Abstract
Background
Health and fitness applications (apps) have gained popularity in interventions to improve diet, physical activity and sedentary behaviours but their efficacy is unclear. This systematic review examined the efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour in children and adults.
Methods
Systematic literature searches were conducted in five databases to identify papers published between 2006 and 2016. Studies were included if they used a smartphone app in an intervention to improve diet, physical activity and/or sedentary behaviour for prevention. Interventions could be stand-alone interventions using an app only, or multi-component interventions including an app as one of several intervention components. Outcomes measured were changes in the health behaviours and related health outcomes (i.e., fitness, body weight, blood pressure, glucose, cholesterol, quality of life). Study inclusion and methodological quality were independently assessed by two reviewers.
Results
Twenty-seven studies were included, most were randomised controlled trials (n = 19; 70%). Twenty-three studies targeted adults (17 showed significant health improvements) and four studies targeted children (two demonstrated significant health improvements). Twenty-one studies targeted physical activity (14 showed significant health improvements), 13 studies targeted diet (seven showed significant health improvements) and five studies targeted sedentary behaviour (two showed significant health improvements). More studies (n = 12; 63%) of those reporting significant effects detected between-group improvements in the health behaviour or related health outcomes, whilst fewer studies (n = 8; 42%) reported significant within-group improvements. A larger proportion of multi-component interventions (8 out of 13; 62%) showed significant between-group improvements compared to stand-alone app interventions (5 out of 14; 36%). Eleven studies reported app usage statistics, and three of them demonstrated that higher app usage was associated with improved health outcomes.
Conclusions
This review provided modest evidence that app-based interventions to improve diet, physical activity and sedentary behaviours can be effective. Multi-component interventions appear to be more effective than stand-alone app interventions, however, this remains to be confirmed in controlled trials. Future research is needed on the optimal number and combination of app features, behaviour change techniques, and level of participant contact needed to maximise user engagement and intervention efficacy.
Similar content being viewed by others
Background
The prevention of non-communicable diseases (NCDs) such as cardiovascular disease, cancer and type 2 diabetes is a major public health goal worldwide [1]. In 2012, NCDs were responsible for 38 million (68%) of the world’s 56 million deaths [1]. Lifestyle behaviours including diet, physical activity and sedentary behaviour are key modifiable risk factors for these diseases and improving these behaviours is considered essential to reducing the financial and health burden of these NCDs [1]. Unhealthy diet, physical inactivity and sedentary behaviour are known to track from childhood into adulthood and are difficult to change later in life [2, 3]. This exacerbates associated health problems and demonstrates why preventing the development of these health risk factors throughout the lifespan is important.
Given the global scale of NCDs, preventative interventions that can reach large populations at low cost are needed. Smartphones and tablets, including the software applications (apps) that run on these devices, have become an integral part of people’s life with large increases in usage rates since their introduction in 2007 [4, 5]. For example, 70% of Americans, 61% of Europeans and 74% of Australians regularly use a smartphone and/or tablet [5, 6]. The growth in mobile technologies has also stimulated the growth in health and fitness apps to provide behavioural interventions that can reach large populations [7]. Clever use of apps in health promotion and prevention of disease has enabled researchers to apply health behaviour changes techniques (e.g., goal setting, self-monitoring, performance feedback) that have proven to facilitate health behaviour change across diverse population groups and settings [7, 8].
Despite the increasing use of apps in health behaviour change studies their efficacy is unclear, particularly for different lifestyle behaviours such as diet, physical activity and sedentary behaviour, as well as for specific population groups including children and adults. Some systematic reviews [9–13] have addressed the potential of health apps to improve diet, physical activity and/or sedentary behaviour. However, the scope of these reviews has been broad and many questions remain. Firstly, most previous reviews [9–11, 14] were on electronic and mobile health (e-& mHealth) interventions, not specifically on app-based interventions. Secondly, many reviews [7, 8, 15–18] have focused on app design, the incorporation of established behaviour change techniques and they examined intervention feasibility rather than efficacy. Thirdly, many previous reviews [19–22] have focused on the use of apps for the treatment of obesity and chronic diseases. As such, little is known about the potential of using apps to change health behaviours for disease prevention. Finally, no reviews have distinguished between app interventions for children versus adults. This is important as app features appealing to children and adolescents may differ from those used by adults, and the choice of app features will likely determine user engagement, retention and ultimately intervention efficacy [22].
This review aimed to address these gaps in the literature by systematically synthesising evidence for the efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour for NCD prevention. Since app features used by children may differ from those used by adults, we distinguished between app interventions targeted to children and adults.
Methods
Literature search
This review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Additional file 1) [23]. Systematic searches were conducted between November and December 2015 in five databases: Scopus, CINAHL, SportDiscuss, PsycINFO and Web of Science. The search was limited to English language literature, humans, and the year of publication between 01 January 2006 and 31 October 2016. It was considered unlikely that app interventions were developed before 2006/2007 when smartphones were introduced. Systematic search strategies were designed using a combination of thesaurus and free terms covering the following terms: application, app, smartphone, smart phone, tablet, mobile game, game, physical activity, walk, physical fitness, leisure activity, motor activity, exercise, sport, sedentary, sedentary behaviour, sedentary behavior, sitting, screen time, inactive, diet, dietary, nutrition, nutritional, healthy eating, food, fruit, vegetable, snack, soft drink, carbonated beverage, intervention, program, programme, health promotion, prevention and trial. The detailed search strategies used for each database are presented in the Additional file 2. Additionally, articles were identified via hand-searching and reviewing reference lists of relevant papers.
Inclusion criteria and study selection
Studies were included in the present review if (1) they used an app in an intervention to influence at least one of the following lifestyle behaviours: dietary intake, physical activity, sedentary behaviour; (2) targeted children and/or adults; (3) focused on behaviour change for disease prevention (i.e., not specifically aiming to treat and manage health conditions such as obesity, hypertension and NCDs); and (4) reported data regarding efficacy for behaviour change (e.g., change in daily minutes of physical activity). In addition, studies could also report (but were not required) other relevant outcomes that may have conceivably been impacted by health behaviour change (i.e., fitness, body weight, blood pressure, glucose, cholesterol, quality of life). All types and units of measurements for the lifestyle behaviours and related health outcomes were acceptable (e.g., objective measure, self-report, minutes, steps, servings, calories, kilograms). The app intervention could be a stand-alone intervention using apps only, or a multi-component intervention where the use of an app was one of several intervention components (e.g., physical education, provision of physical activity equipment, parental education, face-to-face counselling). Studies were excluded from the review if: (1) non-experimental study designs were utilised (i.e., observational or case studies, studies reporting prevalence or trend data, feasibility studies, measurement studies, theoretical papers); and (2) the publication was not a peer-reviewed primary study (i.e., letters, commentaries, conference proceedings, reviews, narrative articles). Initially, titles and abstracts were screened for inclusion by a single reviewer (SS). As per best practice for systematic reviews [23], two reviewers (SA, WVL) independently reviewed the eligibility of studies for inclusion in the review, with disagreement resolved by discussion and consensus with a third reviewer (SS).
Data extraction
Data extraction was conducted using a standardised form developed specifically for this review (Table 1); similar to those used in other systematic reviews [12, 24, 25]. For all included studies, data were extracted for author, year, country, study design, intervention duration, measurement time points, attrition rate, sample, behaviour change theory, app features including behaviour change techniques, intervention components, outcomes, measures and main study results. The primary outcome measures extracted for main study results were dietary intake, physical activity and sedentary behaviour. Other relevant outcome measures closely related to these behaviours included weight status (body mass index, body weight, waist circumference), fitness, blood pressure, cholesterol, glucose and quality of life. To determine whether the interventions had a significant effect on behavioural and health outcomes, data on significance and magnitude of within- and between-group differences was extracted. For each included study, two reviewers independently extracted data (NAB and either SS, SA or WVL). Reviewers one and two agreed on the data extraction in over 70% of the studies. Disagreement was easily resolved by discussion and consensus with a third reviewer (either SS, SA or WVL).
Study quality assessment
The quality of the included studies was assessed using 25-point criteria adapted from the CONSORT checklists for the reporting of randomised controlled trials [26]. While the CONSORT checklist is intended for controlled trials, most criteria are applicable to other study designs and the weaker study designs justifiably received a lower score than studies using a controlled trial design. This approach has been used in other reviews [24]. Each criterion was rated as 1 (fulfilled), 0.5 (not all sub-items making up the criterion were fulfilled), 0 (not fulfilled or unclear), or not applicable (criterion was not applicable to the study design). Not applicable criteria were discounted from the ‘overall study quality score’ (sum of points). Hence, the highest attainable quality score was not 25 for all studies. Adapted from previous reviews [27, 28], the obtained study quality score for each study was divided by the highest attainable score and multiplied by 100 to give a percentage of fulfilled criteria; and studies were then grouped into high (>66.7%), fair (50–66.6%) or low (<50%) study quality (Additional file 3). The study quality assessment was conducted independently by two reviewers (SS, SA), with disagreement resolved by discussion and consensus with a third reviewer (WVL). Percent agreement between reviewers one and two for the scoring of the CONSORT criteria was 89%, with the most common points of discrepancy relating to recruitment methods, outcomes reporting and blinding procedures.
Results
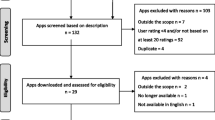
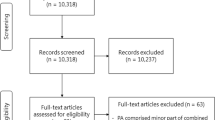
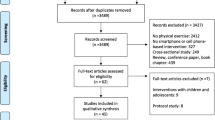
Study selection
A flowchart of the study selection process is presented in Fig. 1. A total of 6926 publications were identified from the database search. After removal of duplicates, 4945 publication titles and abstracts were screened, and 194 full-text articles were considered potentially eligible for inclusion. Of these, 30 articles reporting data on the efficacy of an app-based intervention to improve diet, physical activity and/or sedentary behaviour for prevention were included for final review. Some articles [29–34] reported on the same studies, and as such, a total of 30 articles describing 27 studies were included in this review.
Study characteristics
Characteristics of the app intervention studies included in this review are presented in Table 1.
Twelve studies were conducted in North America [35–46], seven studies in Australia/New Zealand [29–32, 47–51], seven studies in Europe [33, 34, 52–57], and one study in the Middle-East [58]. Most studies were randomised controlled trials (n = 19) with 2-group [29, 31, 35, 40, 43–46, 48, 50, 52–55, 58] or 3-group [33, 34, 42, 47, 56, 57] study designs. The remaining studies were controlled trials (n = 3) [33, 37, 49], randomised trials (n = 1) [39] or pre-post studies (n = 4) [36, 38, 41]. Twenty-three studies [31–36, 38, 39, 41–46, 48–58] targeted adults (mean age: 41.5 years, range: 18–71 years) and four studies [29, 37, 40, 47] targeted children or adolescents (mean age: 12.4 years, range: 8–17 years). The total number of participants across the 27 studies was 2699 (510 children/adolescents, 2189 adults). Samples sizes ranged from 17 to 502 (mean sample size: 100). The duration of interventions ranged from 1–24 weeks, with an average intervention duration of 10 weeks. Follow-up assessments were at 4 weeks (n = 5), 8 weeks (n = 8), 12 weeks (n = 9), 20 weeks (n = 2), 6 months (n = 2), 9 months (n = 1) and 18 months (n = 1). Attrition rates ranged from 0% [36] to 57% [51], with an average attrition rate of 17%. The majority of studies [31, 33, 35–45, 47, 48, 50, 53, 55–58] reported higher rates of female participation (on average 64% of participants were female). The targeted health behaviours were dietary intake (n = 13), physical activity (n = 21) and sedentary behaviour (n = 5). Other reported lifestyle-related health outcomes were: weight status (n = 11); fitness (n = 3); blood pressure (n = 4); blood glucose (n = 1); cholesterol (n = 1); and quality of life (n = 2). Ten studies [33, 36–38, 43–45, 49, 50, 55, 57] targeted a single health behaviour, whilst 17 studies [29, 31, 35, 39–42, 46–48, 50–56, 58] targeted multiple health behaviours and related health outcomes. Fourteen studies [33, 37–40, 42, 45–47, 51, 52, 55–57] involved interventions delivered solely via an app (stand-alone intervention) and 13 studies [29, 31, 35, 36, 41, 43, 44, 48–50, 53, 54, 58] involved interventions that used apps in conjunction with other intervention strategies (multi-component intervention), such as physical education, parental education, counselling sessions, printed materials, motivational emails, websites and pedometer use. Fifteen studies [29, 31, 36–39, 45, 46, 48–50, 52, 56–58] used a newly designed app in the intervention and 12 studies [33, 35, 40–44, 47, 51, 53–55] used a commercially available app. Further, 15 of the 27 studies reported intervention designs based on behaviour change theories, such as Self-determination Theory (n = 3) [29, 35, 37], Transtheoretical Model (n = 4) [31, 33, 41, 48], Social Cognitive Theory (n = 4) [29, 39, 44, 46], Theory of Planned Behaviour (n = 2) [45, 50], Control Systems Theory of Self-regulation (n = 1) [58], and the Behaviour Change Wheel (n = 1) [55].
Study quality
A detailed summary of quality assessments of included studies is presented in the Additional file 3. Overall, study quality ranged from high (n = 11) [29, 31, 43–45, 47, 48, 50, 53, 54, 58], to fair (n = 8) [35, 37, 46, 49, 55–57], and low (n = 8) [33, 36, 38, 39, 41, 42, 51, 52]. Study quality of interventions targeted to children/adolescents was high (n = 2) [29, 47] and fair (n = 2) [37, 40], and study quality of interventions targeted to adults ranged from high (n = 9) [31, 44, 45, 48, 50, 53, 54, 58], to fair (n = 6) [35, 46, 49, 55–57], and low (n = 8) [33, 36, 38, 39, 41, 42, 51, 52]. Most of the 13 interventions that used an app in combination with other intervention strategies were of high quality (n = 9) [29, 31, 43, 44, 48, 50, 53, 54, 58], whilst most of the 14 stand-alone app interventions were of fair (n = 6) [37, 40, 46, 55–57] or low quality (n = 6) [33, 38, 39, 42, 51, 52]. Study quality did not differ markedly between app interventions targeting multiple health behaviours and related health outcomes (high: n = 8, fair: n = 4, low: n = 5) and those targeting a single health behaviour (high: n = 3, fair: n = 4, low: n = 3). On average, the included studies fulfilled 61% of the assessment criteria (range: 34–92%). Most studies met the CONSORT requirements to provide a strong scientific rationale and described their participant eligibility, statistical methods and interventions clearly. Fewer studies reported sample size calculations [29, 31, 35, 43, 47, 50, 53–55, 57, 58] and included randomisation [29, 31, 35, 37, 39, 43–48, 50, 52–55, 58] and blinding procedures [31, 44–50, 53] in their study design. Attrition rates were reported or could be calculated for the majority of studies [29, 31, 33, 35–51, 53–58].
Intervention efficacy
A summary of intervention effects for the included lifestyle behaviour outcomes (diet, physical activity, sedentary behaviour) and related health outcomes (weight status, fitness, blood pressure, glucose, cholesterol, quality of life) are presented in Table 2. Overall, a slightly larger proportion of single health behaviour interventions (5 out of 10; 50%) [33, 45, 49, 55, 57] showed significant between-group improvements than multiple health behaviour interventions (7 out of 17; 41%) [29, 31, 48, 50, 53, 54, 58]. Further, a larger proportion of interventions that used an app in conjunction with other intervention strategies (8 out of 13; 62%) demonstrated significant between-group improvements in the behavioural and health outcomes [29, 31, 48–50, 53, 54, 58] compared to stand-alone app interventions (5 out of 14; 36%) [33, 40, 45, 55, 57].
Children and adolescents
Of the four studies that specifically targeted children and/or adolescents, one study [29] reported significant between-group improvements in diet, sedentary behaviour and fitness in the app intervention group. Another study [37] reported a significant within-group increase in physical activity, but no significant difference between groups. The remaining two studies [40, 47] reported no significant changes in the behavioural or related health outcomes.
Adults
Of the 23 studies that targeted adults, 17 studies reported significant improvements in diet (n = 6) [31, 38, 45, 54, 57, 58], physical activity (n = 13) [31, 33, 36, 37, 39, 41, 43, 48–50, 53–55, 58], sedentary behaviour (n = 1) [39], and other improved outcomes including weight status (n = 4) [31, 41, 42, 58], 49], fitness (n = 1) [56], blood pressure (n = 2) [41, 56] and cholesterol (n = 1) [41]. Of the studies reporting significant findings, 11 studies detected significant between-group differences in diet (n = 5) [31, 45, 54, 57, 58], physical activity (n = 9) [31, 33, 48–50, 53–55, 58] and weight status (n = 2) [31, 58] in favour of the app intervention group. Seven studies found significant within-group improvements in diet (n = 1) [38], physical activity (n = 4) [33, 36, 37, 39, 41, 43], sedentary behaviour (n = 1) [39] and weight status (n = 2) [41, 42, 56], blood pressure (n = 2) [41, 56] and cholesterol levels (n = 1) [41]. Five studies [35, 44, 46, 51, 52] reported no significant changes in the health outcomes of interest, and no significant findings were found in relation to the outcome glucose levels (assessed in one study).
Characteristics of efficacious interventions
App interventions showing significant between-group improvements in the behavioural and health outcomes tended to be multi-component interventions [31, 36, 41, 43, 48–50, 53, 54, 58], with sample sizes above 90 participants [35, 43, 44, 47–49, 53] and intervention durations longer than 8 weeks [37, 42–45, 47, 49]. A slightly larger proportion of single health behaviour [33, 45, 49, 55, 57] versus multiple health behaviour interventions [29, 31, 48, 50, 53, 54, 58] demonstrated between-group improvements (50% versus 41%, respectively). Further, most of the interventions [29, 31, 33, 39, 42, 45, 48–50, 53, 55, 56, 58] showing significant improvements in the behavioural and health outcomes included goal-setting, self-monitoring and performance feedback in the app design. Some efficacious interventions also incorporated other behaviour change techniques, such as motivational messages [29, 36, 57], health education/tailored advice [29, 31, 38, 48, 54, 57], reinforcement [33, 39, 40, 45], gamification in the form of exergames, award and rewards [37–40, 50], social support through interaction with peers [33, 37, 50] and friendly team challenges [29, 37, 39, 45]. There was not enough data to identify which behaviour change techniques determined intervention efficacy. Moreover, there was no difference in the behaviour change techniques incorporated in apps for children compared to those used in apps for adults. Eleven studies [31, 38, 40, 43, 45, 48–50, 54, 56–58] out of the 19 studies showing significant improvements in behavioural and health outcomes reported usage statistics to determine participants’ engagement with the app. Three of these studies [38, 43, 49] examined associations between app usage and changes in the behavioural and health outcomes. Their findings showed that higher app usage was associated with improvements in physical activity and healthy eating [38, 43, 49].
Discussion
This systematic review found modest evidence for the efficacy of app interventions to improve diet, physical activity and sedentary behaviours for NCD prevention. Overall, 19 out of the 27 identified studies reported significant improvements in behavioural and related health outcomes. Most of these studies reported significant between-group improvements in the app intervention group versus comparison group, which is considered the gold standard to demonstrate intervention efficacy [59]. Notwithstanding study limitations, the findings from this review indicate that apps can be an effective tool to improve health behaviours. The advantages of smartphone apps over other intervention delivery modes such as websites, face-to-face counselling and group sessions may partially explain the efficacy of app interventions. Given that many people have busy lifestyles, they value convenient access to health behaviour change programs that provide information and advice, real-time self-monitoring, feedback, reinforcement, social support, and rewards ‘on the go’ [60]. The appeal of smartphones for assistance in health promotion concurs with the trend that more people are seeking health information via mobile devices [61, 62]. In this context, apps provide the opportunity to bring behavioural interventions into real life situations where people make decisions about their health.
Despite the potential of apps, half of the interventions identified in this review used apps in conjunction with other intervention strategies. The remaining interventions were stand-alone interventions where the app was the sole intervention component. Importantly, however, is the observation that most of the multi-component interventions demonstrated significant between-group improvements in behavioural and health outcomes, whereas fewer stand-alone app interventions reported significant between-group improvements. This raises the question whether multi-component interventions yield stronger intervention effects than stand-alone app interventions. Many reviews of health behaviour change interventions [63–67] recommend the use of multiple intervention strategies to achieve long-term health behaviour change. Reviews of website-delivered interventions [9, 28, 68] have also shown stronger behaviour change effects when combined with other intervention strategies such as SMS, telephone coaching and motivational emails. As such, it is likely that the integration of apps in multi-component interventions produces stronger health outcomes compared to stand-alone app interventions; however, this remains to be tested in future trials.
The majority of app interventions were targeted to adults; only four out of the 27 identified app interventions were specifically aimed at children or adolescents. This is consistent with previous e & mHealth reviews [11, 12, 25, 69] showing that internet and mobile phone delivered interventions have mainly targeted adult populations. Although smartphones and tablets have become an integral part of children’s lives [70], surprisingly few interventions have yet utilised app technology in pediatric health behaviour change programs [12]. However, as exergame and serious game apps are becoming increasingly popular among children and adolescents [71], it is likely that more app studies focussing on children will be conducted in the near future.
The average attrition rate (i.e., participant loss to follow-up) reported in the app interventions was 17%, which is lower compared average attrition rates of 23–27% found in web-based interventions [28, 68, 72]. Lower participant attrition indicates less bias in the estimated intervention effects [73]. However, participant attrition does not capture participants’ engagement with the app intervention which also determines intervention effects. For example, web- and app-based interventions that have examined participant engagement found that higher levels of website and app usage were associated with increased intervention efficacy [38, 43, 68]. Despite this, less than half of the studies reported usage statistics to determine participants’ engagement with the app. This is consistent with previous reviews [24, 28, 68] reporting that few internet and mobile interventions recorded participants’ engagement with the intervention technologies. Given the relative ease by which app usage statistics can be tracked, it is unfortunate that this data is not being collected and published for all studies in this area. We know that participant engagement, measured by number of website logins, usually declines after the first few weeks in website and social media interventions [24, 28, 68]. An example is the Australian 10,000 Steps program, a successful, freely available web- and app-based intervention to promote physical activity [61]. Participants’ engagement with the 10,000 Steps website and app lasts on average 5–6 weeks, with longer usage duration (on average 8 weeks) being observed in people who use both the 10,000 Steps website and app [61]. This rapid decline in usage concurs with qualitative research showing that people often lack commitment to using any particular app and they tend to engage in only transient, casual app use [60]. Since participant engagement determines intervention exposure, and level of intervention exposure determines intervention efficacy [28, 61, 74], better understanding of factors that improve participant engagement and retention is needed.
To increase user engagement with health behaviour change apps, more information is needed about what app features and behaviour change techniques people value and use. Recent focus group data showed that [60, 75] that young people value health behaviour apps that require low effort, are pleasant to use, are developed by credential experts, enable self-monitoring, provide advice on how to change behaviour, include positively framed alerts/reminders (but not too frequent), provide accurate tracking functions, incorporate adequate privacy settings, and clearly show what the app will do (no surprises). Some of these user preferences were part of the efficacious apps identified in this review. For example, most apps included goal-setting, self-monitoring and performance feedback [29, 31, 33, 39, 42, 45, 48–50, 53, 55, 56, 58]. Additionally, some apps incorporated tailored advice, motivational prompts and reinforcement, gamification, social support or friendly team challenges [29, 33, 37–40, 45, 48, 50, 54, 57]. Reviews of web-based interventions have demonstrated that interventions including more behaviour change techniques are more effective [74, 76]. This may also apply to app-based interventions. However, it remains unclear what the optimal number and combination of app features and behaviour change techniques is to increase user retention and ultimately intervention efficacy. It is also possible that efficacy declines when too many features or techniques are implemented. Furthermore, socio-demographic factors (e.g., sex, age, education) and psychosocial factors (e.g., attitudes, perceived benefits, enjoyment) may also influence app usage [60]. Emerging research on the adoption of app technology showed that higher app usage is associated with being female and of younger age [61, 77], as well as with personal interest in new technologies, positive attitudes towards smartphone apps and perceived benefit of use [77]. Therefore, targeting and tailoring smartphones apps to specific population groups may also enhance the efficacy of app-based interventions.
Strengths and limitations
Strengths of this systematic review are that it was conducted and reported according to PRISMA guidelines [23], and study quality was systematically assessed using the CONSORT checklist [26]. The search strategy was comprehensive, and study selection, data extraction, and quality rating were completed by two independent reviewers, as is standard practice for high quality systematic review [23]. These procedures ensure accuracy of the reviewed data. The scope of this review was limited to app interventions improving behavioural and related health outcomes for prevention; hence app interventions relating to chronic disease treatment were not captured in this review. Few app interventions identified in this review focused on dietary and sedentary behaviours which makes it more difficult to draw conclusions on the efficacy of app interventions targeting these behaviours, as opposed to those targeting physical activity behaviour. Furthermore, the included studies varied widely in terms of methodological quality, with some studies scoring very poorly, thereby reducing the trust that can be placed in their findings. Finally, the possibility of publication bias should also be acknowledged. As with all systematic reviews examining the efficacy of interventions, it is possible that some studies with null findings have not been published [78].
Recommendations for future research
Based on this review, it is recommended that future studies:
-
Test the efficacy of specific app features and behaviour change techniques in high quality controlled trials to distinguish effective from ineffective intervention components.
-
Directly compare the efficacy of stand-alone app intervention compared to multi-component interventions that use apps in combination with other intervention strategies.
-
Compare the efficacy of app interventions to other intervention delivery modes, such as website, print-based and face-to-face interventions.
-
Utilise larger sample sizes to ensure they are sufficiently powered to detect significant intervention effects.
-
Tailor app interventions to specific population groups (e.g., women, young people) in whom usage and adoption of app technology is high.
-
Report app usage statistics using objective and self-report measures to examine levels of and reasons for participant (dis)engagement and intervention exposure.
-
Explore the optimal duration and intensity of app interventions to ensure user engagement and retention as the intervention progresses.
-
Identify factors that increase user engagement and retention in app interventions to sustain behavioural health improvments in the long-term.
-
Investigate the relationship between user engagement and intervention efficacy, whilst taking into account socio-demographic and psychosocial factors.
Conclusions
Interventions using apps to improve diet, physical activity and sedentary behaviour for prevention show promise for effective behaviour change in children and adults. The evidence base is largest for the use of apps to increase physical activity in adults. Fewer interventions have used apps to improve dietary and sedentary behaviours, and very few app interventions have targeted children and adolescents. Multi-component interventions that combine apps with other intervention strategies appear to be more effective than stand-alone app interventions, however, this remains to be tested further in controlled trials. Overall, there is still considerable scope to improve the efficacy of app-based interventions. In particular, intervention studies should gather more app usage statistics to identify factors that improve user engagement and retention, and its relationship with intervention efficacy. In addition, more formative research is needed to determine the optimal number and combination of app features, behaviour change techniques, and level of participant contact needed to maximise user engagement and ultimately intervention efficacy.
Abbreviations
- Apps:
-
Applications
- CONSORT:
-
Consolidated standards of reporting trials
- NCDs:
-
Non-communicable diseases
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
References
World Health Organization. Global status report on noncommunicable diseases. World Health Organization. 2014. http://www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed 5 Jul 2016.
Biddle SJ, Pearson N, Ross GM, Braithwaite R. Tracking of sedentary behaviours of young people: a systematic review. Prev Med. 2010;51:345–51.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–84.
Statistica. Number of smartphone users worldwide from 2014 to 2019. Statistica. 2016. http://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed 5 Jul 2016.
Australian Communications and Media Authority. Communications report 2014–15. Australian communications and media authority. 2015. http://www.acma.gov.au/theACMA/Library/Corporate-library/Corporate-publications/communications-report-2014-15. Accessed 5 July 2016.
Group Special Mobile Association. The mobile economy. Group special mobile association. 2015. http://www.gsmamobileeconomy.com/GSMA_Global_Mobile_Economy_Report_2015.pdf. Accessed 5 July 2016.
Middelweerd A, Mollee JS, van der Wal CN, Brug J, te Velde SJ. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys Act. 2014;11:97.
Direito A, Pfaeffli Dale L, Shields E, Dobson R, Whittaker R, Maddison R. Do physical activity and dietary smartphone applications incorporate evidence-based behaviour change techniques? BMC Public Health. 2014;14:646.
Hutchesson MJ, Rollo ME, Callister R, Collins CE. Self-monitoring of dietary intake by young women: Online food records completed on computer or smartphone are as accurate as paper-based food records but more acceptable. J Acad Nutr Diet. 2015;115:87–94.
Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012;14:61–71.
Monroe CM, Thompson DL, Bassett DR, Fitzhugh EC, Raynor HA. Usability of mobile phones in physical activity–related research: a systematic review. Am J Health Educ. 2015;46:196–206.
Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014;44:671–86.
Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? An evidence review. J Med Internet Res. 2016;18:e287.
Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011;13:e48.
Schoffman DE, Turner-McGrievy G, Jones SJ, Wilcox S. Mobile apps for pediatric obesity prevention and treatment, healthy eating, and physical activity promotion: Just fun and games? Transl Behav Med. 2016;3:320–5.
Conroy DE, Yang CH, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med. 2014;46:649–52.
Sharp DB, Allman-Farinelli M. Feasibility and validity of mobile phones to assess dietary intake. Nutr. 2014;30:1257–66.
Payne HE, Lister C, West JH, Bernhardt JM. Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR Mhealth Uhealth. 2015;3:e20.
Wang J, Wang Y, Wei C, Yao NA, Yuan A, Shan Y, et al. Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health. 2014;20:570–83.
Woo J, Chen J, Ghanavati V, Lam R, Mundy N, Li LC. Effectiveness of cellular phone-based interventions for weight loss in overweight and obese adults: a systematic review. Orthop Muscul Syst. 2013;3:141.
Okorodudu DE, Bosworth HB, Corsino L. Innovative interventions to promote behavioral change in overweight or obese individuals: a review of the literature. Ann Med. 2015;47:179–85.
Bardus M, van Beurden SB, Smith JR, Abraham C. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int J Behav Nutr Phys Act. 2016;13:35.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review JMIR. 2014;16:e40.
Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28:320–9.
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Deveraux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869.
Schoeppe S, Duncan MJ, Badland H, Oliver M, Curtis C. Associations of children’s independent mobility and active travel with physical activity, sedentary behaviour and weight status: a systematic review. JSAMS. 2013;16:312–9.
Davies C, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Behav Nutr Physl Act. 2012;9:52.
Smith JJ, Morgan PJ, Plotnikoff RC, Dally KA, Salmon J, et al. Smart-phone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT. Pediatrics. 2014;134:e723–31.
Lubans DR, Smith JJ, Plotnikoff RC, Dally KA, Okely AD, Salmon J, et al. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: the ATLAS cluster randomized controlled trial. Int J Behav NutrPhys Act. 2016;13:92.
Partridge SR, McGeechan K, Hebden L, Balestracci K, Wong ATY, Denney-Wilson E, et al. Effectiveness of a mHealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: randomized controlled trial. JMIR Mhealth Uhealth. 2015;3:e66.
Allman-Farinelli M, Partridge SR, McGeechan K, Balestracci K, Hebden L, Wong A, et al. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): Nine-month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth. 2016;4:e78.
Silveira P, van de Langenberg R, van het Reve E, Daniel F, Casati F, de Bruin ED. Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: a phase II preclinical exploratory trial. JMIR. 2013;15:114–30.
van het Reve E, Silveira P, Daniel F, Casati F, de Bruin ED. Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: part 2 of a phase II preclinical exploratory trial. JMIR. 2014;16:99–116.
Cowdery J, Majeske P, Frank R, Brown D. Exergame apps and physical activity: the results of the ZOMBIE trial. Am J Health Educ. 2015;46:216–22.
Fukuoka Y, Vittinghoff E, Jong SS, Haskell W. Innovation to motivation: Pilot study of a mobile phone intervention to increase physical activity among sedentary women. Prev Med. 2010;51:287–9.
Garde A, Umedaly A, Abulnaga SM, Robertson L, Junker A, Chanoine JP, et al. Assessment of a mobile game (‘MobileKids Monster Manor’) to promote physical activity among children. Games Health. 2015;4:145–8.
Gilliland J, Sadler R, Clark A, O'Connor C, Milczarek M, Doherty S. Using a smartphone application to promote healthy dietary behaviours and local food consumption. Biomed Res Int. 2015. doi:10.1155/2015/841368.
King AC, Hekler EB, Grieco LA, Winter SJ, Sheats JL, Buman MP, et al. Harnessing different motivational frames via mobile phones to promote daily physical activity and reduce sedentary behavior in aging adults. Plos One. 2013;8:e62613.
Nollen NL, Mayo MS, Carlson SE, Rapoff MA, Goggin KJ, Ellerbeck EF. Mobile technology for obesity prevention: a randomized pilot study in racial- and ethnic-minority girls. Am J Prev Med. 2014;46:404–8.
Stuckey M, Russell-Minda E, Read E, Munoz C, Shoemaker K, Kleinstiver P, et al. Diabetes and technology for increased activity (DaTA) study: results of a remote monitoring intervention for prevention of metabolic syndrome. J Diabetes Sci Technol. 2011;5:928–35.
Wharton CM, Johnston CS, Cunningham BK, Sterner D. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial. J Nutr Educ Behav. 2014;46:440–4.
Wang JB, Cadmus-Bertram LA, Natarajan L, White MM, Madanat H, Nichols JF, et al. Wearable sensor/device (Fitbit One) and SMS text-messaging prompts to increase physical activity in overweight and obese adults: a randomized controlled trial. Telemed J E Health. 2015;21:782–92.
Choi JW, Lee J, Vittinghoff E, Fukuoka Y. mHealth physical activity intervention: a randomized pilot study in physically inactive pregnant women. Matern Child Health. 2016;20:1091–101.
Mummah SA, Mathur M, King AC, Gardner CD, Sutton S. Mobile technology for vegetable consumption: a randomized controlled pilot study in overweight adults. JMIR Mhealth Uhealth. 2016;4:e51.
Rabbi M, Pfammatter A, Zhang M, Spring B, Choudhury T. Automated personalized feedback for physical activity and dietary behavior change with mobile phones: a randomized controlled trial on adults. JMIR Mhealth Uhealth. 2015;3:e42.
Direito A, Jiang Y, Whittaker R, Maddison R. Apps for IMproving FITness and increasing physical activity among young people: the AIMFIT pragmatic randomized controlled trial. JMIR. 2015;17:e210.
Hebden L, Cook A, van der Ploeg HP, King L, Bauman A, Allman-Farinelli M. A mobile health intervention for weight management among young adults: a pilot randomised controlled trial. J Hum Nutr Diet. 2014;27:322–32.
Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Using smartphone technology to monitor physical activity in the 10,000 Steps program: a matched case-control trial. JMIR. 2012;14:e55.
Maher C, Ferguson M, Vandelanotte C, Plotnikoff R, De Bourdeaudhuij I, Thomas S, et al. A web-based, social networking physical activity intervention for insufficiently active adults delivered via facebook app: randomised controlled trial. JMIR. 2015;17:e174.
Gilson ND, Pavey TG, Vandelanotte C, Duncan MJ, Gomersall SR, Trost SG, et al. Chronic disease risks and use of a smartphone application during a physical activity and dietary intervention in Australian truck drivers. Aust N Z J Public Health. 2016;40:91–3.
Gasser R, Brodbeck D, Degen M, Luthiger J, Wyss R, Reichlinal S. Persuasiveness of a mobile lifestyle coaching application using social facilitation. Pers Technol. 2006;3962:27–38.
Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, Newell J, et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. Br J Gen Pract. 2014;64:e384–91.
van Drongelen A, Boot CRL, Hlobil H, Twisk JWR, Smid T, van der Beek AJ. Evaluation of an mHealth intervention aiming to improve health-related behavior and sleep and reduce fatigue among airline pilots. Scand J Work Environ Health. 2014;40:557–68.
Walsh JC, Corbett T, Hogan M, Duggan J, McNamara A. An mHealth intervention using a smartphone app to increase walking behavior in young adults: a pilot study. JMIR Mhealth Uhealth. 2016;4:e109.
Rospo G, Valsecchi V, Bonomi AG, Thomassen IWG, van Dantzig S, La Torre A, et al. Cardiorespiratory improvements achieved by American College of sports medicine’s exercise prescription implemented on a mobile app. JMIR Mhealth Uhealth. 2016;4:e77.
Elbert SP, Dijkstra A, Oenema A. A mobile phone app intervention targeting fruit and vegetable consumption: the efficacy of textual and auditory tailored health information tested in a randomized controlled trial. J Med Internet Res. 2016;18:e147.
Safran Naimark J, Madar Z, Shahar DR. The impact of a web-based app (eBalance) in promoting healthy lifestyles: randomised controlled trial. JMIR. 2015;17:e56.
Flecha OD, de Oliveira DWD, Marques LS, Gonçalves PF. A commentary on randomized clinical trials: How to produce them with a good level of evidence. Perspect Clin Res. 2016;7:75–80.
Dennison L, Morrison L, Conway G, Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. JMIR. 2013;15:e86.
Guertler D, Vandelanotte C, Kirwan M, Duncan MJ. Engagement and nonusage attrition with a free physical activity promotion program: the case of 10,000 steps Australia. JMIR. 2015;17:e176.
Nikoloudakis IA, Vandelanotte C, Rebar AL, Schoeppe S, Alley S, Duncan MJ, et al. Examining the correlates of online health information-seeking behavior among men compared with women. Am J Mens Health. 2016; 2016. doi:10.1177/1557988316650625.
De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert JM, Rostami C, Brug J, et al. School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Obes Rev. 2011;12:205–16.
Kriemler S, Meyer U, Martin E, Van Sluijs EMF, Andersen LB, Martin BW. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med. 2011;45:923–30.
Rodrigues AL, Ball J, Ski C, Stewart S, Carrington MJ. A systematic review and meta-analysis of primary prevention programmes to improve cardio-metabolic risk in non-urban communities. Prev Med. 2016;87:22–34.
Appleton KM, Hemingway A, Saulais L, Dinnella C, Monteleone E, Depezay L, et al. Increasing vegetable intakes: rationale and systematic review of published interventions. Eur J Nutr. 2016;2016(55):869–96.
Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions. A review of the literature. Am J Prev Med. 2007;33:54–64.
O'Reilly GA, Spruijt-Metz D. Current mHealth technologies for physical activity assessment and promotion. Am J Prev Med. 2013;45:501–7.
Pew Research Center. Teens, social media & technology overview 2015: smartphones facilitate shifts in communication landscape for teens. Pew Research Center. 2015. http://www.pewinternet.org/files/2015/04/PI_TeensandTech_Update2015_0409151.pdf. Accessed 5 Jul 2016.
Boulos MNK, Yang SP. Exergames for health and fitness: the roles of GPS and geosocial apps. Int J Health Geogr. 2013;12:18.
Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev. 2010;11:306–21.
Dumville JC, Torgerson DJ, Hewitt CE. Reporting attrition in randomised controlled trials. BMJ. 2006;332:969–71.
van Genugten L, Dusseldorp E, Webb T, van Empelen P. Which combinations of techniques and modes of delivery in internet-based interventions effectively change health behavior? A meta-analysis. JMIR. 2016;18:e155.
Middelweerd A, van der Laan DM, van Stralen MM, Mollee JS, Stuij M, te Velde SJ, et al. What features do Dutch university students prefer in a smartphone application for promotion of physical activity? A qualitative approach. Int J Behav Nutr Phys Act. 2015;12:31.
Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. JMIR. 2010;12:e4.
Sandholzer M, Deutsch T, Frese T, Winter A. Predictors of students’ self-reported adoption of a smartphone application for medical education in general practice. BMC Med Educ. 2015;15:91.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Acknowledgements
SS is supported by an Early Career Fellowship (GNT1125586) from the Australian National Health and Medical Research Council. CV (ID 100427) and MJD (ID 100029) are supported by Future Leader Fellowships from the National Heart Foundation of Australia.
Funding
SS is supported by an Early Career Fellowship (GNT1125586) from the Australian National Health and Medical Research Council. CV (ID 100427) and MJD (ID 100029) are supported by Future Leader Fellowships from the National Heart Foundation of Australia.
Availability of data and materials
Not applicable.
Authors’ contributions
SS, SA, WVL and CV conceptualised and designed the study. SS, SA, WVL and NAB conducted the search, article selection, data extraction and quality assessment. SS drafted and wrote the manuscript. SA, WVL, CV, MJD, SLW, and NAB were involved in interpretation of data and critically revising the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Completed PRISMA checklist. (DOCX 77 kb)
Additional file 2:
Search strategy used in the databases. (DOCX 32 kb)
Additional file 3:
Quality assessment for all included studies. (DOCX 20 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Schoeppe, S., Alley, S., Van Lippevelde, W. et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act 13, 127 (2016). https://doi.org/10.1186/s12966-016-0454-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-016-0454-y