Abstract
Background
Placenta previa describes a placenta that extends partially or completely over the internal cervical oss. Placenta previa is one of the leading causes of widespread postpartum hemorrhage and maternal mortality worldwide. Another cause of bleeding in pregnant women is Placenta accreta spectrum. Therefore, the aim of the present systematic review and meta-analysis is to determine the effect of prophylactic balloon occlusion of the internal iliac arteries in patients with placenta previa or placental accreta spectrum (PAS).
Methods
In this systematic review and meta-analysis, to identify and select relevant studies, the SID, MagIran, ScienceDirect, Embase, Scopus, PubMed, Web of Science, and Google Scholar databases were searched, using the keywords of internal iliac artery balloon, placenta, previa, balloon, accreta, increta and percreta, without a lower time limit and until 2020. The heterogeneity of the studies was examined using the I2 index, and subsequently a random effects model was applied. Data analysis was performed within the Comprehensive Meta-Analysis software (version 2).
Results
In the review of 29 articles with a total sample size of 1140 in the control group, and 1225 in the balloon occlusion group, the mean difference between the two groups was calculated in terms of Intraoperative blood loss index (mL) and it was derived as 3.21 ± 0.38; moreover, in 15 studies with a sample size of 887 in the control group, and 760 in the balloon occlusion group, the mean difference between the two groups in terms of gestation index (weeks) was found as 2.84 ± 0.49; and also with regards to hysterectomy balloon occlusion after prophylactic closure of the iliac artery, hysterectomy (%) balloon occlusion was calculated as 8.9 %, and this, in the hysterectomy control group (%) was obtained as 31.2 %; these differences were statistically significant and showed a positive effect of the intervention (P < 0.05).
Conclusion
The results of this study show that the use of prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum has benefits such as reduced intraoperative blood loss, reduced hysterectomy and increased gestation (weeks), which can be considered by midwives and obstetricians.
Similar content being viewed by others
Background
Placenta previa is a type of placenta that extends partially or completely over the internal cervical oss [1]. Placenta previa is one of the leading causes of widespread postpartum hemorrhage and maternal mortality worldwide [2]. The prevalence of placenta previa in women is 0.56 % [3]. The risk of hysterectomy after cesarean delivery in the case of placenta previa is 3.5 %, which is higher compared to mothers without it. Increasing the rate of cesarean delivery due to placenta previa has a significant effect on the cost of gynecological medical care [4]. The main cause of placenta previa is unknown. Maternal age, previous cesarean section, abortion, uterine myoma, high body mass index, high infant weight, male fetal, maternal tobacco use, and history of uterine surgery are among the predisposing factors of this disease [5].
Another cause of bleeding in pregnant women is placental adhesions. placental adhesions is an abnormal invasion of the placenta to the uterine wall and is classified as accreta, percreta, or increta depending on the degree of invasion of the myometrium [5, 6]. The prevalence of placental accreta spectrum in the third trimester in pregnant women is between 0.3 and 2 %; this is a life-threatening condition and approximately 90 % of these patients require blood transfusion [7, 8]. In many countries around the world, cesarean section is a growing trend that has increased cases of placental adhesions, which in turn has increases concerns [7].
Establishing homeostasis in placenta requires the use of surgical techniques. These methods include multiple placement of hemostatic sutures in the placental bed, compression sutures of the uterus with or without intrauterine balloon tamponade, use of FLOSEAL in the placental bed, and uterin artery lrgation [9,10,11,12,13]. If these surgical procedures to control bleeding are unsuccessful, hysterectomy is the usual solution to save the patient’s life [14]. However, extensive bleeding often makes surgical treatment even more challenging. Therefore, preventive measures to reduce bleeding can be beneficial [9]. Recently, preoperative placement of internal iliac artery catheters with intraoperative arterial balloon occlusion has become a common preventive procedure [15].
Collapsed intra-arterial balloons do not completely block blood flow to the uterus, yet they lower blood pressure to the site of obstruction. By reducing the amount of bleeding, hemostatic methods can be more practical [16,17,18,19,20,21,22]. Obstructive balloon occlusion was first described by Dubois et al. as, and has since led to dissimilar outcomes in patients with adhesions, making it a controversial procedure [23]. Nonetheless, the advantages of this method include reducing bleeding in the area of surgery to achieve homeostasis or hysterectomy [24].
Considering the importance of reducing bleeding due to placenta previa and Placenta accreta spectrum to reduce their mortality among pregnant women, and also due to the inconsistent results from research in this area, this systematic review and meta-analysis aimed to determine the effect prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum.
Methods
In this meta-analysis, the SID, MagIran, ScienceDirect, Embase, Scopus, PubMed, Web of Science and Google Scholar databases were searched to identify and select relevant studies. The keywords used were: internal iliac artery balloon, placenta, previa, balloon, accreta, increta, and percreta, and all possible combinations of these words. No time constraints were considered in the search. The information of the identified articles was transferred into the EndNote bibliography management software (EndNote X8). In order to maximize the comprehensiveness of the search, the lists of references used within all identified articles were manually reviewed.
Inclusion criteria
Studies that examined the effect prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum, interventional studies, and studies for which a full text was available.
Exclusion criteria
Unrelated studies, studies without sufficient data, duplicate papers, studies with an unclear methodology.
Study selection
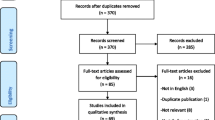
Initially, duplicate studies in various databases were excluded from this study, and only one copy was retained. Then a list of the titles of all the remaining articles was prepared, for further analysis. In the first stage, screening, the title and abstract of the remaining articles were carefully examined, and a number of articles were removed considering the inclusion and exclusion criteria. In the second stage, i.e. eligibility evaluation, the full text of the studies, remaining from the screening stage, were thoroughly examined according to the criteria, and similarly, a number of other unrelated studies were excluded. To prevent subjectivity, article review, and data extraction activities were performed by two reviewers, independently. If an article was not included, the reason for excluding it was mentioned. In cases where there was a disagreement between the two reviewers, a third person reviewed the article.
Quality evaluation
In order to examine the quality of the remaining articles (i.e. methodological validity and results), a checklist appropriate to the type of study was adopted. STROBE checklists are commonly used to critique and evaluate the quality of observational studies. The checklist consists of six scales/general sections that are: title, abstract, introduction, methods, results, and discussion. Some of these scales have subscales, resulting in a total of 32 fields (subscales). In fact, these 32 fields represent different methodological aspects of a piece of research. Examples of subscales include title, problem statement, study objectives, study type, statistical population, sampling method, sample size, the definition of variables and procedures, data collection method(s), statistical analysis techniques, and findings. Accordingly, the maximum score that can be obtained during the quality evaluation phase and using the STROBE checklist is 32. By considering the score of 16 as the cut-off point [25], any article with a score of 16 or above is considered as a medium or a high-quality article.
Data extraction
Information on all final articles was extracted from a different pre-prepared checklist. This checklist includes article title, first author’s name, year of publication, sample size, place of study, maternal age (years), intraoperative blood loss (mL), blood transfusion (units), blood transfusion volume (ml), placenta type, and gestation (weeks), Hysterectomy (%).
Statistical analysis
Frequency and percentage as well as the standardized mean difference indices were used to combine the results of different studies. The I2 test was used to evaluate the homogeneity between studies, and due to the found heterogeneity in the studies, a random effects model was used to combine the studies and perform the meta-analysis. When the I2 index is less than 25 %, heterogeneity was considered as low; between 25 and 275 %, this was considered as moderate heterogeneity, and more than 75 % as high heterogeneity. P value less than 0.05 was considered significant. The Egger’s test and corresponding funnel plots were also used to examine the publication bias. Data analysis was performed within the Comprehensive Meta-Analysis software (version 2).
Results
The study selection process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Based on the initial search in the database, 295 possible related articles were identified and transferred into the EndNote bibliography management software. Moreover, 12 further studies were added after reviewing the lists of references of the identified articles. Out of a total of 307 identified studies, 69 studies were duplicates and were therefore excluded. In the screening phase, out of the remaining 238 studies, 88 articles were removed after examining their titles and abstracts, and based on the inclusion and exclusion criteria. In the eligibility evalaution stage, out of the remaining 150 studies, 115 irrelevant articles were removed by studying the full text of the articles and in accordance with the inclusion and exclusion criteria. In the quality evaluation stage, by reading the full text of the article and based on the score obtained from the STROBE checklist, out of the remaining 35 studies, 6 low quality studies were omitted. Finally, 29 articles that were published between 2006 and August 2020 entered the analysis stage (Fig. 1).
The sample size of the balloon occlusion group was 1225, and the sample size in the control group was 1140. The characteristics of the eligible studies included in the systematic review and meta-analysis are provided in Table 1 (Table 1).
Intraoperative blood loss index (mL)
The first criterion for comparison was the intraoperative blood loss index (mL). In 26 studies [15, 20, 24, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40, 42,43,44,45, 47,48,49,50] prophylactic internal iliac artery balloon occlusion significantly reduced this index in the balloon occlusion group compared to the control group (P < 0.05). According to the results of studies by Yu et al. (2020) [9], Feng et al. (2017) [41] and McGinnis et al. (2019) [46], no significant difference was observed between the control group and the balloon occlusion group with respect to this index (P > 0.05).
Based on the results of I2 test, in the study of intraoperative blood loss index (mL), there was a heterogeneity between the control group and the case group (I2 = 97.4), thus, a random effects method was applied to amalgamate the results of all studies and approximate a final result. Based on the results of the meta-analysis, the mean difference of intraoperative blood loss (mL) in the balloon occlusion, and control groups were obtained as 1436 ± 211 and 403 ± 2503 respectively. Therefore, prophylactic internal iliac artery balloon occlusion reduces postpartum hemorrhage (Figs. 2 and 3). The graph of the mean difference between intraoperative blood loss (mL) in the case and control groups was 3.21 ± 0.38, which shows the positive effect of the intervention. The width of the horizontal line on each square denotes a 95 % confidence interval. Published bias was assessed using the Egger’s test, which showed no publication bias (P = 0.053).
Blood transfusion index (units)
The second criterion is the comparison was blood transfusion index (units). In the studies of Dai et al. (2018) [34], Picel et al. (2018) [37], El-sayed et al. (2016) [39], Dai et al. (2020) [43], McGinnis et al. (2019) [46], Panici et al. (2012) [47] and Zeng et al. (2017) [50] significant differences between the control group and the balloon occlusion group in terms of blood transfusion index (units) ( P < 0.05) was observed. However, in reviewing the results of studies by Yu et al. (2020) [9], Darwish et al. (2014) [27], Omar et al. (2017) [28], Broekman et al. (2015) [30], Bodner et al. (2006) [36] and Feng et al. (2017) [41], no significant difference was observed between the control group and the balloon occlusion group in terms of this index (P > 0.05). Therefore, reduction of blood transfusion index (units) in the balloon occlusion group is not definite, and varies according to the study conditions. Thus, with respect to blood transfusion index (units), it can be argued that prophylactic internal iliac artery balloon occlusion has no advantage.
Gestation index (weeks)
The third criterion for comparison was gestation index (weeks). In 14 studies [9, 15, 24, 26, 30, 32, 33, 40,41,42,43, 46, 47, 50] prophylactic internal iliac artery balloon occlusion did not significantly increased this index in the balloon occlusion group compared to the control group (P˃0.05), while in the study results of Darwish et al. (2014) [27], Ono et al. (2018) [35], Bodner et al. (2006) [36] and Tan et al. (2017) [45], there was a significant difference between the control group and the balloon occlusion group in terms of gestation index (weeks) (P < 0.05).
Based on the results of I2 test, in the study of gestation index (weeks), there was heterogeneity between the control group (I2 = 99.1), thus, a random effects model was applied to combine the results of the studies and approximate a single final outcome. Based on the results of meta-analysis, mean of gestation (weeks) in the balloon occlusion and control groups were 37.0 ± 0.18 and 35.9 ± 0.17 respectively. Therefore, it can be concluded that prophylactic internal iliac artery balloon occlusion increases the gestation index (weeks). The mean difference between the two groups was 2.84 ± 0.49, which indicates the positive effect of the intervention. Figure 4 presents the forest plot for gestation (weeks) for different studies, as well as their confidence intervals. The horizontal line on each square also represents the 95 % confidence interval. Publication bias was assessed using the Egger’s test, which showed no bias in the studies (P = 0.055) (Figs. 4 and 5).
Hysterectomy index (%)
The third criterion for comparison was the hysterectomy index (%). In 8 studies [24, 31, 34, 38, 40, 42, 47, 50] prophylactic internal iliac artery balloon occlusion significantly reduced this index in the balloon occlusion group compared to the control group (P < 0.05). While reviewing the results of studies by Omar et al. (2017) [28], Jiang et al. (2013) [29], Fan et al. (2017) [33], Dai et al. (2020) [43], Zhou et al. (2019) [15], and Cho et al. (2020) [48], no significant difference was observed between the control group and the balloon occlusion group in terms of hysterectomy index (%) (P˃0.05).
Based on the results of I2 test, in the study of hysterectomy index (%), there was a heterogeneity between the control group and the case group (I2 = 74.9), (I2 = 87.5), thus, a random effects method was applied to combine the results of the studies and approximate an overall. Based on the results of meta-analysis; the percentages of hysterectomy (%) in the balloon occlusion and control groups were 8.9 % and and 31.2 % respectively. Therefore, it can be concluded that prophylactic internal iliac artery balloon occlusion reduces the hysterectomy index (%), which indicates the positive effect of the intervention. The horizontal line on each square, in the hysterectomy forest plot, represents the 95 % confidence interval (Figs. 6 and 7). Publication bias was assessed using the Egger’s test, which shows no publication bias (P = 0.294) (P = 0.499) (Figs. 8 and 9).
Discussion
The aim of the present systematic review and meta-analysis was to determine the effect of prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum.
Bleeding is still a major cause of maternal death following childbirth. In many developed countries, bleeding is the most important factor in admitting a pregnant woman to an intensive care unit (ICU). In developing countries, bleeding is the cause of almost half of all maternal mortality [51]. Placenta previa is one of the causes of obstetric bleeding, which, by definition, is a placenta that covers the inner passageway of the cervix [51]. Placenta previa is a known risk factor for placenta accrete [52]; In a case-control study, placental bed biopsy was performed during cesarean section in 50 women with placenta previa and 50 cases with normal placenta. In approximately half of the placenta samples, spiral myometrium had infiltrating trophoblast giant cells, while only 20 % of samples related to normal pair, had such changes [53]. The placenta is an abnormal attachment of all or part of the placenta to uterine wall [54]. Due to the partial or complete absence of regular decidua and the incomplete development of the fibrinoid layer or the nitabuch membrane, the placental feathers stick to the myometrium. In the placenta increta, the villi enter the myometrium, and in the placenta increta, the villi invade the cervix or other pelvic organs. Different types of abnormal Placenta accreta spectrum are important causes of maternal mortality, due to bleeding during pregnancy or postpartum [51].
According to the present systematic review and meta-analysis, the mean difference of the two groups in terms of intraoperative blood loss (mL) was obtained 3.21 ± 0.38, and this difference was statistically significant. This also showed a positive effect of the intervention. The most valid study in terms of sample size, was a research conducted by Wu et al. (2016) [40], in which the authors reported that the intraoperative blood loss (mL) index in the case group was 921 ± 199 ml, whilst this 2790 ± 335 ml in the control group; the findings were statistically significant and consistent with the results of the present study.
Timely transfusion of blood and blood products can save the lives of these patients. Therefore, the use of a variety of blood products, can be prevent the risk of death in 15,000 pregnancies per year, globally [55]. Since blood reserves are sourced by donations, and this vital tissue requires different and sometimes rare blood types, proper management of blood transfusion can prevent surgery delays or even cancellations [56].
In 7 studies [34, 37, 39, 43, 46, 47, 50], a significant difference was reported between the control group and the balloon occlusion group in terms of blood transfusion index (units) (P < 0.05). However, in the results of 6 studies [9, 27, 28, 30, 36, 41], no significant difference was observed between the two groups (P > 0.05). According to the results results, the decrease in blood transfusion index (units) in the balloon occlusion group is not definite and varies according to the study conditions. Therefore, in terms of Blood transfusion index (units), it can be stated that prophylactic internal iliac artery balloon occlusion has no advantage.
Premature birth or gestational age less than 37 weeks from the last date of maternal menstruation is one of the most important indicators of health in any society, and the survival of newborns is directly related to gestational age and birth weight [57]. The prevalence of preterm birth varies in different societies, and statistics show that 8 to 10 % of infants born in the United States, and 5 to 7 % in Europe are born premature [58]. Various factors are involved in the birth of premature infants, including maternal, fetal, etc. [59]. Maternal causes such as maternal disease, chorioamnionitis, multiple births and maternal smoking, Placenta accreta spectrum, placenta previa, uterine defects, etc. can be mentioned [60].
According to the present systematic review and meta-analysis, the mean difference of the two groups in terms of gestation index (weeks) was 2.84 ± 0.49 which was statistically significant, and showed a positive effect of the intervention. The most valid study in terms of sample size was conducted by Wu et al. (2016) [40], which reported that the gestation index (weeks) in the case and control groups were 35.6 ± 1.3 and 35.5 ± 1.5 weeks respectively, which was not statistically significant; the results of the study was also not consistent with the general findings of the present work.
Hysterectomy is a major surgery that is almost always performed in cases of severe, life-threatening bleeding after vaginal delivery or cesarean section [61]. Its prevalence in the last century has been 1.4 ± 0.24 cases per 1000 live births [62]. Risk factors for emergency hysterectomy around delivery include abnormal Placenta adhesiens (percreta, increta, placenta accreta), placenta previa, uterine atony, previous cesarean section, and uterine rupture [63]. The most common cause reported in some studies was abnormal placental adherence with placenta previa in patients with a history of previous cesarean section [64, 65]. This surgery is associated with high maternal mortality even with modern midwifery [66]. Complications such as blood transfusion, fever, DIC and re-laparotomy in high rates, and maternal mortality have been reported in different studies [64, 65, 67].
According to the present systematic review and meta-analysis, the percentage of hysterectomy (%) in the balloon occlusion and hysterectomy control groups were 8.9 % and 31.2 % respectively, which was statistically significant and, showed a positive effect of the intervention. The most comprehensive study in terms of sample size was conducted by Wu et al. (2016) [40], who reported hysterectomy index (%) of 0 % in the case group and 7.89 % in the control group, which was statistically significant and is in line with the general findings of the present study.
In general, according to the present systematic review and meta-analysis; prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum has benefits, such as reduced intraoperative blood loss, reduced hysterectomy, and increased gestation (weeks). Therefore, the procedure can be applied prophylactically by obstetricians and gynecologists.
One of the limitations of this study is that some samples were not based on random selection. Moreover, the non-uniform reporting of articles, and methods of implementation, lack of consistency in the data analysis, incomplete data, and the unavailability of the full text of some of the papers presented at the conferences can be mentioned.
Conclusions
The results of this study show that prophylactic internal iliac artery balloon occlusion in patients with placenta previa or Placenta accreta spectrum has benefits such as reduced intraoperative blood loss, reduced hysterectomy and increased gestation (weeks), which can be considered by midwives and obstetricians.
Availability of data and materials
Datasets are available through the corresponding author upon reasonable request.
Abbreviations
- PAS:
-
Placental accreta spectrum
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology for cross- sectional Study
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
References
Carusi DA, Fox KA, Lyell DJ, Perlman NC, Aalipour S, Einerson BD, et al. Placenta Accreta Spectrum Without Placenta Previa. Obstetrics & Gynecology. 2020.
Sadashivaiah J, Wilson R, Thein A, McLure H, Hammond C, Lyons G. Role of prophylactic uterine artery balloon catheters in the management of women with suspected placenta accreta. Int J Obstet Anesth. 2011;20(4):282–7.
Jauniaux E, Grønbeck L, Bunce C, Langhoff-Roos J, Collins SL. Epidemiology of placenta previa accreta: a systematic review and meta-analysis. BMJ open. 2019;9(11).
Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R. Maternal complications with placenta previa. Am J Perinatol. 2000;17(02):101–6.
Practice CoO. The American College of Obstetricians and Gynecologists Committee opinion no. 630. Screening for perinatal depression. Obstetrics gynecology. 2015;125(5):1268.
Dilauro M, Dason S, Athreya S. Prophylactic balloon occlusion of internal iliac arteries in women with placenta accreta: literature review and analysis. Clinical radiology. 2012;67(6):515–20.
Tan YL, Suharjono H, Lau N, Voon HY. Prophylactic bilateral internal iliac artery balloon occlusion in the management of placenta accreta: a 36-month review. Med J Malaysia. 2016;71(3):111–6.
Anderson-Bagga FM, Sze A. Placenta previa. StatPearls [Internet]: StatPearls Publishing; 2019.
Yu SCH, Cheng YKY, Tse WT, Sahota DS, Chung MY, Wong SSM, et al. Perioperative prophylactic internal iliac artery balloon occlusion in the prevention of postpartum hemorrhage in placenta previa: a randomized controlled trial. American Journal of Obstetrics and Gynecology. 2020.
Cahill AG, Beigi R, Heine RP, Silver RM, Wax JR, Obstetricians ACo, et al. Placenta accreta spectrum. American journal of obstetrics gynecology. 2018;219(6):B2–16.
Jauniaux E, Collins S, Burton GJ. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. American journal of obstetrics gynecology. 2018;218(1):75–87.
Brosens I, Puttemans P, Benagiano G. Placental bed research: I. The placental bed: from spiral arteries remodeling to the great obstetrical syndromes. American journal of obstetrics gynecology. 2019;221(5):437–56.
Jauniaux E, Collins SL, Jurkovic D, Burton GJ. Accreta placentation: a systematic review of prenatal ultrasound imaging and grading of villous invasiveness. American journal of obstetrics gynecology. 2016;215(6):712–21.
Chen M, Lv B, He G, Liu X. Internal iliac artery balloon occlusion during cesarean hysterectomy in women with placenta previa accreta. International Journal of Gynecology Obstetrics. 2019;145(1):110–5.
Zhou Xe, Sun X, Wang M, Huang L, Xiong W. The effectiveness of prophylactic internal iliac artery balloon occlusion in the treatment of patients with pernicious placenta previa coexisting with placenta accreta. The Journal of Maternal-Fetal & Neonatal Medicine. 2019:1–6.
Hansch E, Chitkara U, McAlpine J, El-Sayed Y, Dake MD, Razavi MK. Pelvic arterial embolization for control of obstetric hemorrhage: a five-year experience. American journal of obstetrics gynecology. 1999;180(6):1454–60.
Ojala K, Perälä J, Kariniemi J, Ranta P, Raudaskoski T, Tekay A. Arterial embolization and prophylactic catheterization for the treatment for severe obstetric hemorrhage. Acta obstetricia et gynecologica Scandinavica. 2005;84(11):1075-.
Carnevale FC, Kondo MM, de Oliveira Sousa W, Santos AB, da Leal Filho M, Moreira JM AM, et al. Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accreta. Cardiovascular and interventional radiology. 2011;34(4):758 – 64.
Ballas J, Hull AD, Saenz C, Warshak CR, Roberts AC, Resnik RR, et al. Preoperative intravascular balloon catheters and surgical outcomes in pregnancies complicated by placenta accreta: a management paradox. American journal of obstetrics gynecology. 2012;207(3):216. e1-. e5.
Cali G, Forlani F, Giambanco L, Amico ML, Vallone M, Puccio G, et al. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. European Journal of Obstetrics Gynecology Reproductive Biology. 2014;179:36–41.
Collins SL, Alemdar B, van Beekhuizen HJ, Bertholdt C, Braun T, Calda P, et al. Evidence-based guidelines for the management of abnormally invasive placenta: recommendations from the International Society for Abnormally Invasive Placenta. American journal of obstetrics gynecology. 2019;220(6):511–26.
Frank Wolf M, Singer-Jordan J, Shnaider O, Aiob A, Sgayer I, Bornstein J. The use of pre‐caesarean prophylactic intra‐arterial balloon catheters for suspected placenta accreta. Aust N Z J Obstet Gynaecol. 2019;59(4):528–32.
Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. American journal of obstetrics gynecology. 1997;176(3):723–6.
Peng Y, Jiang L, Peng C, Wu D, Chen L. The application of prophylactic balloon occlusion of the internal iliac artery for the treatment of placenta accreta spectrum with placenta previa: a retrospective case-control study. BMC Pregnancy Childbirth. 2020;20:1–8.
Salari N, Mohammadi M, Vaisi-Raygani A, Abdi A, Shohaimi S, Khaledipaveh B, Daneshkhah A, Jalali R. The prevalence of severe depression in Iranian older adult: a meta-analysis and meta-regression. BMC Geriatrics. 2020;20(1):39.
Sallam HF, Shady NW. Adjunctive intrauterine Foley’s Catheter Balloon adding to hypogastric artery ligation in the conservative management of morbid adherent placenta previa. International Journal of Reproduction, Contraception, Obstetrics and Gynecology.7(6):2094.
Darwish HS, Zaytoun HA, Kamel HA, Habash YH. Prophylactic preoperative balloon occlusion of hypogastric arteries in abnormal placentation; 5 years experience. The Egyptian Journal of Radiology Nuclear Medicine. 2014;45(3):751–9.
Omar K, Galal M. Comparison between Placental Site Injection of Vasopressin and Bilateral Internal Iliac Artery Ligation to Reduce Blood Loss during Cesarean Section for Placenta Praevia: A Randomized Controlled Trial. The Egyptian Journal of Hospital Medicine. 2017;31(5715):1–5.
Jiang Y, Liu H, Chen K. Prophylactic bilateral internal iliac arteries balloon occlusion in 13 patients of pernicious placenta previa with placenta accreta. Chinese Journal of Perinatal Medicine. 2013;16(8):461–4.
Broekman EA, Versteeg H, Vos LD, Dijksterhuis MG, Papatsonis DN. Temporary balloon occlusion of the internal iliac arteries to prevent massive hemorrhage during cesarean delivery among patients with placenta previa. International Journal of Gynecology Obstetrics. 2015;128(2):118–21.
Mei Y, Luo D, Lin Y. Clinical application of prophylactic internal iliac artery balloon occlusion combined with uterine artery embolization in patients with abnormally invasive placenta. The Journal of Maternal-Fetal Neonatal Medicine. 2018;31(24):3287–92.
Soyama H, Miyamoto M, Sasa H, Ishibashi H, Yoshida M, Nakatsuka M, et al. Effect of routine rapid insertion of Bakri balloon tamponade on reducing hemorrhage from placenta previa during and after cesarean section. Archives of gynecology obstetrics. 2017;296(3):469–74.
Fan Y, Gong X, Wang N, Mu K, Feng L, Qiao F, et al. A prospective observational study evaluating the efficacy of prophylactic internal iliac artery balloon catheterization in the management of placenta previa–accreta: A STROBE compliant article. Medicine. 2017;96(45).
Dai Mj J, Gx L, Jh, Zhang Y, Chen Y. Zhang Xb. Pre-cesarean prophylactic balloon placement in the internal iliac artery to prevent postpartum hemorrhage among women with pernicious placenta previa. International Journal of Gynecology Obstetrics. 2018;142(3):315–20.
Ono Y, Murayama Y, Era S, Matsunaga S, Nagai T, Osada H, et al. Study of the utility and problems of common iliac artery balloon occlusion for placenta previa with accreta. Journal of Obstetrics Gynaecology Research. 2018;44(3):456–62.
Bodner LJ, Nosher JL, Gribbin C, Siegel RL, Beale S, Scorza W. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Interv Radiol. 2006;29(3):354–61.
Picel AC, Wolford B, Cochran RL, Ramos GA, Roberts AC. Prophylactic internal iliac artery occlusion balloon placement to reduce operative blood loss in patients with invasive placenta. J Vasc Interv Radiol. 2018;29(2):219–24.
Wang Y-L, Su F-M, Zhang H-Y, Wang F, Zhe R-L, Shen X-Y. Aortic balloon occlusion for controlling intraoperative hemorrhage in patients with placenta previa increta/percreta. The Journal of Maternal-Fetal Neonatal Medicine. 2017;30(21):2564–8.
El-sayed MLM, El-huseiny AM, Ahmed MA, Saber S. Intraoperative internal iliac artery balloon occlusion versus ligation in cases of placenta previa accreta: A randomized trial. Edorium J Gynecol Obstet. 2016;2:34–40.
Wu Q, Liu Z, Zhao X, Liu C, Wang Y, Chu Q, et al. Outcome of pregnancies after balloon occlusion of the infrarenal abdominal aorta during caesarean in 230 patients with placenta praevia accreta. Cardiovasc Interv Radiol. 2016;39(11):1573–9.
Feng S, Liao Z, Huang H. Effect of prophylactic placement of internal iliac artery balloon catheters on outcomes of women with placenta accreta: an impact study. Anaesthesia. 2017;72(7):853–8.
Li K, Zou Y, Sun J, Wen H. Prophylactic balloon occlusion of internal iliac arteries, common iliac arteries and infrarenal abdominal aorta in pregnancies complicated by placenta accreta: a retrospective cohort study. European radiology. 2018;28(12):4959–67.
Dai M, Jin G, Lin J, Zhang Y, Chen Y, Zhou Q, et al. Control of postpartum hemorrhage in women with placenta accreta spectrum using prophylactic balloon occlusion combined with Pituitrin intra-arterial infusion. European radiology. 2020.
Chou MM, Kung HF, Hwang JI, Chen WC, Tseng JJ. Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation. Taiwanese Journal of Obstetrics Gynecology. 2015;54(5):493–8.
Tan CH, Tay KH, Sheah K, Kwek K, Wong K, Tan HK, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. Am J Roentgenol. 2007;189(5):1158–63.
McGinnis JM, Simula NK, Joseph K, Ubhi JS. Internal iliac artery balloon tamponade in placenta accreta: outcomes from the largest tertiary accreta referral centre in British Columbia. Journal of Obstetrics Gynaecology Canada. 2019;41(4):466–72.
Panici PB, Anceschi M, Borgia ML, Bresadola L, Masselli G, Parasassi T, et al. Intraoperative aorta balloon occlusion: fertility preservation in patients with placenta previa accreta/increta. The Journal of Maternal-Fetal Neonatal Medicine. 2012;25(12):2512–6.
Cho SB, Hong SJ, Lee S, Won JH, Choi HC, Ha JY, et al. Preoperative Prophylactic Balloon-Assisted Occlusion of the Internal Iliac Arteries in the Management of Placenta Increta/Percreta. Medicina. 2020;56(8):368.
Sun W, Duan S, Xin G, Xiao J, Hong F, Hong H, et al. Safety and efficacy of preoperative abdominal aortic balloon occlusion in placenta increta and/or percreta. J Surg Res. 2018;222:75–84.
Zeng C, Yang M, Ding Y, Yu L, Deng W, Hu Y, et al. Preoperative infrarenal abdominal aorta balloon catheter occlusion combined with Bakri tamponade reduced maternal morbidity of placenta increta/percreta. Medicine. 2017;96(38).
Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, editors. Williams Obstetrics. 23 rd ed. New York: McGraw Hill; 2010. pp. 757–98.
Bergakker SA. Case report: management of elective cesarean delivery in the presence of placenta previa and placenta accreta. AANA J. 2010;78(5):380–4.
Biswas R, Sawhney H, Dass R, Saran RK, Vasishta K. Histopathological study of placental bed biopsy in placenta previa. Acta Obstet Gynecol Scand. 1999;78(3):173–9.
Tong SY, Tay KH, Kwek YC. Conservative management of placenta accreta: review of three cases. Singapore Med J. 2008;49(6):e156-9.
Mitra J, Mitra K, Nandy S, Roy RN, Mandal PK, Biswas R. Utilisation pattern of blood in teaching hospital of Kolkata. Indian J Public Health. 2004;48(4):205–9.
McCarthy LJ. How do I manage a blood shortage in a transfusion service? Transfusion. 2007;47(5):760–2.
Behrman RE, Kliegman RM, Nelson WE. Nelson textbook of pediatric. 16th ed. Philadelphia: WB Saunders; 1996. 540 – 50.
Patrik SR. Obstetric management of prematurity. In: Avroy A. Neonatal perinatal medicine. Philadelphia, Mosby, 2002; 287.
Barbara J. High risk infant. In: Behrman RE. Nelson’s text book of pediatrics. Philadelphia, Saunders, 2007; 547.
Ville J. Premature delivery and inflammation. J Gynecol Obstet Bio Reprod. 2001;3091:12–6.
El-Jallad MF, Zayed F, Al-Rimawi HS. Emergency peripartum hysterectomy in Northern Jordan: indications and obstetric outcome (an 8-year review). Arch Gynecol Obstet. 2004;270(4):271–3.
Flood KM, Said S, Geary M, Robson M, Fitzpatrick C, Malone FD. Changing trends in peripartum hysterectomy over the last 4 decades. Am J Obst Gynecol. 2009;200(6):632–6.
Habek D, Becarevic R. Emergency peripartum hysterectomy in a tertiary obstetric center: 8-year evaluation. Fetal Diagn Ther. 2007;22(2):139–42.
Kashani E, Azarhoush R. Peripartum hysterectomy for primary postpartum hemorrhage: 10 year evaluation. Eur J Exp Biol. 2012;2(1):32–6.
Wong TY. Emergency peripartum hysterectomy: a 10-year review in a tertiary obstetric hospital. N Z Med J. 2011;124(1345):34–9.
Yucel O, Ozdemir I, Yucel N, Somunkiran A. Emergency peripartum hysterectomy: a 9-year review. Arch Gynecol Obstet. 2006;274(2):84–7.
Najam R, Basal P, Sharma R, Agarwal D. Emergency obstetric hysterectomy: a retrospective study at a tertiary care hospital. J Clin Diagn Res. 2010;4(4):2864–8.
Acknowledgements
This study is the result of Dr Samira Rasouli’s residency dissertation No. 3010295 approved by Kermanshah University of Medical Sciences. We would like to thank the esteemed officials of that center for accepting the financial expenses of this study.
Funding
By Deputy for Research and Technology, Kermanshah University of Medical Sciences (IR) (3010295). This deputy has no role in the study process.
Author information
Authors and Affiliations
Contributions
AN and NS and SR contributed to the design, MM statistical analysis, participated in most of the study steps. MK and MH and MM prepared the manuscript. MK and MH assisted in designing the study, and helped in the, interpretation of the study. All authors have read and approved the content of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval was received from the ethics committee of deputy of research and technology, Kermanshah University of Medical Sciences (3010295).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nankali, A., Salari, N., Kazeminia, M. et al. The effect prophylactic internal iliac artery balloon occlusion in patients with placenta previa or placental accreta spectrum: a systematic review and meta‐analysis. Reprod Biol Endocrinol 19, 40 (2021). https://doi.org/10.1186/s12958-021-00722-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-021-00722-3