior data on baseline levels of school PA practices, this calculation made the assumption that 40% of schools in the control arm could achieve this target at follow-up.
Statistical analyses
All analyses were conducted using SAS, version 9.3, from February to April 2020. Characteristics of schools participating in the trial and those refusing participation were compared using Chi-square analyses and these results are reported in the 12-month midpoint outcomes paper, see Sutherland et al. [17]. School characteristics were summarised for program and control schools [17]. Analysis followed intention to treat principles, where schools were analysed according to their randomised treatment allocation. Given the low prevalence of practices at baseline, the number of schools per group, and almost no implementation by control schools at follow-up, the generalised linear regression models planned were not undertaken. Instead, dichotomous outcomes (implementing at least four of the seven practices (primary outcome) (yes, no) and each of the seven practices (secondary)) at 24-months were analysed using exact logistic regression models adjusting for baseline and for the stratification variables (LHD, school sector). For consistency in analysis approach, a linear regression model was used to assess differences between groups at 24-months on the continuous secondary outcome variable (number of PA practices), adjusting for baseline and the stratification variables. Significance levels for the analyses were set at p < 0.025 as per the trial protocol [11] to allow for program effects at 12 or 24-months.
Descriptive statistics were used to summarise the fidelity and reach of the implementation intervention over 0–12 months (previously published) [17], 12–24 months and 0–24 months (see Supplementary File 6 for further details). Per protocol analyses were undertaken for the primary outcome and one secondary outcome as described in Supplementary File 6. Economic analysis methods are described in Supplementary File 7.
Ethics approval
The trial was prospectively registered (ACTRN12617000681358) and approved by the Hunter New England Research Ethics Committee (Ref No. 11/03/16/4.05), University of Newcastle (Ref No. H-2011-0210), NSW Department of Education (SERAP 2011111), Maitland Newcastle Catholic School Diocese, Broken Bay Catholic School Diocese, Lismore Catholic School Diocese, Armidale Catholic School Diocese, and the Aboriginal Health and Medical Research Council.
Results
Sample characteristics
Figure 1 outlines the flow of schools and participants through the study. There were 184 secondary schools assessed for eligibility of which 78 schools were ineligible due to not meeting the inclusion criteria. Of the remaining 106 schools, 49 consented and 57 declined (Fig. 1, 46% consent rate). The reasons for declining [17] primarily related to lack of executive support, capacity to nominate an in-School Champion and concerns regarding allocation to the control group. There were no significant differences in the characteristics of schools declining to participate compared to consenting schools based on sector, LHD, size, percentage enrolment of Indigenous students or students speaking a language other than English (LOTE), except schools that declined were more likely to have 10% or more students of LOTE background (24/57 42% of refusers, 8/49 16% of consenting, p = < 0.05). The characteristics of participating schools at baseline are provided in Table 2.
Primary outcome: implementation of PA practices
Table 3 presents the school PA practice results, (including the previously published results at 12-months [17]) and the 24-month results. Two schools had missing data for one practice at baseline, and one school did not complete the 24-month follow-up CATI. For the primary outcome, at baseline no schools were implementing four of the seven school PA practices in the current school year. At 24-month follow-up, significantly more schools were implementing four of the seven school PA practices in the program group (16/23, 69.6%) than the control group (0/25, 0%) (p < 0.001). These results remained consistent even when the school missing 24-month data was included in the analysis as not meeting any practice. Figure 2 shows the proportion of schools meeting the primary outcome, implementation of four or more practices at baseline, 12 and 24-months, by group. Supplementary File 8 shows the number of program group schools meeting each practices at neither, 12-months only, 24-months only, or both 12- and 24-month follow-ups.
Secondary outcomes
Mean number of school practices
At 24-months, program schools were implementing a mean of 4.1 (1.7 SD) practices and control schools a mean of 0.5 (0.8 SD) practices, resulting in a difference favouring the program group of 3.6 practices more than schools in the control group (< 0.001). For six of the seven practices, schools in the program group were significantly more likely to implement them than the control group (see Table 3). The remaining school PA practice, links with community PA providers, was not significantly different between groups at 24-month follow-up (OR 3.1, 0.4-∞; p = 0.39). Fig. 3 shows the mean number of practices being implemented per school at baseline, 12 and 24-months, by group.
Per protocol analyses
Per-protocol results are reported in Table 3 and are consistent with the main analyses. The per-protocol program group (n = 13) was defined as up-taking (reach) at or above the median reach score for the implementation support strategies. At 24-month follow-up, significantly more per-protocol program schools had implemented four of the seven practices (10/13, 76.9%) than control group schools (0/25, 0.0%) (p < 0.001). After adjusting for baseline differences, the per-protocol program group was implementing a mean of 3.7 more practices than the control group at 24 months (p < 0.001).
Fidelity and reach of the implementation support strategies
Table 1 shows the overall mean fidelity score over 0–24 months (implementation support provided) across all schools was 94.4% (range 86.1–100.0%). Reach (uptake of the implementation support) was also high over 0–24 months at 75.5% (range 64.3–88.1%).
Cost and cost-effectiveness
Table 1 outlines the cost of each implementation support strategy per school. The total program cost over 24-months was $415,112 (95%UI $410,245 - $420,851), resulting in an incremental cost per school to receive the implementation intervention over 24-months being $17,296 (95%UI$17,094 - $17,535). Based on 3539 students enrolled in the target year 7, the mean incremental cost per student over 24-months was calculated to be $117.30. The incremental cost-effectiveness ratio was calculated to be $25,944 (95%UI $20,512 - $38,259) per percent increase in the proportion of school implementing at least four of the seven school PA practices.
Supplementary File 7 outlines the total cost and mean cost per school of the implementation intervention from baseline to 12-months, between 12 to 24-months and the overall costs of the implementation intervention across the 24-month program.
Discussion
Main findings
This implementation trial provides strong evidence, that with theoretically designed implementation support intended to address identified barriers, schools can overcome commonly reported implementation failure which has plagued many school-based PA trials [7]. At a cost of AUD$17,296 per school, the PA4E1 implementation intervention was effective at increasing secondary schools’ implementation of evidence-based school PA practices at 24-months. More than two thirds (69.6%) of schools in the program group were implementing at least four of the seven PA practices at the desired standard, averaging implementation of 4.1 of the recommended seven practices, whilst control schools implemented a mean of just 0.5 practices and no schools achieving implementation of at least four of the seven practices. Our exploratory per protocol analysis indicated that where uptake of the implementation support was greater, school implementation of practices were even higher, with 76.9% of per-protocol program schools implementing at least four of seven school-based PA practices. Our previous efficacy trial has demonstrated that this level of PA practice implementation within a school translates to greater daily MVPA and slower weight gain in adolescent students [12, 14, 24].
Findings in context
Whilst there are very few implementation trials of school-based PA programs in secondary schools to enable direct comparisons, a systematic review evaluating the effect of the limited number of school-based PA programs indicates that magnitude of the effect size, measured at the individual level, generally halves when programs are scaled up [6]. Given this, the magnitude of our findings, even though measured at a school level, appears large compared to systematic review findings and studies monitoring the implementation of school-based practices in the real world [5, 6]. For example, the unadjusted median effect size reported in a Cochrane systematic review of school-based implementation trials was just 19% (range 8.5 to 66.6%) [5]. Our study appears consistent with one implementation study undertaken within elementary schools utilising similar strategies to increase schools’ implementation of PA policies at scale, which resulted in an effect size of 40% difference between intervention and control group [25]. Both interventions utilised implementation theory to overcome identified school implementation barriers resulting in common implementation support strategies. These included harnessing executive support, appointing in-School champions, external support officers and the provision of equipment and resources [25].
We found that the first 12-months of the implementation intervention resulted in a sharp increase in school PA practice implementation. This impact appeared to be maintained, but not largely extended between 12 to 24-months (Fig. 3). This is similar to effects seen in the Live Life Well @ School (LLW@S) program, a comprehensive obesity prevention program in Australian primary schools. Consisting of ten school nutrition and PA practices, following ongoing implementation support from local health services, the proportion of schools implementing the desirable practices increased from 39.5% in year 2 to 71.4% in year 3 but remained at 72% after 5 years of implementation support. Therefore, intensive implementation support over an extended period may not be necessary to embed evidence-based strategies in a school setting. Instead, future research could examine if a low-intensity support model (at a lower cost) for sustainability may be more appropriate following an intensive initial implementation period.
Varying PA practice implementation
At an individual practice level, our implementation intervention resulted in significantly higher implementation of six of the seven school PA practices in the program group in comparison to the control schools. Formal links with community sport organisations being the only school PA practice that appeared to have very limited implementation by schools, even after 2 years of support. The challenge with formally working in partnership with community sports providers appears to be shared by other schools, and not unique to this trial [26]. Nonetheless, systematic reviews have demonstrated that school-based programs that include a community component result in greater impacts on student PA levels [27]. As a result, a greater emphasis on determining the school-level barriers and support required to overcome these is warranted. Interestingly, between the 12 and 24-months of the intervention, the implementation of four of the school PA practices (quality PE, recess and lunchtime PA, school PA policy and communicating with parents) increased, whilst the implementation of two school PA practices decreased in the same period (enhanced school sport, and slightly for student PA plans). The implementation of two curriculum based strategies decreased, which may demonstrate they are more challenging for schools to achieve. This is perhaps because schools were required to implement the curriculum strategies across the whole year group of students in order to achieve the practice. Additionally, staff turnover of PE teachers in some schools presented particular challenges.
Economic evaluation
In order to achieve population health gains, models of implementation need to be effective in changing practice in the real world, but also cost-effective to be implemented at scale or by segments of the community that would benefit most [28]. This 24-month program cost AUD$17,296 per school or AUD$117 per student. Unsurprisingly, there is a paucity of data regarding economic evaluations of implementation support interventions in general [28], but specifically limited empirical data evaluating the cost-effectiveness of school-based studies. In a systematic review of public health focused implementation studies, only one of the 14 included studies focused on economic evaluation [28], this being the cost-effectiveness evaluation of our previous PA4E1 school-based PA efficacy trial [13]. In comparison to our previous efficacy trial [13], which was deemed to be potentially cost-effective at a cost of AUD$65,990 per school, or AUD$394 per student, or AUD$56 per 1 min increase in MVPA, our implementation intervention (which was adapted from the previous efficacy trial for implementation at scale) is considerably less cost per school (74% less) and per student (70% less).
Comparisons to the pre-scale efficacy trial
The primary outcome of this scale-up trial was the implementation of four or more school PA practices [11], reported here. A secondary outcome is students mean daily MVPA assessed via wrist-worn accelerometer, which will be reported separately in line with methods reported in our trial protocol [11]. In the efficacy trial, the primary outcome was students waist-worn accelerometer measured MVPA, which had significant effects at 12 [12] and 24-month [14] follow-up. In the efficacy trial, implementation of school PA practices was measured via in-school consultant records (different to the current trial which uses Head PE teacher CATI). Although the measures differed, the original trial found a significant effect on student PA with the implementation of 4 of 7 practices [12, 14]. The efficacy trial also found that by 24-months, four of five schools were able to implement all school PA practices. By contrast, only one school in the current trial implemented all practices. It appears that practice implementation in the original trial was therefore higher than the current scale-up trial.
Our previous model of implementation relied primarily on a full time external change agent supporting five schools 1 day per week [14], whilst the current implementation intervention model utilizes a lower cost model, combining a website, an in-School Champion (an existing PE teacher funded 0.5 days per week) and support from an External Support Officer (ideally with PE teacher training) [13]. Given the high level of implementation achieved by schools, but also the relatively high cost of the implementation support, further opportunities to optimize the implementation model [9] should be explored by considering opportunities for further adaptations to reduce the absolute costs, and potentially improving cost-effectiveness. For example, further scale-up of the program could seek to evaluate if schools require a funded in-School Champion position or if this could be allocated within existing school resources. Similarly, if external implementation support could be provided via alternate modes of delivery, other than face-to-face support, further reducing the implementation costs. Evaluating the merit of optimised implementation models could occur via non-inferiority designs, embedded within further scale-up attempts, similar to other novel school-based PA scale-up interventions [25]. A similar process of continual optimization has been applied to a school nutrition program resulting in the development of a more cost-effective model of implementation support and achieving a halving of the ICER through an optimization process [10, 29]. A comprehensive process evaluation will be published separately and will assist decision makers in adapting the program for further scale-up [18].
Strengths and limitations
The primary outcome of this implementation trial relied on self-report via a Head PE teacher telephone interviews, which may be subject to social desirability. This is a limitation shared by other implementation trials [30], however such methods have also shown to be valid and reliable [21, 22]. Further, it is possible that increased implementation of school PA practices does not guarantee that increased activity is delivered or that all students participate, despite our previous trial which demonstrated an effect on student MVPA and weight status [12, 14, 24]. Finally, the 24-month practice data was collected immediately following the program delivery, as such it remains unknown if schools are able to sustain practice implementation, or further maintenance support would be required [25]. Importantly, even with these limitations, this was a large cluster randomised controlled trial that utilised implementation strategies and behaviour change techniques that were explicitly selected to address known barriers and mapped against a robust theoretical framework, evaluating both implementation and cost-effectiveness. This trial is one of the first implementation trials targeting school-based PA practices in secondary schools globally, therefore addressing a much needed research gap and providing critical evidence regarding future implementation of health programs and practices within secondary schools. Additional process evaluation data will be published elsewhere [18], to facilitate the interpretation of the trial outcomes [17]. Further, this trial was implemented over a 24-month period, which is consistent with systematic reviews of school-based programs suggesting that those of greater than 12-month duration were more likely to be effective. Lastly, it provides one of very few cost-effectiveness evaluations of an implementation support intervention in a real world setting. Taken together, the efficacy, implementation, process and cost evidence from the previous efficacy trial [12,13,14,15] and this scale-up trial [11, 17, 18] suggests this implementation intervention may be suitable for further scale-up at a population level (e.g. state-wide dissemination) [16, 31, 32].
Conclusion
This study provides robust evidence of an implementation intervention that is effective and potentially cost-effective to support the scale-up of evidence-based PA practices in secondary schools, a setting and target group in critical need of empirical evidence. To date, secondary school-based PA interventions have been limited by poor implementation, limiting their effectiveness to impact on student physical activity outcomes. Policy makers and researchers looking to support secondary schools to implement efficacious school PA practices should consider the use of a theoretically designed implementation intervention targeting known barriers to implementation.
Availability of data and materials
All study materials are available from the research team upon request to the corresponding author. All data are stored securely as per ethical requirements. All participants were issued a unique identification number following consent for confidentiality. The final trial dataset is stored securely and accessed only by the study statistician. The results of this trial are being disseminated via publications in peer reviewed journals, conference presentations, reports to schools and relevant health and education departments.
Abbreviations
- PA:
-
Physical Activity
- PA4E1:
-
Physical Activity 4 Everyone
- MVPA:
-
Moderate-to-vigorous intensity physical activity
- LOTE:
-
Language other than English
- NSW:
-
New South Wales
- PE:
-
Physical Education
- PDHPE:
-
Personal development, health and physical education
- CATI:
-
Computer assisted telephone interviews
References
Australian Institute of Health and Welfare. Impact of physical inactivity as a risk factor for chronic conditions: Australian burden of disease study. Australian burden of disease study series no. 15 cat. No. BOD 16. Canberra: AIHW; 2017. https://www.aihw.gov.au/getmedia/df392a65-8cf3-4c09-a494-4498ede2c662/aihw-bod-16.pdf.aspx?inline=true
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health. 2019;4;(1):23–35. https://doi.org/10.1016/S2352-4642(19)30323-2.
Milton K, Cavill N, Chalkley A, Foster C, Gomersall S, Hagstromer M, et al. Eight investments that work for physical activity. J Phys Act Health. 2021;18(6)625–30. https://doi.org/10.1123/jpah.2021-0112.
van Sluijs EMF, Ekelund U, Crochemore-Silva I, Guthold R, Ha A, Lubans D, et al. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. Lancet. 2021;398(10,298):429–42. https://doi.org/10.1016/S0140-6736(21)01259-9.
Wolfenden L, Nathan NK, Sutherland R, Yoong SL, Hodder RK, Wyse RJ, et al. Strategies for enhancing the implementation of school-based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst Rev. 2017;11:Cd011677.
Lane C, McCrabb S, Nathan N, Naylor P-J, Bauman A, Milat A, et al. How effective are physical activity interventions when they are scaled-up: a systematic review. Int J Behav Nutr Phys Act. 2021;18(1):16.
Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev. 2019;20(6):859–70. https://doi.org/10.1111/obr.12823.
Borde R, Smith JJ, Sutherland R, Nathan N, Lubans DR. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: a systematic review and meta-analysis. Obes Rev. 2017;18(4):476–90.
Yoong SL, Bolsewicz K, Grady A, Wyse R, Sutherland R, Hodder RK, et al. Adaptation of public health initiatives: expert views on current guidance and opportunities to advance their application and benefit. Health Educ Res. 2020;35(4):243–57.
Yoong SL, Nathan N, Reilly K, Sutherland R, Straus S, Barnes C, et al. Adapting implementation strategies: a case study of how to support implementation of healthy canteen policies. Public Health. 2019;177:19–25.
Sutherland R, Campbell E, Nathan N, Wolfenden L, Lubans DR, Morgan PJ, et al. A cluster randomised trial of an intervention to increase the implementation of physical activity practices in secondary schools: study protocol for scaling up the Physical Activity 4 Everyone (PA4E1) program. BMC Public Health. 2019;19(1):883.
Sutherland R, Campbell L, Lubans D, Morgan P, Okely AD, Nathan N, et al. ‘Physical Activity 4 Everyone’ school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Br J Sports Med. 2015;50(8):488–95.
Sutherland R, Reeves P, Campbell E, Lubans DR, Morgan PJ, Nathan N, et al. Cost effectiveness of a multi-component school-based physical activity intervention targeting adolescents: the ‘Physical Activity 4 Everyone’ cluster randomized trial. Int J Behav Nutr Phys Act. 2016;13:94.
Sutherland RL, Campbell EM, Lubans DR, Morgan PJ, Nathan NK, Wolfenden L, et al. The Physical Activity 4 Everyone cluster randomized trial: 2-year outcomes of a school physical activity intervention among adolescents. Am J Prev Med. 2016;51(2):195–205.
Sutherland R, Campbell E, Lubans DR, Morgan PJ, Okely AD, Nathan N, et al. A cluster randomised trial of a school-based intervention to prevent decline in adolescent physical activity levels: study protocol for the ‘Physical Activity 4 Everyone’ trial. BMC Public Health. 2013;13(1):57.
Lee K, Milat A, Grunseit A, Conte K, Wolfenden L, Bauman A. The intervention scalability assessment tool: a pilot study assessing five interventions for scalability. Public Health Res Pract. 2020;30(2):e3022011.
Sutherland R, Campbell E, McLaughlin M, Nathan N, Wolfenden L, Lubans DR, et al. Scale-up of the Physical Activity 4 Everyone (PA4E1) intervention in secondary schools: 12-month implementation outcomes from a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2020;17(1):100.
McLaughlin M, Duff J, Sutherland R, Campbell E, Wolfenden L, Wiggers J. Protocol for a mixed methods process evaluation of a hybrid implementation-effectiveness trial of a scaled-up whole-school physical activity program for adolescents: Physical Activity 4 Everyone (PA4E1). Trials. 2020;21(1):268.
Number of primary and secondary schools in Australia in 2020, by state. https://www.statista.com/statistics/612199/australia-primary-and-secondary-schools/. Accessed 14 Sept 2021.
Australian Bureau of Statistics. Australian Bureau of Statistics 2033055001 socio-economic indexes for areas (SEIFA). State suburb (SSC) index of relative socio-economicdisadvantage 2011. 2011. Available from: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012011?OpenDocument.
Lounsbery MAF, McKenzie TL, Morrow JR, Holt KA, Budnar RG. School physical activity policy. Assessment. 2013;10(4):496.
Nathan N, Wolfenden L, Morgan PJ, Bell AC, Barker D, Wiggers J. Validity of a self-report survey tool measuring the nutrition and physical activity environment of primary schools. Int J Behav Nutr Phys Act. 2013;10(1):75.
Australian Curriculum Assessment and Reporting Authority (ACARA). My school is a resource for parents, educators and the community to find information about each of Australia's schools. 2019 [Available from: https://myschool.edu.au/].
Hollis JL, Sutherland R, Campbell L, Morgan PJ, Lubans DR, Nathan N, et al. Effects of a ‘school-based’ physical activity intervention on adiposity in adolescents from economically disadvantaged communities: secondary outcomes of the ‘Physical Activity 4 Everyone’ RCT. Int J Obes. 2016;40(10):1486–93.
Nathan N, Hall A, McCarthy N, Sutherland R, Wiggers J, Bauman AE, et al. Multi-strategy intervention increases school implementation and maintenance of a mandatory physical activity policy: outcomes of a cluster randomised controlled trial. Br J Sports Med. 2021;Online first. https://doi.org/10.1136/bjsports-2020-103764.
Casey MM, Harvey JT, Telford A, Eime RM, Mooney A, Payne WR. Effectiveness of a school-community linked program on physical activity levels and health-related quality of life for adolescent girls. BMC Public Health. 2014;14(1):649.
van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335(7622):703.
Reeves P, Edmunds K, Searles A, Wiggers J. Economic evaluations of public health implementation-interventions: a systematic review and guideline for practice. Public Health. 2019;169:101–13.
Reilly KL, Reeves P, Deeming S, Yoong SL, Wolfenden L, Nathan N, et al. Economic analysis of three interventions of different intensity in improving school implementation of a government healthy canteen policy in Australia: costs, incremental and relative cost effectiveness. BMC Public Health. 2018;18(1):378.
Nathan N, Yoong SL, Sutherland R, Reilly K, Delaney T, Janssen L, et al. Effectiveness of a multicomponent intervention to enhance implementation of a healthy canteen policy in Australian primary schools: a randomised controlled trial. Int J Behav Nutr Phys Act. 2016;13(1):106.
Lai SK, Costigan SA, Morgan PJ, Lubans DR, Stodden DF, Salmon J, et al. Do school-based interventions focusing on physical activity, fitness, or fundamental movement skill competency produce a sustained impact in these outcomes in children and adolescents? A systematic review of follow-up studies. Sports Med (Auckland, NZ). 2014;44(1):67–79.
Milat A, Lee L, Grunseit A, Conte K, Wolfenden L, Bauman A. The intervention scalability Assessent tool: a guide for assessing the scalability of health interventions. Sydney: The Australian Prevention Partnership Centre; 2019. https://preventioncentre.org.au/wp-content/uploads/2019/11/The-ISAT-Oct-2019_FINAL.pdf. Accessed 12 Oct 2021.
NSW Department of Education. School sports unit - developing procedures for school sport. 2019 [Available from: www.Gdurl.com/wEEE].
Acknowledgements
The authors wish to acknowledge the NSW Department of Education School Sport Unit for their advice with the study.
Funding
This project is funded by the NSW Ministry of Health, Translational Research Grant Scheme and a Cancer Council NSW Program Grant. The NSW Ministry of Health has not had any role in the design of the study as outlined in this protocol and will not have a role in data collection, analysis of data, interpretation of data and dissemination of findings. The project also received infrastructure support from the Hunter Medical Research Institute (HMRI). RS and NN are supported by a NHMRC TRIP Fellowship (APP1150661 and APP1132450. NN is also supported by a Hunter New England Clinical Research Fellowship; LW is supported by a NHMRC Career Development Fellowship (APP1128348), Heart Foundation Future Leader Fellowship (101175) and a Hunter New England Clinical Research Fellowship; DRL is supported by an Australian Research Council Future Fellowship.
Author information
Authors and Affiliations
Contributions
RS and EC led the development of this manuscript. RS, EC and JW conceived the intervention concept. JW, RS, EC, NN, LW, PJM, DRL, KG, CO, AS, MW, NE and AB secured funding for the study. RS, EC, NN, PJM, DRL, LW, KG and CO guided the design and piloting of the intervention. RS, LC, MM, NN, PJM, DRL, LW, KG and CO guided the evaluation design and data collection. PR and AS contributed to the development of data collection methods specific to the cost and cost-effectiveness measures. MM and TM developed data collection methods specific to the fidelity, reach and per-protocol analyses. CO developed the analysis plan. RS, EC, MM, NN, PJM, DRL, LW, KG, CO, AS, PR, MW, NE, AB, RM and JW are all members of the Advisory Group that oversee the program and monitor data. All authors contributed to developing the protocols and reviewing, editing, and approving the final version of the paper.
Corresponding author
Ethics declarations
Ethics approvals and consent to participate
The study has been approved by the Hunter New England Human Research Ethics Committee (Ref No. 11/03/16/4.05, University of Newcastle (Ref No. H-2011-0210), NSW Department of Education (SERAP 2011111), Maitland Newcastle Catholic School Diocese, Broken Bay Catholic School Diocese, Lismore Catholic School Diocese, Armidale Catholic School Diocese, and the Aboriginal Health and Medical Research Council. To gain schools consent to participate in the study, a letter inviting schools was emailed to all school Principals, requesting the information be shared with the Head PE teacher. The Principal and/ or Head PE teacher was then contacted by telephone by a dedicated recruitment Project Officer with PE teacher training. A face-to-face or telephone meeting was then offered to outline the requirements of the study and confirm eligibility. Following school consent, all PE staff were provided with a study information letter that outlined the purpose of the study and level of involvement expected.
Consent for publication
Not applicable.
Competing interests
Authors RS, LC, NN, LW, KG, MW, NE, AB and JW receive salary support from their respective Local Health Districts. Hunter New England Local Health District contributes funding to the PA4E1 program.. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Supplementary File 1. CONSORT Checklist.
Additional file 2
: Supplementary File 2. StaRI Checklist.
Additional file 3
: Supplementary File 3. TIDieR Checklist.
Additional file 4
: Supplementary File 4. Overview of the evidence-based PA4E1 program (physical activity practices) including standards required of program schools (essential elements) and additional desirable elements.
Additional file 5
: Supplementary File 5. Overview of the interview questions assessing school physical activity practice implementation.
Additional file 6
: Supplementary File 6. Fidelity, reach and per-protocol analyses.
Additional file 7
: Supplementary File 7. Economic evaluation.
Additional file 8
: Supplementary File 8. Practice implementation for each practice.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sutherland, R., Campbell, E., McLaughlin, M. et al. Scale-up of the Physical Activity 4 Everyone (PA4E1) intervention in secondary schools: 24-month implementation and cost outcomes from a cluster randomised controlled trial. Int J Behav Nutr Phys Act 18, 137 (2021). https://doi.org/10.1186/s12966-021-01206-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-021-01206-8