Abstract
Background
Heuristic cadence (steps/min) thresholds of ≥100 and ≥ 130 steps/min correspond with absolutely-defined moderate (3 metabolic equivalents [METs]; 1 MET = 3.5 mL O2·kg− 1·min− 1) and vigorous (6 METs) intensity, respectively. Scarce evidence informs cadence thresholds for relatively-defined moderate (≥ 64% heart rate maximum [HRmax = 220-age], ≥ 40%HR reserve [HRR = HRmax -HRresting, and ≥ 12 Rating of Perceived Exertion [RPE]); or vigorous intensity (≥ 77%HRmax, ≥ 60%HRR, and ≥ 14 RPE).
Purpose
To identify heuristic cadence thresholds corresponding with relatively-defined moderate and vigorous intensity in 21–60-year-olds.
Methods
In this cross-sectional study, 157 adults (40.4 ± 11.5 years; 50.6% men) completed up to twelve 5-min treadmill bouts, beginning at 0.5 mph and increasing by 0.5 mph. Steps were directly observed, HR was measured with chest-worn monitors, and RPE was queried in the final minute of each bout. Segmented mixed model regression and Receiver Operating Characteristic (ROC) curve analyses identified optimal cadence thresholds, stratified by age (21–30, 31–40, 41–50, and 51–60 years). Reconciliation of the two analytical models, including trade-offs between sensitivity, specificity, positive and negative predictive values, and overall accuracy, yielded final heuristic cadences.
Results
Across all moderate intensity indicators, the segmented regression models estimated optimal cadence thresholds ranging from 123.8–127.5 (ages 21–30), 120.2–126.0 (ages 31–40), 117.7–122.7 (ages 41–50), and 113.3–116.1 steps/min (ages 51–60). Corresponding values for vigorous intensity were 140.3–144.1, 139.6–142.6, 139.3–143.6, and 131.6–132.8 steps/min, respectively. ROC analysis estimated chronologically-arranged age groups’ cadence thresholds ranging from 114.5–118, 113.5–114.5, 104.6–112.9, and 103.6–106.0 across all moderate intensity indicators, and 124.5, 121.5, 117.2–122.2, and 113.0 steps/min, respectively, for vigorous intensity.
Conclusions
Heuristic cadence thresholds corresponding to relatively-defined moderate intensity for the chronologically-arranged age groups were ≥ 120, 120, 115, and 110 steps/min, regardless of the intensity indicator (i.e., % HRmax, %HRR, or RPE). Corresponding heuristic values for vigorous intensity indicators were ≥ 135, 130, 125, and 120 steps/min. These cadences are useful for predicting/programming intensity aligned with age-associated differences in physiological response to, and perceived experiences of, moderate and/or vigorous intensity.
Trial registration
Clinicaltrials.gov NCT02650258. Registered 24 December 2015.
Similar content being viewed by others
Introduction
Physical inactivity is a leading risk factor for death worldwide [1, 2]. Strategies are needed to help individuals accumulate recommended levels of physical activity (PA) corresponding to improved health [2, 3]. Walking is the most commonly reported form of exercise (i.e., planned and structured PA) among adults and is an essential characteristic of daily mobility, domestic chores, and occupational pursuits [4, 5]. Therefore, it is a reasonable approach to achieve PA recommendations [3, 4]. The functional unit underlying walking behavior is a step, and the recent surge of commercially available wearable technologies capable of detecting step-by-step ambulatory patterns can quantify step-defined PA [6, 7]. Although the benefits of accumulating a high daily volume of steps are understood [8, 9], a focus on volume overlooks the rate or frequency of stepping (i.e., cadence [steps/min]), and therefore intensity, a critical tenet of health-related PA recommendations [3, 10].
Walking cadence has emerged as a proxy-indicator of ambulatory intensity, and manipulating cadence is a simple way to increase accumulated time spent at moderate or vigorous intensity thresholds associated with optimal health benefits [7]. The 2018 U.S. Physical Activity Guidelines Advisory Committee Scientific Report [3] emphasizes steps accumulated throughout the day may be taken at a light intensity (defined as a slow and leisurely pace) and therefore encouraged brisk (a distinctly non-quantitative directive) walking as a strategy for adults to reach moderate and vigorous intensity. Further, these guidelines specifically state that “as a basis for setting step goals, it is preferable that people know how many steps they take per minute” [3]; however, the guidelines provided little direction on what this specific value for cadence should be.
PA intensity can be defined in absolute or relative terms. Absolutely-defined intensity is the weight-standardized oxygen cost associated with a specific activity (i.e., often expressed in metabolic equivalents, METs; 1 MET = 3.5 mL·kg− 1·min− 1 of O2 uptake), while relatively-defined intensity is typically expressed as a percentage of an individual’s physiological capacity (i.e., percentage of maximal oxygen uptake [%VO2max], percentage of heart rate maximum [%HRmax], percentage of heart rate reserve [%HRR]), or based on Borg rating of perceived exertion (RPE), an indicator of an individual’s personal experience of the intensity [11,12,13]. Public health recommendations are built around absolute definitions of PA intensity [3], whereas clinical exercise prescriptions typically focus on relative definitions that attempt to address intensity-related physiological responses respective to an individual’s performance capacity or perceived experience [11]. In this context, heuristic values, while rounded, are evidence-based, informative, and practical. The purpose of a heuristic strategy is to provide a mental shortcut that enables quick decision making for the user, without requiring complex calculation methods [14]. Heuristic cadence thresholds of ≥100 and ≥ 130 steps/min are consistently associated with absolutely-defined moderate and vigorous intensities, respectively [5, 15,16,17,18,19,20,21]. However, little research currently exists to inform heuristic cadence thresholds corresponding to moderate or vigorous PA intensity in relative terms in adults. The two studies that do exist in adults younger than 65 years [19, 22] yielded clearly dissimilar estimates (i.e., 120 vs. 140 steps/min indicative of relatively-defined moderate intensity). This divergence is possibly due to study design differences in terms of sample size (N = 43 vs. N = 20) or age range (20–64 vs. 18–50 years of age), and discrepant approaches to assessing cadence (direct observation vs. device-derived). Further, one study utilized a submaximal protocol to estimate aerobic capacity [19], while the other utilized a maximal test [22]. Maximal aerobic capacity testing is the acknowledged criterion standard, yet it is not always practical due to the elevated participant burden and/or discomfort associated with the protocol, the expertise required to carry out such tests, and the costs associated with the necessary equipment and space [23]. More accessible and feasible approaches to defining relative intensity have the potential to reach wider audiences. For example, the American College of Sports Medicine (ACSM) [23] defines relative intensity using HR or RPE. Specifically, moderate intensity is defined as 64–76% HRmax, 40–59% HRR, or 12–13 RPE (‘fairly light to somewhat hard’) and vigorous intensity is defined as ≥77%HRmax, ≥ 60%HRR, or ≥ 14 RPE (‘somewhat hard to very hard’). These thresholds are heuristic recommendations widely used by clinicians and health practitioners to prescribe and monitor an individual’s exercise response within an expected range [11, 13, 23]. However, to our knowledge, no studies have utilized these more accessible intensity indicators (i.e., HRmax, HRR, and RPE) for establishing relatively-defined moderate or vigorous cadence-based thresholds.
Adults experience physiological changes as a result of aging, and therefore, an individual’s age should be taken into consideration when monitoring and prescribing exercise. For example, as people grow older, one’s response to acute exercise bouts is influenced by loss of muscle mass, increased blood pressure, and structural changes to the heart muscle [23,24,25]. Because of this well-known relationship between age and physical fitness, more research is needed on relatively-defined cadence thresholds specifically stratified by age groups. Thus, the present study aimed to: 1) analyze the relationship between cadence and relatively-defined PA intensity in a purposeful sex- and age-stratified sample of adults ranging from 21 to 60 years of age; and 2) identify heuristic cadence thresholds associated with accessible and commonly accepted indicators of relatively-defined moderate and vigorous PA intensity, specifically, %HRmax, %HRR, and RPE.
Methods
Study design and regulatory information
CADENCE-Adults was a cross-sectional, laboratory-based study registered with Clinicaltrials.gov (NCT02650258). The University of Massachusetts Amherst Institutional Review Board Data approved the study protocol. Data collection for 21–60-year-old adults was conducted at the University of Massachusetts Amherst from January 2016 to October 2017. Each participant provided signed informed consent. The complete methodology, procedures, and inclusion/exclusion criteria have been described in a previous report [20] and are briefly described herein.
Participants
To ensure a sex- and age-balanced sample, minimize sources of bias and improve the generalizability of the findings, 160 ambulatory adults were recruited, representing 10 men and 10 women for each 5-year age-group between 21 and 60 years (i.e., 21–25, 26–30, 31–35 years of age, etc.). Exclusion criteria included: current tobacco use, pregnancy, hospitalization for mental illness in the past 5 years, body mass index (BMI) < 18.5 kg/m2 or > 40 kg/m2, stroke or cardiovascular disease, Stage 2 hypertension (systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 100 mmHg), use of medication and/or diagnosis of a condition that could alter HR response to exercise, and implantation of a pacemaker or similar implanted medical device. Details regarding sample size calculation, risk stratification process, and clinical safety testing procedures have been previously published [20].
Treadmill testing procedures
Participants (fasted at least 4 h) were fitted with T31 Coded Transmitter chest strap (Polar Kempele, Finland). Resting HR was assessed after 5 min of sitting quietly. Participants then performed up to twelve 5-min treadmill walking bouts separated by 2-min standing rest periods on a Cybex 751 T (Cybex International Inc., MA, USA). Treadmill grade was maintained at 0% for the duration of the protocol and speed (regularly verified using a tachometer) increased from 0.5 mph (13.4 m/min) to a maximum of 6.0 mph (160.9 m/min) in 0.5 mph (13.4 m/min) increments. HR was monitored for the duration of the treadmill test, and participants were asked to self-report RPE during the last minute of each bout using the 6 to 20 Borg scale [26]. The test was terminated when the participant either: 1) transitioned to running; 2) achieved > 75% of age-predicted HRmax [0.75 * (220-age)]; 3) reported ≥14 RPE. However, participants finished their respective bouts in which they exceeded these termination criteria unless a safety concern arose. Additionally, either the participant or the research staff could terminate the protocol for any other reason, including fatigue, instability, or other safety concerns.
Measures and related data treatment
Participant characteristics and anthropometric variables
Sex, age, and race/ethnicity were self-reported for descriptive purposes. Standing height, leg length, and weight were collected using a standardized protocol as detailed previously [20]. Briefly, standing height was measured using a wall-mounted stadiometer (ShorrBoard® Infant/Child/Adult Portable Height-Length Measuring Board; Weigh and Measure LLC, Olney, Maryland, USA). Leg length was calculated by subtracting the seated height, measured by a stadiometer, from standing height. Weight was assessed using a scale (DC-430 U; Tanita Corporation, Tokyo, Japan). For each of these three parameters, up to three measurements were taken if the first two measurements differed by > 0.3 cm, in the case of standing height or leg length, or by > 0.5 kg, in the case of weight. The two closest measurements for each parameter were averaged. Body mass index (BMI) was calculated by dividing body weight by standing height squared (kg/m2) [27].
Cadence
Steps were directly observed and counted via hand-tally during each treadmill bout. A video camera recording of the participants’ feet served as a back-up verification source. Total tallied steps per bout were divided by 5 (bout duration) to obtain a measurement of cadence in steps/min.
Relative intensity variables
To approximate steady-state HR, the HR data were averaged over minutes 2:45–3:45 and 3:45–4:45 of each 5-min bout. HRmax was estimated using the standard equation of 220 - age [23]. HRresting was based on the lowest observed HR during seated rest before the treadmill protocol. HRR was calculated using HRmax - HRresting. RPE was queried in the last minute of each treadmill bout. Relative intensity was interpreted using the ACSM Guidelines for Exercise Testing and Prescription [23]. Thus, the relatively-defined moderate intensity indicators were defined as ≥64%HRmax [100 * (HR/HRmax)], ≥ 40%HRR [100 * (HR - HRresting) / (HRmax - HRresting)], and ≥ 12 RPE. Relatively-defined vigorous intensity was defined as ≥77%HRmax, ≥ 60%HRR, and ≥ 14 RPE.
Analytic sample
Data from four participants were not included due to equipment malfunction. Therefore, the final analytic data set included 156 adults (40.4 ± 11.5 years; 50.6% men) representing 1214 treadmill walking bouts, regardless of whether the participant reached the relatively-defined moderate or vigorous intensity thresholds. Running is a biomechanically distinct ambulatory pattern [3] and therefore the running and walking cadence-intensity relationships differ. Since the purpose of this analysis was to evaluate the relationship between walking cadence and relatively-defined moderate and vigorous intensity, the limited number of running bouts (n = 27 in total, 2.2% of all bouts) were deliberately excluded, leaving 1214 walking bouts for this specific analysis. The final analytical dataset and corresponding data dictionary are provided in Additional files 1 and 2, respectively, formatted in accordance with those previously published in earlier reports from the CADENCE-Adults study [20, 21].
Statistical analysis
Sample characteristics are presented as means and standard deviations or percentages, as appropriate. A non-linear relationship was observed between cadence and each of the relatively-defined intensity indicators. Specifically, the data displayed two distinct linear trends before and after a breakpoint. Therefore, consistent with previous analyses [20, 21], a segmented regression model was used to quantify the cadence-intensity relationship separately for four different age groups (Group 1: participants 21–30 years; Group 2: participants 31–40 years; Group 3: participants 41–50 years; Group 4: participants 51–60 years). The breakpoint was identified using an iterative process to determine that which minimized the mean square error of the model. Also, since each participant provided multiple data points (i.e., they provided repeated measures of variables across treadmill bouts), thus violating the assumption of data independence, the segmented regression model was fitted with fixed and random coefficients. This approach incorporated random intercepts to account for participant effects. Marginal R2 values, which represent the proportion of variance in relatively-defined intensity explained by a model’s fixed effects, were used to assess model fit. Based on previous studies also addressing the relationship between cadence and relatively-defined intensity [19], sex, leg length, and BMI were included as additional variables in separate and individual segmented regression models to control for their potential moderating effects. Marginal R2 values for each of these analyses were interpreted to determine whether these additional variables improved the overall prediction of the model.
Consistent with previous analyses [20, 21], we used the segmented regression equation along with the 95% prediction intervals (PIs) to solve for incremental cadence thresholds corresponding to each relatively-defined moderate and vigorous intensity indicator. Classification accuracy of walking bouts was determined respective to each intensity indicator’s identified optimal cadence threshold. As a single example, walking bouts that were ≥ 40%HRR and also ≥ the identified optimal cadence threshold were classified as true positives (TP). If they were < 40%HRR and also < the identified optimal cadence threshold they were classified as true negatives (TN). Accordingly, false positives (FP) and false negatives (FN) were classified if walking bouts were mismatched between the criterion intensity indicator and the identified optimal cadence threshold. Each optimal cadence threshold was then evaluated in terms of sensitivity (the probability of a cadence threshold accurately identifying walking at greater than or equal to a specific relative intensity threshold), specificity (the probability of a cadence threshold accurately identifying walking below a specific relative intensity threshold), positive predictive value [PPV = TP / (TP + FP); the probability of an individual walking at a given cadence achieving a specified relative intensity level], negative predictive value [NPV = TN / (TN + FN); the probability of an individual walking below a given cadence not achieving a specified relative intensity level], and overall accuracy [(TP + TN)/(TP + TN + FP + FN)].
A Receiver Operating Characteristic (ROC) curve analysis, which evaluates classifiers by displaying the performance of a binary classification method with continuous or discrete ordinal output, was also performed [28]. For relatively-defined moderate intensity, twelve ROC curves were estimated corresponding to cadence-based classifications of reaching ≥64%HRmax, ≥ 40%HRR, or ≥ 12 RPE for each of the four age groups. For vigorous intensity, another twelve ROC curves were estimated corresponding to cadence-based classifications of reaching ≥77%HRmax, ≥ 60%HRR, or ≥ 14 RPE. Also, an optimal threshold was then identified for each ROC curve analysis by selecting the cadence that maximized Youden’s index (a measure of the overall rate of correct classification, i.e., a sum of sensitivity and specificity) [29, 30]. Sensitivity, specificity, PPV, NPV, overall accuracy, and area under the curve (AUC) were also reported. AUC values were interpreted as poor (< 0.70), fair (0.70–0.79), good (0.80–0.89), and excellent (≥ 0.90) [28]. The bootstrap method with 20,000 replicates was used to identify 99% CIs for optimal cadence thresholds and AUC values [31].
The two analytical methods (regression and ROC analysis) were each used to derive two optimal thresholds, one for a particular age group and intensity. Heuristic cadence thresholds (i.e., rounded multiples of 5 steps/min) were set based on optimal thresholds associated with relatively-defined intensity indicators and identified from the segmented regression and ROC analyses. Guided by our previous work [20, 21], we settled upon heuristic values using an a priori systematic reconciliation process that considered the trade-offs in terms of sensitivity, specificity, PPV, NPV, and overall accuracy between the two analytical approaches. The final selected heuristic cadence thresholds purposely reflected a favored tolerance for FN versus FP classifications.
Results
Sample characteristics
Descriptive characteristics of the analytical sample (N = 156) are reported in Table 1. Table 2 presents the number of participants who completed each treadmill bout, including treadmill speed, cadence, and relative intensity indicators at each bout.
Segmented regression model
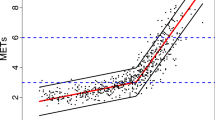
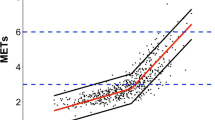
The segmented regression analysis revealed that, among all the relatively-defined intensity indicators, cadence was most strongly associated with %HRR (marginal R2 values ranging from 0.67 in the oldest age group [Group 4] to 0.73 in the youngest age group [Group 1]) (Fig. 1). Figure 1 shows a wider distribution of data points for %HRMax than for %HRR across cadences, and therefore narrower PIs driving higher correlations between cadence and %HRR. Marginal R2 values ranged from 0.54–0.60 for the relationship between cadence and %HRmax and from 0.57–0.71 for the cadence and RPE relationship (from the oldest to youngest group, respectively). There was no substantial improvement in these models’ performance when sex, leg length, or BMI were considered (marginal R2 only varied by ~ 0.02).
Relationship between cadence and relative intensity indicators (%HRMax = %Heart rate maximum; %HR reserve = %Heart rate reserve; RPE = Rate of Perceived Exertion) using a segmented regression model by age groups. Red line is the mean relative intensity value at each corresponding cadence value, and black lines are the 95% prediction intervals. Blue horizontal dotted lines represent moderate and vigorous intensity threshold for each indicator.
Optimal cadence thresholds for relatively-defined moderate and vigorous intensity identified via the segmented regression models are detailed in Table 3. Across all intensity indicators, the optimal cadence thresholds associated with moderate intensity ranged from 123.8–127.5 steps/min for age Group 1, 121.3–126.0 steps/min for Group 2, 117.7–122.7 steps/min for Group 3, and 113.3–116.1 steps/min for Group 4. Corresponding values for relatively-defined vigorous intensity were 140.3–144.1 steps/min (Group 1), 140.2–142.6 steps/min (Group 2), 139.3–143.6 steps/min (Group 3), and 131.6–132.8 steps/min (Group 4). Across all intensity indicators, sensitivity values were 51.6–79.6% for moderate intensity and 12.5–38.1% for vigorous intensity, whereas corresponding specificity values ranged from 89.1–96.7% and 97.2–99.7%. PPV values were 60.0–80.5% for moderate intensity and 33.3–71.4% for vigorous intensity indicators, while NPV values were 80.8–96.1% and 94.2–97.7% for moderate and vigorous intensity indicators, respectively. Across all intensity indicators, overall accuracy was 80.0–91.9% for moderate intensity and 91.8–97.4% for vigorous intensity.
Receiver operating characteristic analyses
Table 3 also presents ROC analysis results for optimal cadence thresholds related to relative-defined intensity. Values for all relatively-defined moderate intensity indicators were 114.5–118.5 steps/min for age Group 1, 113.5–114.5 steps/min for Group 2, 104.6–112.9 steps/min for Group 3, and 103.6–106.0 steps/min for Group 4. Cadence threshold values for relatively-defined vigorous intensity were 127.5 steps/min (Group 1), 121.5 steps/min (Group 2), 117.2–123.2 steps/min (Group 3), and 113.0 steps/min (Group 4). Across all indicators, sensitivity values were 75.3–100.0% for moderate intensity and 81.0–100% for vigorous intensity, while specificity values were 68.8–90.8% for moderate intensity and 72.8–92.9% for vigorous intensity (Table 3). PPV values were 26.7–67.9% and 15.7–27.0% for moderate intensity and vigorous intensity indicators, respectively, while NPV values were 88.2–100% for moderate intensity and 98.4–100% for vigorous intensity indicators. Across all intensity indicators, overall accuracy was 72.8–90.9% for moderate intensity and 74.1–92.1% for vigorous intensity. AUC values were 87.8–96.9% and 82.9–94.6% both for moderate and vigorous intensities, respectively, indicating good to excellent classification [28].
Heuristic thresholds
Table 4 presents the identified heuristic cadence thresholds and associated classification accuracy metrics for each age group. For simplicity of presentation, relatively-defined heuristic cadence thresholds identified for each age group are summarized in Table 5, along with the age group-specific absolutely-defined heuristic threshold previously published [20, 21]. Heuristic thresholds representing all relatively-defined moderate intensity indicators were consistently 120 steps/min for age Group 1 and Group 2, 115 steps/min for Group 3, and 110 steps/min for Group 4. Heuristic thresholds for all vigorous intensity indicators were, in age-defined chronological order, 135, 130, 125, and 120 steps/min. Across all intensity indicators, sensitivity values were 61.2–91.8% and 50.0–82.3% for moderate and vigorous intensities, respectively, while specificity values were 79.6–92.0% for moderate intensity and 87.3–98.0% for vigorous intensity (Table 4, Additional File 3). PPV values were 47.2–74.3% for moderate intensity and 23.9–95.5% for vigorous intensity indicators, while NPV were 83.9–98.3% and 30.2–98.9% for moderate and vigorous intensity indicators, respectively. With all intensity indicators included, overall accuracy was 80.0–96.2% for moderate intensity and 86.9–98.4% for vigorous intensity, again indicating good to excellent classification for both.
Discussion
Heuristic cadence thresholds of ≥120, 120, 115, and 110 steps/minute corresponded with all relatively-defined moderate intensity indicators for age Group 1 (21–30 years), Group 2 (31–40 years), Group 3 (41–50 years), and Group 4 (51–60 years), respectively. After considering possible compromises in terms of each of the classification accuracy metrics calculated from both the segmented regression and ROC analyses, these final heuristic thresholds demonstrated an average overall accuracy (i.e., the proportion of TP plus TN) of 88% across age groups for the classification of relatively-defined moderate intensity final heuristic thresholds. In some cases, we evaluated classification accuracy metrics for several candidate heuristic thresholds before settling on a final value. For example, for age Group 1, the optimal cadence thresholds corresponding to moderate %HRmax ranged from 115.5 (ROC) to 127 steps/min (regression) and therefore possible heuristic threshold candidates were 115, 120, and 125 steps/min. After considering the trade-offs between these two analyses and analyzing the classification accuracy metrics, 120 steps/min was the heuristic cadence threshold that favored the most tolerance for FN versus FP as noted above. Further, heuristic cadence thresholds of ≥135, 130, 125, and 120 steps/min were associated with all vigorous intensity indicators for each chronologically arranged age group. While previous research in adults consistently supports cadence thresholds of ≥100 and ≥ 130 steps/min associated with absolutely-defined moderate and vigorous intensity, respectively [7], the cadences required to reach relatively-defined moderate and vigorous intensities are not only comparatively higher but also dependent on age. For example, while 100 steps/min is a useful minimal threshold for evaluating absolutely-defined moderate intensity as defined by oxygen cost standardized to body weight, an individual within the range of 21–30 years of age would be expected to walk at a heuristic cadence of ≥120 steps/min to reach a moderate intensity relatively-defined by their age-influenced physiological response (e.g., %HRR, which considers age in its formulation) or perceived exertion. Although not personalized, these heuristic thresholds for moderate and vigorous relatively-defined intensity can help guide clinical and individual PA practice by providing evidence-based expectations for age-appropriate, step-defined relative intensity. For example, health practitioners can use this information for exercise prescription and other clinical or personal training-type settings without having to conduct an exercise test to further personalize values. Additionally, researchers can utilize these heuristic thresholds as a reference when analyzing and interpreting ambulatory data obtained from contemporary step-counting wearable technologies or as a guide for age-standardized walking interventions.
Only two previous studies reported cadence thresholds associated with relatively-defined intensity in young and middle-age adults, and results were discrepant [19, 22]. O’Brien et al. [19] directly-observed treadmill-based cadence in 43 adults 20–64 years of age (mean age = 39 years, 42% men) and reported 125 (using mixed-effect modeling) and 120 steps/min (using ROC analysis) as thresholds associated with moderate intensity, defined as ≥40%METmax. Their findings are consistent with the ≥120 steps/min heuristic threshold identified herein for those in Group 1 (21–30 years) and Group 2 (31–40 years). Further, O’Brien et al. reported 134 steps/min associated with vigorous intensity, which they defined as ≥60%METmax. This finding is also consistent with our heuristic threshold of ≥135 steps/min for those in Group 1 (21–30 years). In contrast, Abt et al. [22] derived cadence from a wrist-worn wearable technology (Apple Watch OS 2.0.1) during a treadmill-based study of 20 adults 18–50 years of age (mean age = 32 years, 50% men). They used a Bayesian regression model to extrapolate (not directly measured/observed) that 140 steps/min was indicative of relatively-defined moderate intensity, defined as ≥40%VO2 reserve. Abt et al. [22] did not report a cadence threshold associated with vigorous intensity, and the average cadence reached in their study, 130 steps/min, was associated with an intensity of 34%VO2 reserve at the fastest treadmill speed (3.7 mph). It is important to reiterate that the participants in the Abt et al. study did not actually reach 140 steps/min. Instead, this value was extrapolated and not directly captured by the wrist-worn wearable technology. Furthermore, the walk-to-run transition is known to occur at ~ 140 steps/min [32, 33]. Running is considered a vigorous intensity PA in most adults, and it is distinctly different from walking [34], so the proposed cadence threshold of 140 steps/min [22] is doubtfully a true indicator of moderate intensity walking [35]. This conclusion is also supported by the fact that 140 steps/min is 20 steps/min higher than both the moderate and vigorous intensity thresholds cadences identified herein or by O’Brien et al. [19].
Differences in age ranges, indicators, definitions of relatively-defined intensity, walking speeds (i.e., lack of very low walking speeds such as 0.5 or 1.0 mph), and/or the use of varying statistical approaches may explain the discrepancies between studies. Another possible explanation is the use of different methods for measuring cadence. Abt et al. [22] derived cadence from wrist-worn wearable technology, while O’Brien et al. [19] and the present study utilized direct observation [36]. Notably, prior research on wearable technologies has reported that wrist-worn devices can significantly over-or under-estimate energy expenditure [37] and called for increased accuracy in wrist-worn devices due to low validity findings [38]. Specifically, a review by Moore et al. [39] reported that median aggregated values of step count mean absolute percentage error (MAPE) error representing the comparison between direct observation and wearable technologies were higher for wrist-worn devices (MAPE = 7 to 11%) than for waist-worn (MAPE =1 to 4%), or thigh-worn (MAPE ≤1%).
The present study mitigated the possibility of the aforementioned issues by incorporating a sex-and-age balanced sample (i.e., ~ 40 adults per age decade) as well as direct observation of steps. Further, our analysis employed and harmonized the findings from two analytical approaches (segmented regression and ROC analysis) and incorporated an incremental walking protocol covering a broad range of speeds. Concurrent implementation of these two analytical approaches provided an opportunity for a more thorough exploration and reconciliation of findings ultimately landing on a more robust conclusion.
The potential influence of several anthropometric and biological factors on the relationship between cadence and intensity is debatable and likely shaped by sample characteristics. O’Brien et al. [19] reported an influence of height (i.e., for a 10-cm increase, the cadence threshold decreased by ~ 5 steps/min), but not leg length or BMI, on the cadence-intensity relationship assessed in young and middle-age adults. Abt et al. [22] reported that sex (a reasonable proxy indicator of stature) did not significantly affect the cadence-intensity relationship in a sample of 20 young adults. In samples of adults older than that studied herein, Serrano et al. [40] and O’Brien et al. [41] reported that body weight explained 13%, and BMI and METs together (variance of BMI alone was not reported) explained 77% of the observed variance, respectively, of the cadence-intensity relationship (moderate intensity was defined by ≥40%VO2 reserve and ≥ 40%METmax) and that height, leg length or stride length showed no influence. Herein, the inclusion of sex, leg length, or BMI did not improve the variance explained by the segmented regression models in each age group. While BMI significantly (and as expected) differed across decades in the present study (i.e., ± 2.5 kg/m2 difference between Group 1 and the rest of the age groups; P = 0.008), this difference did not influence the cadence-intensity relationship since the analyses were performed separately by age groups. Therefore, any potential influence of age-associated BMI differences was analytically mitigated by design. Again, it appears that any potential influence of anthropometric or biological factors is only readily apparent in broadly heterogeneous samples with respect to the characteristics under question.
Both the first [20] and second [21] reports from the CADENCE-Adults study supported ≥100 and ≥ 130 steps/min as heuristic cadence thresholds corresponding to absolutely-defined moderate and vigorous intensities (≥ 3.0 METs and ≥ 6.0 METs, respectively) in young and middle-age adults. In the present analyses, the cadence required to reach a relatively-defined moderate intensity, regardless of source indicator, was 10–20 steps/min higher than the previously published corresponding absolutely-defined value. Also, we identified thresholds up to 10 steps/min lower or 5 steps/min higher (depending on the age group) than the ≥130 steps/min corresponding to absolutely-defined vigorous intensity. The relatively-defined thresholds proposed herein do not invalidate the evidence substantiating ≥100 and ≥ 130 steps/min as a translation of absolutely-defined moderate and vigorous intensities [7, 20, 21]. The discrepancy in findings is due to an acknowledged difference in definitions and methods used to define intensity. For example, two individuals of the same age would both consume the same absolutely-defined and weight standardized amount of oxygen to practice slow ballroom dancing (e.g., 3 METs; 10.5 mL-1.kg-1.min-1) [34] even if they may have different maximal aerobic capacities (e.g., 45 ml/kg/min vs. 35 ml/kg/min). However, the two individuals performing this same ballroom dance would elicit different physiological responses and perceived experiences of effort in relative terms (i.e., 23% of maximal capacity vs. 30% of maximal capacity), based on their individual aerobic capacity. While absolutely-defined intensity is vitally important for communicating broadly scaled public health recommendations of PA, cadence thresholds associated with relatively-defined intensity are particularly useful when age-standardized information is known and can be applied (e.g., clinical and personal training-type settings), without having to administer a maximal test for aerobic capacity.
Among the limitations of the current study, a maximum aerobic capacity test that would allow for a more accurate accounting of individual physical fitness differences or measurement of HRmax was not included. Instead, relative intensity indicators were defined using an age-based prediction HR equation or perceived exertion. We acknowledge that age is a factor in the equations used to derive both %HRmax and %HRR; thus, by definition, as age increases, values for both %HRmax and %HRR will decrease. This age-associated phenomenon is well known and accepted [23,24,25]. To be clear, our intent was not to test age-related differences in these indicators; rather, we intended to use these accepted equations to calibrate heuristic cadence thresholds associated with moderate and vigorous intensity as defined by %HRmax and %HRR. Another limitation of the present analysis is that since the aerobic test used was submaximal, some pre-planned termination criteria (i.e., achievement of > 75% of age-predicted HRmax and ≥ 14 RPE) limited the number of data points used in the evaluation of vigorous activity. Thus, the lower PPV values for cadence-based vigorous intensity thresholds are explained by the limited number of TP bouts to inform vigorous intensity thresholds for some age groups [42]. If the prevalence of those who reach vigorous intensity is low, PPV will be low, even if both the sensitivity and specificity are high, as demonstrated in our results. However, as indicated earlier, a maximum aerobic capacity test is not always practical for non-research or diagnostic purposes, while submaximal tests are more feasible and accessible for assessing physiological response. Last, this was a laboratory-based treadmill study and, despite the intention to address an initial needed foundation of evidence, further investigations must confirm these findings under overground walking and/or free-living conditions.
Conclusion
This is the first study to propose age-stratified heuristic cadence thresholds (i.e., rounded, evidence-based values) for reaching relatively-defined moderate and vigorous intensity in adults 21–60 years of age. Cadences of ≥120, 120, 115, and 105 steps/min for moderate intensity and ≥ 135, 130, 125, and 120 steps/min for vigorous intensity are appropriate heuristic thresholds standardized for the age groups of 21–30 years, 31–40 years, 41–50 years and 51–60 years, respectively. The cadences reported herein are useful for guiding and analyzing intensity aligned with expected age-associated differences in physiological response to, and perceived experiences of, relatively-defined moderate and vigorous intensity.
Availability of data and materials
All data generated or analyzed during this study are included in this article and its additional files.
Change history
02 June 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12966-022-01295-z
Abbreviations
- ACSM:
-
American college of sports medicine
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HR:
-
Heart rate
- HRR:
-
Heart rate reserve
- HRmax :
-
Heart rate maximum
- METs:
-
Metabolic equivalents
- mph:
-
Miles per hour
- NPV:
-
Negative predictive value
- PI:
-
Prediction interval
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- RPE:
-
Rating of perceived exertion
- TN:
-
True negative
- TP:
-
True positive
- VO2 :
-
Oxygen consumption
References
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet (London, England). 2012;380(9838):219–29.
Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43(1):1–2.
2008 Physical Activity Guidelines Advisory Committee. 2018 physical activity guidelines advisory committee scientific report. Washington, DC: U.S. Department of Health and Human Services; 2018.
Ham SA, Kruger J, Tudor-Locke C. Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health. 2009;6:1–10.
Tudor-Locke C, Sisson SB, Collova T, Lee SM, Swan PD. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can J Appl Physiol. 2005;30(6):666–76.
Peake JM, Kerr G, Sullivan JP. A critical review of consumer Wearables, Mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front Physiol. 2018;9:743.
Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776–88.
Tudor-Locke C, Craig CL, Brown WJ, et al. How many steps/day are enough? for adults. Int J Behav Nutr Phys Activ. 2011;8:79.
Saint-Maurice PF, Troiano RP, Bassett DR Jr, et al. Association of Daily Step Count and Step Intensity with Mortality among US adults. Jama. 2020;323(12):1151–60.
Le Masurier GC, Sidman CL, Corbin CB. Accumulating 10,000 steps: does this meet current physical activity guidelines? Res Q Exerc Sport. 2003;74(4):389–94.
Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59.
Chen MJ, Fan X, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sports Sci. 2002;20(11):873–99.
Kujala UM, Pietilä J, Myllymäki T, et al. Physical activity: absolute intensity versus relative-to-fitness-level volumes. Med Sci Sports Exerc. 2017;49(3):474–81.
Gigerenzer G, Gaissmaier W. Heuristic decision making. Annu Rev Psychol. 2011;62:451–82.
Abel M, Hannon J, Mullineaux D, Beighle A. Determination of step rate thresholds corresponding to physical activity intensity classifications in adults. J Phys Act Health. 2011;8(1):45–51.
Beets MW, Agiovlasitis S, Fahs CA, Ranadive SM, Fernhall B. Adjusting step count recommendations for anthropometric variations in leg length. J Sci Med Sport. 2010;13(5):509–12.
Rowe DA, Welk GJ, Heil DP, et al. Stride rate recommendations for moderate intensity walking. Med Sci Sports Exerc. 2011;43(2):312–8.
Marshall SJ, Levy SS, Tudor-Locke CE, et al. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–5.
O'Brien MW, Kivell MJ, Wojcik WR, d'Entremont G, Kimmerly DS, Fowles JR. Step rate thresholds associated with moderate and vigorous physical activity in adults. Int J Environ Res Public Health. 2018;15(11)::2454.
Tudor-Locke C, Aguiar EJ, Han H, et al. Walking cadence (steps/min) and intensity in 21-40 year olds: CADENCE-adults. Int J Behav Nutr Phys Activ. 2019;16(1):8.
Tudor-Locke C, Ducharme SW, Aguiar EJ, et al. Walking cadence (steps/min) and intensity in 41 to 60-year-old adults: the CADENCE-adults study. Int J Behav Nutr Phys Activ. 2020;17(1):137.
Abt G, Bray J, Myers T, Benson AC. Walking cadence required to elicit criterion moderate-intensity physical activity is moderated by fitness status. J Sports Sci. 2019;37(17):1989–95.
American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 10th ed. Philadelphia, PA: Wolters Kluwer; 2018.
Georgiopoulou VV, Kalogeropoulos AP, Chowdhury R, et al. Exercise capacity, heart failure risk, and mortality in older adults: the health ABC study. Am J Prev Med. 2017;52(2):144–53.
Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33(6 Suppl):S446–51 discussion S52–3.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81.
Expert WHO. Committee on physical status: the use and interpretation of anthropometry. In: Physical status : the use and interpretation of anthropometry : report of a WHO Expert Committee. Geneva: world health Organization; 1995.
Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8(4):283–98.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–5.
Yin J, Tian L. Joint confidence region estimation for area under ROC curve and Youden index. Stat Med. 2014;33(6):985–1000.
Efron B. Estimating the error rate of a prediction rule: improvement on cross-validation. J Am Stat Assoc. 1983;78(382):316–31.
Diedrich FJ, Warren WH Jr. Why change gaits? Dynamics of the walk-run transition. J Exp Psychol Hum Percept Perform. 1995;21(1):183–202.
Hansen EA, Kristensen LAR, Nielsen AM, Voigt M, Madeleine P. The role of stride frequency for walk-to-run transition in humans. Sci Rep. 2017;7(1):2010.
Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
Moore CC, Aguiar EJ, Gould ZR, Amalbert-Birriel MA, Ducharme SW. Letter to the editor regarding the article "walking cadence required to elicit criterion moderate-intensity physical activity is moderated by fitness status" by Abt et al. (2019). J Sports Sci. 2020;38(3):304–5.
Consumer Technology Association Health and Fitness Technology Subcommittee. Physical activity monitoring for fitness Wearables: step counting. Arlington, VA: Consumer Technology Association; 2016.
de Man M, Vanderploeg E, Aimers N, Macmahon C, Wise L, Parrington L. Validity and inter-device reliability of dominant and non-dominant wrist worn activity trackers in suburban walking. Sensoria J Mind Brain Cult. 2016;12:40–46.
Thiebaud RS, Funk MD, Patton JC, et al. Validity of wrist-worn consumer products to measure heart rate and energy expenditure. Digit Health. 2018;4:2055207618770322.
Moore CC, McCullough AK, Aguiar EJ, Ducharme SW, Tudor-Locke C. Toward harmonized treadmill-based validation of step-counting wearable technologies: a scoping review. J Phys Act Health. 2020:1–13.
Serrano F, Slaght J, Senechal M, Duhamel T, Bouchard DR. Identification and prediction of the walking cadence required to reach moderate intensity using individually-determined relative moderate intensity in older adults. J Aging Phys Act. 2017;25(2):205–11.
O'Brien MW, Kivell MJ, Wojcik WR, D'Entremont GR, Kimmerly DS, Fowles JR. Influence of anthropometrics on step-rate thresholds for moderate and vigorous physical activity in older adults: scientific modeling study. JMIR Aging. 2018;1(2):e12363.
Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994;309(6947):102.
Acknowledgements
Not applicable.
Funding
The CADENCE-Adults study was supported by an award NIH NIA Grant 5R01AG049024. The funding agency had no role in the design of the study, the collection, analysis, or interpretation of data, or in the writing or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
CTL, JMS, TVB designed the study. CTL served as principal investigator. SWD, EJA, CCM, CJC, ZRG, and MAB collected the data. SWD and EJA coordinated data collection and management. SRC served as medical investigator in charge of all clinical aspects of data collection. CRM, CCM and JMG analyzed data with content expert input from CTL, JMS, and JS. All authors were involved in data presentation and interpretation and all actively engaged in collaboratively drafting and revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the University of Massachusetts Amherst Institutional Review Board (Protocol ID: 2015–2601). Informed consent was obtained from all participants prior to enrolment and data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no conflicts of interest. The results of the present study do not constitute endorsement by the American College of Sports Medicine. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Spreadsheet displaying final analytical dataset.
Additional file 2:
Spreadsheet displaying the data dictionary.
Additional file 3:
Figure displaying classification accuracy of heuristic cadence thresholds and relatively-defined moderate and vigorous intensity.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McAvoy, C.R., Moore, C.C., Aguiar, E.J. et al. Cadence (steps/min) and relative intensity in 21 to 60-year-olds: the CADENCE-adults study. Int J Behav Nutr Phys Act 18, 27 (2021). https://doi.org/10.1186/s12966-021-01096-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-021-01096-w