Abstract
Mild therapeutic hypothermia is considered standard care in the treatment of patients resuscitated from cardiac arrest. With increasingly more frequent concomitant use of platelet-inhibiting drugs, clinicians must be cognizant of the ramifications of hypothermia on platelet function as part of hemostasis. The effects of hypothermia on platelet function have been studied for more than 50 years, but the results are inconsistent and may be related to the circumstances during which hypothermia is achieved. This review summarizes current knowledge of platelet function during hypothermia and the impact on hemostasis.
Similar content being viewed by others
Introduction
Although humans are homeothermic, significant body-temperature changes can result in life-threatening situations (including bleeding and thrombosis), particularly in association with certain medical conditions [1]-[10].
Platelets lack nuclei, but perform multiple vital functions of nucleated cells. Platelets can generate new cell bodies packed with respiring mitochondria and α-granules [11]. Whereas platelets were once considered to function exclusively during hemostasis and thrombosis, they are now considered to function as circulating sentinels in the activation, modulation of the host immune response [12]-[14].
This review summarizes current knowledge of platelet function during hemostasis under various hypothermic conditions. The review will not discuss the effect of systemic hypothermia on the pharmacokinetics and pharmacodynamics of anti-platelet drugs [15]-[19].
Review
Fundamental aspects of hypothermia
The research on hemostasis in the setting of hypothermic reveals inconsistent, even conflicting results, ranging from seasonal increase in thromboembolic disease in winter to excessive surgical bleeding in hypothermic patients.
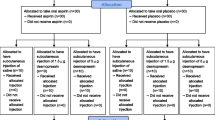
The effects of hypothermia [20] on coagulation and platelet function is influenced by
the actual body temperature during sampling
the pre-analytical and analytical temperature and sample type (in-vivo, ex-vivo, in-vitro; whole blood, washed platelet preparation)
temperature changes during the sampling time (induction, maintenance, and rewarming)
the moment of sampling in relation to agonist stimulation
the duration of hypothermia
the cause of hypothermia (spontaneous, whether induced externally or internally)
coexisting factors (extracorporeal circulation [21], comorbidity, drugs)
the modality of induced hypothermia (local, regional, or general) [2]
Hypothermia can be caused by metabolic dysfunction in association with decreased heat production (hypothyroidism, hypoglycemia, or hypoadrenalism) or disturbed thermoregulation (intracranial tumor or degenerative neurological disorders). Accidental hypothermia is an unintentional decrease of core temperature caused by prolonged exposure to cold [22]. Hypothermia acts as a natural survival strategy in some animals that hibernate, and actively suppresses metabolism. [4],[23],[24].
In trauma patients, extra precautions are required based on inherent bias due to absolute or relative hypovolemia and acidosis [25].
Since the early 1950s, active therapeutic cooling has been used during specific surgical procedures to reduce oxygen requirements of organs such as the brain, heart, and kidney [26],[27]. The use of hypothermia has recently been extended to post-resuscitation care based on results from more intensive and innovative monitoring techniques [28]-[31]. While precluding the current guidelines for platelet storage, research on chilled platelets (at 4°C, ex-vivo) should be differentiated from research on deep hypothermic circulatory arrest at in-vivo temperatures of 15-18°C and from research on cardiopulmonary bypass and post-resuscitation at temperatures > =28°C.
Hypothermia has been shown to result in hemoconcentration, leukopenia and thrombocytopenia, slowing down of coagulation enzymes, disordered fibrinolysis, and disruption of platelet function [6],[32]-[34]. Some hematologic diseases are directly influenced by temperature changes; for example, cold agglutination disease exhibits an increase in cold agglutinin titers [35].
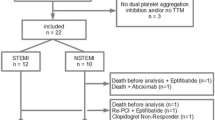
With more frequent use of hypothermia in clinical practice and concomitant use of platelet-inhibiting drugs, there is a growing need to understand the ramifications of platelet-inhibiting drugs on coagulation and platelet function [36],[37].
Effect of hypothermia on platelets
Platelet morphology
Chilling platelets (4°C) in vitro results in volume increase, spherical deformation, and the formation of lose marginal microtubules and pseudopods [38],[39]. The chilling-induced (0°C, ice water), reversible shape-change in platelets correlates with phosphorylation of myosin, subsequent interaction on actin filaments and free cytosolic calcium increase [40]. Human platelets can be maintained in a discoid shape in the cold, in vitro, using a cell-permeable calcium chelator to attenuate calcium mobilization and cytochalasin B to prevent barbed-end actin assembly [39]. FTIR spectroscopy in northern elephant seals confirms three different thermotropic membrane phase transitions [1]. The microtubules of hibernating mammals are more tolerant to cold, which facilitates the rapid shift from a thrombocytopenic, anticoagulant state during torpor to a normal state [3],[4].
Platelet function
Platelet adhesion and activation leads to their aggregation and ultimately to the formation of a fibrin-rich hemostatic plug [41]. Hypothermia promotes platelet margination by increasing hematocrit, changing platelet shape, lowering blood flow rate, and increasing the expression of adhesion molecules.
Low temperature enhances shear-induced platelet aggregation
Platelets interacting with the vessel wall are influenced by the small-scale motions of neighboring erythrocytes, which allows platelets to move across flow streamlines in a form of enhanced diffusion. Platelets contact each other via collisions driven by blood-flow velocity gradients [42]. Adhesive interactions between platelets and the extracellular matrix are strongly influenced by local rheological conditions. Blood is considered a two-phase liquid with a solid–liquid suspension. The viscosity of a liquid is temperature-dependent, and blood viscosity increases with decreasing temperature [43]. Thus low temperature may enhance shear-induced platelet aggregation by increasing blood viscosity [44].
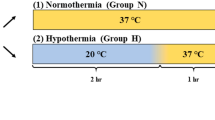
Hypothermia and life span of platelets
Chilled platelets subjected to refrigeration before transfusion rapidly leave circulation. Therefore, blood banks store platelets at room temperature [32],[45]. The normal in vivo lifespan of platelets (7–10 days) does not appear to be affected by hypothermia. A surface-induced deep hypothermia study (20°C) on dogs reported that the mean survival of platelets (4.9 days) is slightly but significantly longer in the hypothermic group compared to that in the control group (4.2 days) [46].
Storage, clearance and release underlies the (reversible) thrombocytopenia
The decrease in platelet count observed in vivo during hypothermia is reversible as normal body temperature is restored. This change in platelet count is explained by hepatic and splenic sequestration, and possibly margination of platelets, relative to hypothermic depth and duration, and with a maximum decline between 25-30°C [47]-[49]. Under mild hypothermia, the reduction in platelet count is modest and remains within the normal range [45]. As core body temperature drops below 37°C, platelets become more susceptible to activation by thrombotic stimuli, a phenomenon known as priming. Therefore, platelets can act as thermosensors. The ability for priming at peripheral body sites, where temperatures are lower and chances for trauma higher evolved as a protective effect against bleeding, whereas more central body sites (brain and coronary vessels) are more protected against thrombosis [39].
Subjecting platelets to chilling changes its surface configuration. In response to cooling, the GPIbα subunit of the vWf receptor complex undergoes clustering and becomes a target for recognition by hepatic macrophage complement receptor type 3 (CR3), which is strongly expressed in liver macrophages, and leads to platelet phagocytosis and clearance. Compared to mice that are CR3-deficient, mice overexpressing CR3 demonstrate a rapid reduction in platelets counts when exposed to cold leading to platelet phagocytosis and clearance in the liver [47].
vWF retention is prolonged on the cell surface at low temperatures
vWF is a protein that circulates in a globular form under conditions of low shear-stress, but changes into an elongated form under the influence of stronger hydrodynamic shear forces [50],[51]. Expression of vWF in endothelial cells is higher at low temperature than at normal temperature [52]. The kinetics of vWF proteolysis by the cleaving metalloprotease ADAMTS-13 is temperature-dependent, with slower but complete activity at 4°C and at 22°C. A sub-physiological temperature might influence the proteolysis kinetics due to minor variations in ADAMTS-13 structure, or further modification of the vWF substrate [53]. The failure of secreted vWF to form long cell-surface strings following its secretion at low temperatures (≤17°C) results in formation of predominantly globular deposits. This failure of vWF to unfurl at lower temperatures, combined with its reduced thermal motions, may interfere with the prolonged retention of this protein on the cell surface, and may result in hemostatic disorders [54].
The recognition of vWF with factor VIII is sensitive to temperature changes
Closely related to vWF is factor VIII which, after its extracellular release, forms a complex with vWF [51]. Thermodynamic analysis reveals that the recognition process of factor VIII with vWF is very sensitive to temperature changes. Generally, interactions between proteins with pre-optimized binding sites are stimulated by increases in the system kinetic energy (temperature). By contrast, interactions between proteins driven by conformational changes are generally reduced by temperature increases. The stimulatory effect of higher temperatures on the association kinetics and affinity of factor VIII for vWF suggests that this interaction does not require significant conformational changes [55]. The impact of body temperature changes on the recognition process of factor VIII with vWF is currently unknown.
Hypothermia increases the ability of platelets to respond to activating stimuli
Moderate hypothermia results in a minor increase in spontaneous platelet activation but a significant rise in agonist- induced responsiveness. In-vitro research in mice demonstrates that with incubation at temperatures of 34°C and 31°C, spontaneous expression of P-selectin and the activated conformation of GPIIb-IIIa does not change markedly. A small yet statistically significant increase in PAC-1 binding in unstimulated samples at 31°C suggested spontaneous hypothermia-induced activation. TRAP exposure during hypothermia causes an increase of PAC-1 binding with increased activation during hypothermia. In line with this, binding of fluorescent-labeled fibrinogen increases at 34°C and 31°C after TRAP exposure [56].
Although early research only referred to cold effects on platelets as “activation,” chilled platelets do not resemble platelets activated by classical agonists such as thrombin, ADP, or collagen. Whole blood aggregation assays demonstrated that platelet aggregation and P-selectin expression are enhanced under hypothermic temperatures but the effect depends on the agonist used. The potency of the agonist does not seem to be related to the susceptibility of platelets to the effects of temperature [57]-[68].
Interestingly, the platelet intrinsic function is maintained throughout torpor/arousal in hibernators as well as throughout cooling/rewarming and pharmacological induced torpor, as demonstrated by P-selectin expression and platelet aggregometry. P-selectin expression on circulating platelets, however, are significantly decreased in torpid hamsters, but restores to normal euthermic levels shortly after arousal [49].
Factors regulating thrombus formation may be tissue and temperature dependent
Mechanisms that limit or prevent the process of thrombus growth are essential in the balance between prothrombotic and antithrombotic forces. Cold-induced vasodilatation mediates cyclic regulation of blood flow during prolonged cooling of protruding limbs, reducing localized cold injury [69]. The protective effect of NO and prostacyclin on platelet aggregation during temperature-dependent vasoconstriction and vasodilation, is currently unknown but might be tissue and temperature dependent [70].
The machinery for executing platelet apoptosis is temperature dependent
Studies on the effects of chemotherapeutic drugs revealed that apoptosis in platelets, as determined by mitochondrial inner membrane potential depolarization is much more efficient at 37°C than at room temperature [71]. Cold-storage of platelets followed by rewarming has been shown to trigger apoptosis through a GN-sensitive GPIbα-change indicative of receptor clustering [72].
Conclusion
The impact of hypothermia on platelet function and its effect on hemostasis has been studied for more than 50 years, yet its effects and the mechanisms behind the observed phenomena have not been fully elucidated. Studies differ in the circumstances under which hypothermia is achieved, and in the duration and extent of temperature decrease. Comparative studies are challenging as the parameters defining sufficient platelet function have not been clearly identified, and experimental studies have not used standardized techniques and platelet-stimulating agents. Conflicting results suggest that the heterogeneous techniques do not accurately reflect in vivo hemostatic function, which involves platelets, coagulation factors, plasma proteins, endothelial and other cells and flow characteristics. Animal models may not be directly translatable to humans as demonstrated in hibernating mammals. The hypothermia-associated coagulopathy is more likely related to a reduced availability of platelet activators, rather than a consequence of an intrinsic defect in platelet function. More research is required to elucidate the activation of platelets, the interaction of platelets and leukocytes and the production of proinflammatory cytokines at different temperatures are required.
Abbreviations
- °:
-
Degrees
- C:
-
Celsius
- F:
-
Fahrenheit
- L:
-
Liter
- kDa:
-
kilodalton
- GP:
-
Glycoprotein
- vWF:
-
von Willebrand factor
- α:
-
alpha
- β:
-
beta
- FTIR:
-
Fourier transform infrared spectroscopy
- CR3:
-
Complement receptor type 3
- ADAMTS:
-
A disintegrin and metalloproteinase with thrombospondin motifs
- TRAP:
-
Thrombin receptor activating peptide
- ADP:
-
Adenosine diphosphate
- FeCl3:
-
Ferric chloride
- CPA:
-
Cone and platelet analyzer
- NO:
-
Nitric oxide
- PAF:
-
Platelet-activating factor
- BH:
-
Bcl-2 homology domain
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- ACT:
-
Activated clotting time
- TEG:
-
Thromboelastography
- ROTEM:
-
Rotational thromboelastometry
- MA:
-
Maximal amplitude
- MCF:
-
Maximum clot firmness
- PFA:
-
Platelet function analysis
- PAC-1:
-
Monoclonal antibody against GP IIb-IIIa
References
Field CL, Tablin F: Response of Northern Elephant Seal platelets to pressure and temperature changes: a comparison with human platelets. Comp Biochem Physiol A Mol Integr Physiol. 2012, 162: 289-295. 10.1016/j.cbpa.2012.01.023.
Hurd PL, van Anders SM: Latitude, digit ratios, and Allen’s and Bergmann’s rules: a comment on Loehlin, McFadden, Medland, and Martin (2006). Arch Sex Behav. 2007, 36: 139-141. 10.1007/s10508-006-9149-9. author reply 143
Cooper ST, Richters KE, Melin TE, Liu Z, Hordyk PJ, Benrud RR, Geiser LR, Cash SE, Shelley CS, Howard DR, Ereth MH, Sola-Visner MC: The hibernating 13-lined ground squirrel as a model organism for potential cold storage of platelets. Am J Physiol Regul Integr Comp Physiol. 2012, 302: R1202-R1208. 10.1152/ajpregu.00018.2012.
Britton SW: Extreme hypothermia in various animals and in man. Can Med Assoc J. 1930, 22: 257-261.
Lee S, Alston T: A little hypothermia goes a long way. Crit Care Med. 2012, 40: 1369-1370. 10.1097/CCM.0b013e31823b8b6a.
Díaz M, Becker DE: Thermoregulation: physiological and clinical considerations during sedation and general anesthesia. Anesth Prog. 2010, 57: 25-32. 10.2344/0003-3006-57.1.25. quiz 33–4
Guly H: History of accidental hypothermia. Resuscitation. 2011, 82: 122-125. 10.1016/j.resuscitation.2010.09.465.
Horosz B, Malec-Milewska M: Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2013, 45: 38-43. 10.5603/AIT.2013.0009.
Bratincsák A, Palkovits M: Activation of brain areas in rat following warm and cold ambient exposure. Neuroscience. 2004, 127: 385-397. 10.1016/j.neuroscience.2004.05.016.
Kurz A: Physiology of thermoregulation. Best Pract Res Clin Anaesthesiol. 2008, 22: 627-644. 10.1016/j.bpa.2008.06.004.
Schwertz H, Rowley JW, Tolley ND, Campbell RA, Weyrich AS: Assessing protein synthesis by platelets. Methods Mol Biol. 2012, 788: 141-153. 10.1007/978-1-61779-307-3_11. [Methods in Molecular Biology]
Jenne CN, Urrutia R, Kubes P: Platelets: bridging hemostasis, inflammation, and immunity. Int J Lab Hematol. 2013, 35: 254-261. 10.1111/ijlh.12084.
Horstman LL, Jy W, Ahn YS, Zivadinov R, Maghzi AH, Etemadifar M, Steven Alexander J, Minagar A: Role of platelets in neuroinflammation: a wide-angle perspective. J Neuroinflammation. 2010, 7: 10-10.1186/1742-2094-7-10.
Jurk K, Kehrel BE: Platelets: physiology and biochemistry. Semin Thromb Hemost. 2005, 31: 381-392. 10.1055/s-2005-916671.
Gawaz M: Intelligent platelet inhibitors are on the horizon. Arterioscler Thromb Vasc Biol. 2011, 31: 1949-1950. 10.1161/ATVBAHA.111.232173.
Topcic D, Kim W, Holien JK, Jia F, Armstrong PC, Hohmann JD, Straub A, Krippner G, Haller CA, Domeij H, Hagemeyer CE, Parker MW, Chaikof EL, Peter K: An activation-specific platelet inhibitor that can be turned on/off by medically used hypothermia. Arter Thromb Vasc Biol. 2011, 31: 2015-2023. 10.1161/ATVBAHA.111.226241.
Han HS, Park J, Kim J-H, Suk K: Molecular and cellular pathways as a target of therapeutic hypothermia: pharmacological aspect. Curr Neuropharmacol. 2012, 10: 80-87. 10.2174/157015912799362751.
Hall R, Mazer CD: Antiplatelet drugs: a review of their pharmacology and management in the perioperative period. Anesth Analg. 2011, 112: 292-318. 10.1213/ANE.0b013e318203f38d.
Johansson BW: Drugs affect and are affected by body temperature. Lakartidningen. 2001, 98: 2178-2181.
Mackowiak PA, Wasserman SS, Levine MM: A critical appraisal of 98.6°F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA. 1992, 268: 1578-1580. 10.1001/jama.1992.03490120092034.
Krajewski S, Kurz J, Geisler T, Peter K, Wendel HP, Straub A: Combined blockade of ADP receptors and PI3-kinase p110beta fully prevents platelet and leukocyte activation during hypothermic extracorporeal circulation. PLoS One. 2012, 7: e38455-10.1371/journal.pone.0038455.
Marx J: Rosen’s emergency medicine: concepts and clinical practice. Mosby/Elsevier; 2006:2239.
Fröbert O, Christensen K, Fahlman A, Brunberg S, Josefsson J, Särndahl E, Swenson JE, Arnemo JM: Platelet function in brown bear (Ursus arctos) compared to man. Thromb J. 2010, 8: 11-10.1186/1477-9560-8-11.
Storey KB: Out cold: biochemical regulation of mammalian hibernation - a mini-review. Gerontology. 2010, 56: 220-230. 10.1159/000228829.
Morrison JJ, Ross JD, Poon H, Midwinter MJ, Jansen JO: Intra-operative correction of acidosis, coagulopathy and hypothermia in combat casualties with severe haemorrhagic shock. Anaesthesia. 2013, 68: 846-850. 10.1111/anae.12316.
Mohr J, Ruchholtz S, Hildebrand F, Flohé S, Frink M, Witte I, Weuster M, Fröhlich M, van Griensven M, Keibl C, Mommsen P: Induced hypothermia does not impair coagulation system in a swine multiple trauma model. J Trauma Acute Care Surg. 2013, 74: 1014-1020. 10.1097/TA.0b013e3182826edd.
Kheirbek T, Kochanek AR, Alam HB: Hypothermia in bleeding trauma: a friend or a foe?. Scand J Trauma Resusc Emerg Med. 2009, 17: 1-15. 10.1186/1757-7241-17-65.
Meex I, Dens J, Jans F, Boer W, Vanhengel K, Vundelinckx G, Heylen R, De Deyne C: Cerebral tissue oxygen saturation during therapeutic hypothermia in post-cardiac arrest patients. Resuscitation. 2013, 84: 788-793. 10.1016/j.resuscitation.2013.01.003.
Absalom AR, Scheeren TWL: NIRS during therapeutic hypothermia: cool or hot?. Resuscitation. 2013, 2013: 95-96.
Frink M, Flohé S, Van Griensven M, Mommsen P, Hildebrand F: Facts and fiction: the impact of hypothermia on molecular mechanisms following major challenge. Mediat Inflamm. 2012, 2012: 762840-
Broessner G, Fisher M, Schubert G, Metzler B, Schmutzhard E: Update on therapeutic temperature management. Crit Care. 2012, 16 (Suppl 2): 1-42.
Palmiere C, Bardy D, Letovanec I, Mangin P, Augsburger M, Ventura F, Iglesias K, Werner D: Biochemical markers of fatal hypothermia. Forensic Sci Int. 2013, 226: 54-61. 10.1016/j.forsciint.2012.12.007.
Brändström H, Eriksson A, Giesbrecht G, Angquist K-A, Haney M: Fatal hypothermia: an analysis from a sub-arctic region. Int J Circumpolar Health. 2012, 71: 1-7. 10.3402/ijch.v71i0.18502.
Escalda A, Marques M, Silva-Carvalho L, Barradas MA, Silva-Carvalho J, Cruz JM, Mikhailidis DP: Hypothermia-induced haemostatic and biochemical phenomena. An experimental model. Platelets. 1993, 4: 17-22. 10.3109/09537109309013191.
Heni M, Saur SJ: Blood clotting at room temperature in cold agglutinin disease. Blood. 2013, 121: 4975-4975. 10.1182/blood-2012-12-472324.
Penela D, Magaldi M, Fontanals J, Martin V, Regueiro A, Ortiz JT, Bosch X, Sabaté M, Heras M: Hypothermia in acute coronary syndrome: brain salvage versus stent thrombosis?. J Am Coll Cardiol. 2013, 61: 686-687. 10.1016/j.jacc.2012.10.029.
Polderman KH: Hypothermia and coagulation. Crit Care. 2012, 16 (Suppl 2): A20-10.1186/cc11278.
Andrews RK, Berndt MC: Platelet physiology: in cold blood. Curr Biol. 2003, 13: R282-R284. 10.1016/S0960-9822(03)00202-1.
Winokur R, Hartwig JH: Mechanism of shape change in chilled human platelets. Blood. 1995, 85: 1796-1804.
Kawakami H, Higashihara M, Ohsaka M, Miyazaki K, Ikebe M, Hirano H: Myosin light chain phosphorylation is correlated with cold-induced changes in platelet shape. J Smooth Muscle Res. 2001, 37: 113-122. 10.1540/jsmr.37.113.
Broos K, Feys HB, De Meyer SF, Vanhoorelbeke K, Deckmyn H: Platelets at work in primary hemostasis. Blood Rev. 2011, 25: 155-167. 10.1016/j.blre.2011.03.002.
Grabowski EF, Yam K, Gerace M: Evaluation of hemostasis in flowing blood. Am J Hematol. 2012, 87 (Suppl 1): S51-S55. 10.1002/ajh.23207.
Baskurt OK, Meiselman HJ: Blood rheology and hemodynamics. Semin Thromb Hemost. 2003, 29: 435-450. 10.1055/s-2003-44551.
Zhang J, Wood J, Bergeron AL, McBride L, Ball C, Yu Q, Pusiteri AE, Holcomb JB, Dong J: Effects of low temperature on shear-induced platelet aggregation and activation. J Trauma Inj Infect Crit Care. 2004, 57: 216-223. 10.1097/01.TA.0000093366.98819.FE.
Egidi MG, D’Alessandro A, Mandarello G, Zolla L: Troubleshooting in platelet storage temperature and new perspectives through proteomics. Blood Transfus. 2010, 8 (Suppl 3): s73-s81.
Hessel EA, Schmer G, Dillard DH: Kinetics during Deep Hypothermia. J Surg Res. 1980, 34: 23-34. 10.1016/0022-4804(80)90078-5.
Hoffmeister KM, Felbinger TW, Denis V, Bergmeier W, Mayadas TN, Von Andrian UH, Wagner DD, Stossel TP, Hartwig JH: The clearance mechanism of chilled blood platelets Brigham and women’ s hospital. Cell. 2003, 112: 87-97. 10.1016/S0092-8674(02)01253-9.
Ao H, Moon JK, Tashiro M, Terasaki H: Delayed platelet dysfunction in prolonged induced canine hypothermia. Resuscitation. 2001, 51: 83-90. 10.1016/S0300-9572(01)00380-X.
De Vrij EL, Vogelaar PC, Goris M, Houwertjes MC, Herwig A, Dugbartey GJ, Boerema AS, Strijkstra AM, Bouma HR, Henning RH: Platelet dynamics during natural and pharmacologically induced torpor and forced hypothermia. PLoS One. 2014, 9: e93218-10.1371/journal.pone.0093218.
Tanaka KA, Key NS, Levy JH: Blood coagulation: hemostasis and thrombin regulation. Anesth Analg. 2009, 108: 1433-1446. 10.1213/ane.0b013e31819bcc9c.
Lenting PJ, Casari C, Christophe OD, Denis CV: von Willebrand factor: the old, the new and the unknown. J Thromb Haemost. 2012, 10: 2428-2437. 10.1111/jth.12008.
Ai X, Gu Y: The effect of low temperature on von Willbrand factor expression of cultured human umbilical vein endothelial cells. Chin J Surg. 1997, 35: 597-599.
Perutelli P, Amato S, Molinari AC: Cleavage of von Willebrand factor by ADAMTS-13 in vitro: effect of temperature and barium ions on the proteolysis kinetics. Blood Coagul Fibrinolysis. 2005, 16: 607-611. 10.1097/01.mbc.0000187251.32630.1f.
Carter T, Mashanov G, Ogden D, Zupančič G, Hannah MJ, Hewlett L, Knipe L: Temperature-dependence of weibel-palade body exocytosis and cell surface dispersal of von Willebrand factor and its propolypeptide. PLoS One. 2011, 6: e27314-10.1371/journal.pone.0019177.
Dimitrov JD, Christophe OD, Kang J, Repessé Y, Delignat S, Kaveri SV, Lacroix-Desmazes S: Thermodynamic analysis of the interaction of factor VIII with von Willebrand factor. Biochemistry. 2012, 51: 4108-4116. 10.1021/bi300232d.
Lindenblatt N, Menger MD, Klar E, Vollmar B: Sustained hypothermia accelerates microvascular thrombus formation in mice. Am J Physiol Heart Circ Physiol. 2005, 289: H2680-H2687. 10.1152/ajpheart.00425.2005.
Berger G, Hartwell DW, Wagner DD: P-Selectin and platelet clearance. Blood. 1998, 92: 4446-4452.
Michelson AD, MacGregor H, Barnard MR, Kestin AS, Rohrer MJ, Valeri CR: Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994, 71: 633-640.
Faraday N, Rosenfeld B: In vitro hypothermia enhances platelet GPIIb-IIIa activation and P-selectin expression. Anesthesiology. 1998, 88: 1579-1585. 10.1097/00000542-199806000-00022.
Scharbert G, Kalb ML, Essmeister R, Kozek-Langenecker SA: Mild and moderate hypothermia increases platelet aggregation induced by various agonists: a whole blood in vitro study. Platelets. 2010, 21: 44-48. 10.3109/09537100903420269.
Frelinger AL, Furman MI, Barnard MR, Krueger LA, Dae MW, Michelson AD: Combined effects of mild hypothermia and glycoprotein IIb/IIIa antagonists on platelet-platelet and leukocyte-platelet aggregation. Am J Cardiol. 2003, 92: 1099-1101. 10.1016/j.amjcard.2003.06.007.
Högberg C, Erlinge D, Braun OÖ: Mild hypothermia does not attenuate platelet aggregation and may even increase ADP-stimulated platelet aggregation after clopidogrel treatment. Thromb J. 2009, 7: 2-10.1186/1477-9560-7-2.
Lantz N, Hechler B, Ravanat C, Cazenave J-P, Gachet C: A high concentration of ADP induces weak platelet granule secretion independently of aggregation and thromboxane A2 production. Thromb Haemost. 2007, 98: 1145-1147.
Xavier RG, White AE, Fox SC, Wilcox RG, Heptinstall S: Enhanced platelet aggregation and activation under conditions of hypothermia. Thromb Haemost. 2007, 98: 1266-1275.
Straub A, Krajewski S, Hohmann JD, Westein E, Jia F, Bassler N, Selan C, Kurz J, Wendel HP, Dezfouli S, Yuan Y, Nandurkar H, Jackson S, Hickey MJ, Peter K: Evidence of platelet activation at medically used hypothermia and mechanistic data indicating ADP as a key mediator and therapeutic target. Arter Thromb Vasc Biol. 2011, 31: 1607-1616. 10.1161/ATVBAHA.111.226373.
Scharbert G, Kalb M, Marschalek C, Kozek-Langenecker SA: The effects of test temperature and storage temperature on platelet aggregation: a whole blood in vitro study. Anesth Analg. 2006, 102: 1280-1284. 10.1213/01.ane.0000199399.04496.6d.
Wang X: Comparative analysis of various platelet glycoprotein IIb/IIIa antagonists on shear-induced platelet activation and adhesion. Blood. 2002, 100: 61B-
Wolberg AS, Meng ZH, Monroe DM, Hoffman M: A systematic evaluation of the effect of temperature on coagulation enzyme activity and platelet function. J Trauma Inj Infect Crit Care. 2004, 56: 1221-1228. 10.1097/01.TA.0000064328.97941.FC.
Wallin BG: Neural control of human skin blood flow. J Auton Nerv Syst. 1990, 30 (Suppl): S185-S190. 10.1016/0165-1838(90)90128-6.
Evora PRB, Cable DG, Chua YL, Rodrigues AJ, Pearson PJ, Schaff HV: Nitric oxide and prostacyclin-dependent pathways involvement on in vitro induced hypothermia. Cryobiology. 2007, 54: 106-113. 10.1016/j.cryobiol.2006.12.002.
Gyulkhandanyan AV, Mutlu A, Freedman J, Leytin V: Selective triggering of platelet apoptosis, platelet activation or both. Br J Haematol. 2013, 161: 245-254. 10.1111/bjh.12237.
van der Wal DE, Du VX, Lo KSL, Rasmussen JT, Verhoef S, Akkerman JWN: Platelet apoptosis by cold-induced glycoprotein Ibα clustering. J Thromb Haemost. 2010, 8 (11): 2554-2562. 10.1111/j.1538-7836.2010.04043.x.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The authors declare that they have no competing interests.
Authors’ contributions
All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Van Poucke, S., Stevens, K., Marcus, A.E. et al. Hypothermia: effects on platelet function and hemostasis. Thrombosis J 12, 31 (2014). https://doi.org/10.1186/s12959-014-0031-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-014-0031-z