Abstract
Background
Across the care economy there are major shortages in the health and care workforce, as well as high rates of attrition and ill-defined career pathways. The aim of this study was to evaluate current evidence regarding methods to improve care worker recruitment, retention, safety, and education, for the professional care workforce.
Methods
A rapid review of comparative interventions designed to recruit, retain, educate and care for the professional workforce in the following sectors: disability, aged care, health, mental health, family and youth services, and early childhood education and care was conducted. Embase and MEDLINE databases were searched, and studies published between January 2015 and November 2022 were included. We used the Quality Assessment tool for Quantitative Studies and the PEDro tools to evaluate study quality.
Results
5594 articles were initially screened and after applying the inclusion and exclusion criteria, 30 studies were included in the rapid review. Studies most frequently reported on the professional nursing, medical and allied health workforces. Some studies focused on the single domain of care worker education (n = 11) while most focused on multiple domains that combined education with recruitment strategies, retention strategies or a focus on worker safety. Study quality was comparatively low with a median PEDro score of 5/10, and 77% received a weak rating on the Quality Assessment tool for Quantitative Studies. Four new workforce strategies emerged; early career rural recruitment supports rural retention; workload management is essential for workforce well-being; learning must be contextually relevant; and there is a need to differentiate recruitment, retention, and education strategies for different professional health and care workforce categories as needs vary.
Conclusions
Given the critical importance of recruiting and retaining a strong health and care workforce, there is an immediate need to develop a cohesive strategy to address workforce shortfalls. This paper presents initial evidence on different interventions to address this need, and to inform care workforce recruitment and retention.
Rapid Review registration PROSPERO 2022 CRD42022371721 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022371721
Similar content being viewed by others
Background
Care work refers to labour that focuses on the well-being or development of people, requiring skills in communication, interaction and evidence-based practice in healthcare and social care roles [1]. Key domains of the care economy include aged care, disability, healthcare, mental health, family care, youth services, early childhood education, indigenous services, rural health, drug and alcohol services and social housing [2]. Despite similar workforce needs and challenges faced by these sectors, individual services typically operate in silos [2] and people with multiple morbidities often present to several facilities. There is little collaboration across these industry sectors to address common problems relating to recruiting, supporting, and retaining the care workforce, to deliver high quality care. The workforce are increasingly required to innovate and improve services and adapt new technologies. Care workers also need to address the increasing divergence of consumer needs (including clients, patients family members and other informal carers) and ensure that consumers have a voice in their own care [3,4,5].
The COVID-19 pandemic highlighted the critical role of workers in the healthcare economy to global health security [6]. The healthcare economy is at the forefront of securing the health and well-being of citizens globally. A nation’s economy is dependent on a care workforce that is adequately resourced, supported, and remunerated [7]. The pandemic exacerbated pre-existing challenges in workforce recruitment, retention and burnout in the health and social care sectors [8,9,10,11]. There is evidence that many of these workforce issues are relevant across care economy sectors, particularly in relation to staffing levels, low staff morale and attrition [12,13,14].
There are several co-ordinated workforce strategies internationally (e.g., see https://www.england.nhs.uk/ournhspeople/) that have sought to establish more compassionate working environments in terms of staff well-being support and tackling discrimination. Many aim to strengthen workforce recruitment and retention through better job incentives, staff education, training and by ensuring worker safety [7]. Recruitment and retention strategies apply to the skilled, registered, and professional care workforces and the informal and unregistered workforce (care workers), in addition to volunteer and peer-support workforces.
World-wide, social care sectors have reported challenges in maintaining a professional care workforce [8,9,10, 15]. The care workforce has ample and growing employment opportunities, leading to high staff turnover with supply outstripping demand [3]. This increase in demand is a global trend [16] and particularly affects older care recipients in residential care settings, such as care homes. Staff burnout (a state of chronic stress and exhaustion plus chronic workplace stress that can lead to sickness and absence) is also a common, debilitating and a costly issue [17]. Career pathways across the care workforce and educational opportunities have not universally been addressed in a systematic way [6] to enable individuals to plan and sustain their contribution to professional practice.
Critical changes need to be made to foster future care economy prosperity and there is growing research literature, especially on the need to improve recruitment and retention of the care workforce. For example, the World Health Organisation (WHO) developed a guideline for increasing access to health professional workers and care workers in remote and rural areas through improved staff retention [18]. The WHO guidelines contained 17 recommendations pertaining to education, regulation, staff incentives and staff support. Sixteen recommendations had low or very low certainty of evidence, highlighting the need to develop a cohesive evidence-based strategy to address workforce shortfalls.
In addition to the WHO guidelines, a systematic review involving 34 studies and 58,188 participants evaluated interventions to assist recruitment of the professional healthcare workforce in rural and remote areas [18]. Aligned to WHO guidelines [19] for the professional care workforce, the systematic review found that optimisation of training pathways at both undergraduate and postgraduate levels was effective at improving retention. Together with other literature, there was evidence that retention was facilitated by preferential selection of university students from a rural background [20,21,22,23,24] and supporting rurally placed health professionals to take further education and training [25,26,27,28,29]. A narrative review by Beccaria et al. (2022) [30] showed the importance of attachment to place in retaining a sustainable care economy workforce. Rapid reviews by Moriarty (2019) [31] and Marafu (2019) [32] also highlighted the value of continuous professional development in workforce retention yet these were limited to the health sector.
With previous reviews limited to pre-COVID-19 pandemic literature, the aim of this rapid review was to present recent evidence (January 2015–November 2022) across care economy sectors, settings, and geographical regions to establish evidence-based strategies to improve professional workforce recruitment, retention, safety, and education. We also aimed to examine whether new approaches were aligned with the WHO guidelines on health workforce development, attraction, recruitment, and retention in rural and remote areas [19]. Our synthesis also provides a critical appraisal of opportunities for learning and improvement across care sectors to facilitate the adoption of effective cross-sector interventions and policies.
Methods
The rapid review, focussed on the professional care workforce, was prospectively registered with PROSPERO (PROSPERO 2022 CRD42022371721 https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022371721) and PRISMA [33, 34]. The approach was based on methods of Murad et al. (2017), who suggested how review results can be synthesised and the certainty of evidence estimated when a meta-analysis cannot be completed. Defining the care workforce can be a challenge [35]. For example, the line between direct and indirect care is often not made clear, where workers such as cleaners and chefs play an important but indirect role in care. In addition, for people receiving support to live in the community, unpaid care plays a crucial and often under-acknowledged role [10]. For this review, we examined the professional care workforce, defined as paid, educated, skilled workers providing direct care in home, community, hospital, residential aged care and other social service settings. We did not examine the literature on personal care assistants, nursing assistants or allied health assistants. The research question for the review was, what methods can improve the recruitment, retention, safety, and education of the professional care workforce?
Search strategy
This rapid review was conducted in Embase and MEDLINE. The search was be limited to studies published in English, and time limited to between January 2015 and November 2022 (refer to Appendix 1 for the full MEDLINE search strategy).
Inclusion and exclusion criteria
Inclusion criteria:
-
1.
“Consumer focused” care workforce professions or professionals, inclusive of but not limited to people paid to work in healthcare services, aged care, home care, community care, disability, rehabilitation, social housing or homelessness, early childhood education and care and child protection, drug and alcohol services, rural and remote care, mental health, family services, domestic violence or Indigenous health and social care.
-
2.
Interventions pertaining to recruitment, retention, safety, and education of the “client focused” professional care workforce.
-
3.
All forms of quantitative research with adequate data and information provided to ascertain results.
-
4.
Must include a comparator (pre–post, RCT against different interventions).
-
5.
English language articles.
-
6.
Studies published between the months of January 2015–November 2022.
Exclusion criteria:
-
1.
Professions or staff other than the direct “client focused” care workforce, as defined above.
-
2.
Unqualified, non-professional, unskilled or non-registered care workforce
-
3.
Peer support workers
-
4.
Pre-implementation, pilot, and feasibility studies of an intervention.
-
5.
Qualitative studies, opinion pieces, commentaries, editorials, and theses.
-
6.
Articles published prior to the year 2015.
Participants
The care workforce as defined in the inclusion criteria. This rapid review was focused on the qualified professional care workforce, and any patient, client, or consumer outcomes were not reported.
Interventions
Interventions involved the care workforce and related to staff recruitment, retention, safety, and education. Retention pertains to the longevity of a period of employment within the care workforce. Recruitment refers to the ability to fill vacant advertised positions. Safety pertains to all elements of working safely from the care workforce perspective. Examples pertain to occupational health and safety and include, for example, needle stick injuries, workplace violence, back injuries, burnout. Education is the ongoing education, training, and professional development of the care workforce. Included studies were required to have data and a comparator, for example, pre and post intervention data. Studies were excluded if they only described the pre-implementation phase of an intervention, or if they were a pilot or feasibility study, case report or descriptive summary.
Outcome
The primary outcome was interventions, policies and procedures designed to support, retain, and facilitate the professional, qualified care workforce and synthesise of the evidence from these outcomes.
Data extraction
Data from database searches were downloaded into Endnote, duplicates removed, then exported to Covidence. As per Rapid Review guidelines [36], two researchers conducted a pilot screening exercise using the same 30–50 abstracts to calibrate and test the review criteria, with discrepancies resolved by discussion and a review of the full text as required. One researcher then screened the titles and abstracts of all identified studies against the inclusion and exclusion criteria. Two researchers then conducted a second pilot exercise to review the full text articles, using the same 5–10 full text articles to ensure consistency, with discrepancies resolved by discussion. A researcher then reviewed the full texts of the articles to determine the final selection. The final selected articles also had their reference lists hand searched for any additional articles of interest.
Data extraction of full text included articles was completed by one reviewer and a second reviewer checked for correctness and completeness of extracted data, with discrepancies resolved by discussion. The Physiotherapy Evidence Database (PEDro) scale [37, 38] and the Quality Assessment Tool for Quantitative Studies (QATQS) [39] were used to analyse the quality of the included articles. We used PEDro, because it is a validated tool for objectively measuring the reliability and clinical usefulness of trials. The Canadian QATQS added more detail to the quality of public health investigations. Data extraction included details of the intervention (abbreviated TIDIER checklist), study characteristics, control group—population and primary outcome results, intervention quality scores.
Risk of bias and quality assessment
The PEDro scale [37, 38] items include: eligibility criteria specified; random allocation of subjects to groups; allocation concealment; similarity of groups at baseline regarding the most important prognostic indicators; blinding of all subjects; blinding of all therapists who administered the therapy or intervention; blinding of all assessors who measured at least one key outcome; measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups; all subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analysed by “intention to treat”; the results of between-group statistical comparisons are reported for at least one key outcome, and the study provides both point measures and measures of variability for at least one key outcome.
The Quality Assessment Tool for Quantitative Studies rated the methodological quality for each study based on selection bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts, intervention integrity and the analysis [39]. This assessment tool provides an overall rating of weak, medium, or high quality.
Data synthesis and analysis
A purpose-built Excel database was used to extract study characteristics, intervention details, outcome measures and risk of bias. A descriptive analysis was provided for interventions for each of the different care workforces, in addition a descriptive analysis was provided for each of the four intervention types. Meta-analysis was planned when two or more studies had heterogeneity with the following factors: discipline of the care workforce, the type of intervention, primary outcome of the intervention, and comparable follow-up period. Data for synthesis included primary outcomes which measure the intervention impact on care workforce recruitment, retention, safety, or education. When two or more studies met these criteria, Review Manager (RevMan) Version 5.4. was used to complete the meta-analysis based on the mean-difference and measures of variability.
Results
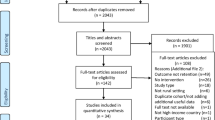
The initial search strategy resulted in 8343 studies, of which 2749 were duplicates. Following screening of title and abstracts, as well as full text, 30 studies were included [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69] (Fig. 1).
Study characteristics and results are detailed in Tables 1 and 2, respectively, noting that studies could report on more than one workforce intervention category. Studies most frequently reported on the nursing (n = 22), medical (n = 13) and allied health (n = 8) workforces (Fig. 2). Regarding the domains the intervention aimed to influence, some studies focused on the single domain of education (n = 11) [50, 51, 55, 57, 58, 62, 64] while most focused on multiple domains which combined education with recruitment, retention and/or safety. Seven studies included consumer engagement or co-design, as defined by McKercher et al. (2022) [5], while none of the studies included an economic evaluation. Meta-analysis was not appropriate due to the heterogeneity of the intervention, the included workforce, the setting, the study design, and the outcome measures.
PEDro scores for risk of bias ranged from 1 to 6 out of 10, with an average of 5 out of 10 (Appendix 2). Only two studies used randomisation [49, 58] and none reported blinding of participants or assessors, or allocation concealment. Most investigations reported on the remaining criteria. Study quality was comparatively low with 23/30 of the studies receiving a weak rating on the Quality Assessment tool for Quantitative Studies, with the remaining receiving a moderate rating (Appendix 3). Studies were most often weak for blinding (n = 23), cofounders (n = 18), and data collection methods (n = 16).
While the included articles often reported multiple domains that the intervention aimed to influence, the following paragraphs are based on the primary outcome domains.
Education
For the 24 studies with a primary focus on a care workforce education program, there were marked variations in the education interventions provided (e.g., leadership development, condition-based education programs, extending scope of practice), the location (e.g., USA, Australia, East Africa), the setting (e.g., hospitals, aged care, primary care), and the outcome measures used. As shown in Tables 1 and 2, both validated and unvalidated measurement tools were to measures the change in workforce knowledge [40,41,42,43,44,45,46, 48,49,50,51,52, 55,56,57,58,59,60,61,62, 64,65,66,67]. Of the 24 studies, only two used a randomised controlled trial design, [49, 58] with the rest using a pre–post study design. Only four did not report a significant improvement in staff knowledge. The education included topics, such as cancer education [56], obesity management, [57] simulation training for a breast examination, [58] leadership development, [67], and clinical nursing skills [66].
Of the six studies that included consumer engagement and co-design, all reported benefits. These investigations reported significant improvements in staff knowledge relating to topics, such as electronic health record implementation, [50] dementia care, [51] smoking cessation, [55] care-giver centred care, [62] cancer survivorship, [64] and paediatric nursing [65]. Of the five education studies that focused on the rural workforce, all reported a significant improvements. This pertained to staff knowledge related to midwifery, [41] non-physician extended scope of practice, [49] leadership development, [67] smoking cessation, [55] and cancer survivorship [64].
Of the 24 education investigations, 18 were conducted in high income countries, [40, 43,44,45,46, 50,51,52, 55,56,57, 59,60,61, 64, 66, 67] and six were conducted in low-to-low–middle income countries, [41, 42, 48, 49, 58, 65]. Of the four studies that did not demonstrate significant findings, three were based on the USA (high income country) and aimed to improve cancer knowledge, [57] nursing leadership, [60], and care workforce needs during COVID-19 [66]. One was based on Rwanda and focussed on low and high fidelity medical education for clinical breast examination. Both groups showed improvements in knowledge, yet there were no between group differences [58].
Recruitment and retention
Two studies reported on interventions that focused on rural workforce recruitment and retention, and both were conducted in Australia (high income country) [20, 63]. The first was on the Training for Health Equity Network (THEnet) to improve staff recruitment into the rural medical workforce. This did not report an increase in the proportion of learners intending to practice in rural areas [54]. The study was directed towards allied health and nursing students completing a rural placement in their final year of study [63]. The authors reported a significant association between the number of weeks of rural placement in the final year of study, and initial rural recruitment. However, the significant association reported for recruitment was not maintained for retention 15–17 years later [63].
Safety
Three investigations reported on safety relating to staff mental health and well-being [53, 68, 69]. These showed a significant improvement in primary outcomes. These included an increase in well-being and satisfaction following the introduction of the electronic medical record for the nursing workforce in Australia (high income country), [53] an increase in coping skills following the Helping Health Workers Cope program for the rural health and nursing workforce in West Africa (Sierra Leone; low income country), [68] and a reduction in perceived stress following the introduction of a triage and disinfection protocol for the medical, nursing and allied health workforce in South Sudan (low income country) [69]. There was an additional study the focussed on minimum nurse-to-patient ratios with the rational of improving patient safety. While this reported a significant improvement in the nurse to patient ratios following the introduction of staffing mandates, it did not specifically report the impact on patient safety (conducted in USA; high income country) [47].
Four effective evidence-based strategies from this rapid review have been established to add to the current literature base and improve professional workforce recruitment, retention, safety, and education. Where appropriate, it has been noted when the strategy is aligned to the WHO guideline on health workforce development, attraction, recruitment and retention in rural and remote areas [19].
Strategy 1 (recruitment and retention)
To support long term retention, implement strategies to recruit early career staff, especially to rural locations.
-
a.
New evidence from this rapid review: As the location of nursing and allied health practice in the first year post-graduation is a significant predictor for retention and the location of practice 15 + year post-graduation, there is a need to implement strategies to recruit professionals to rural locations, especially in the first year of practice.
-
b.
Alignment to WHO guidelines: “WHO recommends using targeted admission policies to enrol students with a rural background in health worker education programmes” [19] and “WHO recommends exposing students of a wide array of health worker disciplines to rural and remote communities and rural clinical practices” [19]
Strategy 2 (safety)
To support health professional mental and physical well-being, implement strategies for workload management alongside safety training and psychological support.
-
a.
New evidence from this rapid review: Optimising workload management can improve health professional health and well-being. Examples include an effective triage process [69], workload management using streamlined electronic medical records [53], and implementing staff to client ratio mandates [47].
-
b.
Alignment to WHO guidelines: “WHO recommends ensuring a safe and secure working environment for health workers …” [19]
Strategy 3 (education)
To maximise learning, ensure that health professionals have access to contextually relevant and ongoing professional development to improve capabilities and professional knowledge.
-
a.
New evidence from this rapid review: Contextually relevant professional education and development improves staff retention by focussing on staff needs, interventions relevant to the care setting, the patient population, cultural considerations, as well as providing evaluations of the impact of the new knowledge and skills.
-
b.
Aligned to WHO guidelines: “WHO recommends designing and enabling access to continuing education and professional development programmes that meet the needs of … workers to support their retention …” [19]
Strategy 4 (align recruitment and retention strategies to workforce categories)
There is a need to differentiate recruitment, retention and education strategies for different professional health and care workforce categories as needs vary.
-
a.
New evidence from this rapid review: Contextually relevant education, training and support needs to be matched to specific requirements of different professions, such as nursing, allied health and medicine. Non-registered, non-credentialed care workers may have different learning needs and interventions need to be tailored accordingly [70].
Discussion
From this rapid review, four new workforce strategies emerged; early career rural recruitment supports rural retention; workload management is essential for workforce well-being; learning must be contextually relevant; and there is a need to differentiate recruitment, retention and education strategies for different professional health and care workforce categories because needs vary. The care economy is one of the most rapidly growing sectors in the world and significant workforce shortages are predicted [3, 16]. The International Centre on Nurse Migration (2022), recommends the implementation of national and international action plans to improve care workforce recruitment and retention, supported by high-quality, large-scale research trials [71]. Trials are needed to measure the impact and outcomes of interventions to address issues, such as workforce demand–supply gaps, staff burnout and how to enhance work satisfaction. A recurrent theme in the articles reviewed was that staff education is a powerful determinant of these elements. Education was evaluated in most trials and other interventions included leadership training, mental health support for workers and training in the use of new technologies to support care delivery. Digital innovations, care delivery simulations, and implementation of electronic medical records improved worker satisfaction. Another theme was the need to establish a considered, co-ordinated, responsive, co-designed approach to support the care workforce and to maximise workforce recruitment, retention, safety, career progression and knowledge.
Consistent with Randell et al. (2021) [72], no global investigations were identified that provided a world-wide approach to coordinated workforce recruitment, retention, and enhancement. Each of the studies reviewed was site-specific and directed towards local needs and priorities. There was no clear pattern as to the impact of the economic status of the different countries on care workforce recruitment, retention, knowledge or safety. Many of the trials had similar designs and findings, yet they lacked the scale or reach across care economy domains to have a sustained impact nationally or globally. Of concern, most were of low methodological quality and only a few were of moderate quality. Our review also highlighted minimal involvement of consumers of health and social care services in the co-design of research or services. The economic evaluations of care workforce interventions were not reported.
A previous systematic review [4] showed low poor levels of care worker recruitment, as well as burnout and high staff turnover in the child welfare sector. These problems were related to personal factors, such as low levels of commitment to welfare, as well as emotional exhaustion in some people, and organisational factors, such as poor supervision and low co-worker support. Low salaries and benefits were also important elements that influenced decisions by child welfare workers to stay in the field. The emotional labour of working with people with poor health and other distressing circumstances was associated with fatigue and burnout. Job-related stress was associated with high workloads, combined with time pressures and ambiguous roles [73]. The current review also reiterated that most research has been focused on health, with social care largely overlooked, despite indications of increasing demands including global demographic trends projecting reduced availability of informal carers and growing need for long-term care for elderly people [74,75,76].
Our findings are congruent with Johnston’s rapid review on staff recruitment, retention, and development in the social care domain [77]. In addition the results align with the Australian National Care and Support Workforce Strategy (2022) [3] which identified five principles to support a strong workforce: target migration, activate and coordinate industry, remove barriers, skill up workers and use data to drive change. Across the care economy there is a need to attract people from diverse backgrounds, including migrants, youth and older women returning to the workforce, to meet the growing needs of diverse populations. Education and training of staff is central to retention, as is designing safe work environments and enabling attractive career pathways, supported by programs that include care provider well-being. A recent practical inquiry about attracting young people, particularly young indigenous people, into care work found that strategies of engagement were central and essential to interest them. There was also a need to identify specific care roles for which they were suited, preparing them for those roles and retaining them in that workforce [78].
Our review indicated that industry could play a pivotal role in removing barriers to care worker recruitment, retention, education and safety. The actions of care organisations and companies are influenced by key legislative drivers and those operating in the care economy sector are not immune. In the UK and Australia legislation has been adopted to combat forced labour and uphold decent working conditions. The Modern Slavery Act (2018) [79] requires companies with annual turnover in excess of $100m to report against risks in their supply chains and operations that signify significant risks in the employment of workers. Moreover, the United Nations Sustainable Development Goals (Sustainable Development Goals, 2021 [80]) of which Australia and many countries are signatories, pertain to decent work, economic growth, full and productive employment and equal pay for work of equal value. Companies and organisations are increasingly reporting on labour issues, including discrimination, human resource management, working conditions, industrial relations, and occupational health and safety [81]. Even through organisations and companies operating in the care economy arguably have less normative and regulatory pressures to adopt such practices compared to those operating in high-risk settings, such as mining and energy, the advent of legislation may increase such pressures across the sector. As the health and social care sectors are finding themselves under pressure to recruit qualified workers, recruitment and retention are likely to be influenced by how company actions are perceived by potential workers. Workers have many options for employment due to shortage of labour that followed the impact of COVID-19 restrictions, and they expect their employers to abide by legislation, and to act ethically in terms of their employment practices. Health and social care organisations are increasingly recognising the strong link between care worker well-being and safe and high-quality services [82].
When reviewing the literature, it became clear that specific strategies are needed for different health and care categories. The current manuscript focused on professional, qualified care workforces, such as nurses, doctors and allied health professionals, who have already spent many years in education and training to prepare them for their roles. Other members of the care workforce such as peer support workers, volunteers, personal care attendants, allied health assistants and nursing assistants have different needs for training in the workplace [70, 83, 84]. For example, over 50% of personal care attendants and 37% of aged care and disability workers are non-English speaking migrants [85]. There is emerging evidence of poor job quality for this cohort of workers, with a survey of 16,000 residential and community care workforce reporting predominantly casual status and underemployment [86]. Education, training, policies and systems need to take into account the needs of different workforce sectors, as recommended by recent reports [87, 88].
There are several limitations of this rapid review. The focus was over 8 recent years, and relevant studies outside of this time period were excluded. The search strategy also excluded studies published in languages other than English, and may have overlooked meaningful cultural contexts [89]. We also excluded qualitative studies, which can provide data to better understand the experiences of care workers and organisations. Future studies need to include a sector specific analysis of care workforce needs and recommendations.
Conclusion
With the growing importance of the care workforce and predicted long term global shortages exacerbated by ageing populations, evidence-based strategies to recruit and retain workers are vital. The growing and increasingly diverse workforce within the care economy requires attention to improve the quality of care for consumers and the service systems they access. Efforts to support the well-being and retention of care workers need to include the voice and lived experience of consumers, be sustainable and based on evidence. Recruiting a more diverse workforce, ensuring worker well-being and safety, and providing education and career development are essential to meet the current and future needs of the care economy.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Dwyer RE. The care economy? Gender, economic restructuring, and job polarization in the US labor market. Am Sociol Rev. 2013;78(3):390–416.
Macklin. Future Skills for Victoria, Driving collaboration and innovation in post-secondary education and training. 2020.
Job Skills Australia. Australian Government Workforce Australia National Care and Support Workforce Strategy https://www.labourmarketinsightsgovau/occupation-profile/social-workers?occupationCode=2725#outlook. 2008.
DePanfilis D, Zlotnik JL. Retention of front-line staff in child welfare: a systematic review of research. Child Youth Serv Rev. 2008;30(9):995–1008.
McKercher JP, Slade SC, Jazayeri JA, Hodge A, Knight M, Green J, et al. Patient experiences of codesigned rehabilitation interventions in hospitals: a rapid review. BMJ Open. 2022;12(11): e068241.
Buchan J, Catton H, Shaffer F. Sustain and Retain in 2022 and Beyond: The global nursing workforce and the COVID-19 pandemic. Philadelphia, USA: International Centre on Nurse Migration. 2022.
Eckert M. COVID-19-nurses and midwives impact on global security. AJAN Aust J Adv Nurs. 2020;37(2).
Gilster SD, Boltz M, Dalessandro JL. Long-term care workforce issues: practice principles for quality dementia care. Gerontologist. 2018;58(1):S103–13.
Campbell J, Koca F. Financing and protection for the health and care workforce. Bull World Health Organ. 2021;99(1):2.
Birchall J, Holt A. Who cares? The grandmother kinship carers shouldering the burden within a gendered care economy. J Women Aging. 2022:1–11.
Foster. Adult social care workforce in England. https://www.commonslibraryparliamentuk/research-briefings/cbp-9615/. 2022.
Douglas K, editor 1. Demanding labour: How essential disability support workers are marginalised in Australian industrial relations. Decent Work or Decent Income; 2021: Rainer Hampp Verlag.
Eagar K, Westera AB, Snoek M, Kobel C, Loggie CL, Gordon R. How Australian residential aged care staffing levels compare with international and national benchmarks. 2019.
Fenech M, Wong S, Boyd W, Gibson M, Watt H, Richardson P. Attracting, retaining and sustaining early childhood teachers: an ecological conceptualisation of workforce issues and future research directions. Aust Educ Res. 2022;49(1):1–19.
Dromey J, Hochlaf D. Fair care: A workforce strategy for social care. Institute for Public Policy Research. 2018.
Truell R. Social work is booming worldwide–because it’s proven to work. The Guardian. 2018.
Prasad K, McLoughlin C, Stillman M, Poplau S, Goelz E, Taylor S, et al. Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35: 100879.
Russell D, Mathew S, Fitts M, Liddle Z, Murakami-Gold L, Campbell N, et al. Interventions for health workforce retention in rural and remote areas: a systematic review. Hum Resour Health. 2021;19(1):1–24.
WHO. WHO guideline on health workforce development, attraction, recruitment and retention in rural and remote areas. World Health Organization Geneva; 2021.
Johnson G, Byun R, Foster K, Wright F, Blinkhorn A. A longitudinal workforce analysis of a Rural Clinical Placement Program for final year dental students. Aust Dent J. 2019;64(2):181–92.
Carson DB, Schoo A, Berggren P. The ‘rural pipeline’ and retention of rural health professionals in Europe’s northern peripheries. Health Policy. 2015;119(12):1550–6.
Kwan MMS, Kondalsamy-Chennakesavan S, Ranmuthugala G, Toombs MR, Nicholson GC. The rural pipeline to longer-term rural practice: general practitioners and specialists. PLoS ONE. 2017;12(7): e0180394.
McGrail MR, Russell DJ, Campbell DG. Vocational training of general practitioners in rural locations is critical for the Australian rural medical workforce. Med J Aust. 2016;205(5):216–21.
Playford D, Ngo H, Atkinson D, Puddey IB. Graduate doctors’ rural work increases over time. Med Teach. 2019;41(9):1073–80.
Murray MF, Havener J-M, Davis PS, Jastremski C, Twichell ML. The rural pipeline: building a strong nursing workforce through academic and service partnerships. Nurs Clin. 2011;46(1):107–21.
Nilsen G, Huemer J, Eriksen L. Bachelor studies for nurses organised in rural contexts–a tool for improving the health care services in circumpolar region? Int J Circumpolar Health. 2012;71:1–8.
Norbye B, Skaalvik MW. Decentralized nursing education in Northern Norway: towards a sustainable recruitment and retention model in rural Arctic healthcare services. Int J Circumpolar Health. 2013;72:22793.
Gorsche RG, Woloschuk W. Rural physicians’ skills enrichment program: a cohort control study of retention in Alberta. Aust J Rural Health. 2012;20(5):254–8.
Woolley T, Sen Gupta T, Bellei M. Predictors of remote practice location in the first seven cohorts of James Cook University MBBS graduates. Rural Remote Health. 2017;17(1):3992.
Beccaria L, McIlveen P, Fein EC, Kelly T, McGregor R, Rezwanul R. Importance of attachment to place in growing a sustainable Australian Rural Health Workforce: a rapid review. Aust J Rural Health. 2021;29(5):620–42.
Moriarty J, Steils N, Manthorpe J, Calder RI, Martineau SJ, Norrie CM, et al. Rapid review on the effectiveness of continuing professional development in the health sector. 2019.
Marufu TC, Collins A, Vargas L, Gillespie L, Almghairbi D. Factors influencing retention among hospital nurses: systematic review. Br J Nurs. 2021;30(5):302–8.
Sarkis-Onofre R, Catalá-López F, Aromataris E, Lockwood C. How to properly use the PRISMA statement. Syst Rev. 2021;10(1):1–3.
Tricco A, Lillie E, Zarin W, O’Brien K, Colquhoun H, Levac D, Tunçalp Ö, Straus SE, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. 2018;169(7):467–73.
Birch E, Preston A. The Australian labour market in 2020. J Ind Relat. 2021;63(3):303–20.
Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22.
Moseley AM, Rahman P, Wells GA, Zadro JR, Sherrington C, Toupin-April K, et al. Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: a meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE. 2019;14(9): e0222770.
Moseley A, Szikszay T, Lin C-W, Mathieson S, Elkins M, Herbert R, et al. A systematic review of the measurement properties and usage of the Physiotherapy Evidence Database (PEDRO) scale. Physiotherapy. 2015;101: e1043.
Thomas B, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs. 2004;1(3):176–84.
Abdulla E, Johnson J, Munir S, O’Dwyer R. Assessing primary health care nurses’ knowledge toward immunizations: a quantitative study. J Public Health Res. 2020;9(4):381–7.
Alwy Al-Beity F, Pembe AB, Marrone G, Baker U, Hanson C. Predictors of change of health workers’ knowledge and skills after the Helping Mothers Survive Bleeding after Birth (HMS BAB) in-facility training in Tanzania. PLoS ONE. 2020;15(5): e0232983.
Ayisi-Boateng NK, Sarfo FS, Opoku DA, Nakua EK, Konadu E, Tawiah P, et al. Educational intervention to enhance the knowledge of Ghanaian health workers on Alzheimer’s disease and related dementias. Afr. 2022;14(1):e1–7.
Azoulay D, Eshkenazy R, Pery R, Cordoba M, Haviv Y, Inbar Y, et al. The impact of establishing a dedicated liver surgery program at a university-affiliated hospital on workforce, workload, surgical outcomes, and trainee surgical autonomy and academic output. Ann Surg. 2021.
Bennett P, Burns R, Champion S, Gordon S. Effectiveness of an aged simulation training suit to support development of compassion and person-centred care in the aged-care workforce. Australas J Ageing. 2022;41(2):314–24.
Chicoine G, Cote J, Pepin J, Dyachenko A, Fontaine G, Jutras-Aswad D. Improving the self-efficacy, knowledge, and attitude of nurses regarding concurrent disorder care: results from a prospective cohort study of an interprofessional, videoconference-based programme using the ECHO model. Int J Mental Health Nurs. 2022;27.
Clancy EM, McIntosh J, Booth AT, Sheen J, Johnson M, Gibson T, et al. Training maternal and child health nurses in early relational trauma: an evaluation of the MERTIL workforce training. Nurse Educ Today. 2020;89: 104390.
Dierkes A, Do D, Morin H, Rochman M, Sloane D, McHugh M. The impact of California’s staffing mandate and the economic recession on registered nurse staffing levels: a longitudinal analysis. Nurs Outlook. 2022;70(2):219–27.
Downing J, Batuli M, Kivumbi G, Kabahweza J, Grant L, Murray SA, et al. A palliative care link nurse programme in Mulago Hospital, Uganda: an evaluation using mixed methods. BMC Palliative Care. 2016;15(1).
Gajewski J, Cheelo M, Bijlmakers L, Kachimba J, Pittalis C, Brugha R. The contribution of non-physician clinicians to the provision of surgery in rural Zambia-a randomised controlled trial. Hum Resour Health. 2019;17(1):60.
Gordon JE, Belford SM, Aranguren DL, Blair D, Fleming R, Gajarawala NM, et al. Outcomes of Mayo Clinic reBoot camps for postimplementation training in the electronic health record. J Am Med Inform Assoc. 2022;29(9):1518–24.
Islam MM, Parkinson A, Burns K, Woods M, Yen L. A training program for primary health care nurses on timely diagnosis and management of dementia in general practice: an evaluation study. Int J Nurs Stud. 2020;105: 103550.
Jafari P, Kostas T, Levine S, Martinchek M, Johnson D, Graupner J, et al. ECHO-Chicago Geriatrics: using telementoring to “geriatricize” the primary care workforce. Gerontol Geriatr Educ. 2020;41(3):333–41.
Jedwab RM, Hutchinson AM, Manias E, Calvo RA, Dobroff N, Redley B. Change in nurses’ psychosocial characteristics pre- and post-electronic medical record system implementation coinciding with the SARS-CoV-2 pandemic: pre- and post-cross-sectional surveys. Int J Med Inf. 2022;163:104783.
Johnston K, Guingona M, Elsanousi S, Mbokazi J, Labarda C, Cristobal FL, et al. Training a fit-for-purpose rural health workforce for low- and middle-income countries (LMICs): how do drivers and enablers of rural practice intention differ between learners from LMICs and high income countries? Front. 2020;8: 582464.
Martin K, Dono J, Stewart HB, Sparrow A, Miller C, Roder D, et al. Evaluation of an intervention to train health professionals working with Aboriginal and Torres Strait Islander people to provide smoking cessation advice. Aust N Z J Public Health. 2019;43(2):156–62.
Mikolajczyk AE, Zilberstein N, McConville JF, Pan A, Aronsohn AI, Te HS, et al. Mandatory hepatology education for internal medicine residents: long-term effects and implications for workforce needs. Hepatol. 2021;5(11):1953–63.
Morshed AB, Ballew P, Elliott MB, Haire-Joshu D, Kreuter MW, Brownson RC. Evaluation of an online training for improving self-reported evidence-based decision-making skills in cancer control among public health professionals. Public Health. 2017;152:28–35.
Murthy SS, Ntakiyiruta G, Ntirenganya F, Ingabire A, Defregger SK, Reznor G, et al. A randomized cross-over trial focused on clinical breast exam skill acquisition using high fidelity versus low fidelity simulation models in Rwanda. J Surg Educ. 2020;77(5):1161–8.
Neikrug AB, Stehli A, Xiong GL, Suo S, Le-Bucklin KV, Cant W, et al. Train new trainers primary care psychiatry fellowship-optimizing delivery of behavioral health care through training for primary care providers. J Contin Educ Health Prof. 2022;42(2):105–14.
Ortega J, Hooshmand M, Foronda C, Padron M, Simon D, Waters M, et al. Developing nurse leaders across the Americas: evaluation of an online nursing leadership course. Revista Panamericana de Salud Publica/Pan American Journal of Public Health. 2018;42 (no pagination).
Ortega Vega M, Williams L, Saunders A, Iannelli H, Cross S, Attoe C. Simulation training programme to improve the integrated response of teams in mental health crisis care. BMJ Simul Technol Enhanc Learn. 2021;7(2):116–8.
Parmar JK, L’Heureux T, Anderson S, Duggleby W, Pollard C, Poole L, et al. Optimizing the integration of family caregivers in the delivery of person-centered care: evaluation of an educational program for the healthcare workforce. BMC Health Serv Res. 2022;22(1):364.
Playford D, Moran MC, Thompson S. Factors associated with rural work for nursing and allied health graduates 15–17 years after an undergraduate rural placement through the University Department of Rural Health program. Rural Remote Health. 2020;20(1):5334.
Risendal B, Westfall JM, Zittleman L, Hodgson C, Garrington T, Sutter C, et al. Impact of cancer survivorship care training on rural primary care practice teams: a mixed methods approach. J Cancer Educ. 2022;37(1):71–80.
Salehi R, Asamoah A, de Young S, Acquah H, Agarwal N, Aryee SE, et al. Scaling up pediatric nurse specialist education in Ghana—a longitudinal, mixed methods evaluation. BMC Nurs. 2021;20(1):32.
Sibrian J, Hutapea K, Dunbar GB, Kawar LN. A virtual world: new graduate education in the era of COVID-19. J Contin Educ Nurs. 2022;53(7):307–11.
Tran AN, Nevidjon B, Derouin A, Weaver S, Bzdak M. Reshaping nursing workforce development by strengthening the leadership skills of advanced practice nurses. J Nurses Prof Dev. 2019;35(3):152–9.
Vesel L, Waller K, Dowden J, Fotso JC. Psychosocial support and resilience building among health workers in Sierra Leone: interrelations between coping skills, stress levels, and interpersonal relationships. BMC Health Serv Res. 2015;15(Suppl 1):S3.
Zhang Y, Xiang D, Alejok N. Coping with COVID-19 in United Nations peacekeeping field hospitals: increased workload and mental stress for military healthcare providers. BMJ Military Health. 2021;167(4):229–33.
Murphy C, Turner T. Formal and informal long term care work: policy conflict in a liberal welfare state. Int J Sociol Soc Policy. 2017;37(3/4):134–47.
International Centre on Nurse Migration. THE GLOBAL NURSING WORKFORCE AND THE COVID-19 PANDEMIC. https://www.icnch/system/files/2022-01/Sustain%20and%20Retain%20in%202022%20and%20Beyond-%20The%20global%20nursing%20workforce%20and%20the%20COVID-19%20pandemicpdf. 2022.
Randell R. Recruitment and retention of care workers: A rapid review. https://www.bradscholarsbradacuk/handle/10454/19006. 2021.
Hussein S, Turnpenny A. Recruitment and retention of the social care workforce: longstanding and emerging challenges during the COVID-19 pandemic. Recruitment and retention of the social care workforce: longstanding and emerging challenges during the COVID-19 pandemic. 2020.
Colombo F, Llena-Nozal A, Mercier J, Tjadens F. Help wanted. Ageing Long-term Care. 2011;17(2–3):3.
Edwards D, Trigg L, Carrier J, Cooper A, Csontos J, Day J, et al. A rapid review of innovations for attraction, recruitment and retention of social care workers, and exploration of factors influencing turnover within the UK context. J Long-Term Care. 2022:205–21.
Commission E, Committee SP. Long-Term Care Report. Trends, Challenges and Opportunities in an Ageing Society. https://www.ifsw.org/wp-content/uploads/2021/07/KE-09-21-202-EN-N-1.pdf. https://www.pssru.ac.uk/resscw/f: Publications Office of the European Union Luxembourg; 2021.
Johnston, McCartan, Davidson, Webb. A rapid review of the international evidence on the most effective approaches to staff recruitment, development and retention in social care. http://www.praxiscareorg/wp-content/uploads/2022/08/Workforce-rapid-review_10-08-22pdf. 2022.
Billett, Millichap, Meyer. Health Education to Employment Pathways Program. Queensland Health. 2022.
Australian Government. Modern Slavery Act. 2018, No 153, 2018, Federal Register of Legislation. https://www.legislationgovau/Details/C2018A00153/Download. 2018.
Moussa T, Allam A, Elmarzouky M. Global modern slavery and sustainable development goals: does institutional environment quality matter? Bus Strateg Environ. 2022;31(5):2230–44.
Young S, Marais M. A multi-level perspective of CSR reporting: the implications of national institutions and industry risk characteristics. Corp Gov. 2012;20(5):432–50.
Safer Care Victoria. Running on empty: practical ways to support a depleted workforce. https://www.safercarevicgovau/news/running-on-empty-practical-ways-to-support-a-depleted-workforce#:~:text=Jo%20said%20there%20is%20also,mental%20health%20and%20lower%20stress. 2022.
Huglin J, Whelan L, McLean S, Greer K, Mitchell D, Downie S, et al. Exploring utilisation of the allied health assistant workforce in the Victorian health, aged care and disability sectors. BMC Health Serv Res. 2021;21:1–12.
Miller VJ, Maziarz L, Wagner J, Bell J, Burek M. Nursing assistant turnover in nursing homes: a scoping review of the literature. Geriatr Nurs. 2023;51:360–8.
Statistics ABo. Labour Force, Australia 2018. Available from: https://www.abs.gov.au/statistics/labour/employment-and-unemployment/labour-force-australia/latest-release.
Mavromaras K, Knight G, Isherwood L, Crettenden A, Flavel J, Karmel T, et al. The aged care workforce, 2016. Canberra: Australian Government Department of Health. 2017.
Beks H, Clayden S, Shee AW, Binder MJ, O’Keeffe S, Versace VL. Evaluated nurse-led models of care implemented in regional, rural, and remote Australia: A scoping review. Collegian. https://www.sciencedirect.com/science/article/pii/S1322769623000513 2023.
Australian Government. Unleashing the Potential of our Health Workforce (Scope of Practice Review). https://www.healthgovau/resources/publications/unleashing-the-potential-of-our-health-workforce-scope-of-practice-review-terms-of-reference?language=en. 2023.
Dan B. The many languages of developmental disability research. Wiley Online Library; 2022. p. 808–9.
Downing. Quality Assessment Tool for Quantatative Studies; Effective Public Healthcare Panacea Project. https://www.ephppca/quality-assessment-tool-for-quantitative-studies/. 2016.
Acknowledgements
All contributing researchers have been acknowledged as an author.
Funding
This rapid review was funded by the Academic and Research Collaborative in Health (ARCH) at La Trobe University.
Author information
Authors and Affiliations
Contributions
Conceptualisation: MM, NB, RM, IB; methodology: MM, NB, RM, IB; validation: all authors; formal analysis: all authors; investigation: MM, NB, RM, IB; data curation: all authors; writing—original draft: all authors; writing—review and editing: all authors; supervision MM; project administration: MM; funding: MM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: example of rapid review search strategy for Ovid MEDLINE
Query | Results from 15 Nov 2022 | |
|---|---|---|
1 | Care Workforce.mp | 1560 |
2 | Health Workforce.mp | 16,950 |
3 | Ageing Workforce.mp | 94 |
4 | Aged Care Workforce.mp | 56 |
5 | Disability Workforce.mp | 11 |
6 | Rehabilitation Workforce.mp | 38 |
7 | Nursing Workforce.mp | 2054 |
8 | Allied Health Workforce.mp | 62 |
9 | Medical Workforce.mp | 699 |
10 | Mental Health Workforce.mp | 209 |
11 | Social Workforce.mp | 4 |
12 | Housing Workforce.mp | 0 |
13 | Homelessness Workforce.mp | 0 |
14 | Childcare Workforce.mp | 0 |
15 | Child Protection Workforce.mp | 1 |
16 | Family Violence Workforce.mp | 1 |
17 | Domestic Violence Workforce.mp | 0 |
18 | Family Service* Workforce.mp | 1 |
19 | Rural Workforce.mp | 205 |
20 | Remote Workforce.mp | 18 |
21 | Indigenous Workforce.mp | 14 |
22 | Hospital Workforce.mp | 73 |
23 | Home Care Workforce.mp | 31 |
24 | Community Workforce.mp | 20 |
25 | Drug Workforce.mp | 6 |
26 | Alcohol Workforce.mp | 2 |
27 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 | 21,027 |
28 | Recruit*.mp | 402,763 |
29 | Retention.mp | 187,007 |
30 | Safe*.mp | 964,726 |
31 | Educat*.mp | 1,067,939 |
32 | 28 or 29 or 30 or 31 | 2,489,424 |
33 | 27 and 32 | 8997 |
34 | limit 33 to English language | 8449 |
35 | limit 34 to year = "2015 -Current" | 3420 |
Appendix 2: Scores for the PEDro [37, 38] risk of bias assessment
PEDro: risk of Bias (Yes = 1; No = 0) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Included paper | Random allocation of participants to groups | Allocation concealment | Similarity of groups at baseline regarding the most important prognostic indicators | Blinding of all participants | Blinding of all therapists who administered the therapy or intervention | Blinding of all assessors who measured at least one key outcome | Measures of at least one key outcome were obtained from more than 85% of the participants initially allocated to groups | All participants for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analysed by “intention to treat” | The results of between-group statistical comparisons are reported for at least one key outcome | The study provides both point measures and measures of variability for at least one key outcome | Score out of 10 |
Abdulla et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Alwy Al-Beity et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Ayisi-Boateng et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Azoulay et al. 2021 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Bennett et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 4 |
Chicoine 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Clancy et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Dierkes et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Downing et al. 2016 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Gajewski et al. 2019 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
Gordon et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Islam et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Jafari et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Jedwab et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Johnston et al. 2020 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 |
Martin et al. 2019 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Mikolajczyk et al. 2021 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Morshed et al. 2017 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
Murthy et al. 2020 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
Neikrug et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Ortega et al. 2018 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
Ortega et al. 2021 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 4 |
Parmar et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Playford et al. 2020 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Risendal et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Salehi et al. 2021 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Sibrian et al. 2022 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
Tran et al. 2019 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Vesel et al. 2015 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Zhang et al. 2021 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Appendix 3: Individual scores for the quality assessment tool for quantitative studies [90]
Quality assessment tool for quantitative studies: quality assessment | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Included paper | Selection Bias (S = Strong; M = Moderate; W = Weak) | Study Design (S = Strong; M = Moderate; W = Weak) | Confounders (S = Strong; M = Moderate; W = Weak) | Blinding (S = Strong; M = Moderate; W = Weak) | Data Collection Methods (S = Strong; M = Moderate; W = Weak) | Withdrawals and Drop-outs (S = Strong; M = Moderate; W = Weak) | Intervention Integrity: received allocated intervention/exposure | Intervention Integrity: consistency of intervention measured | Intervention Integrity: likelihood of contamination | Analysis: unit of allocation | Analysis: unit of analysis | Analysis: appropriate statistical analysis | Analysis: is analysis via intention to treat | Global rating |
Abdulla et al. 2020 | S | M | M | M | W | S | 80–100% | Can’t tell | No | Individual | Individual | Yes | No | M |
Alwy Al-Beity et al. 2020 | M | M | M | W | S | S | 80–100% | Can’t tell | No | Individual | Individual | Yes | No | M |
Ayisi-Boateng et al. 2022 | W | W | W | W | S | N/A | 80–100% | Can’t tell | No | Practice | Individual | Yes | Can’t tell | W |
Azoulay et al. 2021 | W | M | W | M | S | N/A | 80–100% | Can’t tell | Can’t tell | Individual | Individual | Yes | No | W |
Bennett et al. 2022 | M | S | S | W | S | S | 80–100% | Can’t tell | Can’t tell | Community | Community | Yes | Can’t tell | M |
Chicoine 2022 | W | M | W | W | M | W | < 60% | Can’t tell | Can’t tell | Organisation | Individual | Yes | No | W |
Clancy et al. 2020 | S | S | M | W | S | S | 80–100% | Can’t tell | No | Organisation | Organisation | Yes | Can’t tell | M |
Dierkes et al. 2022 | S | S | M | W | S | N/A | 80–100% | Yes | No | Organisation | Organisation | Yes | Can’t tell | M |
Downing et al. 2016 | W | M | W | W | W | S | 80–100% | Can’t tell | No | Organisation | Individual | Can’t tell | No | W |
Gajewski et al. 2019 | M | M | M | M | W | W | 80–100% | Can’t tell | Can’t tell | Organisation | Organisation | No | Can’t tell | W |
Gordon et al. 2022 | W | W | W | W | M | W | Can’t tell | Can’t tell | Can’t tell | Individual | Individual | Yes | Can’t tell | W |
Islam et al. 2020 | M | W | W | W | W | W | 80–100% | Can’t tell | No | Individual | Individual | Yes | Can’t tell | W |
Jafari et al. 2020 | M | W | W | W | W | M | 60–79% | Can’t tell | No | Individual | Individual | Yes | Can’t tell | W |
Jedwab et al. 2022 | W | M | W | M | M | M | < 60% | Can’t tell | Can’t tell | Organisation | Organisation | Yes | Can’t tell | W |
Johnston et al. 2020 | M | M | M | W | M | M | 60–79% | Can’t tell | Can’t tell | Organisation | Organisation | Yes | Can’t tell | M |
Martin et al. 2019 | M | M | W | W | W | W | Can’t tell | Yes | Can’t tell | Individual | Individual | Yes | Can’t tell | W |
Mikolajczyk et al. 2021 | M | M | W | W | W | S | 80–100% | Can’t tell | No | Individual | Individual | Yes | Yes | W |
Morshed et al. 2017 | W | W | M | W | W | S | Can’t tell | Can’t tell | Can’t tell | Individual | Individual | Yes | No | W |
Murthy et al. 2020 | S | S | S | M | W | S | 80–100% | Yes | No | Individual | Individual | Yes | Yes | M |
Neikrug et al. 2022 | W | M | S | W | S | W | 80–100% | Yes | No | Individual | Individual | Yes | Yes | W |
Ortega et al. 2018 | W | W | W | W | W | W | Can’t tell | Can’t tell | Can’t tell | Community | Community | Yes | No | W |
Ortega et al. 2021 | M | M | W | W | W | N/A | Can’t tell | Can’t tell | Can’t tell | Community | Community | Yes | Can’t tell | W |
Parmar et al. 2022 | S | M | W | W | S | S | 80–100% | Yes | Can’t tell | Individual | Individual | Yes | No | W |
Playford et al. 2020 | W | M | W | W | S | W | 80–100% | Yes | Can’t tell | Individual | Individual | Yes | No | W |
Risendal et al. 2022 | M | W | M | W | W | W | 60–79% | Can’t tell | No | Organisation | Individual | Yes | No | W |
Salehi et al. 2021 | W | M | W | M | W | S | Can’t tell | Yes | Yes | Organisation | Organisation | Yes | Can’t tell | W |
Sibrian et al. 2022 | W | M | W | M | W | W | Can’t tell | Can’t tell | Can’t tell | Organisation | Organisation | Can’t tell | Can’t tell | W |
Tran et al. 2019 | M | M | M | W | W | M | < 60% | No | No | Organisation | Organisation | Yes | Can’t tell | W |
Vesel et al. 2015 | M | M | W | W | S | M | 80–100% | Can’t tell | Can’t tell | Organisation | Organisation | No | No | W |
Zhang et al. 2021 | M | W | W | W | W | W | Can’t tell | No | No | Practice | Practice | Yes | Can’t tell | W |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Morris, M.E., Brusco, N.K., McAleer, R. et al. Professional care workforce: a rapid review of evidence supporting methods of recruitment, retention, safety, and education. Hum Resour Health 21, 95 (2023). https://doi.org/10.1186/s12960-023-00879-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-023-00879-5