Abstract
Background
In healthcare, analysing patient-reported outcome measures (PROMs) on an aggregated level can improve and regulate healthcare for specific patient populations (meso level). This mixed-methods systematic review aimed to summarize and describe the effectiveness of quality improvement methods based on aggregated PROMs. Additionally, it aimed to describe barriers, facilitators and lessons learned when using these quality improvement methods.
Methods
A mixed-methods systematic review was conducted. Embase, MEDLINE, CINAHL and the Cochrane Library were searched for studies that described, implemented or evaluated a quality improvement method based on aggregated PROMs in the curative hospital setting. Quality assessment was conducted via the Mixed Methods Appraisal Tool. Quantitative data were synthesized into a narrative summary of the characteristics and findings. For the qualitative analysis, a thematic synthesis was conducted.
Results
From 2360 unique search records, 13 quantitative and three qualitative studies were included. Four quality improvement methods were identified: benchmarking, plan-do-study-act cycle, dashboards and internal statistical analysis. Five studies reported on the effectiveness of the use of aggregated PROMs, of which four identified no effect and one a positive effect. The qualitative analysis identified the following themes for facilitators and barriers: (1) conceptual (i.e. stakeholders, subjectivity of PROMs, aligning PROMs with clinical data, PROMs versus patient-reported experience measures [PREMs]); (2a) methodological—data collection (i.e. choice, timing, response rate and focus); (2b) methodological—data processing (i.e. representativeness, responsibility, case-mix control, interpretation); (3) practical (i.e. resources).
Conclusion
The results showed little to no effect of quality improvement methods based on aggregated PROMs, but more empirical research is needed to investigate different quality improvement methods. A shared stakeholder vision, selection of PROMs, timing of measurement and feedback, information on interpretation of data, reduction of missing data, and resources for data collection and feedback infrastructure are important to consider when implementing and evaluating quality improvement methods in future research.
Key messages
What is already known on this topic
The aggregated patient-reported outcome measures (PROMs) can be used for analytical and organizational aspects of improving and regulating healthcare, but there is little empirical evidence regarding the effectiveness of aggregated PROMS.
What this study adds
This study adds a detailed overview of the types of quality improvement methods and recommendations for implementation in practice.
How this study might affect research, practice or policy
Researchers and policy-makers should consider the barriers, facilitators and lessons learned for future implementation and evaluation of quality improvement methods, as presented in this manuscript, to further advance this field.
Similar content being viewed by others
Background
Since the introduction of value-based healthcare by Porter [1] in 2006, an increase in the use of patients’ perspectives on health outcomes for quality and safety improvement in healthcare has been observed [2], in addition to process and clinical outcomes [3,4,5]. These so-called patient-reported outcome measures (PROMs) capture a person’s perception of their own health through standardized, validated questionnaires [6]. The main purpose of PROMs is to improve quality of care and provide more patient-centred care by quantifying important subjective outcomes, such as perceived quality of life and physical and psychosocial functioning.
For the purpose of quality improvement in healthcare, PROMs are used on a micro, meso and macro level. On a micro level, PROMs are useful screening and monitoring tools to facilitate shared decision-making and patient-centred care [7,8,9]. On a meso level, aggregated PROMs (i.e. PROM outcomes on the group level) provide analytical and organizational angles for improving and regulating health in specific populations as a result of enhanced understanding, self-reflection, benchmarking and comparison between healthcare professionals and practices [10,11,12]. At a macro level, PROMs are used for overall population surveillance and policy [2, 13, 14]. The use of structurally collected PROMs is increasingly adopted in national quality registries [15, 16], and it increased even further after the Organisation for Economic Co-operation and Development (OECD) recommended the collection of aggregated PROMs to obtain insight into system performance and to enable comparative analysis between practices [17].
The use of aggregated PROMs is a relatively young field. In 2018, Greenhalgh et al. showed that there was little empirical evidence that PROMs, at a meso level, led to sustained improvements in quality of care [18]. However, since then, there has been growing interest in this field, with a plethora of quantitative and qualitative research currently available. Therefore, the aim of this mixed-methods systematic review was threefold: (1) to summarize quality improvement methods based on aggregated PROMs at the meso level in hospital care; (2) to describe the effectiveness of quality improvement methods; and (3) to describe barriers, facilitators and lessons learned when using aggregated PROMs for quality improvement in healthcare.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used to design and report this review [19]. The review was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO) 07-12-2020 (PROSPERO 2020: CRD42020219408).
Search strategy
Embase, MEDLINE, CINAHL and the Cochrane Library were searched for studies published up to May 2021. The search strategy (Additional file 1: Appendix I) included terms related to outcome measurements, quality management and quality improvement. Search terms consisted of Medical Subject Headings (MeSH) and free-text words, wherein for most terms, synonyms and closely related words were included. The search was performed without date or language restriction. Additional references were obtained by hand-searching reference lists of included studies and systematic reviews (backwards selection) and by identifying studies that cited the original included studies (forward selection). Duplicate studies were removed.
Eligibility criteria
Studies were considered eligible for inclusion if they described, implemented or evaluated a quality improvement method based on aggregated PROMs in the curative hospital setting. Both quantitative and qualitative studies were included in this review. Quantitative studies included experimental study designs, such as randomized controlled trials, controlled trials, cluster trials, controlled before–after studies and time-series studies. Qualitative studies included semi-structured interviews, focus groups or studies with a mixed-methods approach (e.g. process evaluation studies). Studies were excluded for the following: (1) the quality improvement was based on the use of PROMs in the individual setting only (e.g. in the consultation room); (2) written in a language other than English; (3) not peer-reviewed; (4) conference and editorial papers and reviews; or (5) the full text could not be obtained.
Study selection
All records found were uploaded to Rayyan, an online web application that supports independent selection of abstracts [20]. Two researchers (KvH and MD) independently screened the titles and abstracts of the identified studies for eligibility. Discrepancies were resolved by discussion with the involvement of a third researcher (JJ) when necessary. Subsequently, full texts were screened against the eligibility criteria independently by two researchers (KvH and MD).
Data extraction and synthesis
Due to the mixed-methods design of this review, two researchers (KvH and MD) extracted data from qualitative and quantitative studies separately [21] using a standardized form. Details on the study design, aims, setting, sample size, quality improvement method, PROMs and outcomes were extracted and synthesized into a narrative summary. The described quality improvement methods were summarized, and when available, the effect of these methods was reported.
For the qualitative synthesis, the approach outlined by Thomas and Harden [22] was followed, which involved a thematic synthesis in the form of three stages: (1) free line-by-line coding of the findings performed by three researchers; (2) organization of these codes into related areas to construct descriptive themes; and (3) the development of analytical themes. A fourth researcher (MO) was consulted for verification and consensus. The qualitative synthesis was structured around facilitators, barriers and lessons learned for the implementation of quality improvement interventions based on PROM data. Finally, both quantitative and qualitative synthesis were combined in the discussion section.
Quality assessment
Study quality was assessed independently by two researchers (KvH and MD) with the validated Mixed Methods Appraisal Tool (MMAT) [23] informing the interpretation of findings rather than determining study eligibility. The MMAT is a critical appraisal tool that is designed for mixed-methods systematic reviews and permits us to appraise the methodological quality of five study designs: qualitative research, randomized studies, non-randomized studies, descriptive studies and mixed-methods studies. Aspects covered included (dependent on study design) quality of study design, randomization, blinding, selection bias, confounding, adherence and completeness of data. The MMAT does not provide a threshold for the acceptability of the quality of the studies [23].
Results
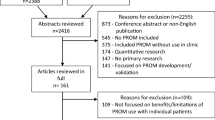
A flow diagram of the study selection process is presented in Fig. 1. A total of 3700 records were identified. After removing duplicates, 2360 records were screened on title–abstract, and 83 records were screened on full text. Three studies were found through hand searching [24,25,26]. Finally, 13 quantitative studies [24, 25, 27,28,29,30,31,32,33,34,35,36] and three qualitative studies [10, 11, 37] met the inclusion criteria. Research questions 1 and 2 are addressed in the “Quantitative studies” section, and research question 3 is addressed in the “Qualitative studies” section.
Quality of the studies
The quality assessment was performed according to study design: quantitative randomized [24, 28], quantitative non-randomized [25,26,27, 29, 30, 33, 34, 36], quantitative descriptive [31, 32, 35] and qualitative studies [10, 11, 37]. Five studies were assessed as good-quality studies, and the other 11 were assessed as moderate-quality studies. Neither randomized study was able to blind healthcare professionals to the intervention provided, although since receipt or non-receipt of feedback in these studies could not be disguised, this was not weighed as poor quality. Lack of complete outcome data was a shortcoming in five of the studies [24, 26, 29, 30, 33, 34]. In addition, for two descriptive studies [31, 35], it was not possible to assess response bias. The quality assessment can be found in Additional file 2: Appendix II.
Quantitative studies
Study characteristics
Table 1 summarizes the study characteristics of the 13 included quantitative papers. The search yielded two randomized controlled trials [24, 28], eight non-randomized controlled studies [25,26,27, 29, 30, 33, 34, 36] and three single-centre descriptive studies [31, 32, 35]. Studies were performed in the United States [24, 26, 27, 35], United Kingdom [30, 32, 34], Netherlands [25, 33], Sweden [31], Denmark [29], Canada [36] and Ireland [28]. Twelve studies focused on patients from surgical specialties, including orthopaedic [26, 28, 30, 32, 35], thoracic [29, 33], urologic [27, 36], ophthalmic [31], rhinoplastic [25] and general surgery [34]. One study focused on primary care [24]. In eight studies, data were obtained from a regional or national quality registry [27, 29,30,31,32,33,34,35]. The included studies used generic PROMs [30, 33], disease-specific PROMs [25, 27, 29, 31] or a combination of generic and specific PROMs [24, 26, 28, 32, 34,35,36].
Effect and impact
Only five out of 13 studies reported on the effect of quality improvement methods based on aggregated PROMs [24, 28, 32, 34, 36]. Four of these studies, including both randomized controlled trials, showed no effect [24, 28, 36] to a minimal effect [34] on patient-reported outcomes after the use of individual benchmarking as a quality improvement method (Table 1). One of the studies showed a significant improvement in the Oxford Knee Score after a plan-do-study-act (PDSA) cycle in a cross-sectional post-intervention cohort [32]. The other eight studies described the method of implementation without effect measurement [25, 27, 33, 35], or discussed (statistical) models for using aggregated outcomes as performance indicators [29,30,31].
Methods used to accomplish quality improvements
Four quality improvement methods were identified: benchmarking [24, 27,28,29,30, 34,35,36], PDSA cycles [32, 33], dashboards as feedback tool [25, 26] and internal statistical analysis [31] (Table 2).
Benchmarking
Benchmarking was applied in eight studies [24, 27,28,29,30, 34,35,36]. Aggregated data were used to provide peer-benchmarked feedback for individual healthcare professionals [24, 27, 28, 34, 36] or at a practice and individual level [35]. Two studies proposed different statistical models to use data as a performance indicator to benchmark surgical departments [29, 30]. Benchmarking was performed once [24, 27,28,29,30] or more frequently [34,35,36], and feedback was provided via web-based systems [27, 28, 34, 35], individual report cards [24, 36] or via a peer-reviewed study [29, 30]. When individual healthcare professionals were benchmarked, most studies used adjusted outcome information to provide fair comparisons between individual healthcare professionals [28,29,30, 34,35,36]. In addition to benchmarked feedback, two studies also provided individual healthcare professionals with educational support [24, 28]. Four of eight studies reported on the impact of benchmarking, all showing no clinical effect.
PDSA cycle
Two studies used a PDSA cycle to improve the quality of care [32, 33]. Van Veghel et al. (2014) reported on the establishment of an online transparent publication service for aggregated patient-relevant outcomes. Subsequently, these data enable benchmarking between Dutch heart centres to improve quality and efficiency. However, this study was not able to provide benchmarked patient-reported data due to a low response rate and a lack of data [33]. The study from Partridge et al. was a cross-sectional post-intervention study and compared their outcomes with a previously published report from the Health and Social Care Information Centre (HSCIC) from August 2011. A significant improvement in the Oxford Knee Score was found after changing the practice of care [32].
Dashboard as a feedback tool
Two studies used a web-based dashboard as a feedback tool [25, 26]. In the study by van Zijl et al. (2021), feedback was available through graphical analysis of patient characteristics and PROMs for individual rhinoplastic surgeons. The purpose of this dashboard was to identify learning and improvement needs or provide data-driven motivation to change concepts or surgical techniques [25]. In Reilly et al., a dashboard was established to consistently measure the value of total hip and total knee arthroplasty by combining surgeon-weighted PROMs, clinical outcomes and direct costs [26]. Neither study reported on the impact of these methods.
Aggregated statistical analysis
One study investigated how clinical outcome measures can be linked to PROMs and concluded that the following methods were most appropriate: (1) analysing the factors related to a good or poor patient-reported outcome, and (2) analysing the factors related to agreement or disagreement between clinical and patient-reported outcomes [31].
Qualitative studies
Study characteristics
Table 3 shows the study characteristics of the qualitative studies included in this research. All three studies comprised semi-structured interviews [10, 11, 37]. Interviews were conducted amongst experts from the United Kingdom [10, 11], US [11], Ireland [37], Sweden [10] and the Netherlands [11]. The study from Boyce et al. comprises the qualitative evaluation [37] of a randomized controlled trial, which is discussed in the quantitative section [28].
Barriers, facilitators and lessons learned
In the qualitative analysis, barriers, facilitators and lessons learned/neutral statements were derived and were grouped into the following three themes: (1) conceptual, (2) methodological and (3) practical (Table 4). The overview and description of the themes (i.e. codebook) with the occurrence of facilitators, barriers and lessons learned can be found in Table 4. The most important lessons learned for future implementation and research can be found in Table 5.
(1) Conceptual
The following four themes were derived: stakeholders, subjectivity of PROMs, aligning PROMS with clinical data, and PROMs versus patient-reported experience measures (PREMs). One facilitator for success that was mentioned was the engagement and commitment of stakeholders at both the meso and macro levels from the beginning [10, 11, 37]. Champions can advocate the added value of collecting PROMs, and governance and political will can be decisive for its success and sustainability [10, 37]. Healthcare providers differ in their attitudes regarding the usage of PROMs for quality improvements; some advocate for sceptics [37]. As a start, small-scale projects with willing clinicians is recommended instead of teams with limited interest or readiness [11].
These advocates often need to convince other healthcare professionals due to concerns about the scientific properties of PROM measures, in particular the subjective characteristics of these measures. Thus, healthcare professionals have underlying doubt about the patient’s ability to answer PROM questionnaires [10, 37]. Furthermore, difficult-to-accept discrepancies between the PROM outcome and the clinical experience from healthcare professionals' point of view were found, since expectations were that these two outcome measures would align [37]. Moreover, Boyce et al. (2018) found that healthcare professionals were not able to distinguish the difference between PROMs and measures of PREMs [37].
(2) Methodological
Within this main theme, a distinction was made between data collection (2a) and data processing (2b).
(2a) Data collection
The following four themes were derived: choice of measure, timing of data collection, response rate of measurement and focus of measurement. Patient-reported measures should be selected cautiously to be appropriate for the targeted population [37], to ensure comparability and to prevent burdening the patient [10, 11]. The combination of generic and disease-specific measures was seen as feasible and complementary [10, 11, 37], especially since generic measures facilitate good comparison, but are less able to detect variation [10]. Moreover, standardization of time points for data collection is advocated, as timing may influence the results [10]. For example, outcomes were measured during short-term follow-up when patients were not fully recovered [37]. Furthermore, to obtain high response rates, it is important to discuss the results of PROMs with the patient during consultation, especially during long-term follow-up [11]. Another reported barrier concerned the clinical value of performance measurement for interventions in a field where small variability a priori could be expected [37].
(2b) Data processing
Four themes were derived: representativeness of collected data, responsibility of healthcare professionals, inadequate case-mix control and interpretation of feedback.
It was mentioned that some healthcare professionals mistrusted quality improvement measures based on aggregated PROMs. First, the representativeness of the data used for benchmarking or quality improvement was seen as a barrier. Healthcare professionals expressed concern that the data would not reflect practice, the individual practitioner or the population of patients [10, 11, 37]. Furthermore, some patient groups were identified as a possible source of information and recall bias, such as patients with low health literacy or those with comorbidities who might confuse problems from one condition with another [37]. Additionally, patients’ answers might be influenced by their care expectations, with the belief that this information is used to rate care, or by the need to justify their decision to have an operation [10, 37]. Additionally, healthcare professionals may be tempted to manipulate data to obtain good performance rates by recruiting patients who are more likely to have good outcomes (i.e. selection bias) [10, 11, 37]. Second, healthcare professionals were afraid to be held unfairly responsible for outcome data that could be biased by differences in resources across hospitals [37], differences in support services at the community level [37] or factors that occurred outside of their control [10, 11]. Third, healthcare professionals worried that inadequate case-mix control of confounders would bias comparisons of healthcare providers. In addition, the lack of transparency of the statistical analysis made it difficult to engage with the data. Two solutions were provided to address these barriers: (1) only providing aggregated data collection for quality improvement at a very generic level, or (2) presenting results stratified into subgroups instead of risk- or case-mix adjustment [11]. Furthermore, healthcare professionals expressed difficulty in understanding the data, a lack of norms for good or poor performance [11], and a need for training or guided sessions to correctly interpret the aggregated PROM data [10, 37]. Quality improvement reports were able to identify how hospitals and healthcare professionals stand relative to one another, but they are often general and lack the ability to identify opportunities for real quality improvement or action [10], which is key for clinicians in engaging with data and processes [11].
(3) Practical
Statements related to practical implementation were grouped under “practical”.
One theme, resources, was derived. Funding to get the programmes started was seen as a key facilitator for further development in structural embedding in routine care. Overall, commitment and support from the government and healthcare organizations were seen as facilitators [10, 37]. The availability of resources for routine data collection and monitoring without disruption of workflow or additional workload was seen as important [10, 11, 37]. For example, the need for sufficient IT capacity and software to analyse the data enabled the data to be available quickly for healthcare professionals [10, 11, 37]. Additionally, the availability of tablets and assistance in the waiting room for completing questionnaires, the establishment of infrastructure for developing and disseminating annual reports [10], and the opportunity for data linkage and integration in hospital records were mentioned.
Discussion
The aim of this mixed-methods systematic review was to describe and investigate the experience and effectiveness of quality improvement methods based on aggregated PROMs. Four quality improvement methods were identified, including benchmarking, PDSA cycles, web-based dashboards as feedback tools, and the provision of aggregated statistical analysis reports. In total, 13 quantitative and three qualitative studies revealed that there is limited empirical evidence concerning quality improvements based on aggregated use of available PROMs. Only five studies reported on the effectiveness of the applied quality improvement method, and only one descriptive study reported a significant improvement of PROMs after implementation of aggregated PROM feedback. The qualitative studies identified that the belief of stakeholders, the use of generic and disease-specific PROMs, and the availability of funding and resources were important facilitators for success. One reported barrier was that sceptical healthcare professionals mistrusted the use of aggregated PROMs due to the subjectivity of PROMs and the contradictory results of PROMs and clinical outcomes. Furthermore, they were afraid to be held unfairly accountable for biased results as a result of case mix, differences in resources across hospitals, differences in support services at the community level or factors that occurred outside of their control. Lessons learned from the qualitative studies included creating shared stakeholder vision and that feedback on individual performance should be directed to individual healthcare professionals to learn from the outcomes of their own patients.
One quantitative study did find an effect of using aggregated PROMs in the PDSA cycle [32], and used specific facilitating factors to generate representative data, such as engagement of all stakeholders, the use of a combination of generic and disease-specific questionnaires, and obtainment of a high response rate. However, the results of this methodologically inferior cross-sectional post-intervention study should be interpreted cautiously.
Methodological and practical barriers were considered a reason for not finding an effect of benchmarking. Weingarten et al. suggested that no effect of peer-benchmarked feedback was found due to the choice of measure, since only one generic outcome measure (functional status) was used [24]. The themes timing of data collection and timing of feedback were mentioned as important barriers in the included quantitative studies as well; a follow-up measurement was taken too early after providing peer-benchmarked feedback [28], provision of feedback started too late in the study [34] or the authors mentioned that the duration of the intervention was too short to be fully adopted by all participating healthcare professionals [36]. Multiple studies had shortcomings in reporting on bias due to an insufficient response rate of the measurement. As PROMs are prone to missing data, it is important that studies adequately report on the completeness of data and take possible bias into account when drawing conclusions.
Another issue mentioned was the representativeness of the collected data, as some outcomes could not be linked to one specific surgeon, or low-volume surgeons were excluded from the analysis, which caused less variation [34]. Kumar et al. (2021) mentioned that the difficulty in feedback interpretation for healthcare professionals caused a lack of effect [36]. To improve understanding and interpretation, the use of training (e.g. statistics and visualization) and educational interventions was mentioned explicitly within the two randomized controlled trials addressing the quality improvement method of peer-benchmarked feedback [24, 28]. The importance of training was also addressed by the qualitative findings [10, 11, 37]. Previous research indicates that educational support is an important contextual factor for success in quality improvement strategies [38].
Additionally, the importance of good resources was mentioned in the discussion of the quantitative studies [24, 28, 34]. The importance of structural implementation was underlined by Varagunam et al. (2014), who stated that the small effect of the national PROMs programme was partly caused by the delay in the representation of the collected data.
Strengths and limitations
A major strength of this review is the mixed-methods design with the inclusion of overall moderate- to good-quality studies, which enabled a comprehensive overview of all available quantitative and qualitative research within this field. Furthermore, due to the mixed-methods design of this review, the quantitative findings were discussed in light of the derived qualitative barriers, facilitators and lessons learned. As a result of the lack of empirical research concerning quality improvement methods based on the aggregated use of PROMS, a meta-analysis was not performed. Additionally, it was purposively decided to include only peer-reviewed studies, and it is acknowledged that important studies from the grey literature may have been missed.
Future perspective
Future implementation of aggregated PROM feedback can be substantiated with the reported facilitators, barriers and lessons learned from the current review (Tables 4, 5). It is important that every institution using aggregated PROMs make their results available, including possible biases and completeness of outcome data. Furthermore, the strength of combining PROMs, clinical data and PREMs should be recognized. The use of aggregated clinical data and PREMs has already been shown to be effective in quality improvement [5, 39,40,41], while using aggregated PROMs for quality improvement is still in its infancy.
As qualitative outcomes mainly addressed the issue of obtaining accurate data and consequently gaining professionals’ trust in the concept and relevance of quality improvement, this research did not find best practices on how to learn and improve based on aggregated PROM data. Future research should focus on organizational and individual aspects that contribute to the optimal use of the obtained aggregated PROMs for quality improvement [42].
Conclusion
This review synthesized the evidence on the methods used and effectiveness for quality improvement in healthcare based on PROMs. The findings demonstrate that four quality improvement methods are used: benchmarking, PSDA cycles, dashboards and aggregated analysis. These methods showed little to no effect, which may be due to methodological flaws, as indicated by the qualitative results. In conclusion, this field of research is in its infancy, and more empirical research is needed. However, the descriptive and effectiveness findings provide useful information for the future implementation of value-based healthcare at the meso level and further quality improvement research. In future studies, it is important that a shared stakeholder vision is created, PROMs and timing of measurement and feedback are appropriately chosen, interpretation of the feedback is optimal, every effort is made to reduce missing data, and finally, practical resources for data collection and feedback infrastructure are available.
Availability of data and materials
Data collection forms and Rayyan extraction files can be obtained on request.
References
Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81.
Williams K, Sansoni J, Morris D, Grootemaat P, Thompson C. Patient-reported outcome measures. Lit Rev. 2016.
Shah A. Using data for improvement. BMJ. 2019;364: l189.
Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83:691–729.
Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard‐Jensen J, French SD, O'Brien MA, Johansen M, Grimshaw J, Oxman AD. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012.
Howell D, Molloy S, Wilkinson K, Green E, Orchard K, Wang K, Liberty J. Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol. 2015;26:1846–58.
Valderas JM, Kotzeva A, Espallargues M, Guyatt G, Ferrans CE, Halyard MY, Revicki DA, Symonds T, Parada A, Alonso J. The impact of measuring patient-reported outcomes in clinical practice: a systematic review of the literature. Qual Life Res. 2008;17:179–93.
Boyce MB, Browne JP. Does providing feedback on patient-reported outcomes to healthcare professionals result in better outcomes for patients? A systematic review. Qual Life Res. 2013;22:2265–78.
Damman OC, Jani A, Jong BA, Becker A, Metz MJ, Bruijne MC, Timmermans DR, Cornel MC, Ubbink DT, Steen M, et al. The use of PROMs and shared decision-making in medical encounters with patients: an opportunity to deliver value-based health care to patients. J Eval Clin Pract. 2020;26:524–40.
Prodinger B, Taylor P. Improving quality of care through patient-reported outcome measures (PROMs): expert interviews using the NHS PROMs Programme and the Swedish quality registers for knee and hip arthroplasty as examples. BMC Health Serv Res. 2018;18:87.
Van Der Wees PJ, Der Nijhuis-Van S, En MWG, Ayanian JZ, Black N, Westert GP, Schneider EC. Integrating the use of patient-reported outcomes for both clinical practice and performance measurement: views of experts from 3 countries. Milbank Q. 2014;92:754–75.
Wu AW, Kharrazi H, Boulware LE, Snyder CF. Measure once, cut twice–adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. J Clin Epidemiol. 2013;66:S12-20.
Sutherland HJ, Till JE. Quality of life assessments and levels of decision making: differentiating objectives. Qual Life Res. 1993;2:297–303.
Krawczyk M, Sawatzky R, Schick-Makaroff K, Stajduhar K, Öhlen J, Reimer-Kirkham S, Mercedes Laforest E, Cohen R. Micro-meso-macro practice tensions in using patient-reported outcome and experience measures in hospital palliative care. Qual Health Res. 2019;29:510–21.
Nilsson E, Orwelius L, Kristenson M. Patient-reported outcomes in the Swedish National Quality Registers. J Intern Med (GBR). 2016;279:141–53.
Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307:1583–4.
OECD. Recommendations to OECD Ministers of Health from the high level reflection group on the future of health statistics: strengthening the international comparison of health system performance through patient-reported indicators. 2017.
Greenhalgh J, Dalkin S, Gibbons E, Wright J, Valderas JM, Meads D, Black N. How do aggregated patient-reported outcome measures data stimulate health care improvement? A realist synthesis. J Health Serv Res Policy. 2018;23:57–65.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ Br Med J. 2015;349: g7647.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Research in the schools: a nationally refereed journal sponsored by the Mid-South Educational Research Association and the University of Alabama 2006; 13:29–29.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24:459–67.
Weingarten SR, Kim CS, Stone EG, Kristopaitis RJ, Pelter M, Sandhu M. Can peer-comparison feedback improve patient functional status? Am J Manag Care. 2000;6:35–9.
van Zijl F, Lohuis P, Datema FR. The Rhinoplasty Health Care Monitor: using validated questionnaires and a web-based outcome dashboard to evaluate personal surgical performance. Facial Plast Surg Aesthet Med. 2021.
Reilly CA, Doughty HP, Werth PM, Rockwell CW, Sparks MB, Jevsevar DS. Creating a value dashboard for orthopaedic surgical procedures. J Bone Joint Surg Am. 2020;102:1849–56.
Lucas SM, Kim TK, Ghani KR, Miller DC, Linsell S, Starr J, Peabody JO, Hurley P, Montie J, Cher ML. Establishment of a web-based system for collection of patient-reported outcomes after radical prostatectomy in a Statewide quality improvement collaborative. Urology. 2017;107:96–102.
Boyce MB, Browne JP. The effectiveness of providing peer benchmarked feedback to hip replacement surgeons based on patient-reported outcome measures–results from the PROFILE (Patient-Reported Outcomes: Feedback Interpretation and Learning Experiment) trial: a cluster randomised controlled study. BMJ Open. 2015;5: e008325.
Brønserud M, Iachina M, Green A, Grønvold M, Jakobsen E. P3.15-05 patient reported outcomes (PROs) as performance measures after surgery for lung cancer. J Thorac Oncol. 2018; 13:S992–S993.
Gutacker N, Bojke C, Daidone S, Devlin N, Street A. Hospital variation in patient-reported outcomes at the level of EQ-5D dimensions: evidence from England. Med Decis Making. 2013;33:804–18.
Lundström M, Stenevi U. Analyzing patient-reported outcomes to improve cataract care. Optom Vis Sci. 2013;90:754–9.
Partridge T, Carluke I, Emmerson K, Partington P, Reed M. Improving patient reported outcome measures (PROMs) in total knee replacement by changing implant and preserving the infrapatella fatpad: a quality improvement project. 2016.
van Veghel D, Marteijn M, de Mol B. First results of a national initiative to enable quality improvement of cardiovascular care by transparently reporting on patient-relevant outcomes. Eur J Cardio Thorac Surg. 2016;49:1660–9.
Varagunam M, Hutchings A, Neuburger J, Black N. Impact on hospital performance of introducing routine patient reported outcome measures in surgery. J Health Serv Res Policy. 2014;19:77–84.
Zheng H, Li W, Harrold L, Ayers DC, Franklin PD. Web-based comparative patient-reported outcome feedback to support quality improvement and comparative effectiveness research in total joint replacement. EGEMS (Wash DC). 2014;2:1130.
Kumar RM, Fergusson DA, Lavallée LT, Cagiannos I, Morash C, Horrigan M, Mallick R, Stacey D, Fung-Kee Fung M, Sands D, Breau RH. Performance feedback may not improve radical prostatectomy outcomes: the surgical report card (SuRep) study. J Urol. 2021:101097JU0000000000001764.
Boyce MB, Browne JP, Greenhalgh J. Surgeon’s experiences of receiving peer benchmarked feedback using patient-reported outcome measures: a qualitative study. Implement Sci. 2014;9:84.
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, Margolis P. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88:500–59.
Gleeson H, Calderon A, Swami V, Deighton J, Wolpert M, Edbrooke-Childs J. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open. 2016;6: e011907.
Bastemeijer CM, Boosman H, van Ewijk H, Verweij LM, Voogt L, Hazelzet JA. Patient experiences: a systematic review of quality improvement interventions in a hospital setting. Patient Relat Outcome Meas. 2019;10:157–69.
Haugum M, Danielsen K, Iversen HH, Bjertnaes O. The use of data from national and other large-scale user experience surveys in local quality work: a systematic review. Int J Qual Health Care. 2014;26:592–605.
Weggelaar-Jansen A, Broekharst DSE, de Bruijne M. Developing a hospital-wide quality and safety dashboard: a qualitative research study. BMJ Qual Saf. 2018;27:1000–7.
Acknowledgements
We would like to thank our consortium members P.J. van der Wees, M.M. van Muilekom, I.L. Abma, L. Haverman, C.T.B. Ahaus, H.J. van Elten, M. Leusder, H.F. Lingsma, N. van Leeuwen, E.S. van Hoorn and T.S. Reindersma for their contribution. We would also like to thank W.M. Bramer, biomedical information specialist from the Erasmus MC.
Funding
Ministry of Health, Welfare and Sport, The Netherlands.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly to the establishment of the manuscript, take full responsibility for the research reported and approve the submission of this manuscript. MD is the main author and conducted the search and review process together with KvH and JJ. MO, RBdJ and ED provided support and consultation during data extraction, qualitative analysis and review of the manuscript. MO and MdB supervised the study and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors hereby declare that there are no conflicts of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix I: Search strategy.
Additional file 2:
Appendix II: Quality appraisal of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dorr, M.C., van Hof, K.S., Jelsma, J.G.M. et al. Quality improvements of healthcare trajectories by learning from aggregated patient-reported outcomes: a mixed-methods systematic literature review. Health Res Policy Sys 20, 90 (2022). https://doi.org/10.1186/s12961-022-00893-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12961-022-00893-4