Abstract
In the first part of this review, the nature of the associations between alcohol use and HIV/AIDS is discussed. Alcohol use has been found to be strongly associated with incidence and progression of HIV/AIDS, but the extent to which this association is causal has traditionally remained in question. Experiments where alcohol use has been manipulated as the independent variable have since helped establish a causal effect of alcohol use on the intention to engage in condomless sex. As the intention to engage in condomless sex is a surrogate measure of actual condom use behavior, which itself is linked to HIV incidence and re-infection, the causal chain has been corroborated. Moreover, there are biological pathways between alcohol use and the course of HIV/AIDS, only in part being mediated by adherence to antiretroviral medication. In the second part of the contribution, we provide suggestions on the quantification of the link between alcohol use and HIV incidence, using risk relations derived from experimental data. The biological links between alcohol use and course of HIV/AIDS are difficult to quantify given the current state of knowledge, except for an operationalization for the link via adherence to medication based on meta-analyses. The suggested quantifications are exemplified for South Africa.
Similar content being viewed by others
Background
Alcohol use is a major risk factor for burden of disease and injury [1–4]. It has been shown to affect not only non-communicable chronic diseases [5, 6] and injuries [7, 8], but also communicable diseases [9, 10]. To date, two communicable diseases have been included into the Global Burden of Disease Comparative Risk Factor Assessment as being causally impacted by alcohol, starting with the 2010 study ([11]; see also the 2013 [4] and the 2015 [3] studies): tuberculosis [12, 13] and lower respiratory infections [14]. The Global Status Report on Alcohol and Health of the World Health Organization [1] included these two disease categories as well, but added the effect of alcohol use on antiretroviral medication adherence and its impact on AIDS mortality ([15]; based on a number of reviews [16–20]).
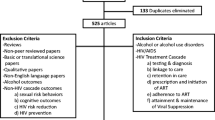
The status of alcohol use as a cause for HIV infection, and its effects separate from non-adherence, on the course of HIV/AIDS have been discussed in recent years [21–23] but were found to be non-conclusive at a meeting to discuss the causal role of alcohol use on HIV/AIDS organized by WHO and the South African Medical Research Council [24]. However, since this meeting took place, considerable new scientific evidence seems to support a causal role of alcohol. Furthermore, systematic reviews and meta-analyses are now available to allow quantification of the impact in a way in line with the quantification of other risks attributable to alcohol or other risk factors in the global Comparative Risk Assessments (for methodology see [25]). The present contribution first summarizes the evidence on the relationship between alcohol use and HIV/AIDS, mainly based on systematic reviews and meta-analyses. In the second part, a methodology to quantify this impact is introduced.
The establishment of causality is key in these deliberations. Causality is defined here based on Rothman [26–28] as a multiple components model, where all components need to be present to produce the effect. In the specific case for alcohol and HIV incidence, different such sets of components have been identified, which can be seen as causal pathways, where alcohol use plays a necessary role (see below). The case for causality seems convincing, because in addition to fulfilling the usual epidemiological and thus observational Bradford Hill criteria [29] such as association, temporality, and plausibility, we have experimental evidence for key parts of several pathways, including the pathway of alcohol use on decision-making.
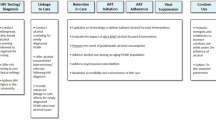
Review: Alcohol use and HIV/AIDS: association and causal considerations
Alcohol use was found to be associated with HIV in recent systematic reviews and meta-analyses [30–36]. Three different explanations have been brought forward to explain the association: a) the impact of alcohol use on decision-making, resulting in riskier sexual behaviors (reviews of [34, 37–43]); b) biological effects of alcohol use on HIV transmission and disease progression ([44] as overview; see also [16, 45–47]), including but not limited to effects of alcohol on treatment course and medication adherence [16–19, 48]; and c) that most or all of the effects of alcohol on HIV incidence and disease progression can be explained by third variables, especially the effect of risk-taking and other personality variables [49, 50].
To exclude the third explanation and corroborate the causality of the alcohol-HIV incidence via impacts on decision-making on safer sex practices, a number of experimental trials have been conducted, where alcohol use was experimentally manipulated as the main factor. Systematic reviews and meta-analysis of the results of these trials indicated a causal impact of alcohol use on decisions about unsafe sex practices, both when alcohol use was compared to placebo, or to intake of non-alcoholic beverages [42, 43]. It should be noted that the underlying experiments have been conducted in different populations, including people living with HIV (PLWH) (e.g., [51]).
The reservation must be made that for ethical and practical reasons, experimental studies, which are necessary to determine causality, can only use surrogate endpoints (i.e., intention for condomless sex) rather than condomless sex itself or HIV infection. However, the results of experimental studies corroborate the results of epidemiological cohort and cross-sectional studies with condomless sex [34, 37–39, 41, 52–55], sexually transmitted disease [56, 57], or HIV incidence [31] as endpoints. Moreover, there are meta-analyses that show a clear link between intentions for unsafe sex and resulting behavior [58, 59], as well as between condomless sexual practices and HIV seroconversion [60–62].
The above seems to be in contradiction to some event-level studies, which have not always found a negative impact of alcohol on unsafe sex [63, 64]. However, event-level studies have been often done in select non-probability samples, or via surveys without adequate control, so that the experimental evidence mentioned is clearly preferable to control for potential confounding [65].
With respect to biological impacts, there seems to be clear evidence that heavy drinking or alcohol use disorders are associated with viral load increases and/or CD4 count declines, general weakening of the immune system, and more negative outcomes of antiretroviral therapy (ART), partly mediated by treatment adherence and partly by the pharmacological interactions of alcohol with ART and other medications to treat co-morbidities (for the association regarding adherence see above; for the other associations see for heavy drinking: [46, 66]; for AUD: [16]; for mechanisms see [20, 46, 48, 67, 68]; for pharmacological interactions see [69, 70]). It should be noted, however, that delineation of causality in these biological pathways is difficult, as many factors interact, and even when causality has potentially been established, it is hard to quantify the causal contribution of alcohol to HIV/AIDS disease progression based on biological mechanisms [20, 66–68, 71].
Quantification of the effect of alcohol use on HIV
The effect of alcohol on decision-making
In a meta-analysis of experimental studies, [42] alcohol use associated with a blood alcohol concentration (BAC) level of 0.07 g/dl was shown to impact decision-making for condomless sex (based on averaging the 28 individual studies). The latter findings can be used for illustrative burden of disease quantifications. Participants with a BAC level of 0.07 g/dl were 1.54 (95% CI 1.31–1.78) times more likely to consider condomless sex compared to those who had not used alcohol (see also Additional file 1). For normal, non-experimental drinking situations, this BAC would correspond to an average of 49 g pure alcohol ingested for women and of 61 g for men. The grams of alcohol corresponding to a BAC of 0.07 g/dl were derived from standard tables based on sex-specific average body weight from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) [72, 73].
In order to quantify the effect of alcohol use on HIV/AIDS at the population level, we selected people who consume on average at least at this level per day, corresponding to a small minority of the drinkers in each country. We provide the example of South Africa to illustrate these quantifications in a country with very high prevalence and burden of HIV/AIDS [74–76] and comparably high levels of heavy alcohol use among current drinkers [1] (see also Additional file 1).
There are several assumptions in this choice of operationalization. First, it assumes that sexually active people drink at least at the same level as the general population. Second, it assumes that people with HIV/AIDS continue to have sex and drink at the same level as the general population. And third, it is assumed that there are no interactions with other variables that could change the causal relation.
The first assumption seems to be without a problem; at least there is no empirical evidence for the contrary, and some specific evidence that sexual activity is associated with drinking in some groups. Regarding the second set of assumptions, alcohol consumption and HIV have been shown to be associated among cross-sectional samples in Africa [35]. This general association held true, despite the high stigma of alcohol use which may lead people with HIV or AIDS to withhold reporting their drinking status or drinking level, especially if they are seeking treatment for ART [77, 78]. Some of the results from Africa for people on ART showed less involvement with alcohol after treatment initiation, whereas other findings have demonstrated high alcohol consumption among ART patients [79, 80]. Regarding the assumption that people with HIV/AIDS continue to be sexually active, this has certainly been the case, even though evidence showed that their level of sexual activity and condomless sex may be reduced after testing positive in general, or after ART initiation ([81]; for papers specifically from South Africa: [82–84]). However, other evidence from South Africa suggested that alcohol use was associated with a high likelihood of condomless sex after a positive HIV test [85]. Overall, the main assumptions of the model about continuation of sexual activities and consumption of alcohol after seroconversion seem to be justified. The third assumption postulated lack of interactions. While we cannot control for all these interactions, such as use of vaginal microbicide gels [86] or socioeconomic status and related malnutrition [87], many of these seem to increase the impact of alcohol use on HIV infection.
Illustrative quantification of the effect of alcohol use on HIV incidence in South Africa
Applying the above-derived drinking level cutoffs results in 29.6% (95% Uncertainty Interval (UI): 24.7%–32.3%) (15.6% women and 36.8% men; see all UIs in the Additional file 1) of adult (15 years of age and older) drinkers drinking above the cutoff; and 12.0% (95% UI: 9.3%–14.1%) (4.1% women and 20.7% men) of the total adult population. Combining this exposure, stratified by age, with the risk relations found in the most recent meta-analysis [42] resulted in the following estimates with respect to HIV incidence for South Africa in 2012: 18,200 incident cases (95% UI: 8,400–28,000) (7,000 among women, 11,200 among men) attributable to alcohol use; population attributable fraction 3.9% (95% UI: 1.8%–6.0%) (2.2% for women, 7.4% for men) (incidence data from [88]; for a detailed description of the methodology and all uncertainty intervals please see Additional file 1).
Illustrative quantification of the effect of alcohol use on disease course and mortality including adherence to medication in South Africa
Combining the above-described sex- and age-specific exposure estimates with the risk relations reported in experimental studies yielded population attributable fractions of 4.5% (95% UI: 2.2%–6.8%) for HIV/AIDS mortality (2.3% for women and 6.8% for men) and 4.3% (95% UI: 2.1%–6.5%) (2.2% for women and 6.6% for men) for HIV/AIDS-related burden of disease, as quantified in disability-adjusted life years (DALYs) for 2012 in South Africa (for methodology see Additional file 1).
Combining this burden with the alcohol-attributable burden of disease caused by non-adherence to highly active ART (based on [15]), we estimate that in South Africa in 2012, alcohol use caused 12,200 (95% UI: 6,000–18,400) HIV- or AIDS-related deaths (2,900 deaths among women, 9,300 deaths among men); 634,800 (95% UI: 309,300–960,100) HIV/AIDS-related years of life lost due to premature mortality (YLL; 157,600 YLLs among women, 477,200 YLLs among men); 44,000 (95% UI: 21,300–66,700) HIV/AIDS-related years lived with disability (YLDs; 11,400 YLDs among women, 32,600 YLDs among men); and 678,800 (95% UI: 330,600–1,026,800) DALYs (169,100 DALYs among women, 509,700 DALYs among men). Uncertainty intervals for all estimates can be found in the Additional file 1.
Discussion
The above estimates are likely to underestimate the alcohol-attributable HIV incidence and disease burden for a number of reasons. First, a dose–response relationship has not been quantified, and the estimate reported above was based on a step function with an increased risk for a BAC of 0.07 g/dl taken for all BACs above this threshold. However, a dose–response relationship where higher levels of BAC correspond with a higher risk to engage in/consider condomless sex can be expected. This relationship is hard to quantify, as BAC levels beyond 0.11 g/dl cannot be tested experimentally for ethical and practical reasons ([43]; for general dose–response relationships between alcohol and other behaviors such as drunk driving: [8]). It has also been shown that even below a BAC of 0.07 g/dl participants were roughly 50% more likely to report the intention of having condomless sex compared to those who did not drink alcohol [42]. However, the lower limits for the respective BAC were not quantified/reported.
Second, the above estimation is based on regular heavy use and thereby does not include single drinking occasions where a BAC above 0.07 g/dl is reached. This may have further contributed toward potential underestimation, as irregular heavy drinking occasions are a common drinking pattern in South Africa [89] and are generally more prevalent than regular heavy drinking (i.e., an average daily use above the threshold).
Finally, it should be noticed that the amount of alcohol needed to reach a specific BAC depends on body weight (e.g., [90]). The estimation of 49 g and 61 g of pure alcohol for women and men, respectively, is based on the average weight in the North American region. As the average weight in the African region is about 20 kg below the average weight in the North American Region [91], the amount of pure alcohol needed to reach a BAC of 0.07 g/dl can be considered as an overestimate for South Africa.
However, there may also be some attenuation of the risk relationship, as the link between intention and actual behavior is not perfect. This may be modeled in future analyses by including the strength of the association between intention and actual behavior from meta-analyses [58, 59].
Most important, however, is the fact that all the biological pathways of alcohol use (see above for discussion and references) are not considered in the current model. The above-derived population attributable fractions would also be markedly smaller than any fractions derived from the classic formulas [92, 93], combining the prevalence of drinking (around 40% in South Africa [1]) with relative risk for incident HIV (about 2 overall for all studies; [31]), which would result in a population-attributable fraction of 28%.
Overall, the above calculation presents a first approach to quantifying the impact of alcohol use on incidence of HIV and disease burden of HIV/AIDS, which goes beyond modeling only the effect on medication adherence. However, while this approach was able to estimate one additional pathway, there are other pathways such as the pharmacological effects on the immune system and the pharmacological interactions with medications, or the effect of alcohol use on re-infection [94], which remain to be quantified.
Moreover, different pathways may interact with each other. Even for the pathway modeled here, in the future continuous risk functions based on the continuous exposure distributions need to be created. Thus, while the current effort is one step to better modeling the impact of alcohol use on HIV incidence and burden of HIV/AIDS, more research on the above details is needed.
While the current paper has been confined to methodological aspects on the causality of the relationship between alcohol use and HIV/AIDS and on the quantification of identified pathways, the results of the review also have implications for health policy. Given the high impact of HIV/AIDS on the disease burden in South Africa and sub- Saharan Africa in general [74, 75, 95], the identification of alcohol as a causal factor for incidence opens new ways to reduce the disease burden of these conditions [94]. These include classic alcohol policy measures [96] as well as the integration of alcohol interventions into the treatment of HIV/AIDS [97].
Conclusion
Alcohol use is strongly associated with the incidence and course of HIV/AIDS, and based on experimental data where alcohol use has been manipulated as the independent variable, a causal effect of alcohol use on the intention of condomless sex can be asserted. Condomless sex intentions can be seen as a surrogate measure of actual condom use behavior, which itself is linked to HIV incidence and re-infection. Moreover, there are biological links between alcohol use and worsening the course of HIV/AIDS, in part being mediated by adherence to medication.
To quantify the link between alcohol use and HIV incidence, we rely on risk relations based on experimental data. Other pathways from alcohol use to HIV/AIDS burden of disease cannot be quantified given the current state of knowledge, except for an operationalization for the link via adherence to medication based on meta-analyses. Overall, this approach to model alcohol-attributable incidence of HIV and burden of HIV/AIDS needs to be further developed in the future, especially with regard to accounting for dose–response relationships and binge drinking occasions.
Abbreviations
- AIDS:
-
Acquired Immunodeficiency Syndrome
- ART:
-
Antiretroviral therapy
- AUD:
-
Alcohol Use Disorders
- BAC:
-
Blood Alcohol Concentration
- DALYs:
-
Disability-adjusted life years
- HIV:
-
Human Immunodeficiency Virus
- UI:
-
Uncertainty interval
- YLDs:
-
Years lived with disability
- YLLs:
-
Years of life lost due to premature mortality
References
World Health Organization. Global status report on alcohol and health. Geneva, Switzerland: World Health Organization; 2014.
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol use disorders. Lancet. 2009;373:2223–33.
GBD. Risk Factors Collaborators: Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2015;2016(388):1659–724.
Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–323.
Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, et al. Contribution of six risk factors to achieving the “25 × 25” NCD mortality reduction target. Lancet. 2014;384:427–37.
Parry C, Patra J, Rehm J. Alcohol consumption and non-communicable diseases: epidemiology and policy implications. Addiction. 2011;106:1718–24.
Shield KD, Gmel Jr G, Patra J, Rehm J. Global burden of injuries attributable to alcohol consumption in 2004: a novel way of calculating the burden of injuries attributable to alcohol consumption. Popul Health Metr. 2012;10:9.
Cherpitel C, Ye Y, Bond J, Borges G, Autonoma M, Monteiro M, et al. Alcohol attributable fraction for injury morbidity from the dose–response relationship of acute alcohol consumption: emergency department data from 18 countries. Addiction. 2015;110:1724–32.
Rehm J, Baliunas D, Borges GL, Graham K, Irving HM, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease - An overview. Addiction. 2010;105:817–43.
Rehm J, Gmel Sr G, Gmel GE, Hasan OSM, Imtiaz S, Popova S, Probst C, Roerecke M, Room R, Samokhvalov AV, Shield KD, Shuper PA. (2017). The relationship between different dimensions of alcohol use and the burden of disease - an update. Addiction.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Rehm J, Samokhvalov AV, Neuman MG, Room R, Parry CD, Lönnroth K, et al. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review BMC Public Health. 2009;9:450.
Lönnroth K, Williams B, Stadlin S, Jaramillo E, Dye C. Alcohol use as a risk factor for tuberculosis - a systematic review. BMC Public Health. 2008;8:289.
Samokhvalov AV, Irving HM, Rehm J. Alcohol consumption as a risk factor for pneumonia: systematic review and meta-analysis. Epidemiol Infect. 2010;138:1789–95.
Gmel G, Shield K, Rehm J. Developing a methodology to derive alcohol-attributable fractions for HIV/AIDS mortality based on alcohol’s impact on adherence to antiretroviral medication. Popul Health Metr. 2011;9:5.
Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112:178–93.
Grodensky CA, Golin CE, Ochtera RD, Turner BJ. Systematic review: effect of alcohol intake on adherence to outpatient medication regimens for chronic diseases. J Stud Alcohol Drugs. 2012;73:899–910.
Braithwaite RS, Bryant KJ. Influence of Alcohol Consumption on Adherence to and Toxicity of Antiretroviral Therapy and Survival. Alcohol Res Health. 2010;33:280–7.
Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52:180–202.
Neuman MG, Schneider M, Nanau RM, Parry C. Alcohol consumption, progression of disease and other comorbidities, and response to antiretroviral medication in people living with HIV. AIDS Research & Treatment. 2012;2012:751827. doi:10.1155/2012/751827.
Hahn JA, Woolf-King SE, Muyindike W. Adding Fuel to the Fire: Alcohol’s Effect on the HIV Epidemic in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2011;8:172–80.
Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376:398–400.
Rehm J, Parry CD. Alcohol consumption and infectious diseases in South Africa. Lancet. 2009;374:2053.
Parry CDH, Rehm JR, Poznyak V, Room R. Alcohol and infectious diseases: are there causal linkages? Addiction. 2009;104:331–2.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global Burden of Disease and Risk Factors. New York & Washington: The World Bank and Oxford University Press; 2006.
Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
Rothman KJ, Greenland S. Causation and causal inference in epidemiology. Am J Public Health. 2005;95:S144–50.
Frick U, Rehm J. Can we establish causality with statistical analyses? The example of epidemiology. In: Wiedermann W, von Eye A, editors. Statistics and causality: methods for applied empirical research. Hoboken, NJ: Wiley; 2016. p. 407–32.
Hill A. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300.
Schensul JJ, Singh SK, Gupta K, Bryant K, Verma R. Alcohol and HIV in India: a review of current research and intervention. AIDS Behav. 2010;14 Suppl 1:S1–7.
Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55:159–66.
Pithey A, Parry C. Descriptive systematic review of sub-Saharan African studies on the association between alcohol use and HIV infection. SAHARA J. 2009;6:155–69.
Van Tieu H, Koblin BA. HIV, alcohol, and noninjection drug use. Curr Opin HIV AIDS. 2009;4:314–8.
Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13:757–82.
Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34:856–63.
Lan CW, Scott-Sheldon LA, Carey KB, Johnson BT, Carey MP: Prevalence of Alcohol Use, Sexual Risk Behavior, and HIV Among Russians in High-Risk Settings: a Systematic Review and Meta-Analysis. Int J Behav Med. 2016. doi:10.1007/s12529-016-9596-1.
Scott-Sheldon LA, Walstrom P, Carey KB, Johnson BT, Carey MP. Alcohol use and sexual risk behaviors among individuals infected with HIV: a systematic review and meta-analysis 2012 to early 2013. Curr HIV/AIDS Rep. 2013;10:314–23.
Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behavior in Sub-Saharan Africa: a narrative review. Arch Sex Behav. 2011;40:17–42.
Sales JM, Brown JL, Vissman AT, DiClemente RJ. The association between alcohol use and sexual risk behaviors among African American women across three developmental periods: a review. Curr Drug Abuse Rev. 2012;5:117–28.
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8:141–51.
Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13:1021–36.
Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP. Alcohol Use Predicts Sexual Decision-Making: A Systematic Review and Meta-Analysis of the Experimental Literature. AIDS Behav. 2015;20 Suppl 1:S19-S39. doi:10.1007/s10461-015-1108-9.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107:51–9.
Pandrea I, Happel KI, Amedee A, Bagby GJ, Nelson S. Alcohol’s Role in HIV Transmission and Disease Progression. Alcohol Res Health. 2010;33:203–18.
Amedee AM, Nichols WA, Robichaux S, Bagby GJ, Nelson S. Chronic alcohol abuse and HIV disease progression: studies with the non-human primate model. Curr HIV Res. 2014;12:243–53.
Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. 2010;7:226–33.
Justice AC, McGinnis KA, Tate JP, Braithwaite RS, Bryant KJ, Cook RL, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016;161:95–103.
Kumar S, Jin M, Ande A, Sinha N, Silverstein PS, Kumar A. Alcohol consumption effect on antiretroviral therapy and HIV-1 pathogenesis: role of cytochrome P450 isozymes. Expert Opin Drug Metab Toxicol. 2012;8:1363–75.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS - a systematic review. Alcohol Alcohol. 2010;45:159–66.
Shuper PA, Joharchi N, Rehm J. Personality as a predictor of unprotected sexual behavior among people living with HIV/AIDS: a systematic review. AIDS Behav. 2014;18:398–410.
Shuper PA, Joharchi N, Rehm J. Protocol for a controlled experiment to identify the causal role of acute alcohol consumption in condomless sex among HIV-positive MSM: study procedures, ethical considerations, and implications for HIV prevention. AIDS Behav. 2015;20:173–84.
Cooper ML: Alcohol use and risky sexual behavior among college students and youth. J Stud Alcohol. 2002;14 Suppl 4:101–117. doi:10.15288/jsas.2002.s14.101.
Halpern-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health. 1996;19:331–6.
Heath J, Lanoye A, Maisto SA. The Role of Alcohol and Substance Use in Risky Sexual Behavior Among Older Men Who Have Sex With Men: A Review and Critique of the Current Literature. AIDS Behav. 2011;16:578–89.
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48:1035–45.
Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sex Transm Dis. 2005;32:156–64.
Li Q, Stanton B. Alcohol use and sexual risk behaviors and outcomes in China: a literature review. AIDS Behav. 2010;14:1227–36.
Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125:90–132.
Sheeran P, Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. Br J Soc Psychol. 1998;37:231–50.
Detels R, English P, Visscher BR, Jacobson L, Kingsley LA, Chmiel JS, et al. Seroconversion, sexual activity, and condom use among 2915 HIV seronegative men followed for up to 2 years. J Acquir Immune Defic Syndr. 1989;2:77–83.
Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Soc Sci Med. 1997;44:1303–12.
Smith DK, Herbst JH, Zhang X, Rose CE. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015;68:337–44.
Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis. 2002;29:476–82.
Kiene SM, Subramanian SV. Event-level association between alcohol use and unprotected sex during last sex: evidence from population-based surveys in sub-Saharan Africa. BMC Public Health. 2013;13:583.
Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. New York, U.S: Houghton Mifflin Company; 2002.
Baum MK, Rafie C, Lai S, Sales S, Page JB, Campa A. Alcohol use accelerates HIV disease progression. AIDS Research & Human Retroviruses. 2010;26:511–8.
Molina PE, Amedee AM, Winsauer P, Nelson S, Bagby G, Simon L. Behavioral, Metabolic, and Immune Consequences of Chronic Alcohol or Cannabinoids on HIV/AIDs: Studies in the Non-Human Primate SIV Model. J Neuroimmune Pharmacol. 2015;10:217–32.
Pandrea I, Happel KI, Amedee AM, Bagby GJ, Nelson S: Alcohol’s Role in HIV Transmission and Disease Progression. Bethesda, MD: 2010.
Neuman MG, Monteiro M, Rehm J. Drug interactions between psychoactive substances and antiretroviral therapy in individuals infected with human immunodeficiency and hepatitis viruses. Subst Use Misuse. 2006;41:1395–463.
Neuman MG, Schneider M, Nanau RM, Parry C. HIV-antiretroviral therapy induced liver, gastrointestinal, and pancreatic injury. Int J Hepatol. 2012;2012:760706. doi:10.1155/2012/760706.
Schneider M, Neuman M, Chersich M, Parry C. Alcohol and Antiretroviral Therapy - A Lethal Cocktail. J AIDS Clin Res. 2011;S1:005.
Roberts LJ, McCrady BS. Alcohol problems in intimate relationships: identification and intervention - A guide for marriage and family therapists. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003.
National Institute on Alcohol Abuse and Alcoholism: NIAAA Council Approves Definition of Binge Drinking. NIAAA Newsletter, No. 3, 2004. http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. Accessed 18 Oct 2016.
GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–58.
GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–544.
Institute for Health Metrics and Evaluation: South Africa. 2016. http://www.healthdata.org/south-africa. Accessed 19 Oct 2016.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131:23–35.
Kekwaletswe C, Morojele NK. The links between alcohol consumption and ART adherence: Perceptions of ART recipients and health care providers in Gauteng, South Africa. In 30th International Congress of Psychology. Cape Town, South Africa; 2012.
Morojele NK, Kekwaletswe C. Associations between alcohol use, other psychosocial factors, structural factors and antiretroviral therapy (ART) adherence among South African ART recipients. AIDS Behav. 2014;18:519–24.
Kader R, Seedat S, Koch JR, Parry CD. A preliminary investigation of the AUDIT and DUDIT in comparison to biomarkers for alcohol and drug use among HIV-infected clinic attendees in Cape Town, South Africa. Afr J Psychiatry (Johannesbg). 2012;15:346–51.
Doyle JS, Degenhardt L, Pedrana AE, McBryde ES, Guy RJ, Stoové MA, et al. Effects of HIV antiretroviral therapy on sexual and injecting risk-taking behavior: a systematic review and meta-analysis. Clin Infect Dis. 2014;59:1483–94.
McGrath N, Richter L, Newell ML. Sexual risk after HIV diagnosis: a comparison of pre-ART individuals with CD4500 cells/ml and ART-eligible individuals in a HIV treatment and care programme in rural KwaZulu-Natal, South Africa. J Int AIDS Soc. 2013;16:18048. doi:10.7448/IAS.16.1.18048.
Venkatesh KK, de Bruyn G, Lurie MN, Mohapi L, Pronyk P, Moshabela M, et al. Decreased sexual risk behavior in the era of HAART among HIV-infected urban and rural South Africans attending primary care clinics. AIDS. 2010;24:2687–96.
Eisele TP, Mathews C, Chopra M, Lurie MN, Brown L, Dewing S, et al. Changes in risk behavior among HIV-positive patients during their first year of antiretroviral therapy in Cape Town South Africa. AIDS Behav. 2009;13:1097–105.
Shuper PA, Pillay S, MacDonald S, Christie S, Cornman DH, Fisher WA, et al. One in 4 HIV-Positive South Africans Awaiting ART Initiation Report Condomless Sex With a Serodiscordant Partner. Journal of Aquired Immune Deficiency Syndromes. 2016;72:e77–9.
Williams BG, Abdool Karim SS, Karim QA, Gouws E. Epidemiological impact of tenofovir gel on the HIV epidemic in South Africa. Journal of Aquired Immune Deficiency Syndromes. 2011;58:207–10.
Probst C, Simbayi LC, Parry C, Shuper PA, Rehm J. Alcohol use, socioeconomic status and risk of HIV infections. AIDS Behav 2016, in peer-review.
Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press; 2014.
Peltzer K, Davids A, Njuho P. Alcohol use and problem drinking in South Africa: findings from a national population-based survey. Afr J Psychiatry (Johannesbg). 2011;14:30–7.
Fisher HR, Simpson RI, Kapur BM. Calculation of Blood-Alcohol Concentration (BAC) by sex, weight, number of drinks and time. Can J Public Health. 1987;78:300–4.
Walpole SC, Prieto-Merino D, Edwards P, Cleland J, Stevens GA, Roberts I. The weight of nations: an estimation of adult human biomass. BMC Public Health. 2012;12:439. doi:10.1186/1471-2458-12-439.
Walter SD. The estimation and interpretation of attributable risk in health research. Biometrics. 1976;32:829–49.
Walter SD. Prevention of multifactorial disease. Am J Epidemiol. 1980;112:409–16.
Morojele NK, Nkosi S, Kekwaletswe CT, Saban A, Parry CDH. Review of research on alcohol and HIV in Sub-Saharan Africa. South African Medical Resesarch Council; 2013. http://www.mrc.ac.za/policybriefs/AlcoholSubSaharan.pdf. Accessed 18 Oct 2016.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602.
Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No ordinary commodity. Research and public policy. 2nd edition. Oxford and London: Oxford University Press; 2010.
Parry C, Ferreira-Borges C, Poznyak V, Lönnroth K, Rehm J. The International Study on Alcohol and Infectious Diseases: three priorities for research. Addiction. 2013;108:1–2.
Acknowledgments
None.
Funding
This research did not receive specific funding. Part of the work was carried out within the tasks of the WHO Collaborating Centre for Mental Health and Addiction.
Availability of data and materials
All data sources are clearly referenced in the manuscript.
Authors’ contributions
JR conceptualized the overall work and wrote the first draft. KDS and CP provided the quantifications and assumptions for South Africa. PAS contributed much of the specific knowledge about literature on people living with HIV and AIDS. CP also led the revision, to which all authors contributed. All authors worked on various drafts of the manuscript and approved the final version.
Competing interests
All authors declare no potential conflict of interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable, as we used only published data sources.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Supplemental methodological information. (DOCX 31 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rehm, J., Probst, C., Shield, K.D. et al. Does alcohol use have a causal effect on HIV incidence and disease progression? A review of the literature and a modeling strategy for quantifying the effect. Popul Health Metrics 15, 4 (2017). https://doi.org/10.1186/s12963-017-0121-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12963-017-0121-9