Abstract
Elraglusib (formerly 9-ING-41) is an ATP-competitive inhibitor of glycogen synthase kinase-3β (GSK3β) undergoing clinical trials for the treatment of various cancers including non-Hodgkin lymphoma (NHL). The drug reduces proliferation of several NHL cell lines and has efficacy in xenograft models of the disease. To confirm the importance of its action on GSK3β, we treated 3 lymphoma cell lines with selective, structurally distinct GSK3 inhibitors: CT99021, SB216763, LY2090314, tideglusib, and elraglusib. Stabilization of β-catenin and reduced phosphorylation of CRMP2, two validated targets of GSK3, were used as functional read-outs for GSK3 inhibition. CT99021, SB216763, and LY2090314 failed to reduce proliferation or viability in any cell line at concentrations that stabilized β-catenin and reduced CRMP2 phosphorylation. There was partial reduction of CRMP2 phosphorylation but no significant effect on β-catenin at cytotoxic doses of elraglusib. There was no indication of GSK3 inhibition at doses of tideglusib that affected cell viability and apoptosis. Cell-free kinase screening confirmed several other targets of elraglusib, distinct from the GSK3 inhibitors with no anti-lymphoma actions, including PIM kinases and MST2. These data question GSK3 as the target of elraglusib in lymphoma, and hence the utility of GSK3 expression as a ‘stand-alone’, therapeutic biomarker in NHL.
Video Abstract
Similar content being viewed by others
Main text
Introduction
Despite improvements in outcomes, high-grade B- and T-cell non-Hodgkin lymphoma (NHL) represent a significant area of unmet therapeutic need, particularly in the context of relapsed or refractory disease [1, 2].
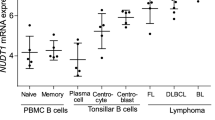
Glycogen synthase kinase 3 (GSK3) is a ubiquitously expressed, serine/threonine kinase involved in diverse cellular functions [3,4,5]. Two paralogs, GSK3α and GSK3β, are expressed from independent genes [6]. GSK3 dysregulation is found in numerous cancers and higher GSK3 expression correlates with poorer survival in NHL [7, 8]. Several GSK3 inhibitors are commercially available and in vitro cytotoxicity has been observed in chronic lymphocytic leukemia (CLL), acute myeloid leukemia (AML), and chemotherapy-resistant NHL [9,10,11].
A recently developed GSK3 inhibitor, elraglusib (formerly 9-ING-41), is particularly noteworthy for its anti-lymphoma effects in both B- and T-cell NHL lines and immunocompromised mouse patient-derived lymphoma xenograft models [8, 12].
Elraglusib has now progressed to early-phase clinical trials for several malignant conditions, including lymphoma, with clinical efficacy reported in case studies of refractory adult T-cell leukemia/lymphoma [13, 14]. The therapeutic rationale for GSK3 inhibition in lymphoma is largely based on these early elraglusib data together with GSK3 gene knock-out models and differences in GSK3 expression between lymphoma tissue and normal lymphocytes [8, 12]. Therefore there are limited data to indicate that cytotoxicity in lymphoma can be achieved solely through the targeted pharmacological inhibition of GSK3. To clarify that the cytotoxicity observed with elraglusib is a consequence of GSK3 inhibition we investigated a panel of structurally diverse GSK3 inhibitors, including elraglusib, in both B- and T-cell NHL cell lines and assessed their effects on cell viability, apoptosis, and cellular GSK3 inhibition [4].
Methods
Compounds
Doxorubicin, SB216763, elraglusib (9-ING-41) and tideglusib were purchased from Cambridge Bioscience, LY2090314 from Stratech, CT99021 was synthesized as previously described [15]. All compounds were dissolved in DMSO (dimethyl sulfoxide).
Cell culture
HS-Sultan cells were gifted from Dr Banerjee, University of Dundee. Karpas-299 cells were purchased from Public Health England and HH cells from American Type Culture Collection. Cells were grown in RPMI-1640 media containing glycine, 10% fetal bovine serum supplemented with 100 units/ml penicillin, 100 µg/ml streptomycin (all Gibco).
To measure changes in protein expression, cells in the exponential phase of growth were cultured in serum-free media overnight, prior to 4 h of drug treatment. For PARP (Poly [ADP-ribose] polymerase) cleavage assays, cells were cultured in serum-containing media for 24 h prior to protein extraction [16].
Immunoblotting
Expression of β-catenin and phosphorylation of collapsin response-mediator protein 2 (CRMP2) were used as functional read-outs of GSK3 inhibition and PARP cleavage for apoptosis, all measured by immunoblotting. Rabbit anti-PARP (9542), rabbit anti-CRMP2 (9393) and rabbit anti-β-catenin (9562) were from Cell Signaling. Mouse anti-actin (A3853) was from Sigma-Aldrich. Sheep anti-phospho-CRMP2 (Thr509/514) was made in-house as described previously [17].
Anti-rabbit (Licor Goat anti-Rabbit (926–32211)) and anti-mouse (Thermofisher Invitrogen Goat anti-Mouse (A21057)) secondary antibodies were used at 1:10,000. Rabbit anti-sheep HRP (horseradish peroxidase) secondary (ThermoFisher 31480) was used at 1:2500. All antibodies were diluted in 1% BSA in TBS-T. Cell lysates were prepared for SDS-PAGE (sodium dodecyl sulfate–polyacrylamide gel electrophoresis) as previously described [18], and protein quantified by Bradford (BioRad). Blot analysis was on either the LICOR-Odyssey Scanner (β-catenin and β-actin) or on film using ECL (enhanced chemiluminescence) (Phospho-CRMP2), then ImageStudio Lite 5.2 and Graphpad Prism, with one-way ANOVA and p = < 0.05 for statistical significance.
Cell viability
This was assessed using CellTiter 96® Aqueous One Solution Cell Proliferation Assay Kit (Promega) according to manufacturer’s instructions. In brief, 8000 cells/well were seeded into 96-well plates. Compounds were incubated with cells for 72 h prior to the addition of MTS (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) reagent for 2 h followed by absorbance assessment at 450 nM by Modulus Microplate reader. Analysis was performed using Graphpad Prism 9.
Kinase assays
33P cell-free screens were performed by the MRC Protein Phosphorylation Unit, University of Dundee as previously described [19].
Results and discussion
Elraglusib (1-5 µM) reduced cell viability and induced apoptosis in both B- and T-cell NHL cell lines in keeping with its reported anti-lymphoma properties (Fig. 1). If the inhibition of GSK3 alone was sufficient to explain this property of elraglusib then we would expect structurally unrelated, selective inhibitors of GSK3 to have similar anti-lymphoma actions. We, therefore, investigated the effects of the GSK3 inhibitors, tideglusib, CT99021, SB216763 and LY2090314.
Effect of various GSK3 inhibitors on lymphoma cell viability and PARP cleavage: HS-Sultan (A,D), Karpas-299 (B,E), and HH (C,F) cells were exposed to a panel of small molecule GSK3 inhibitors. Doxorubicin, an anthracycline chemotherapeutic, was used as a positive control. Cell viability assessments were performed using the MTS assay following a 72-h exposure to the compounds. PARP cleavage assays (marker of apoptosis) were performed on lysates generated after 24 h exposure to compounds. Quantification of PARP blots from 3 separate experiments is provided for HS-Sultan (G), Karpas-299 (H), and HH (I) cells
Tideglusib (5-10 µM) produced a weak reduction in cell viability and only induced apoptosis in one of three cell lines, while none of the other GSK3 inhibitors reduced cell viability or induced apoptosis at concentrations previously reported to result in GSK3 inhibition (Fig. 1).
CRMP2 and β-catenin are validated targets for GSK3, with β-catenin phosphorylation promoting degradation of the protein [4, 20, 21]. CT99021, SB216763 and LY2090314 all significantly stabilized β-catenin protein and reduced CRMP2 phosphorylation in every cell line at concentrations that did not alter cell viability within 4 h (Fig. 2A-C). The relative strength of these effects was consistent with reported in vitro GSK3 inhibitory potency (LY > CT > SB, Fig. 2D). Neither elraglusib nor tideglusib increased β-catenin levels in any cell line (even at 5-10 µM), although elraglusib did partly reduce the phosphorylation of CRMP2 at 5 µM in one line (Fig. 2A-C). The effects of CT99021 and LY2090314 on β-catenin were sustained for 24 h (data not shown), while the action of SB216763 declined by 24 h. Longer incubations up to 24 h with elraglusib or tideglusib did not result in any significant actions on β-catenin stability (data not shown). We confirmed the in vitro IC50 of our batch of elraglusib against GSK3 (0.37 µM, Fig. 2E). Therefore, the lack of correlation between the regulation of cellular GSK3 substrates and altered cell viability or apoptosis implies that a GSK3-independent action of elraglusib is responsible for its anti-lymphoma actions.
Analysis of GSK3 substrate regulation in lymphoma cells: HS-Sultan (A), Karpas-299 (B), and HH (C) cells were exposed to the compounds for 4 h prior to cell lysis and western blotting for the GSK3 substrates β-catenin and phospho-CRMP2, using b-actin and total CRMP2 as loading controls. D IC50 determination (0.37 µM) in an in vitro GSK3β assay. E Comparison of reported IC50 measures for the GSK3 inhibitors used in this study. F The 22 kinases which were inhibited more than 50% by 5 µM elraglusib in a cell-free kinase screen (100 kinases) performed within the MRC PPU at the University of Dundee. Available published data for CT99021 and SB216763 are given as comparison against these kinases in the same assay conditions. Data are ‘remaining kinase activity’ relative to DMSO carrier control and are the average of triplicate assays
Next, we examined the in vitro sensitivity of over 100 different kinases to elraglusib and found that 22 kinases were inhibited > 50% at 5 µM (Fig. 2F). Elraglusib had potent action against GSK3b (87% inhibition at 5 µM), but equivalent potency against PIM (proto-oncogene serine/threonine-protein kinase) kinases 1 and 3, and MST2 (serine/threonine-protein kinase 3), also known as STK3. These kinases were not as sensitive to CT99021 or SB216763 (Fig. 2F) and are examples of differential off-target effects of elraglusib, worthy of further study. While this data emphasizes the need to consider other mechanism(s) of action for elraglusib it is not unusual for clinically useful drugs to have additional off-target effects, and of course, all of the known inhibitors of GSK3 have additional off-target effects.
Hence our data provide two lines of argument to suggest the anti-lymphoma action of elraglusib is not a consequence of GSK3 inhibition. Firstly, several other, more potent inhibitors of GSK3 do not alter the proliferation of lymphoma cells despite significant GSK3 inhibition. Secondly, validated targets of GSK3 action are relatively weakly inhibited by elraglusib (compared to other GSK3 inhibitors) at concentrations that generate changes in cell viability.
These are important observations as GSK3 is increasingly recognized as a potential therapeutic target in hematological malignancy. Structurally distinct GSK3 inhibitors can induce apoptosis in patient-derived CLL cells, reduce proliferation in AML cell lines and re-sensitize TP53-mutant Burkitt lymphoma cell lines to anthracycline chemotherapy [9,10,11]. Since GSK3 RNA/protein levels are higher within lymphoma cells in comparison to normal lymphocytes, and Wu et al. were unable to generate GSK3β knockouts in four of five lymphoma cell lines, an intrinsic dependence upon GSK3β for lymphoma survival was suggested [8]. These data led to the assumption that the efficacy of elraglusib in B- and T-cell lymphoma cell lines and patient-derived lymphoma xenograft models was due to GSK3 inhibition [8]. However, our studies demonstrate that GSK3 inhibition is unlikely to explain these actions of elraglusib. This compound inhibits additional kinases with similar potency to GSK3 including PIM kinases that are implicated in lymphomagenesis and are frequently overexpressed in human lymphomas [22,23,24]. Similarly, MST2 is a key member of the Hippo signaling pathway with putative roles in several cancers, including AML [25].
In conclusion, we re-affirm the anti-lymphoma effects of elraglusib but argue that this action cannot be attributed to GSK3 inhibition. Hence, we caution against the assumption that selective GSK3 inhibitors will have clinical benefit in lymphoma and against GSK3 activity as a mechanistic biomarker.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The raw data from the kinase screen for elraglusib will be available after publication on the MRC PPU website.
Abbreviations
- AML:
-
Acute myeloid leukemia
- CLL:
-
Chronic lymphocytic leukemia
- CRMP2:
-
Collapsin response-mediator protein 2
- DMSO:
-
Dimethyl sulfoxide
- ECL:
-
Enhanced chemiluminescence
- GSK3:
-
Glycogen synthase kinase 3
- HRP:
-
Horseradish peroxidase
- MST2/STK3:
-
Serine/threonine-protein kinase 3
- MTS:
-
3-(4,5-Dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium
- NHL:
-
Non-Hodgkin lymphoma
- PARP:
-
Poly (ADP-ribose) polymerase
- PIM:
-
Proto-oncogene serine/threonine-protein kinase
- SDS-PAGE:
-
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis
References
Liu Y, Barta SK. Diffuse large B-cell lymphoma: 2019 update on diagnosis, risk stratification, and treatment. Am J Hematol. 2019;94(5):604–16.
Fox CP, Ahearne MJ, Pettengell R, Dearden C, El-Sharkawi D, Kassam S, et al. Guidelines for the management of mature T- and natural killer-cell lymphomas (excluding cutaneous T-cell lymphoma): a British Society for Haematology Guideline. Br J Haematol. 2022;196(3):507–22.
Embi N, Rylatt DB, Cohen P. Glycogen synthase kinase-3 from rabbit skeletal muscle. Separation from cyclic-AMP-dependent protein kinase and phosphorylase kinase. Eur J Biochem. 1980;107(2):519–27.
Sutherland C. What Are the bona fide GSK3 Substrates? Int J Alzheimers Dis. 2011;2011:505607.
Jope RS, Johnson GV. The glamour and gloom of glycogen synthase kinase-3. Trends Biochem Sci. 2004;29(2):95–102.
Frame S, Cohen P, Biondi RM. A common phosphate binding site explains the unique substrate specificity of GSK3 and its inactivation by phosphorylation. Mol Cell. 2001;7(6):1321–7.
Quintayo MA, Munro AF, Thomas J, Kunkler IH, Jack W, Kerr GR, et al. GSK3beta and cyclin D1 expression predicts outcome in early breast cancer patients. Breast Cancer Res Treat. 2012;136(1):161–8.
Wu X, Stenson M, Abeykoon J, Nowakowski K, Zhang L, Lawson J, et al. Targeting glycogen synthase kinase 3 for therapeutic benefit in lymphoma. Blood. 2019;134(4):363–73.
Ougolkov AV, Bone ND, Fernandez-Zapico ME, Kay NE, Billadeau DD. Inhibition of glycogen synthase kinase-3 activity leads to epigenetic silencing of nuclear factor kappaB target genes and induction of apoptosis in chronic lymphocytic leukemia B cells. Blood. 2007;110(2):735–42.
Wagner FF, Benajiba L, Campbell AJ, Weiwer M, Sacher JR, Gale JP, et al. Exploiting an Asp-Glu “switch” in glycogen synthase kinase 3 to design paralog-selective inhibitors for use in acute myeloid leukemia. Sci Transl Med. 2018;10(431):eaam8460.
Harrington CT, Sotillo E, Robert A, Hayer KE, Bogusz AM, Psathas J, et al. Transient stabilization, rather than inhibition, of MYC amplifies extrinsic apoptosis and therapeutic responses in refractory B-cell lymphoma. Leukemia. 2019;33(10):2429–41.
Karmali R, Chukkapalli V, Gordon LI, Borgia JA, Ugolkov A, Mazar AP, et al. GSK-3beta inhibitor, 9-ING-41, reduces cell viability and halts proliferation of B-cell lymphoma cell lines as a single agent and in combination with novel agents. Oncotarget. 2017;8(70):114924–34.
ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 20 Sep 2018. Identifier NCT03678883, 9-ING-41 in Patients With Advanced Cancers . Available from: https://clinicaltrials.gov/ct2/show/NCT03678883. Updated 7 Dec 2022, Accessed 25 Jan 2023.
Hsu A, Huntington KE, De Souza A, Zhou L, Olszewski AJ, Makwana NP, et al. Clinical activity of 9-ING-41, a small molecule selective glycogen synthase kinase-3 beta (GSK-3beta) inhibitor, in refractory adult T-Cell leukemia/lymphoma. Cancer Biol Ther. 2022;23(1):417–23.
Finlay D, Patel S, Dickson LM, Shpiro N, Marquez R, Rhodes CJ, et al. Glycogen synthase kinase-3 regulates IGFBP-1 gene transcription through the thymine-rich insulin response element. BMC Mol Biol. 2004;5:15.
Logie L, Ruiz-Alcaraz AJ, Keane M, Woods YL, Bain J, Marquez R, et al. Characterization of a protein kinase B inhibitor in vitro and in insulin-treated liver cells. Diabetes. 2007;56(9):2218–27.
Cole AR, Noble W, van Aalten L, Plattner F, Meimaridou R, Hogan D, et al. Collapsin response mediator protein-2 hyperphosphorylation is an early event in Alzheimer’s disease progression. J Neurochem. 2007;103(3):1132–44.
Rena G, Guo S, Cichy SC, Unterman TG, Cohen P. Phosphorylation of the transcription factor forkhead family member FKHR by protein kinase B. J Biol Chem. 1999;274(24):17179–83.
Bain J, Plater L, Elliott M, Shpiro N, Hastie CJ, McLauchlan H, et al. The selectivity of protein kinase inhibitors: a further update. Biochem J. 2007;408(3):297–315.
Cole AR, Knebel A, Morrice NA, Robertson LA, Irving AJ, Connolly CN, et al. GSK-3 phosphorylation of the Alzheimer epitope within collapsin response mediator proteins regulates axon elongation in primary neurons. J Biol Chem. 2004;279(48):50176–80.
Beurel E, Grieco SF, Jope RS. Glycogen synthase kinase-3 (GSK3): regulation, actions, and diseases. Pharmacol Ther. 2015;148:114–31.
Nawijn MC, Alendar A, Berns A. For better or for worse: the role of Pim oncogenes in tumorigenesis. Nat Rev Cancer. 2011;11(1):23–34.
Hsi ED, Jung SH, Lai R, Johnson JL, Cook JR, Jones D, et al. Ki67 and PIM1 expression predict outcome in mantle cell lymphoma treated with high dose therapy, stem cell transplantation and rituximab: a Cancer and Leukemia Group B 59909 correlative science study. Leuk Lymphoma. 2008;49(11):2081–90.
Care MA, Barrans S, Worrillow L, Jack A, Westhead DR, Tooze RM. A microarray platform-independent classification tool for cell of origin class allows comparative analysis of gene expression in diffuse large B-cell lymphoma. PLoS ONE. 2013;8(2):e55895.
Wermke M, Camgoz A, Paszkowski-Rogacz M, Thieme S, von Bonin M, Dahl A, et al. RNAi profiling of primary human AML cells identifies ROCK1 as a therapeutic target and nominates fasudil as an antileukemic drug. Blood. 2015;125(24):3760–8.
Acknowledgements
The authors would like to thank Sourav Banerjee, University of Dundee, for providing the HS-Sultan cells.
Funding
Funding for this work was provided equally by the Ninewells Cancer Campaign Fraser Fellowship Doctoral Training Programme and the Tayside Haematology and Leukaemia Research Endowment Fund.
Author information
Authors and Affiliations
Contributions
JTC performed all of the work while ST and CS designed the project, raised the funding and supervised the work. All authors contributed to manuscript preparation. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Coats, J.T., Tauro, S. & Sutherland, C. Elraglusib (formerly 9-ING-41) possesses potent anti-lymphoma properties which cannot be attributed to GSK3 inhibition. Cell Commun Signal 21, 131 (2023). https://doi.org/10.1186/s12964-023-01147-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-023-01147-8