Abstract
There is a broad consensus and evidence that shows qualified, accessible, and responsive human resources for health (HRH) can make a major impact on the health of the populations. At the same time, there is widespread recognition that HRH crises particularly in low- and middle-income countries (LMICs) impede the achievement of better health outcomes/targets. In order to achieve the Sustainable Development Goals (SDGs), equitable access to a skilled and motivated health worker within a performing health system is need to be ensured. This review contributes to the vast pool of literature towards the assessment of HRH for maternal health and is focused on interventions delivered by skilled birth attendants (SBAs). Studies were included if (a) any HRH interventions in management system, policy, finance, education, partnership, and leadership were implemented; (b) these were related to SBA; (c) reported outcomes related to maternal health; (d) the studies were conducted in LMICs; and (e) studies were in English. Studies were excluded if traditional birth attendants and/or community health workers were trained. The review identified 25 studies which revealed reasons for poor maternal health outcomes in LMICs despite the efforts and policies implemented throughout these years. This review suggested an urgent and immediate need for formative evidence-based research on effective HRH interventions for improved maternal health outcomes. Other initiatives such as education and empowerment of women, alleviating poverty, establishing gender equality, and provision of infrastructure, equipment, drugs, and supplies are all integral components that are required to achieve SDGs by reducing maternal mortality and improving maternal health.
Similar content being viewed by others
Background
Maternal health is one of the main global health challenges in which least progress was witnessed in the year 2015 [1]. Hence, greater progress is required to meet the newly developed Sustainable Development Goals (SDGs) by ensuring equitable access to a skilled and motivated health worker within a performing health system. Less than 1% of the annual maternal deaths occur in the developed world, while a large proportion of these occur in low- and middle-income countries (LMICs). Further, for every woman dying, at least 30 others suffer complications which often end up being long-term and devastating which includes infertility and damage to the reproductive organs. It is widely agreed that there is not a single straightforward intervention, which can bring significant decrease in maternal mortality, but it can only be addressed by strengthening and providing an efficient health system with the provision of trained health workers being its key component [2–4]. The shortage of health workers was the most significant constraint noticed for not attaining the three health-related Millennium Development Goal (MDG) targets by many countries [3, 5–8].
Unfortunately, the workforce is distributed unevenly [9, 10]. Asia, a continent with half of the world’s population, has access to only 30% of the world’s health professionals [11]. Africa, with the highest burden of disease, has access to only 1% of the world’s health professionals [11]. Whereas America which has 10% of the global burden of disease has approximately 40% of the world’s health professionals [11]. The scenario within each country also shows asymmetry in the distribution of health professionals with low number of professionals in the rural compared to urban areas [12, 13]. Apart from mal-distribution, many countries face difficulties in recruiting and retaining health professionals. Insufficient number of medical schools, low salaries of the existing health workforce, poor working conditions, lack of supervision, low morale and motivation, and lack of infrastructure are few prominent causes for the loss of health professionals, where they immigrate to wealthier countries [14–18].
The shortage of emergency obstetric care (EmOC) and surgical services in LMICs over the last decade has attracted substantial attention [19–22]. In response, governments, health organizations, and communities have taken actions to address human resources for health (HRH) needs. There is a substantial evidence that highlights initiatives and innovative actions which have increased efficiency in utilizing existing human resources, including team approaches for delivery of intervention, multi-tasking, task shifting and sharing, and increased involvement by the communities [23]. However, most of them are implemented on a small scale or at limited capacity. In this context, it is important to realize that there is immense need for better planning, distribution, and management of limited human resources to address SDGs and strong need for formative evidence learned through lessons towards achieving this goal. This review has focused on the impact of HRH interventions for maternal health delivered by skilled birth attendants (SBAs) [24, 25] (Table 1). We have also derived lessons, identified research gaps, and formulated recommendations based on the studies from LMICs.
Methods
The review derived evidence from randomized controlled trials (RCTs), quasi-RCTs, and prospective before/after and cohort studies on SBAs working at the national, provincial, district, and community levels (home, community or referral facility interventions). Studies were included if (a) they implemented any HRH interventions in management system, policy, finance, education, partnership, and leadership; (b) those were related to SBAs; (c) have reported outcomes related to maternal health such as changes in morbidity, mortality, coverage, or other interrelated outcomes; (d) were conducted in LMICs [26]; and (e) were written in English. Studies in which traditional birth attendants and/or community health workers were trained were excluded.
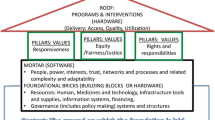
The search strategy included PubMed articles published from January 2000 to December 2015. The reason to select this time period was to evaluate what progress has been made since the 2000 deadline of the Alma Ata health for all and what improvements followed on the agreement on MDGs. The HRH Global Resource Centre was also searched to access the available studies. Detailed examination of cross-references and bibliographies of identified studies was also performed to identify additional sources of information. The following search strategy was primarily used. [(“health worker*” OR “health care worker*” OR “health professional” OR “health personnel” OR doctor* OR nurse* OR physician* OR midwi* OR “nurse midwi*” OR “skilled birth attendant*”) AND (training OR education OR curriculum OR teaching OR learning OR “patient centered care” OR “patient focused care” OR “staff development” OR medicine OR “postgraduate training” OR “diploma training” OR recruitment OR attraction OR deployment OR employment OR personnel selection OR incentive OR reward OR “cash award”)]. The quality of RCTs and quasi-RCTs was assessed using the Cochrane methods [27]; however, the quality of prospective studies/pre-post trials was assessed using the criteria adopted from Loevinsohn (Table 2) [28]. To assess the different dimensions of the HR planning and management spectrum, this review used the HRH action framework (Fig. 1) as defined by WHO [29]. The framework has six action fields, each of which has several areas of intervention. For a better response to HRH crises, each of the six action fields needs to be addressed. These are described in Table 3.
Results
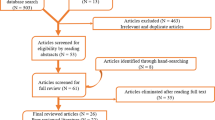
The defined search strategy identified 4565 studies. Of these, 217 were retrieved for full-text review; however, only 25 papers passed the eligibility criteria for inclusion (Fig. 2). Studies were grouped and analyzed according to different dimensions and components of HRH interventions. However, we found studies related to education, policies, and those with multiple combined interventions.
Education (training/task shifting)
We identified 15 low- to moderate-quality studies. Of these, four were RCTs [30–33], eight were prospective (before/after) [34–41], two were quasi-experimental [42, 43], and one was a prospective cohort [44]. Most of these were from African and South East Asian regions (Table 4).
To improve access to health care and conserve scarce health resources, some countries have trained mid-level providers and other cadre of health workers to deliver health care services. A study from Turkey and the Philippines compared intrauterine device (IUD) insertion by auxiliary nurse midwives (ANMs) with physicians at teaching hospitals and found no difference in those who were referred to a specialist after insertion of IUD (RR 0.93; 95% CI, 0.45–1.90) [31]. Similarly, in Thailand, a study compared postpartum tubal ligation by midlevel health workers and found no difference between the groups in postoperative complications (RR 2.43; 95% CI, 0.64–9.22) [30]. In a study from Nepal, the effectiveness of administration of early medical abortion by certified nurses and auxiliary nurses was compared with doctors [33]. Similarly, in South Africa and Vietnam, they compared manual vacuum aspiration (MVA) in women performed by an ANM or doctor’s assistants [32]. No significant difference in the likelihood of an incomplete abortion between groups of patients managed by ANMs and those managed by doctors (RR 0.93; 95% CI, 0.45–1.90) was found. No differences were found in the likelihood of a complication during (RR 3.07; 95% CI, 0.16–59.1)—or an adverse event after (RR 1.36; 95% CI, 0.54–3.40)—the MVA.
In Malawi [44], clinical officers (COs) were trained locally to perform major emergency and elective surgery. The study found no difference in postoperative maternal health outcomes, such as fever, wound infection, need for re-operation, and maternal death, when procedures performed by CO were compared to medical officers (MOs) (RR 0.99; 95% CI, 0.95–1.03). No difference was observed in stillbirth (RR 0.75; 95% CI, 0.52–1.09) or neonatal death (RR 1.40; 95% CI, 0.51–3.87). However, maternal deaths were 1.17% and 0.39% in the CO and MO group, respectively.
A study from Ethiopia [34] discussed the national program “Save the Mothers Project” that focused on providing three rounds of 3-month teaching to train service providers (general physicians (GPs), midwives, and others) on life-saving procedures in obstetrics and reported an increase in total number of instrumental deliveries from 6% in 1998 to 23% in 2001 due to considerable increase in the admission of complications. Similarly, in Bangladesh [38], MOs were trained for a year in obstetrics and anesthesia, nurses in midwifery for 6 months, and lab technicians in safe blood transfusions for a period of 2 weeks. As a result of the acquired skills, natural deliveries in the districts increased to 63%, admissions of complicated cases increased to 135%, and cesarean sections increased to 70%. The cost per trainee was approximately $1550 for MOs, $340 for nurses, and $140 for laboratory technicians.
The cost of training and deploying trained assistant medical officers (AMOs) was also compared among physicians in Mozambique [37]. They found that 30-year cost for major obstetric surgery was approximately $39 for AMOs and $144 for physicians. Doubling the salaries of AMOs resulted in smaller but still substantial difference in cost per surgery. Similar results were obtained from a study conducted in Tanzania [39], which started training AMOs for cesarean sections and other emergency surgeries in 1963. As a result, the met need increased and case fatality rate (CFR) decreased. There were no differences in outcomes, risk indicators, or quality of care in obstetric operations performed by AMOs and MOs.
A different approach was taken in studies conducted in Mozambique [43]. AMOs with previous surgical experience were trained for 3 years and were compared to obstetricians [43]. The only significant difference observed between the two groups was in superficial wound separation due to hematoma, which was slightly higher in AMOs (0.35%) versus the specialists (0.05%). Similarly, Nigeria [36] in 1993 trained midwives and residents with principles and practices of EmOC and henceforth found a reduction in treatment interval from 3.7 h to 1.6 h, and the proportion of women treated in less than 30 min increased from 39% to 87%. CFR fell from 14% to 11%. The annual number of women with complication declined as well.
Nepal, on the other hand, trained doctors, midwives, and nurses on different aspects of basic and comprehensive EmOC services [41] and found a reduction in CFR from 3.0% to 0.3%. Similarly, in Paraguay [40], nurses, auxiliary nurses, and auxiliary midwives were trained on theoretical and clinical aspects of life-saving skills in obstetric emergencies and reported an increase in knowledge. A study from Ghana [42] provided 6 months of self-paced and 1-week of residential training to midwives and physicians and compared them to a similar cadre given 3-week residential training on life-saving skills, obstetric and infant care, family planning counseling, and post abortion care. The residential group performed slightly better; however, overall levels of knowledge and performance remained low.
Policy implementation
We identified four moderate-quality [12, 45–47] prospective before/after studies (Table 5).
In the beginning of 1994, Bangladesh upgraded its EmOC facilities and trained service providers in those facilities [46]. However, from the beginning of 2001, to complement the facility approach to obstetric care, a skilled birth attendant strategy was initiated with guidance from the World Health Organization and UNFPA. As a result, measles, mumps, and rubella (maternal mortality ratio (MMR)) declined to 22% in the 11 intervening years. Professional care increased from 13% to 18% and rates of cesarean section from 0.9% to 5.4%. The policy implementation also affected the antenatal consultation which doubled from 27% in 1991–1994 to 60% in 2005–2007.
Similarly, the Nepal National Safe Motherhood Project [47], implemented from 1997 to 2004, focused on improving emergency obstetric services and midwifery care in selected health facilities. Government policy was developed to increase access to midwifery and obstetric services to improve management of service provision for women of reproductive age by working with NGOs for training and service provision and non-state health workers. As a result, the average annual met need increased from 1.3% to 14%. Deliveries attended by ANMs or nurse increased from 3% in 2001 to 8% in 2006. Free or reduced cost for services and transport was valued by the communities, and the intervention increased their confidence to cope with emergencies.
In Cambodia, to compensate low wages, health care workers demanded unofficial payments from patients in facilities where health care services were provided free of charge. Introduction of a user fee at the national maternal and child health center of Cambodia [45] assisted the hospital to retain revenue and improve the quality of services focusing on the work environment and conditions of HR intervention. Patient satisfaction increased to 93%, and average monthly number of deliveries increased from 319 to 585.
The Indonesian government in order to overcome the shortage of health workers [12] implemented compulsory services in rural areas to support the recruitment and deployment of medical staff in remote and very remote areas. Doctors, dentists, and midwives were assigned as temporary staff on contract basis for a certain time. In addition, a special assignment program was implemented which included other health cadres as well where they received travel expenses and additional incentives for a period of service and according to the remoteness. Both these programs improved the availability of health workers in remote areas. As a result, in 2010, only 17% of the 9000 very remote health centers were without a doctor, compared with 30% of 8000 health centers in 2006.
Combined interventions
We found six low- to moderate-quality prospective before/after studies [24, 48–52] with combined interventions which focused on HR training, policy and advocacy, partnerships, and supervision [49] (Table 6).
In one study from Rwanda [50], CARE’s work supported a comprehensive package of interventions which included training of the doctors and midwives to manage major obstetric complications. As a result, numbers of deliveries and management of obstetric complications increased by almost 25% and 27%, respectively, from 2001 to 2002. A continuous decrease in the CFR was also observed from 2.2% in 2001 to 1.8% in 2002 and finally 1.2% in 2004.
Similarly, in Peru [51], a decline in CFR from 1.7% to 0.1% and increase in met needs from 30% to 84% were observed after the implementation of a 15-day training and supervision program to improve the quality of care. Likewise, Mozambique [52] trained 137 different professionals and adopted an enhanced policy for the improvement of the quality, access, and utilization of the EmOC such as supportive supervision, logistics for supplies, provision of equipment and drugs, record keeping, monitoring and evaluation, and quality improvement techniques. Maternal death audits showed an increase in met needs from 11% to 33% and decrease in CFR from 3% to 1.6%. Similarly, in Nepal [24], utilization of antenatal care services increased from 39% to 72%, delivery by trained SBAs from 9% to 19%, institutional delivery from 8% to 18%, cesarean sections from 1% to 3%, and CFR decreased from 0.5% to 0.4% after the establishment of policy to provide EmOC to the most deprived population. Incentives were given to the mothers and health workers to address the financial barriers to women accessing maternal services. A range of external agencies supported staff training; infrastructure and equipment; behavior change interventions promoting antenatal, skilled delivery, and postpartum care; and community emergency funds and transport schemes.
Discussion
A major part of this review was aimed at exploring how HRH interventions lead to improved maternal health outcomes, and we also came across studies with successful HRH strategies pertaining to general health outcomes [12, 16, 18, 53]. The findings, although mostly from low- to moderate-quality studies, showed that HRH interventions can contribute positively to the health worker’s performance and improved maternal outcomes. However, we still feel that HRH interventions in relation to maternal health are not widely researched.
The WHO framework (Fig. 1) shows the steps required for improving general health outcomes; we developed a framework to facilitate understanding of mechanisms, based upon dimensions of health worker performance (Fig. 3), to explain the effect on maternal mortality. It reveals a variety of interrelated mechanisms which can lead to improved health worker performance and maternal health outcomes provided other associated or confounding factors are addressed. Implementation of a HRH management system to improve the availability, training, education, and retention of doctors, nurses, midwives, and technicians is one of the factors contributing to improved maternal health. Other components included in the studies were supervision and partnerships which improved the health system effectiveness and hence maternal health. Increase in knowledge and competence with concomitant increase in accountability and productivity of SBAs will lead to better health outcomes resulting in decrease in maternal mortality and morbidity.
The review of 25 studies revealed certain reasons why maternal mortality and morbidity is still high in LMICs despite the efforts and policies implemented throughout these years. It is observed that in many LMICs some components of the HRH intervention were applied with positive effects on the maternal health and health care delivery to the rural areas. When a professional (doctor or midwife) is linked up with a strong referral system, maternal health outcomes improve and mortality decreases significantly irrespective of whether the birth took place at home or in a health facility [54]. Programs should therefore integrate maternal health and family planning as decline in fertility can reduce maternal mortality which can be achieved by aligning formal/informal linkages or partnering different programs [55]. Secondly, it is important to educate women about their health and complications during pregnancy, and evidence suggests that awareness improves care seeking [55, 56]. However, poverty is one of the main factors affecting the access to maternal health care in rural areas which warrants combating gender inequalities [56, 57]. In such scenarios, community involvement has been found to be integral in raising the awareness in community which can further be scaled up to integrate micro-financing schemes to help improve the financial stability in families/community.
In the review, we found that only few components of the HRH management system were investigated. Most of the studies explored the impact of training and continuing education of the health care providers on maternal health individually or as combined intervention. However, less or no work was found on the HRH systems studying the impact of recruitment, employment, hiring, deployment, migration, health safety, and retirement on maternal health outcomes. Similarly, no study was found on the financial component addressing the budget allocation for salaries and allowances, education and training, and HRH expenditure data. Gaps were identified in other HRH interventions related to staff motivations such as job satisfaction, appraisals, workplace safety, career development, and improvement in the work environment as well as the HRH information system. Moreover, studies that reported the impact of training SBAs on improved health outcomes rarely reported if those results were merely because of training alone or there was a role of other related co-interventions as well.
Improvements in HRH are required to be made by LMICs to raise the awareness among women for health care seeking from SBAs and at the same time improving the delivery of health care. The need for a multi-sectoral approach to women health is emphasized. This includes the training of staff, their employment and retention, and improved management systems in the formal health care [58]. It is important to address the keen desire of continued education/training of health workers especially doctors. The training and education programs implemented in some countries need to be taken on the larger scale. Also, the keen desire of health workers especially doctors embarking higher positions should be addressed. Government should work in conjunction with other stakeholders and donors to form policies for education and finance and develop health care models to suit the needs of the countries in managing EmOC and decreasing maternal mortality.
We recommend that more studies need to be conducted on the other HRH management system components such as supervision, partnership, and proper HRH information system development especially in the context of SBAs and their impact on the maternal health. Financial constraint remains the most important barrier to achieve the targets. Therefore, interventions targeting the budget allocations for the salaries and education of the health care providers need to be implemented and their impact on maternal mortality to be studied. It is well documented that more lives of mothers can be saved if adequate importance is given to the EmOC services and if they are made an integral part of the health system [59, 60]. The importance of collaboration between SBAs and other health care providers like obstetricians and anesthesiologists as well as lay health providers has also been emphasized [25, 61], and its integration in national policies has also been underscored for better outcomes [58, 62–64]. Political sensitization is needed at the local level, particularly with local policies [65]. Investment at all levels to strengthen the comprehensive EmOC and family-planning program is required [55]. Political parties, stakeholders, and donors need to work together to invest in improving the availability and quality of maternal care services [56]. A high level of political commitment is also required in investing, developing, deploying, and supporting a cadre of health providers with midwifery skills [66].
It is important to assess and urgently address the barriers to recruitment, deployment, and retention of skilled personnel in LMICs [67] and to discourage the process of “brain drain” [68, 69]. The deployment, recruitment, and retention of care providers especially nurses and specialists are a major challenge on the supply side [69–71].
Furthermore, it is important to provide health care professionals with ongoing training [72, 73]. A study from Kenya reported that only 18% of the staff had received life-saving skills and only 37% received training related to prevention of mother-to-child HIV transmission, which is the utmost required skill in a country like Africa [73]. Thus, it emphasizes the importance of training to meet the needs of the population.
The limited management capacity is one of the main reasons of slow progress in maternal health [71]. It is observed that a well-functioning health system with appropriate supply of equipment, drugs, and other supplies is required for timely management of delivery complications to prevent maternal deaths [2]. Studies found that the utilization of health services may be low because of the gender inequality and status of the women as well as cultural barriers. Empowerment of women and education has shown to positively influence the health-seeking behavior and decrease in maternal mortality [74–77]; thus, efforts should be made to improve this area for sustainability of the interventions to decrease maternal mortality and improve overall health care utilization.
It is seen that HRH interventions alone cannot improve the functioning and availability of the skilled health workers. There are many other areas to gain the best outcome regarding maternal health. Female education, empowerment, and gender equality should be emphasized [62]. Effective provision of services can only be made possible when huge inequalities in maternal care are removed from the community. The poor-rich inequalities in delivery care can be reduced by providing equal services to all by rigorous efforts made towards equity oriented research, policy making, implementation, and proper monitoring of the services provided [57]. Investment in social and economic development with emphasis on achieving gender equality should be the goal [66]. Similarly, access and availability of affordable transportation in rural areas as well as appropriate supply of drugs, equipment, and infrastructure of the health facilities are needed to improve EmOC and reduce maternal mortality.
Conclusions
This review suggested an urgent and immediate need for formative evidence-based research on effective HR interventions for improved maternal health in LMICs. The principal challenges in these countries are to strengthen research systems, identify key research questions, and generate the capacity to turn research into practical applications [78]. The studies showed that all the HRH interventions implemented individually or in combination had a positive impact on improving maternal health. However, implementation alone is not enough to bring about this change but also other essential steps like educating and empowering women, alleviating poverty, establishing gender equality, and providing infrastructure, availability of equipment, drugs, and supplies are all an integral part of working towards the achievement of SDGs and reducing maternal mortality. Leaders and stakeholders are required to work together as a team to construct new models of health care according to the individual needs of each country.
Abbreviations
- AMO:
-
assistant medical officer
- ANM:
-
auxiliary nurse midwife
- CFR:
-
case fatality rate
- CO:
-
clinical officer
- EmOC:
-
emergency obstetric care
- GP:
-
general physician
- HRH:
-
human resources for health
- LMICs:
-
low- and middle-income countries
- MDG:
-
Millennium Development Goal
- MO:
-
medical officer
- MVA:
-
manual vacuum aspiration
- RCT:
-
randomized controlled trial
- SBA:
-
skilled birth attendant
References
Simwaka BN, Theobald S, Amekudzi YP, Tolhurst R. Meeting Millennium Development Goals 3 and 5. BMJ. 2005;331(7519):708–9.
Rasch V. Maternal death and the Millennium Development Goals. Dan Med Bull. 2007;54(2):167–9.
Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, Cueto M, Dare L, Dussault G, Elzinga G et al. Human resources for health: overcoming the crisis. Lancet. 2004;364(9449):1984–90.
Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, Jensen J, Johansen M, Aja GN, Zwarenstein M et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010;3(Issue 3):CD00401.
Cometto G, Witter S. Tackling health workforce challenges to universal health coverage: setting targets and measuring progress. Bull World Health Organ. 2013;91:881–5.
Travis P, Bennett S, Haines A, Pang T, Bhutta Z, Hyder AA, Pielemeier NR, Mills A, Evans T. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364(9437):900–6.
Haines A, Cassels A. Can the Millennium Development Goals be attained? BMJ. 2004;329(7462):394–7.
Bhutta ZA, Lassi ZS, Pariyo G, Huicho L. Global experience of community health workers for delivery of health related Millennium Development Goals: a systematic review, country case studies, and recommendations for integration into national health systems. In.: Global Health Workforce Alliance/World Health Organization. 2010. Available at http://www.who.int/workforcealliance/knowledge/publications/CHW_FullReport_2010.pdf?ua=1.
Speybroeck N, Ebener S, Sousa A, Paraje G, Evans DB, Prasad A. Inequality in access to human resources for health: measurement issues. Geneva: World Health Organization; 2006.
Sousa A, Tandon A, Dal Poz MR, Prasad A, Evans DB. Measuring the efficiency of human resources for health in attaining health outcomes across sub national units in Brazil. Geneva: World Health Organization; 2006.
World Health Organization. The world health report: working together for health. 2006.
Efendi F. Health worker recruitment and deployment in remote areas of Indonesia. Rural Remote Health. 2012;12:2008.
Zurn P, Dal Poz MR, Stilwell B, Adams O. Imbalance in the health workforce. Hum Resour Health. 2004;2(1):13.
Ferrinho P, Van Lerberghe W, da Cruz GA. Public and private practice: a balancing act for health staff. Bull World Health Organ. 1999;77(3):209.
Kirigia JM, Gbary AR, Muthuri LK, Nyoni J, Seddoh A. The cost of health professionals’ brain drain in Kenya. BMC Health Serv Res. 2006;6:89.
Lassey AT, Lassey PD, Boamah M. Career destinations of University of Ghana Medical School graduates of various year groups. Ghana Med J. 2013;47(2):87–91.
Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 2008;8:19.
Ramani S, Rao KD, Ryan M, Vujicic M, Berman P. For more than love or money: attitudes of student and in-service health workers towards rural service in India. Hum Resour Health. 2013;11:58.
Anyangwe SC, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health. 2007;4(2):93–100.
Berer M. Maternal mortality and morbidity: is pregnancy getting safer for women? Reprod Health Matters. 2007;15(30):6–16.
Brugha R, Pritze-Aliassime S. Promoting safe motherhood through the private sector in low-and middle-income countries. Bull World Health Organ. 2003;81:616–23.
Ozgediz D, Riviello R. The “other” neglected diseases in global public health: surgical conditions in sub-Saharan Africa. PLoS Med. 2008;5(6):e121.
Lassi ZS, Cometto G, Huicho L, Bhutta ZA. Quality of care provided by mid-level health workers: systematic review and meta-analysis. Bull World Health Organ. 2013;91:824–33.
Barker CE, Bird CE, Pradhan A, Shakya G. Support to the Safe Motherhood Programme in Nepal: an integrated approach. Reprod Health Matters. 2007;15(30):81–90.
de Bernis L, Sherratt DR, AbouZahr C, Van Lerberghe W. Skilled attendants for pregnancy, childbirth and postnatal care. Br Med Bull. 2003;67(1):39.
2012 list of developing countries. In: World Bank; 2012. Available at https://www.usaid.gov/sites/default/files/documents/1876/310maa.pdf. Accessed on 21 June 2012.
Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. London: BMJ Books; 2001.
Loevinsohn BP. Health education interventions in developing countries: a methodological review of published articles. Int J Epidemiol. 1990;19(4):788–94.
HRH action framework. In: Capacity Project, Global Health Workforce Alliance. United States Agency for International Development, World Health Organization; 2007. Available at: http://www.capacityproject.org/framework/.
Dusitsin NCS, Varakamin S, Boonsiri B, Ningsanon P, Gray RH. Post-partum tubal ligation by nurse-midwives and doctors in Thailand. Lancet. 1980;1(8169):638–9.
Eren N, Ramos R, Gray RH. Physicians vs. auxiliary nurse-midwives as providers of IUD services: a study in Turkey and the Philippines. Stud Fam Plann. 1983;14(2):43–7.
Warriner IKMO, Hoffman M, Morroni C, Harries J, My Huong NT, et al. Rates of complication in first-trimester manual vacuum aspiration abortion done by doctors and mid-level providers in South Africa and Vietnam: a randomised controlled equivalence trial. Lancet. 2006;368(9551):1965–72.
Warriner IKWD, Huong NT, Thapa K, Tamang A, Shah I, et al. Can midlevel health-care providers administer early medical abortion as safely and effectively as doctors? A randomised controlled equivalence trial in Nepal. Lancet. 2011;377(9772):1155–61.
Mekbib T, Kassaye E, Getachew A, Tadesse T, Debebe A. The FIGO save the mothers initiative: the Ethiopia–Sweden collaboration. Int J Gynaecol Obstet. 2003;81(1):93–102.
Djan JO, Kyei-Faried S, Twum S, Danquah JBO, Ofori M, Browne ENL, Pmm Team TK. Upgrading obstetric care at the health center level, Juaben, Ghana. Int J Gynaecol Obstet. 1997;59:83–90.
Ifenne D, Essien E, Golji N, Sabitu K, Alti-Mu’azu M, Musa A, Adidu V, Mukaddas M. Improving the quality of obstetric care at the teaching hospital, Zaria, Nigeria. Int J Gynaecol Obstet. 1997;59:37–46.
Kruk ME, Pereira C, Vaz F, Bergstrom S, Galea S. Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG. 2007;114(10):1253–60.
Lawn JE, Tinker A, Munjanja SP, Cousens S. Where is maternal and child health now? Lancet. 2006;368(9546):1474–7.
McCord C, Mbaruku G, Pereira C, Nzabuhakwa C, Bergstrom S. The quality of emergency obstetrical surgery by assistant medical officers in Tanzanian district hospitals. Health Aff. 2009;28(5):w876.
Ohnishi M, Nakamura K, Takano T. Training of healthcare personnel to improve performance of community-based antenatal care program. Adv Health Sci Educ Theory Pract. 2007;12(2):147–56.
Rana TG, Chataut BD, Shakya G, Nanda G, Pratt A, Sakai S. Strengthening emergency obstetric care in Nepal: the Women’s Right to Life and Health Project (WRLHP). Int J Gynaecol Obstet. 2007;98(3):271–7.
Combine learning approaches to improve maternal health. In. Edited by Motherhood GS. Washington D.C. Population Council; 2006.
Pereira C, Bugalho A, Bergström S, Vaz F, Cotiro M. A comparative study of caesarean deliveries by assistant medical officers and obstetricians in Mozambique. BJOG. 2005;103(6):508–12.
Chilopora GPC, Kamwendo F, Chimbiri A, Malunga E, Bergström S. Postoperative outcome of caesarean sections and other major emergency obstetric surgery by clinical officers and medical officers in Malawi. Hum Resour Health. 2007;14(5):17.
Akashi H, Yamada T, Huot E, Kanal K, Sugimoto T. User fees at a public hospital in Cambodia: effects on hospital performance and provider attitudes. Soc Sci Med. 2004;58(3):553–64.
Koblinsky M, Anwar I, Mridha MK, Chowdhury ME, Botlero R. Reducing maternal mortality and improving maternal health: Bangladesh and MDG 5. J Health Popul Nutr. 2009;26(3):280.
Rath AD, Basnett I, Cole M, Subedi HN, Thomas D, Murray SF. Improving emergency obstetric care in a context of very high maternal mortality: The Nepal Safer Motherhood Project 1997–2004. Reprod Health Matters. 2007;15(30):72–80.
Islam MT, Haque YA, Waxman R, Bhuiyan AB. Implementation of emergency obstetric care training in Bangladesh: lessons learned. Reprod Health Matters. 2006;14(27):61–72.
Jamisse L, Songane F, Libombo A, Bique C, Faúndes A. Reducing maternal mortality in Mozambique: challenges, failures, successes and lessons learned. Int J Gynaecol Obstet. 2004;85(2):203–12.
Kayongo M, Butera J, Mboninyibuka D, Nyiransabimana B, Ntezimana A, Mukangamuje V. Improving availability of EmOC services in Rwanda—CARE’s experiences and lessons learned at Kabgayi Referral Hospital. Int J Gynaecol Obstet. 2006;92(3):291–8.
Kayongo M, Esquiche E, Luna MR, Frias G, Vega-Centeno L, Bailey P. Strengthening emergency obstetric care in Ayacucho, Peru. Int J Gynaecol Obstet. 2006;92(3):299–307.
Santos C, Diante D, Baptista A, Matediane E, Bique C, Bailey P. Improving emergency obstetric care in Mozambique: the story of Sofala. Int J Gynaecol Obstet. 2006;94(2):190–201.
Monica Desai JWR, Adisasmito W, Mounier-Jack S, Coker R. Critical interactions between Global Fund-supported programmes and health systems: a case study in Indonesia. Health Policy Plan. 2010;25 Suppl 1:i43–7.
Campbell OMR. What are maternal health policies in developing countries and who drives them? A review of the last half-century. Safe motherhood strategies: a review of the evidence 2000.
Chowdhury ME, Ahmed A, Kalim N, Koblinsky M. Causes of maternal mortality decline in Matlab. Bangladesh J Health Popul Nutr. 2009;27(2):108.
Gill K, Pande R, Malhotra A. Women deliver for development. Lancet. 2007;370(9595):1347–57.
Houweling TAJ, Ronsmans C, Campbell OMR, Kunst AE. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ. 2007;85:745–54.
Falconer A, Crisp E, Warick C, Day-Strik F. Scaling up human resources for women’s health. BJOG. 2009;116 Suppl 1:11–4.
Abe E, Omo-Aghoja LO. Maternal mortality at the Central Hospital, Benin City Nigeria: a ten year review. Afr J Reprod Health. 2008;12(3):17–26.
Gupta M, Mavalankar D, Trivedi P. A study of referral system for EmOC in Gujarat. 2009.
Mavalankar D, Sriram V. Provision of anaesthesia services for emergency obstetric care through task shifting in South Asia. Reprod Health Matters. 2009;17(33):21–31.
Costello A, Azad K, Barnett S. An alternative strategy to reduce maternal mortality. Lancet. 2006;368(9546):1477–9.
Figo SM. Human resources for health in the low-resource world: collaborative practice and task shifting in maternal and neonatal care. Int J Gynaecol Obstet. 2009;105(1):74–6.
Mridha MK, Anwar I, Koblinsky M. Public-sector maternal health programmes and services for rural Bangladesh. J Health Popul Nutr. 2009;27(2):124.
Filippi V, Ronsmans C, Campbell OMR, Graham WJ, Mills A, Borghi J, Koblinsky M, Osrin D. Maternal health in poor countries: the broader context and a call for action. Lancet. 2006;368(9546):1535–41.
ten Hoope-Bender P, Liljestrand J, MacDonagh S. Human resources and access to maternal health care. Int J Gynaecol Obstet. 2006;94(3):226–33.
Adegoke AA, van den Broek N. Skilled birth attendance-lessons learnt. BJOG. 2009;116(s1 International Reviews):33–40.
Naicker S, Plange-Rhule J, Tutt RC, Eastwood JB. Shortage of healthcare workers in developing countries—Africa. Ethn Dis. 2009;19(1):60.
Serour GI. Healthcare workers and the brain drain. Int J Gynaecol Obstet. 2009;106(2):175–8.
Anwar I, Kalim N, Koblinsky M. Quality of obstetric care in public-sector facilities and constraints to implementing emergency obstetric care services: evidence from high-and low-performing districts of Bangladesh. J Health Popul Nutr. 2009;27:139–55.
Mavalankar DV, Vora KS, Ramani KV, Raman P, Sharma B, Upadhyaya M. Maternal health in Gujarat, India: a case study. J Health Popul Nutr. 2009;27(2):235.
Narchi NZ. Exercise of essential competencies for midwifery care by nurses in São Paulo, Brazil. Midwifery. 2009;27(1):23–9.
Olenja J, Godia P, Kibaru J, Egondi T. Influence of provider training on quality of emergency obstetric care in Kenya. Calverton, Maryland, USA: Macro International Inc; 2009.
Bhuiya A, Hanifi SMA, Mahmood SS. Action monitoring for equity and gender in health. J Health Popul Nutr. 2009;26(3):378.
Cotter K, Hawken M, Temmerman M. Low use of skilled attendants’ delivery services in rural Kenya. J Health Popul Nutr. 2006;24(4):467.
Fernando D, Jayatilleka A, Karunaratna V. Pregnancy—reducing maternal deaths and disability in Sri Lanka: national strategies. Br Med Bull. 2003;67(1):85.
Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60.
Kayentao K, Garner P, van Eijk AM, Naidoo I, Roper C, Mulokozi A, MacArthur JR, Luntamo M, Ashorn P, Doumbo OK et al. Intermittent preventive therapy for malaria during pregnancy using 2 vs 3 or more doses of sulfadoxine-pyrimethamine and risk of low birth weight in Africa systematic review and meta-analysis. JAMA. 2013;309(6):594–604.
World Health Organization. Making pregnancy safer: the critical role of the skilled attendant. Geneva: A joint statement by WHO, ICM & FIGO. WHO; 2004.
Graham W. Can skilled attendance at delivery reduce maternal mortality in developing countries? Safe motherhood strategies: a review of the evidence. In. Edited by W. DBVVL. Antwerp: Studies in Health Services Organisation & Policy; 2001.
Mcdonald, Starr. Saving women’s lives, improving newborn health. Washington: Family Care International; 2002.
MacDonagh S. Achieving skilled attendance for all; a synthesis of current knowledge and recommended actions for scaling up. London: DFID Health Resource Centre; 2005.
Acknowledgements
This report is part of a wider study commissioned and funded by the WHO/PMNCH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ZSL and NBM wrote the first draft of the manuscript with subsequent inputs from BM, AF, KT, and ZAB. ZSL and NM oversaw the systematic review of interventions, with inputs from BM, KT, AF, and ZAB. NBM and ZSL updated the evidence base under the supervision of ZAB. All authors (ZSL, NBM, BM, NM, AF, KT, ZAB) contributed to writing and review of the paper. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lassi, Z.S., Musavi, N.B., Maliqi, B. et al. Systematic review on human resources for health interventions to improve maternal health outcomes: evidence from low- and middle-income countries. Hum Resour Health 14, 10 (2016). https://doi.org/10.1186/s12960-016-0106-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-016-0106-y